Appendix H. Hospitals: Quantitative Evidence Section A
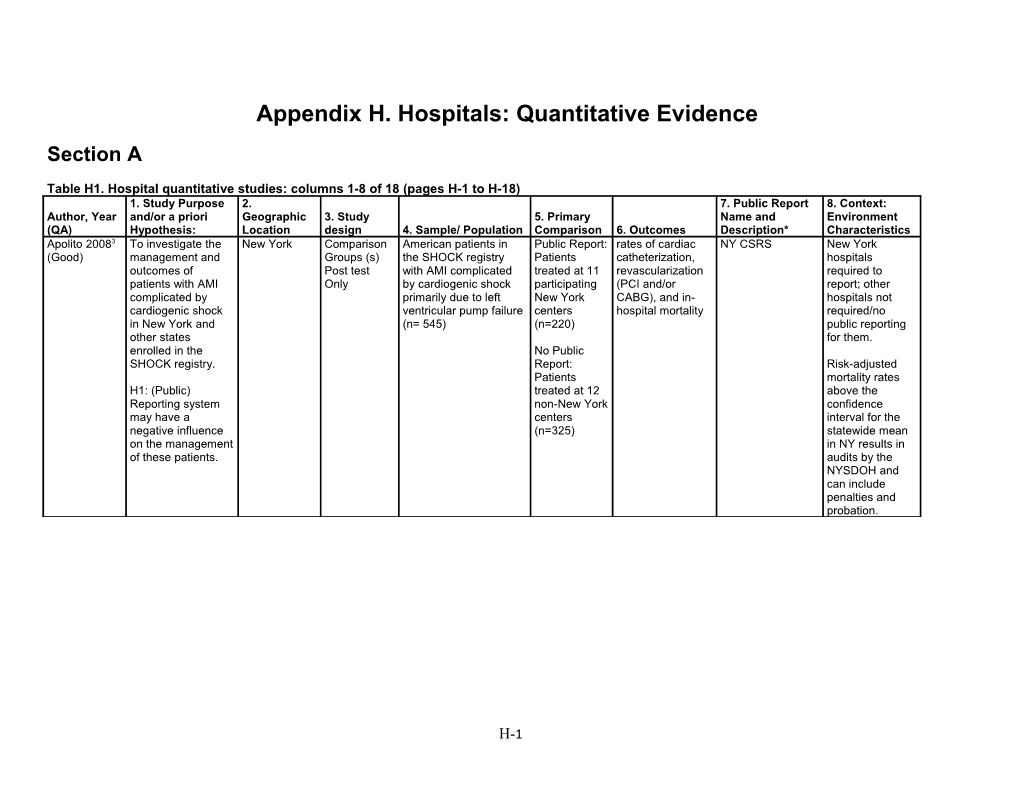
Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) 1. Study Purpose 2. 7. Public Report 8. Context: Author, Year and/or a priori Geographic 3. Study 5. Primary Name and Environment (QA) Hypothesis: Location design 4. Sample/ Population Comparison 6. Outcomes Description* Characteristics Apolito 20083 To investigate the New York Comparison American patients in Public Report: rates of cardiac NY CSRS New York (Good) management and Groups (s) the SHOCK registry Patients catheterization, hospitals outcomes of Post test with AMI complicated treated at 11 revascularization required to patients with AMI Only by cardiogenic shock participating (PCI and/or report; other complicated by primarily due to left New York CABG), and in- hospitals not cardiogenic shock ventricular pump failure centers hospital mortality required/no in New York and (n= 545) (n=220) public reporting other states for them. enrolled in the No Public SHOCK registry. Report: Risk-adjusted Patients mortality rates H1: (Public) treated at 12 above the Reporting system non-New York confidence may have a centers interval for the negative influence (n=325) statewide mean on the management in NY results in of these patients. audits by the NYSDOH and can include penalties and probation.
H-1 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Baker 20025 To examine Northeast Interrupted Time Hospitals in 30 nonfederal Mortality: Cleveland None (Fair) temporal trends Ohio/Cleveland Series (this Northeast Ohio hospitals in In-hospital Health Quality in risk-adjusted metropolitan article doesn’t Cleveland, OH death: Death Choice (CHQC) mortality area say, another were compared during the index between 1991 does. CHQC on 3 measures admission and 1997 for public reporting of mortality rates Medicare started 1993) (In hospital 30-day death: patients death, 30 day Death within 30 hospitalized in death, and Early days of Northeast Ohio post discharge admission for six medical death) of (including in- conditions: Medicare hospital and acute MI, CHR, patients across post discharge gastrointestinal multiple years. deaths) hemorrhage, COPD, Early post pneumonia, and discharge death: stroke. Discharged alive after the index hospitalization but dying within 30-days of admission.
H-2 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Baker 20034 (1) To examine Cleveland, OH Interrupted Time Nonfederal 12 six-month Market Share: Cleveland 30 hospitals, with 12 six-month (Fair) whether Series Hospitals, CHQC study The number of Health Quality periods of mortality data. hospitals that N=30(Outliers, periods between discharges for 6 Choice (CHQC) were identified n=17) July 1991 and general medical as mortality participating in December 1997 conditions at a outliers were the Cleveland (no data for hospital divided more likely to health Quality January-June by the total lose or gain Choice public 1992). number of market share reporting Comparison: general medical compared with program. Change in admissions at all hospitals with market share hospitals average during outlier participating in mortality. time period vs. CHQC. (2) To examine non-outlier time whether period. hospitals with higher than expected mortality had greater declines in 30-day mortality over time compared with hospitals with average mortality rates.
H-3 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Bridgewater To study Northwest Interrupted Time Data collected Pre-public Observed Multiple Reports Policy requiring public reporting of 20076 changes in England Series on 25,730 reporting period: Mortality: Any on named hospital specific morality data (Good) coronary artery consecutive April 1997 to in-hospital death Surgeon and surgery in years patients March 2001; Predicted Hospital spanning undergoing Post-public Mortality: Risk outcomes in UK publication of adult cardiac reporting period: adjusted cardiac surgery surgery (isolated April 2001- mortality based mortality data in coronary artery March 2005 on EuroSCORE. the UK. surgery) between April 1, Changes in the 1997 and March number of very 31, 2005 in the high risk northwest of patients England. undergoing coronary artery surgery: Stratified risk spectrum of patients undergoing surgery: low risk <6 EuroSCORE, high risk >=6 EuroSCORE, and very high risk >=11 EuroSCORE
H-4 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Carey 20067 To study the California One Group Hospitals in Pre public Mortality: In- California Public reporting prior to 2002 (Fair) impact of public Pretest Posttest California report: 1998- hospital death Coronary Artery voluntary, after mandatory in CA reporting and performing 2002 Post public and 30 day Bypass Graft changes in the CABG and PCI report: 2003- mortality or Mortality incidence of PCI operations 2004 readmission for Reporting and CABG Hospitals in both repeat Program procedures in groups: N = 115 procedure California. Hospitals Volume: performing Number of given CABG and PCI: procedures N~120 (6 (CABG vs PCI) stopped performing during study period and 7 started performing sometime during study period) Caron 19999 To identify Greater One Group, Hospitals after Cesarean rates Cesarean Cleveland None (Poor) whether Cleveland, OH Post Only publication of after CHQC section rates, Health Quality hospitals in the CHQC, with 3 in report VBAC rates Choice (CHQC) Cleveland, Ohio depth case area have reports, n=18. responded to Also survey of public concern quality about improving management their cesarean directors or section and personnel VBAC rates. deemed appropriate by the director, obstetricians, or labor and delivery nurses.
H-5 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Caron 20048 To assess Greater Time Series Hospitals in the Comparison Acute MI: CHQC None (Fair) whether Cleveland, OH post only Greater across 4 or 5 Length of stay, improvement in Cleveland area. time points on Mortality; CHF: one clinical area n=27 hospitals CHQC Length of stay, was associated for non- outcomes: Mortality; with obstetrics Acute MI: Stroke: Length improvements in outcomes. n=20 Length of stay, of stay, other areas. for obstetrics Mortality; CHF: Mortality; outcomes. Length of stay, Obstetrics: Total Mortality; caesarean Stroke: Length delivery rate, of stay, primary Mortality; caesarean Obstetrics: Total delivery rate, caesarean vaginal birth delivery rate, after caesarean primary delivery rate. caesarean delivery rate, vaginal birth after caesarean delivery rate Clough 2002 To determine Cleveland, OH Comparison Hospital 30 hospitals in Inpatient CHQC None (Fair)10 whether the vs. rest of Ohio Group (s) mortality rates in Cleveland area mortality CHQC had a Interrupted Time Cleveland and participated in beneficial effect Series Hospital CHQC vs. on inpatient mortality rates in hospitals in the mortality in the rest of Ohio rest of Ohio that Cleveland. did not participate in public reporting. Mortality data from 1992 to 1995. Cutler 200411 To examine the New York Time Series Cardiac surgery Mortality level of CABG cases NY CSRS None (Fair) impact of report post only hospitals on hospitals in performed, risk- cards on the New York states high-mortality adjusted allocation of report card and low- mortality rate patients across mortality (RAMR) hospitals. hospitals. Dranove 200313 To develop a New York and Interrupted Time Cohorts of Assuming NY Hospital Level NY CSRS and None H-6 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics (Good) framework and Pennsylvania Series Acute introduced Analysis: PA CABG Guide test three Myocardial report cards in 1. Mean of the potential effects Infarction (AMI) 1991 and PA in illness severity of report cards patients and 1993: before on the treatment patients NY: 4 years Pre admission or of cardiac receiving CABG and 3 years treatment of illness. in New York and Post hospital. This Pennsylvania PA: 6 years Pre outcome is from 1987-1994 and 1 year Post estimated by: A. Mean of Also Compare Patient’s total NY to other hospital states that do expenditures not have public one year prior to reporting. admission B. Mean of patients’ total days in hospital one year prior to admission Patient Level Analysis: 1. Illness severity in the year prior to treatment 2. Overall intensity of treatment in the year after admission 3. Whether patients received CABG, PTCA or Cath in the year after admission with AMI 4. All-case mortality and cardiac H-7 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics complications such as readmission for heart failure in the year after admission Dranove 200812 To propose and New York Interrupted Time Hospitals (n=18) Hospital Hospital NY CSRS None (Good) implement a Series in the NYC demand pre and Demand methodology to metropolitan post report card assess the area and CABG implementation; effectiveness of patients from Pre: 1989, Post: the “news” that the counties in 1991 report cards the same area provide to the (1989, n=6978; market. 1990, n=7916; 1991, n=8960). Elliott 201014 To assess how Across USA One Group Hospitals 1) Reporting at HCAHPS survey HCAHPS Annual reporting, 2008 and 2009 (Good) patients’ Pretest Posttest reporting on the 2008 vs. completed by All hospitals participating experiences Hospital reporting at patients with inpatient Compare 2009 care are website 2) Newly changing since between 2006 participating public reporting and 2008 with hospitals vs. reporting in original 2008 and 2009 participating hospitals 3) Hospitals with <100 beds vs. hospitals with >100 beds
H-8 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Evans 199715 To document Pennsylvania One Group All Pennsylvania One year to Change in PHC4: HER None (Fair) responses of Posttest Only acute care another: 1990 hospital Pennsylvania hospitals vs. 1992 efficiency hospitals to the measures public (length of stay dissemination and charges) by the Changes in Pennsylvania outcome Health Care measures Cost Containment Council (PHC4) of mandated hospital disclosures of financial and nonfinancial information. Foreman 199516 To examine Pennsylvania One Group Hospitals in Pre: fully Change in Hospital Only one year of publicly reported (Poor) whether Posttest Only Pennsylvania released data Yearly Number Effectiveness data for some of the hospitals. Pennsylvania’s n=156 (27 of (for 1989 or of Hospital Report (HER) Other hospitals did not have any Health Care 183 excluded 1990, released Patients by high publicly reported data, but Cost due to missing in 1991 or 1992) or low quality Consumer privately/internally reported data Containment data) (Quality Guide to were available to physicians for Council (PHC4) Post: Publicly determined by Coronary Artery referrals. public reports released data mortality rates) Bypass Graft led to market (for 1990, Surgery (CABG changes. released in Guide) Specifically, to 1992) determine whether Note: not all hospitals that data in the post received high or group were low quality public. ratings experienced growth or decline in patient admissions
H-9 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Friedberg To determine USA Interrupted Time Patients at least Pre-Public ED diagnosis: One of 10 Began public reporting in 2004; 200917 whether public Series 18 years old Report: Before Pneumonia, Hospital-level HQA receives performance data (Good) reporting has visiting EDs January 1, 2004 Bronchitis, performance from more than 98% of US acute been associated between 2001- Post-Public Congestive measures care hospitals with 2005 with Report: After heart failure reported by the overdiagnosis of primary January 1, 2004 (CHF), Other Hospital Quality pneumonia, respiratory Antibiotic use: Alliance excessive symptoms first dose of antibiotic use, or (excluding antibiotics within inappropriate conditions 4 hours of prioritization of limited to upper hospital arrival; patients with respiratory tract) inappropriate respiratory at hospitals with use of symptoms. Antibiotic Timing antibiotics Scores for at classified as least 25 antibiotic use in observations visits for asthma and CHF when pneumonia not present Waiting time to see a physician: not described
H-10 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Ghali, 199718 To compare Massachusetts Comparison All CABG cases No Report: Observed and NY CSRS and None (Fair) trends in Group (s) Time from fiscal years Massachusetts risk-adjusted in- Northern New mortality after Series Post 1990, 1992, and CABG patients hospital England CABG surgery Only 1994 in Public report mortality in Massachusetts and outcomes Massachusetts at all 12 feedback: New Changes in with the hospitals York and Patient Care decreases in performing Northern New linked to New York and CABG England CABG Performance northern New surgeries: patients Information England Case Selection from New York and northern New England included cases having undergone isolated CABG procedure. 1990 N=5395; 1992 N=5,818; 1994 N=5,915 from 12 hospitals Guru 200619 To evaluate the Ontario, Canada Interrupted Time All patients No Report: 1991 thirty-day Ontario Cardiac All CABG surgeons agreed to (Fair) differences in Series undergoing to 1994 (n = adjusted Reports publicly report outcomes (i.e., not patient isolated CABG 12691) mortality mandated, voluntary). Confidential characteristics surgery at 9 Confidential reporting instituted prior to public and outcomes cardiac surgery Report: 1995- reporting observed during institutions in 1998 (n = the transition Ontario between 32,272) from no Sept. 1, 1991 Public Report: reporting to and March 31, 1999-2001 (n = confidential, and 2002 (n = 22,730) ultimately public 67,693 perform report cards for CABG surgery in Ontario
H-11 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Hannan 199421 1) To examine New York Interrupted Time 30 providers Baseline: Three Intra-group NY CSRS Public Reporting of CABG for (Good) changes in the Series (hospitals and different groups changes in Hospitals and Surgeons required risk-adjusted surgeons) of ten created RAMR: RAMR in NY CABG performing using RAMR for each tercile outcomes CABG surgeries prior to public (Group 1= among in New York release. Then lowest RAMR, providers that state look at Group 2 = occurred during performance middle RAMR, 1989-1992 as a before and after Group 3 = function of the public report. Highest RAMR) risk-adjusted in initial period mortality in (1989 for 1989. hospitals; 1989 to 1990 for 2) To examine surgeons) changes in the compared to volume of RAMR for same patients tercile in 1992. undergoing CABG as a For surgeons: function of the Same performance of breakdown of providers in terciles, but 1989. groups 1 and 2 have an N of 32 each, while group 3 has an N of 31
Outlier status (high outliers, non-outliers, and low outliers, with low outliers having significantly lower than expected mortality rates)
Volume of procedures: H-12 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Hannan 1994b22 To assess New York Interrupted Time 30 New York Change over Risk-adjusted NY CSRS Public reporting mandatory (Good) changes in Series Hospitals. time after the mortality rate, outcomes of 57,187 patients release of report Expected CABG surgery undergoing cards. Baseline: mortality rate, in NY related to CABG surgery 1989 CABG surgery CABG report in New York volume, card from 1989 between 1989 Relationship through 1992. and 1992 between hospital RAMR and average severity of illness of patients Hannan 200320 To compare USA Multiple Group Outcomes of Hospitals In-hospital, 30- NYS CSRS; PA Good) CABG mortality Time Series Medicare participating in day, and risk HC4; NJ rates and patients public reporting adjusted in- Department of changes in undergoing efforts in NY, hospital/30-day Health and CABG mortality CABG PA, NJ, and OH mortality, Senior Services rates in regions procedures and internal changes in out- Registry; with quality between 1994 quality of-region CABG CHQC; Northern improvement/pu and 1999 who improvement surgery New England blic were 65 or older efforts in New Cardiovascular dissemination (n=911,407) England Study Group efforts with the compared to the (not public) rest of the rest of the country United States between 1994 and 1999 Hibbard 200324 To evaluate the Wisconsin Comparison Wisconsin Public reporting Increase in QI QualityCounts None (Fair) impact on Groups (s) hospitals hospitals (n=24) activities in quality Pretest Posttest -24 hospitals Private reporting obstetrics and improvement of (2 of 3 groups utilizing public hospitals (n=41) cardiac care (0- reporting Randomly reporting No reporting 7 possible QI hospital Assigned) -98 hospitals hospitals (n=46) activities) performance randomized to Public image publically versus either private perception (0-5 privately back to reporting or no scale) the hospital. reporting
H-13 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Hibbard 200523 To assess Wisconsin Comparison 24 hospitals in Hospitals in Improvements in QualityCounts None (Fair) hospital’s’ Groups (s) south central report vs. performance performance in Pretest Posttest Wisconsin. And hospitals given overall and in the 2 years (2 of 3 groups survey on long a report of just clinical areas following the Randomly term impacts their release of the Assigned) among performance vs. report community hospitals that members (n = received no 803). report Hollenbeak To identify Pennsylvania Comparison Patients treated Group 1, Time In-hospital PA Hospital None 200825 associations Groups (s) for 6 acute 1: Pennsylvania mortality Effectiveness/ (Good) between Pretest Posttest conditions: AMI, patients during Performance intensive public congestive heart period of Report reporting and in- failure, ‘limited’ public hospital hemorrhagic reporting, from mortality. stroke, ischemic 1997-1999 stroke, (n=515,266; 206 pneumonia, and hospitals) sepsis. Group 1, Time 2: Pennsylvania patients during period of ‘intensive’ public reporting, from 2000-2003 (n=689,006; 200 hospitals)
Comparison (Propensity matched to Pennsylvania): Group 2, Time 1: Patients in different states with limited public reporting, from 1997-1999 (propensity matched to Pennsylvania) H-14 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics (n=103,864; 53 hospitals) Group 2, Time 2: Patients in different states with limited public reporting, from 2000-2003 (n=59,239; 34 hospitals) Group 3: Limited reporting in CO and TX, from 1997-1999 (only 3 outcomes measures: AMI, CHF, pneumonia; n=21,952; 8 hospitals) Group 4: Intensive reporting in CO, TX, and CA from 200-2003 (only 3 outcomes measures: AMI, CHF, Pneumonia; n=9,456; 7 Hospitals)
4 Major comparisons: 1) Intensive Pennsylvania vs limited non- Pennsylvania 2) Limited Pennsylvania vs H-15 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics limited non- Pennsylvania (see note) 3) Limited PA vs Limited CO and TX (3 Outcomes) 4) Intensive PA vs Intensive CA, CO, TX (3 Outcomes)
N=168,104 Matched patient pairs Howard 200626 To determine USA Time Series Transplant Post only data Number of University Renal Released every 6 months online. (Fair) whether report post only Centers in the comparing patients Research and cards influence US patient choosing Education the number of transplant transplant Association kidney registrations and center during semiannual transplant hospital each report card reports on waiting list performance period. kidney registrations and across time transplant graph donor Intervention: survival transplants at Internet transplant reporting of the hospitals. Scientific Registry of Transplant Recipients Jang 201027 To assess the Korea Pre-Post Hip Public report vs Readmission Not named, None (Fair) impact of hemiarthroplasty no report rates Presented on reporting cases in Korea Pre: January Length of Stay National Heath performance from January 2006-December Change in Cost Insurance information on 2006-April 2008 2007 Patient selection Corporation the readmission (n=22851 Post: December website and in rate, length of surgeries at 851 2007-April 2008 press stay and cost of medical hip institutions) hemiarthroplasty . H-16 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Jang 201128 To evaluate the Korea One Group, Pre- Korean Cesarean rate; Cesarean rates Cesarean None (Fair) effect of Post hospitals that Pre-report: section rates Repeated Public provide August 2004- released by the Releases (RPR) cesarean July 2005, Post- Health for reducing sections report: August Insurance adjusted (N=1194) 2005- June Review and cesarean 2007 Assessment section rates Service and to analyze the characteristics of institutions responsive to RPR. Jha 200629 To determine if New York Time Series hospitals and Intervention: Performance: NY CSRS Required publication of (Good) high or low post only cardiac Public Release each hospital’s performance data for cardiac performance by surgeons in of Cardiac or surgeon’s surgeries in NY surgeons or New York Performance for RAMR. hospitals hospitals predicts (yearly) and Market Share: performance in surgeons number of cases the period when (released yearly of isolated data are most for three year CABG surgeries likely to be used periods) performed by a by consumers. Baseline: How given surgeon well hospitals or hospital in a To determine performed on given time whether hospital report cards period, divided or surgeon released in 1995 by the total performance (performance number of affects patient data for 1993); isolated CABG market share. How well surgeries surgeons performed by all To assess performed on surgeons/hospit whether the 1999 report als in NY during surgeon card that period. performance is (performance associated with Data for 1997) Discontinuation likelihood of Post: How well of surgeries: ceasing hospitals Any surgeon practice. performed in who did not H-17 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics 1996 (a year perform a single after release); surgery in a How well given calendar surgeons year assumed to performed in have left the 2000 (a year system. after release)
(For Market Share) Pre: Hospital or surgeon market share prior to the release of report card Post: Hospital or surgeon market share one year after release of report card
(For Surgeons Quitting) Pre: Performing surgeries prior to release Post: Discontinuing surgeries over the course of two years from release of public data
H-18 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Longo 199730 To examine the Missouri One Group Hospitals in Change after Number of ShowMe Buyers None (Fair) impact of an Pretest Posttest Missouri, N=82. release of public facilities that Guide: obstetrics Response report among 82 previously did Obstetrical consumer report rate=93% Hospitals listed not have Services developed and (82/88). in the Show Me service, but issued by the Buyer’s Guide: instituted Missouri Obstetrical service after Department of Services guide published. Health on published in hospital 1993. Data Number of behavior. collected 1994. facilities with policies changed, planned to change, or with change under discussion.
Obstetrical outcome trends.
H-19 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Mennemeyer To examine USA Interrupted Time All community Baseline/Pre- Use of hospital: HCFA mortality Media Coverage: whether or not 199731 whether the Series hospitals with a HCFA mortality change in yearly report the media (specifically (Fair) HCFA data standardized release: 1983; discharges newspapers) report rates and releases had an HCFA mortality Intervention: whether or not the media include impact on rate of more yearly release of stories that have positive or community than one HCFA mortality negative spins. hospital standard report. discharges over deviation from Change in the period 1984 the mean hospital to 1992. (outliers) in any discharges year during the attributed to period 1984- HFCA release of 2002. In information addition, 50% verses other sample of sources such hospitals that as: Media were never attention: outliers under Dummy this definition. variables Data from 1983 relating to included for newspaper changes over articles reporting time (baseline). either high or Over 9 year low mortality period, n= outlier at 23,564. specific hospitals and whether presence of a favorable story, unfavorable story, government action, and unusual death.
H-20 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Moscucci 200532 To compare Michigan and Comparison No public No public In-hospital NY CSRS None (Fair) demographic New York Groups (s) Post reporting: reporting: mortality data, test Only Hospitals in Michigan indications, and Michigan (n=8) Public in-hospital performing Reporting: New mortality from 11,374 York large multicenter consecutive PCI databases PCIs from 1998- in Michigan, 1999 where public Public reporting is not Reporting: mandated, and Hospitals in in New York New York where it is. (n=34) performing 69,048 consecutive PCIs during same time period. Mukamel, To test the New York One Group Hospitals and Compare Market shares NY CSRS None 199833 hypotheses that Posttest Only surgeons in hospitals over (Fair) hospitals and New York different years surgeons with (1990 vs. 1991 better outcomes vs. 1992) reported in the NYS Cardiac Surgery Reports experience a relative increase in their market share and prices.
H-21 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Omoigui 199634 It has been New York and Multiple Group n=9442 isolated Time trends of Mortality NY CSRS None (Poor) suggested that Cleveland, OH Time Series CABG mortality, this program operations morbidity and played a undertaken at referral case- significant role the Cleveland mix at the in the 41% clinic between Cleveland clinic. decrease in the Jan 1, 1989 to Post Only - risk-adjusted December 31, 1989 to 1993 mortality rate 1993. between 1989 and 1992. We hypothesized that some high- risk patients had migrated out of state for surgery. The purpose of this study was to determine whether cross- border risk- shifting resulted in changes in referral source case-mix and outcome from 1989 through 1993 at the Cleveland Clinic, a major regional, national, and international referral center located in the city of Cleveland, Ohio, 110 miles from the western border of New York state. H-22 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Peterson 199835 To examine the New York Interrupted Time All Medicare 2 yrs Pre-public 1. Percentage of NY CSRS None (Good) effects of Series patients age reporting: 1987- patients going provider profiling >=65 yrs who 89 out-of-state for on bypass underwent 2 yrs Post-public bypass surgery surgery access bypass surgery reporting: 1990- 2. Use of and outcomes in between 1987 92 bypass surgery elderly patients and 1992 in a following a MI in New York US hospital. had declined in n=39,396 in NY NY’s elderly Hospitals since the n=662,675 in initiation of non-NY (US) report cards 3. Whether bypass surgery outcomes were improving more rapidly in NY that in the rest of the nation. Pope Estimate the effect CA and rest of Time Series All hospitalized Comparing the Number of USNWR has None 200936 of the US News USA Post Test Medicare patients in USNWR ranking patients Specialty and (Fair) and World Only California (1998– by specialty (volume) and Hospital-level data Report hospital 2004) and a sample starting in 1993 to revenue rankings on both of other hospitals 1994-2002 in rest generated patient volume and around the of the country and from patients. hospital revenues. country (1994– 1998 to 2004 in 2002) California. N=446 Romano 200437 To determine New York and Times Series Outlier hospitals Pre: monthly Volume: total CHOP (CA) and Both states require public (Good) whether California Post Only in New York and volume prior to number of CSRS (NY) reporting hospitals California NY report for each patients with a recognized as using CSRS specific hospital topic condition performance report from Post: monthly or procedure, or outliers (either December 1992, volume for each related condition lower or higher December 1993, specific hospital or procedure, than expected) and June up to a year who were experience 1995CA using later admitted to a volume changes CHOP report specific hospital after publication from December in a specific of a report card. 1993 and from calendar month. May 1996 H-23 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics H1: Hospitals CA Hospitals with lower-than- volume by: expected AMI, mortality or AMI-related complication procedures rates experience (CABG, significant Percutaneous volume coronary increases, and angioplasty, hospitals with congestive heart higher-than- failure), expected Cervical mortality or Diskectomy, complication Lumbar rates experience Diskectomy, significant Diskectomy- volume related (Back or decreases in the neck year after procedures, publication of a Medical back report card. problems, Knee arthroplasty, Hip H2: Hospitals arthroplasty) with lower-than- expected NY Hospitals mortality or monthly volume complication by: rates attract CABG more patients CABG-related from long procedures distances, or (AMI, from outside Percutaneous their usual coronary catchment angioplasty, areas, after a Congestive report is heart failure) published. Labeled as “bypass effect,” and vice versa for higher-than- H-24 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics expected hospitals. Romano 200437 H3: Hospitals (Good) with lower-than- Cont. expected mortality or complication rates lead to an increased volume of clinically related conditions or procedures, and vice versa for higher-than- expected hospitals.
H4: Certain sociodemograph ic groups are more likely to hear about the release of a hospital report card and are better able tor more likely to use this information to select a hospital than other groups. Romano, 201138 To evaluate the California Multiple Group Hospitals in Pre and post Change in California CABG None (Fair) impact of 3 Time Series. California that public data Hospital Market Mortality reports from the perform isolated reporting for Share: The Reporting voluntary CA CABG three data difference in Program reports CABG Mortality surgeries: release time each hospital’s risk adjusted Reporting 2001: N=79 points, July market share operative Program on hospitals 2001, August between the 6 mortality for hospital market 2003: N=70 2003, and month periods surgeons and H-25 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics share, hospital 2005: N=77 February 2005 immediately hospitals mortality, and after and before performing patient selection release of a isolated CABG for coronary report. Market surgery. artery bypass share is graft surgery. determined by dividing its After Public number of Reporting: CABG surgery H1: Low discharges by mortality outliers the total number would of CABG experience discharges in increased nonfederal CABG market hospitals in share. California during the same H2: High period. mortality outliers would Change in experience Hospital decreased risk Mortality: adjusted Difference in inpatient CABG risk-adjusted mortality (due to hospital enhanced mortality quality between improvement specified efforts. periods after and before the H3: The release of each CCMRP public report. program would stimulate an overall decrease in risk adjusted inpatient CABG mortality for participants, without a parallel change H-26 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics in mean hospital severity of illness or high risk patient selection. Rosenthal To determine Cleveland, OH Interrupted Time 30 hospitals in Before reporting Changes in CHQC None 199739 changes in Series Northern Ohio vs. after mortality rates (Good) hospital reporting mortality that may have occurred in association with the Cleveland Health Quality Choice (CHQC) Program
H-27 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Shabino 200640 To report on Wisconsin One Group Hospitals in Changes in AMI, Acute MI Wisconsin None (Poor) CheckPoint Pretest Posttest Wisconsin, CHF, and outcomes: CheckPoint progress and to December 2004, Pneumonia % on aspirin at propose new n=115; outcomes arrival, % on measures. September between: aspirin at 2006, n=117 Early post-public discharge, % reporting beta blocker at (December arrival, % beta 2004) and 2 blocker at years after discharge, % public reporting ACEI/ARB Left (September ventricular 2006) systolic dysfunction, smoking counseling.
CHF outcomes: % Left ventricular function assessment, % ACEI/ARB Left ventricular function assessment, % Smoking counseling,% Discharge instructions
Pneumonia outcomes: % Oxygen assessment, % pneumonia vaccine, % smoking counseling, % antibiotic within 4 hours H-28 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Tu 2009 To evaluate Ontario, Canada Randomized Acute Care Both groups Primary: Mean AMI and CHF None (Fair) 41 whether the Delayed Hospitals in receive performance on Process public release of Intervention Ontario treating feedback. One each of 2 Measures for data on cardiac Trial (hospitals more than 15 receives early composite acute care quality randomized to patients with feedback process-of-care hospital indicators early public AMI per year. (January 2004) indicators: a) effectively reporting, or and then the percentage of stimulates reporting 21 data are publicly opportunities for hospitals to months later) released and applying each of undertake the media report 12 AMI quality the results; the indicators that improvement other receives were fulfilled activities delayed b) CHF quality feedback indicator (September “defined in a 2005) and then similar manner” public release, using 6 CHF but no media process-of-care feedback. indicators.
Secondary: 1 year and 30 day Hospital mortality; individual indicators creating the primary composite indicators; hospital report card impact survey results.
H-29 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Vladeck 198842 Hypothesize New York One Group Occupancy Group 1: NY Occupancy HCFA mortality New York City metropolitan (Poor) that occupancy Pretest Posttest rates for all New Hospitals with rates report hospitals overrepresented among in hospitals with York City higher-than- 269 outlier hospitals: 45 were from higher-than- general acute expected New York City or from surrounding expected death care hospitals; mortality rates counties; two-thirds had higher rates would n=70 (n=14); Group 2: than expected mortality, one-third decline after NY Hospitals had lower-than-expected rates. public release; with as- occupancy in expected hospitals with mortality rates as-expected (n= 47); Group death rates 3: NY Hospitals would not with lower-than- change; and expected occupancy in mortality rates hospitals with (n=9) lower-than- expected Pre: five mortality would calendar rise. quarters preceding March 12, 1986 release of HCFA data Post: three calendar quarters following release
H-30 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Wang 201143 Examines the Pennsylvania Times Series PA residents Post Only: 1998 Hospital PA CABG Guide None (Good) impact of CABG Post Only (aged 30 and to 2006 Quarterly report cards on above) who Volume a provider’s were Surgeon aggregate undergoing an Quarterly volume and isolated CABG Volume volume by procedure in PA patient severity hospitals and and then employ who were a mixed logit admitted model to between Q3 investigate the 1998 and Q1 of matching 2006. N= between 114,039) patients and providers Werner 201044 To examine USA Times Series 3476 acute care Change in Performance on CMS Hospital None (Good) changes in Post Only non federal US performance individual and Compare hospital process hospitals that level between composite performance in publicly reported 2004 and 2006 performance the first three quality of low vs. low- measures years after information on middle vs. Change in Hospital the CMS middle-high vs. hospital Compare was Hospital high performing performance initiated and test Compare hospitals from 2004 to whether these website from 2006 changes in 2004-2006 performance were correlated with changes in hospital mortality rates, length of stay, and readmission rates
H-31 Table H1. Hospital quantitative studies: columns 1-8 of 18 (pages H-1 to H-18) (continued) 1. Study 7. Public Purpose and/or Report Name Author, Year a priori 2. Geographic 4. Sample/ 5. Primary and 8. Context: Environment (QA) Hypothesis: Location 3. Study design Population Comparison 6. Outcomes Description* Characteristics Wuebker 200845 H1: The Rhine-Ruhr area Multiple Groups, 157 German Case numbers, Case Numbers: Klinikfuhrer None (Fair) publication of and Colgne- Time Series hospitals in two market share Hospital case Rhein-Ruhr quality Bonn area, regions, Rhine- and quality numbers (Clinic Guide), information has Germany Ruhr (study before (2003- Market share 74 hospitals in reduced patient group) and 2005) and after 35: Hospital the Rhine-Ruhr uncertainty. Cologne-Bonn public reporting market share for region Therefore (control group) (2005-2006) the market voluntarily published delineation of participated. hospitals extend 35km; Market Contains patient their market share 50: satisfaction, share or case Hospital market case numbers, numbers when share for the process, and compared with market outcome competing- non- delineation of indicators. publishing- 50km; hospitals Log_Distance: Average H2: From the logarithmized total of distance of the publishing treated patient hospitals, those to the hospital hospitals with overaverage quality tend to be preferred to competing hospitals with a quality below average. In other words: “good hospitals: should be able to extend their market shares or case numbers in comparison to “poor hospitals” * Public report descriptions are in Appendix E.
H-32