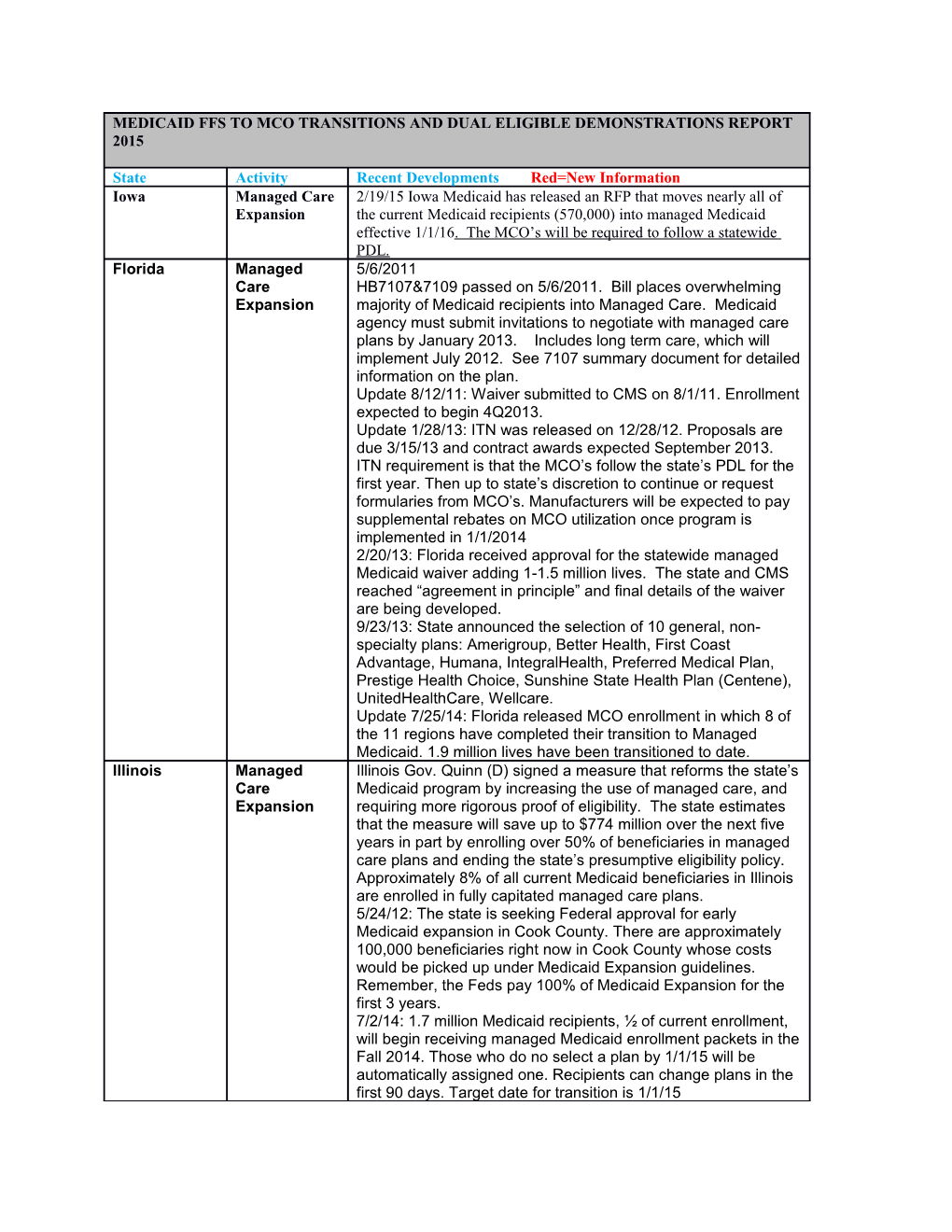
MEDICAID FFS TO MCO TRANSITIONS AND DUAL ELIGIBLE DEMONSTRATIONS REPORT 2015
State Activity Recent Developments Red=New Information Iowa Managed Care 2/19/15 Iowa Medicaid has released an RFP that moves nearly all of Expansion the current Medicaid recipients (570,000) into managed Medicaid effective 1/1/16. The MCO’s will be required to follow a statewide PDL. Florida Managed 5/6/2011 Care HB7107&7109 passed on 5/6/2011. Bill places overwhelming Expansion majority of Medicaid recipients into Managed Care. Medicaid agency must submit invitations to negotiate with managed care plans by January 2013. Includes long term care, which will implement July 2012. See 7107 summary document for detailed information on the plan. Update 8/12/11: Waiver submitted to CMS on 8/1/11. Enrollment expected to begin 4Q2013. Update 1/28/13: ITN was released on 12/28/12. Proposals are due 3/15/13 and contract awards expected September 2013. ITN requirement is that the MCO’s follow the state’s PDL for the first year. Then up to state’s discretion to continue or request formularies from MCO’s. Manufacturers will be expected to pay supplemental rebates on MCO utilization once program is implemented in 1/1/2014 2/20/13: Florida received approval for the statewide managed Medicaid waiver adding 1-1.5 million lives. The state and CMS reached “agreement in principle” and final details of the waiver are being developed. 9/23/13: State announced the selection of 10 general, non- specialty plans: Amerigroup, Better Health, First Coast Advantage, Humana, IntegralHealth, Preferred Medical Plan, Prestige Health Choice, Sunshine State Health Plan (Centene), UnitedHealthCare, Wellcare. Update 7/25/14: Florida released MCO enrollment in which 8 of the 11 regions have completed their transition to Managed Medicaid. 1.9 million lives have been transitioned to date. Illinois Managed Illinois Gov. Quinn (D) signed a measure that reforms the state’s Care Medicaid program by increasing the use of managed care, and Expansion requiring more rigorous proof of eligibility. The state estimates that the measure will save up to $774 million over the next five years in part by enrolling over 50% of beneficiaries in managed care plans and ending the state’s presumptive eligibility policy. Approximately 8% of all current Medicaid beneficiaries in Illinois are enrolled in fully capitated managed care plans. 5/24/12: The state is seeking Federal approval for early Medicaid expansion in Cook County. There are approximately 100,000 beneficiaries right now in Cook County whose costs would be picked up under Medicaid Expansion guidelines. Remember, the Feds pay 100% of Medicaid Expansion for the first 3 years. 7/2/14: 1.7 million Medicaid recipients, ½ of current enrollment, will begin receiving managed Medicaid enrollment packets in the Fall 2014. Those who do no select a plan by 1/1/15 will be automatically assigned one. Recipients can change plans in the first 90 days. Target date for transition is 1/1/15 MEDICAID FFS TO MCO TRANSITIONS AND DUAL ELIGIBLE DEMONSTRATIONS REPORT 2015
State Activity Recent Developments Red=New Information Iowa Managed Care 2/19/15 Iowa Medicaid has released an RFP that moves nearly all of Expansion the current Medicaid recipients (570,000) into managed Medicaid effective 1/1/16. The MCO’s will be required to follow a statewide PDL. North Managed April 2013: Governor announced the intent to develop a plan to Carolina Medicaid move FFS lives to Managed Medicaid. The program is called: Expansion Partnership for a Healthy North Carolina. 12/5/13: NC Medicaid Reform Committee met and began discussions. 3 more meetings to take place in 2014 (Jan-Mar). Reform proposal expected to be presented to the legislature in Spring 2014 March 2014: Medicaid Reform Advisory Group proposes to begin moving to ACO model in July 2015. By 2018, 80% of Medicaid lives would be managed by ACO’s. ACO’s would be at full risk. Alabama Managed 3/27/13: The Alabama Medicaid Advisory Commission is Medicaid recommending that they move all lives into MCO’s by 2017. The Expansion plan is being presented to the House and Senate. 6/17/13: State released a proposal of the 5 regions in the state. MCO plans to be selected and ready to go by Oct 2016. 5/30/14 Alabama submitted a 1115 Demonstration waiver allowing them to move FFS to a RCO (capitated) model. Delaware Managed On 1/31/14 a RFP was released for the re-procurement of the Medicaid MCO’s. Proposals are due April 4, 2014. Currently Delaware carves out the pharmacy benefit from the MCO’s and manages it in the FFS benefit. The RFP indicates the state will be removing the carve out and instead implementing a statewide PDL. Delaware has come to agreement with United HealthCare and soon with Highmark. Effective 1/1/15 Nebraska Managed State intends to release a RFP in July 2014 for it’s statewide Medicaid managed care program. Transition expected in 2015. No Expansion progress to date
Louisiana Managed Bayou Health Program contracts with MCO’s are expiring and Medicaid the state intends to release an RFP for plans to change to a fully Expansion capitated model. New contracts will take place in Feb 2015. This impacts 900,000 lives Indiana Managed Healthy Indiana Plan 2.0 Medicaid This is Indiana’s Medicaid expansion that will assist about Expansion 350,000 These recipients will be managed by MCO’s who will be fully capitated for all services. Pharmacy will NOT be carved out as standard FFS is. Coverage begins 2/1/15 Michigan Managed Michigan will carve out pharmacy benefit from MCO’s beginning Medicaid 2/1/16 DUAL ELIGIBLE DEMONSTRATION PROJECTS Missouri Dual Eligible Timeframe: Not Pursuing Demonstratio n MEDICAID FFS TO MCO TRANSITIONS AND DUAL ELIGIBLE DEMONSTRATIONS REPORT 2015
State Activity Recent Developments Red=New Information Iowa Managed Care 2/19/15 Iowa Medicaid has released an RFP that moves nearly all of Expansion the current Medicaid recipients (570,000) into managed Medicaid effective 1/1/16. The MCO’s will be required to follow a statewide PDL. California Dual Eligible Timeframe: January 2014 MOU executed with CMS Demonstratio Program will cover 685,000 Duals. Program will begin June n 2013 using a capitated model. Opt enrollment bagan 4/1/14. Passive enrollment 5/1/14 HEALTH PLANS: CALOPTIMA, CARE 1ST PARTNER PLAN, COMMUNITY HEALTH GROUP PARTNER, HEALTH NET, HEALTH PLAN OF SAN MATEO, INLAND EMPIRE HALTH PLAN, LA CARE, MOLINA, SANTA CLARA FAMILY HEALTH PLAN, ANTHEM Colorado Dual Eligible Timeframe: MOU executed 2/28/14 Demonstratio Duals program will cover 62,982 lives. Passive enrollment n began 9/1/14 Connecticut Dual Eligible Timeframe: 2013 Delayed MOU Pending Demonstratio Program will cover 57,569 lives . n Idaho Dual Eligible CANCELLED Demonstratio n Iowa Dual Eligible Timeframe: Not pursuing Demonstratio n Illinois Dual Eligible Timeframe: 1/1/14 (voluntary enrollment) MOU executed with Demonstratio CMS n Contracts were awarded to Aetna Better Health, IliniCare Health Plan (Centene), Meridian Health Plan of Illinois, HealthSpring of Illinois, Humana Health Plan, BCBS of Illinois, Molina Healthcare of Illinois, and Health Alliance Medical Plans. The program began 1/1/13 and will cover 156,000 Duals. Voluntary enrollment begins 3/1/14 and passive enrollment will begin 6/1/14 Massachusett Dual Eligible Timeframe: Oct 2013 MOU executed with CMS s Demonstratio Contracts awarded to BCBS of Mass, Boston Medical Center n HealthNet Plan, Commonwealth Care Alliance, Fallon Total Care, Neighborhood Health Plan, and Network Health. The state was first to enter a MOU with CMS. Program will cover 90,000 Duals between ages of 21-64. Contracts begin 4/1/13 8/7/13: Neighborhood Health, BCBS, and Boston Medical Ctr have dropped out of participation citing low rates and losses. MEDICAID FFS TO MCO TRANSITIONS AND DUAL ELIGIBLE DEMONSTRATIONS REPORT 2015
State Activity Recent Developments Red=New Information Iowa Managed Care 2/19/15 Iowa Medicaid has released an RFP that moves nearly all of Expansion the current Medicaid recipients (570,000) into managed Medicaid effective 1/1/16. The MCO’s will be required to follow a statewide PDL. Michigan Dual Eligible Timeframe: MOU executed 4/3/14 Demonstratio 100,000 duels will be impacted. Opt In enrollment begins n 10/1/14. Program Opt-IN enrollment is effective 3/1/15. Passive enrollment begins 5/1/15 It will be a 3-way capitated model between Michigan-CMS-8 ICO’s (Integrated Care Organizations. Behavior health is carved out to Michigan’s Prepaid Inpatient Health Plans (PIHP). The Behavior Health carve out includes substance abuse disorder. Participating plans are: AmeriHealth Michigan, Coventry, Fidelis, SecureCare, Meridian Health Plan, Midwest Health Plan, Molina Healthcare, UnitedHealthcare, Upper Peninsula Health Plan Minnesota Dual Eligible Timeframe: Not pursuing Demonstratio n Ohio Dual Eligible Timeframe: MOU executed 12/11/12 Demonstratio Contracted with Aetna, Molina, CareSource/Humana, Centene, n and UnitedHealth. Will cover 114,972 Duals. Medicaid population will begin enrollment in May-June 2014. Medicare population from May-December. 1/1/15 will begin auto- enrollment for Medicare population Oklahoma Dual Eligible Timeframe: 2013 MOU Pending Demonstratio Program will cover 79,891 Duals. n Wisconsin Dual Eligible Timeframe: 2013 MOU Pending Demonstratio Program to begin 4/1/13 and will cover 17,600 Duals n Arizona Dual Eligible Timeframe: 2014 Demonstratio Project Cancelled n Hawaii Dual Eligible Timeframe: 2014 Demonstratio Program will begin 1/1/14 and will cover 24,189 Duals n Project Cancelled Idaho Dual Eligible Timeframe: 2014 Demonstratio Proposals from MCO’s due May-June 2013. Capitated model n will cover 17,735 Duals. Program to begin 1/1/14 New York Dual Eligible Timeframe: 2014 MOU Executed with CMS Demonstratio Program to begin 1/1/14 and will cover 133,880 Duals using a n capitated model. Voluntary enrollment begins 1/1/15. Passive enrollment begins 4/1/15. Update 1/15/15: Letters sent to 100,000 recipients on 1/1/15 telling they would be passively enrolled effective 4/1/15. Recipients have the ability to opt out of the demonstration program MEDICAID FFS TO MCO TRANSITIONS AND DUAL ELIGIBLE DEMONSTRATIONS REPORT 2015
State Activity Recent Developments Red=New Information Iowa Managed Care 2/19/15 Iowa Medicaid has released an RFP that moves nearly all of Expansion the current Medicaid recipients (570,000) into managed Medicaid effective 1/1/16. The MCO’s will be required to follow a statewide PDL. Rhode Island Dual Eligible Timeframe: Nov 2013 MOU Pending Demonstratio RFP issued 5/30/14. n Impacts 31,668 Duals Program start date of 1/1/15 Opt In enrollment to begin 4-2015 South Dual Eligible Timeframe: MOU executed 10/25/13 Carolina Demonstratio MCO contracts to Absolute Total Care (Centene), Advicare, n Molina, Select Health, and Welcare Program will cover 53,000 Duals and will use a capitated model. Opt IN enrollment begins 2/1/15. Passive enrollment begins 6/1/15 Tennessee Dual Eligible Timeframe: Not pursuing Demonstratio n Texas Dual Eligible Timeframe: 2015 MOU Approved Demonstratio Program will pilot in six of the states most populous counties n (Bexar, Dallas, El Paso, Harris, Hidalgo, and Tarrant) Expects to cover 147,000 lives. Participating plans include: Amerigroup, Molina, Superior, United, and Cigna-HealthSpring Enrollment has begun 3/1/15http://www.hhsc.state.tx.us/medicaid/managed-care/dual- eligible/
Vermont Dual Eligible Timeframe: Not pursuing Demonstratio n Virginia Dual Eligible Timeframe: Feb 1, 2014 Demonstratio MCO contract awards expected July 2013. Program covers n 78,600 of the 110,634 Duals. Program begins 1/1/14 using capitated model. MOU executed 5/22/13 7/12/13: state has selected three plans: Anthem HealthKeepers, Humana, and Virginia Premier Enrollment completed 5/1/14 Washington Dual Eligible Timeframe: 2014 MOU executed with CMS Demonstratio MCO contract awards expected July 2013. Covers 115,000 n Duals. Program begins 1/1/14. Capitated model.
Updated 7/9/15