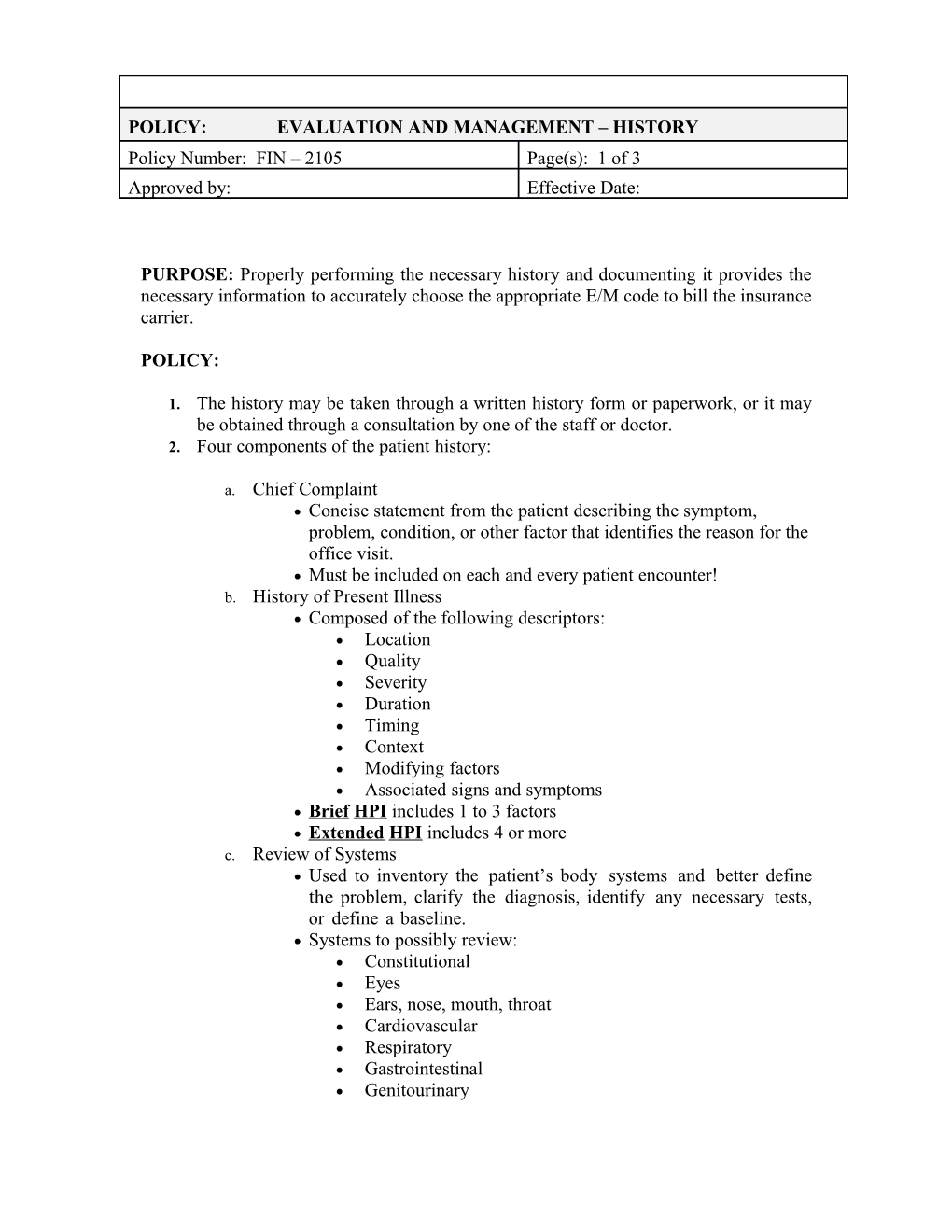
POLICY: EVALUATION AND MANAGEMENT – HISTORY Policy Number: FIN – 2105 Page(s): 1 of 3 Approved by: Effective Date:
PURPOSE: Properly performing the necessary history and documenting it provides the necessary information to accurately choose the appropriate E/M code to bill the insurance carrier.
POLICY:
1. The history may be taken through a written history form or paperwork, or it may be obtained through a consultation by one of the staff or doctor. 2. Four components of the patient history:
a. Chief Complaint Concise statement from the patient describing the symptom, problem, condition, or other factor that identifies the reason for the office visit. Must be included on each and every patient encounter! b. History of Present Illness Composed of the following descriptors: Location Quality Severity Duration Timing Context Modifying factors Associated signs and symptoms Brief HPI includes 1 to 3 factors Extended HPI includes 4 or more c. Review of Systems Used to inventory the patient’s body systems and better define the problem, clarify the diagnosis, identify any necessary tests, or define a baseline. Systems to possibly review: Constitutional Eyes Ears, nose, mouth, throat Cardiovascular Respiratory Gastrointestinal Genitourinary Musculoskeletal Integumentary Neurological Psychiatric Endocrine Hematologic/lymphatic Allergic/immunologic Problem-pertinent ROS – only one system is reviewed Extended ROS – review of 2 to 9 systems Complete ROS – review of 10 or more systems Must at minimum document positive and then state “all other systems are negative” d. Past, Family, and Social History An overall look at the patient’s past medical history, as well as any social or familial factors that might influence present condition. There are three elements of the PFSH: Past History - Information about past injuries, operations, allergies, illnesses, current medications Family History - Information about medical events in the patient’s family, such as diseases that may be hereditary or place the patient at risk. - At minimum, should include cancer, heart disease, stroke, diabetes, MS, and arthritis Social History - Marital status - Occupational history - Use of drugs, alcohol, and/or tobacco (mandatory that ALL patients over the age of 13 that are seen 3 or more times be asked about these…and document the answers) - Level of education “ Past Family History: Negative” is not adequate but “History of drug allergies is negative” would be adequate. Pertinent PFSH – review of history area directly related to the problem identified in the HPI. Must document at least ONE specific item from any of the three history areas. Complete PFSH – review of TWO or all THREE history areas depending on the category E/M service. Services that include a comprehensive assessment/reassessment of the patient require a review of all three areas. A review of two of the three history areas is sufficient for all other services.
3. Four levels of history based on the lowest classification of any of the above listed components:
a. Problem – focused HPI = Brief ROS = N/A PFSH = N/A b. Expanded Problem – focused HPI = Brief ROS = Problem pertinent PFSH = N/A c. Detailed HPI = Extended ROS = Extended PFSH = Pertinent d. Comprehensive HPI = Extended ROS = Complete PFSH = Complete