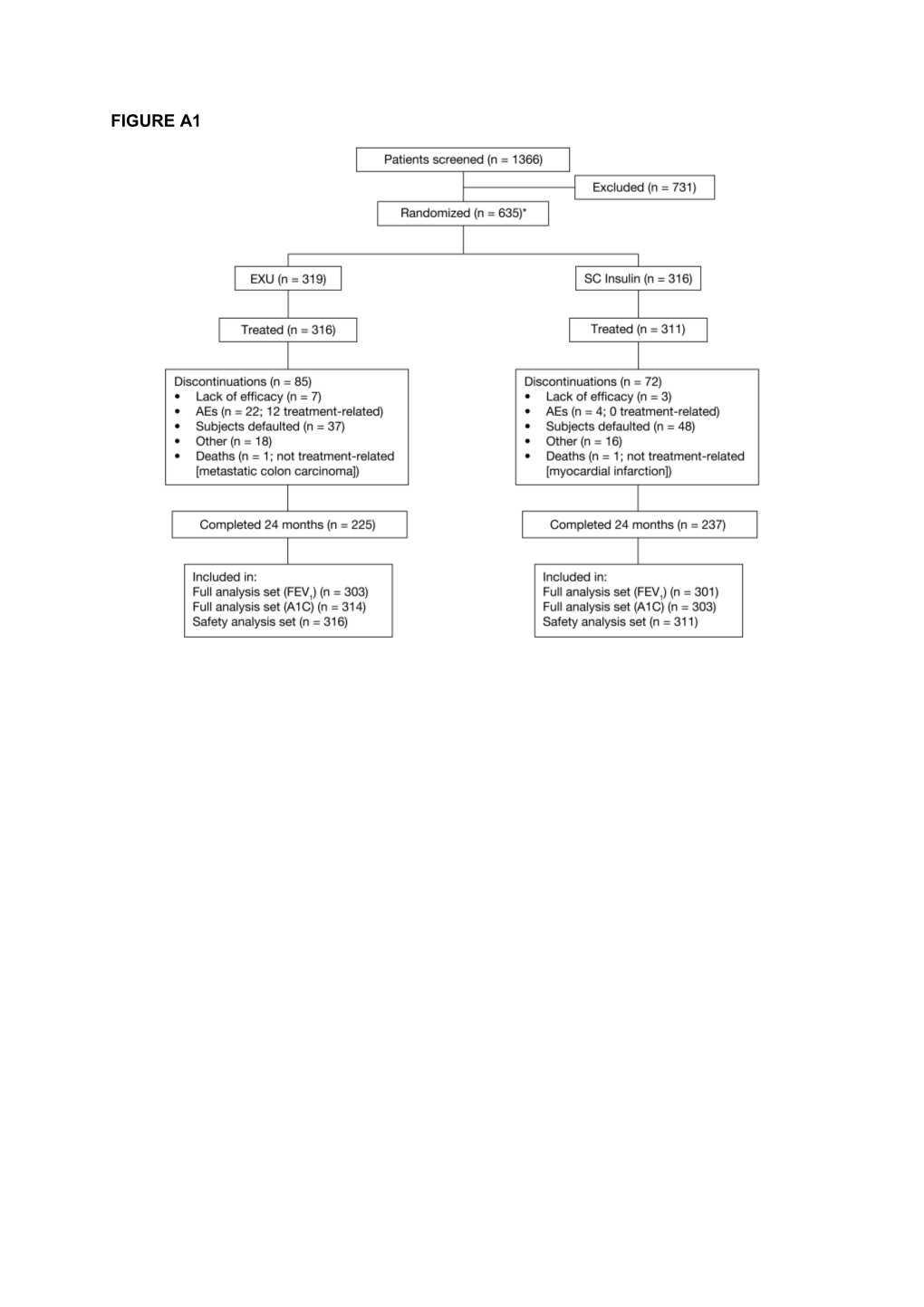
FIGURE A1 Table A1
Incidence and Number of Coughs in the EXU and SC Insulin Treatment Groups
Period EXU SC Insulin n Incidence Total n Incidence Total (% number (% number subjects) of cough subjects) of cough events events 0–3 Months 316 73 (23.1) 84 311 11 (3.5) 12 >3–6 Months 289 24 (8.3) 25 297 14 (4.7) 14 >6–9 Months 278 15 (5.4) 15 290 2 (0.7) 2 >9–12 Months 269 15 (5.6) 16 285 4 (1.4) 4 >12–15 Months 263 7 (2.7) 7 270 6 (2.2) 6 >15–18 Months 252 10 (4.0) 10 259 6 (2.3) 6 >18–21 Months 242 7 (2.9) 7 250 4 (1.6) 4 >21–24 Months 232 10 (4.3) 10 244 6 (2.5) 6
The majority of coughs were mild in severity: only 1 patient in each group reported severe cough. Changes in FEV1 were similar between EXU-treated subjects with and without cough (data not shown). A cough questionnaire was used in all patients at baseline, and subsequently in patients reporting cough that could not be explained by a concomitant condition such as respiratory infection. This questionnaire assessed 6 domains of cough on a 5-point scale ranging from 0 (none) to 4 (constant or severe). The domains were: cough frequency at night, frequency during the day, severity during the day, severity related to short-acting insulin dosing, timing related to short-acting insulin dosing, and cough productivity. Analysis of the cough questionnaire data showed that in the EXU group cough usually developed seconds or minutes after insulin inhalation and was seldom productive. Most patients reported that they rarely, or only occasionally, experienced cough during the day, and rarely or never at night. Table A2
Incidence (Number (%)) of Normal and Abnormal High Resolution Computerized Tomography (HRCT) Scans in Subjects who Underwent a Baseline and at Least 1 Post- baseline HRCT Scan of the Thorax
Normal HRCT scan at: Month 12 Month 24 Month 24 LOCF Baseline Specified EXU SC Insulin EXU SC Insulin EXU SC Insulin Time Point (n = 95) (n = 97) (n = 71) (n = 73) (n = 98) (n = 98) Yes Yes 64 (67.4) 63 (64.9) 41 (57.7) 49 (67.1) 62 (63.3) 62 (63.3) No 4 (4.2) 13 (13.4) 9 (12.7) 9 (12.3) 9 (9.2) 15 (15.3)
No Yes 6 (6.3) 5 (5.2) 4 (5.6) 6 (8.2) 8 (8.2) 7 (7.1) No 21 (22.1) 16 (16.5) 17 (23.9) 9 (12.3) 19 (19.4) 14 (14.3) - No 20 (21.1) 11(11.3) 17 (23.9) 7 (9.6) 19 (19.4) 10 (10.2) significant change - More 0 2 (2.1) 0 1 (1.4) 0 2 (2.0) abnormal - Less 1 (1·1) 3 (3.1) 0 1 (1.4) 0 2 (2.0) abnormal
LOCF, last observation carried forward.
A subgroup of patients from both treatment groups underwent high resolution computerized tomography (HRCT) of the thorax. To ensure comparability between the 2 treatment groups, baseline HRCTs were performed prior to randomization but after subjects had met all respiratory entry criteria. Subjects with abnormal HRCT findings at baseline that were judged to be clinically insignificant were allowed into the study. Follow-up HRCTs were performed at Months 12 and 24 or at time of discontinuation. All HRCTs were interpreted as either normal or abnormal by a third party radiologist without knowledge of treatment group assignment. For subjects with normal baseline scans, the incidence of abnormal HRCT results was comparable between treatment groups at Month 24. For subjects with abnormal baseline scans, no additional worsening of HRCT results occurred in EXU subjects at Month 24. The types of HRCT abnormalities identified were similar between groups (data not shown). Pfizer Statement
On October 18, 2007, Pfizer Inc announced that it would cease marketing Exubera because it did not meet customers’ needs or financial expectations. On April 9, 2008, Pfizer Inc announced that it was updating the Exubera Product Insert to include the following statement: In studies of Exubera in people with diabetes, lung cancer occurred in a few more people who were taking Exubera than in people who were taking other diabetes medicines. All of the people in these studies who developed lung cancer used to smoke cigarettes. There were too few cases to know if the lung cancer was related to Exubera.
Study Investigators
Study investigators were: Marie A. Adamczyk, Sallie O. Adams, Jorge L. Aguilera-Montalvo, Richard F. Arakaki, Stephen L. Aronoff, Gordon R. Bailey, Andre Belanger, Richard I. Bernstein, Jeffrey M. Bloom, Makram A. Boctor, Michael A. Bolognese, Robert R. Boomer, Gerard W. Boynton, Christina R. Bratcher, John B. Buse, Edwin Camilo-Vazquez, William T Cefalu, Merl A. Charles, Sidney E. Clevinger, Martin J. Conway, Larry C. Deeb, Jerry Drucker, Steven V. Edelman, Daniel Einhorn, Freddy G. Eliaschewitz, Norman Fishman, David Fitzpatrick, Vivian A. Fonseca, Miguel A. Franco Jr., David L. Fried, Jeffrey G. Geohas, Jorge L. Gross, George A. Grunberger, Jean-Pierre Halle, Lane T. Handke, Kenneth S. Hershon, Priscilla A. Hollander, Barry S. Horowitz, Edward S. Horton, Robert C. Hood, Irene M. Hramiak, Rajeev K. Jain, Philip B. James, Howard J. Kerstein, Charles Kilo, Steven Landgarten, Robert Lang, David C. Lau, Samuell Lerman, Seymour R. Levin, Peter A. Lewitt, Mark K. Lindley, Thomas W. Littlejohn III, Heather A. Lochnan, Sergio R. Mather, Avishai Mendelson, Joseph L. Milburn Jr., David B. Miller, Liam J. Murphy, Paul C. Norwood Jr., William A. Petit Jr., John R. Pullman, Efrain Rodriquez-Vigil, Julio Rosenstock, Stuart A. Ross, Richard C. Rowe, Joel J. Schnure, Sherwyn L. Schwartz, Terry W. Sherraden, Rubens Sievert, Jay Silverberg, James W. Snyder, Norman G. Soler, Joseph Soufer, David C. Subich, Daniel H. Sugimoto, Allen M. Sussman, Jose A. Tavarez-valle, Barbara E. Troupin, Clarence N. Uy, Mervyn U. Weerasinghe, Richard L. Weinstein, Peter N. Weissman, James P. Wigand, Jean-Francois Yale.