Reduction of Adhesions Using a Composite Alloderm/Polypropylene Mesh for Abdominal Wall Reconstruction
Charles E. Butler, M.D. and Victor G. Prieto, M.D., Ph.D.
Introduction
Polypropylene (PP) mesh is the most commonly used structural biomaterial for ventral hernia repair. Its high tensile strength and macroporous structure allow fibrovascular tissue to surround the PP fibers, resulting in incorporation of the mesh into the abdominal wall to form a strong, permanent repair. PP mesh placed adjacent to peritoneal structures, however, causes dense abdominal adhesions, makes re-operation more complicated, and increases the risk of bowel obstruction and fistula.
A means of reducing or eliminating abdominal adhesions when prosthetic mesh is used would have a tremendous clinical impact by reducing complication rates and potentially reducing hospital costs. Numerous substances, both permanent and biodegradable, have been used as a barrier to adhesions with a wide range of success. Despite the commercial availability of numerous antiadhesive barrier products, their widespread use has not occurred, largely because of inconsistent results and difficulties associated with their use.
We previously demonstrated that adhesions to PP mesh can be significantly reduced by using composite mesh constructed with an acellular synthetic dermal analogue (collagen-glycosaminoglycan matrix) incorporated into PP mesh.1
Alloderm, a commercially available dermal analogue, consists of decellularized human dermis and has excellent handeling properties. This material contains a preformed, three-dimensional collagen matrix with native basement membrane (BM) components on one surface and is gradually revascularized and replaced with autologous tissue.
Hypothesis
Alloderm can be combined with PP mesh to reduce adhesions and serve as a biodegradable scaffold to generate an autologous vascularized tissue layer separating and protecting the abdominal viscera from the PP mesh and the BM containing surface of Alloderm may reduce adhesions to a greater degree than the dermal surface.
Materials and Methods
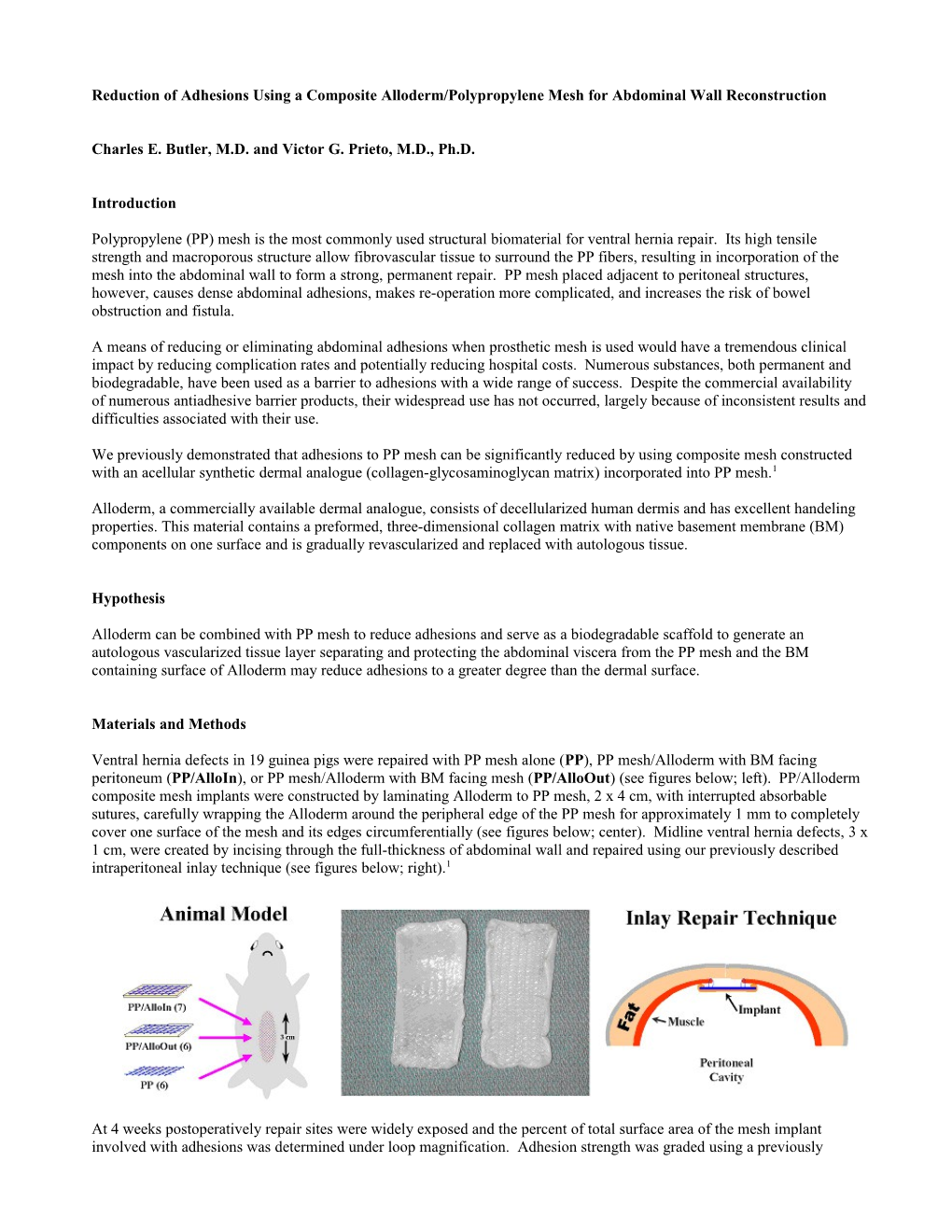
Ventral hernia defects in 19 guinea pigs were repaired with PP mesh alone (PP), PP mesh/Alloderm with BM facing peritoneum (PP/AlloIn), or PP mesh/Alloderm with BM facing mesh (PP/AlloOut) (see figures below; left). PP/Alloderm composite mesh implants were constructed by laminating Alloderm to PP mesh, 2 x 4 cm, with interrupted absorbable sutures, carefully wrapping the Alloderm around the peripheral edge of the PP mesh for approximately 1 mm to completely cover one surface of the mesh and its edges circumferentially (see figures below; center). Midline ventral hernia defects, 3 x 1 cm, were created by incising through the full-thickness of abdominal wall and repaired using our previously described intraperitoneal inlay technique (see figures below; right).1
At 4 weeks postoperatively repair sites were widely exposed and the percent of total surface area of the mesh implant involved with adhesions was determined under loop magnification. Adhesion strength was graded using a previously described scale 1 from 0 to 3 with intervals of 0.5; where 0 = no adhesions, 1 = adhesions easily freed with gentle tension, 2 = adhesions freed with blunt dissection, and 3 = adhesions requiring sharp dissection to be freed from the implant site. Using computer-aided planimetry, the resulting thickness and degree of cellular infiltration into the Alloderm was quantified.
Sections from each group underwent immunohistochemical staining for basement membrane components (laminin and type IV collagen), vascular endothelial cells (factor VIII) and peritoneal cells (pancytokeratin cocktail including: AE1/AE3, CAM5, Zym5.2 and MNF116).
The Fisher’s exact test was used to compare the incidence of bowel involvement. The Mann-Whitney test was used for all other statistical comparisons with values of p<0.05 considered significant.
Results
Gross Results All implants were firmly attached to the musculofascial edges of the abdominal wall defect. There was a significantly lower adhesion surface area involvement in both the PP/AlloIn (12.4% 8.3%) and PP/AlloOut (9.5% 12.1%) groups than the PP group (79.5% 6.1%) (see figures below).
Adhesion grade was also significantly lower in the PP/AlloIn (1.0 0.41) and PP/AlloOut (0.50 0.45) groups than the PP group (2.9 0.20). Bowel was adherent to 67% of PP repair sites and 0% of the PP/AlloIn and PP/AlloOut repairs. There was, however, no significant difference in adhesion surface area or grade, or bowel involvement between the PP/AlloIn and PP/AlloOut repairs.
Histologic Results All implants were fully incorporated into the musculofascial edges of the repair sites with dense fibrovascular infiltration into the PP mesh. There was no obvious difference in the degree of fibrovascular incorporation or foreign-body giant cell reaction surrounding the PP mesh fibers between the 3 groups. There were fragments of intestinal tissue firmly attached to the PP but not PP/Alloderm repair sites. The incompletely degraded Alloderm formed a vascularized tissue layer (Allo) beneath the mesh (unlike scar tissue) with a thickness of 634 175 m and 541 161 m in the PP/AlloIn and PP/AlloOut groups, respectively, whereas a significantly thinner, dense scar layer 52 6 m thick was formed in the PP group.
2 A distinct tissue layer (SubAllo) consisting of blood vessels and an acute and chronic infiltrate (macrophages, neutrophils and lymphocytes) was formed beneath the Allo layer in all PP/AlloIn and PP/AlloOut repairs. There was no significant difference in the Allo or SubAllo layer thickness or degree of cellular infiltration into the Allo layer between PP/AlloIn and PP/AlloOut repairs.
Immunohistochemical labeling for type IV collagen and laminin clearly localized the BM zone in the incompletely degraded Alloderm. Factor VIII labeling showed neovascularization throughout the Alloderm. Vessels from the repair site were seen entering the Alloderm regardless of BM surface orientation. There was no obvious difference in the amount of neovascularization between PP/AlloIn and PP/AlloOut repairs. Anticytokeratin staining confirmed the presence of peritoneal cells on the undersurface of the SubAllo layer in PP/AlloIn and PP/AlloOut repairs.
Discussion
The combination of Alloderm and structural prosthetic mesh used for abdominal wall reconstruction is an appealing strategy to reduce abdominal adhesions to the repair site. The Alloderm markedly reduced the surface area and strength of adhesions to the repair sites. Moreover, adhesions to bowel were completely prevented.
All cellular elements, responsible for the majority of skin alloantigenicity, are removed during the processing, leaving the native dermal extracellular matrix, including collagen fiber network and glycosaminoglycans intact. It is degraded by the host and replaced with autologous vascularized tissue, unlike scar, that both inhibits adhesion formation and provides a protective barrier between the mesh and intra-abdominal structures. This tissue layer could reduce the incidence of subsequent visceral adhesion, erosion, and/or fistula formation by preventing direct, ongoing mesh fiber exposure to intraperitoneal structures and facilitate re-operative surgery by providing a safe plane of dissection. Furthermore, gross and histologic results demonstrated that the Alloderm did not reduce fibrovascular infiltration and incorporation of the abdominal wall defect edges into the PP mesh.
In contradiction to our original hypothesis, it appeared that the BM surface orientation of Alloderm (either towards or away from intraperitoneal structures) did not significantly effect adhesion formation. In addition there was no difference in the thickness or degree of cellular infiltration into the Allo layer, or thickness of the SubAllo layer in this animal model.
To our knowledge, this is the first study to characterize the gross, histologic, histomorphologic and immunohistologic response of Alloderm exposed to an intraperitoneal environment and the effects of BM surface orientation. Future studies in this area will be important to help develop strategies to optimize the efficacy of adhesion reduction to prosthetic materials.
Conclusions
Composite Alloderm/PP mesh markedly reduces adhesions to abdominal wall repair sites without impairing fibrovascular tissue incorporation into the mesh. The Alloderm functioned as a biodegradable tissue scaffold enabling formation of a well-vascularized tissue layer separating the PP mesh from intraperitoneal structures. Orientation of the BM does not appear to significantly influence these effects. Our results indicate that the combination of biodegradable tissue scaffolds with prosthetic materials may have useful clinical applications for abdominal wall repair, reducing the morbidity associated with prosthetic implants and facilitating possible subsequent re-operations.
References
1. Butler, C.E., Navarro, F.A., Orgill, D.P. Reduction of abdominal adhesions using composite collagen-GAG implants for ventral hernia repair. J. Biomed. Mater. Res. 58: 75-80, 2001.
3