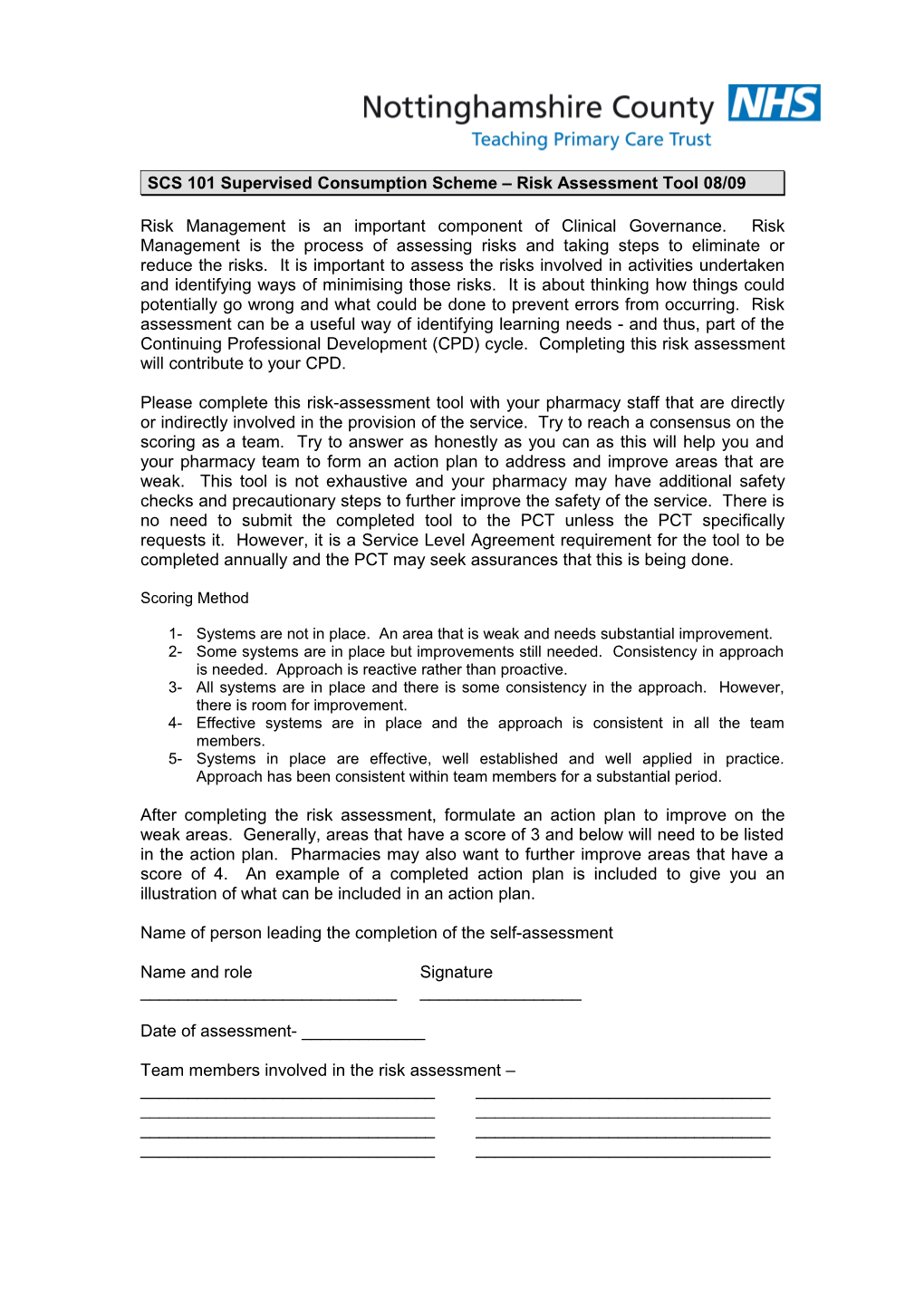
SCS 101 Supervised Consumption Scheme – Risk Assessment Tool 08/09
Risk Management is an important component of Clinical Governance. Risk Management is the process of assessing risks and taking steps to eliminate or reduce the risks. It is important to assess the risks involved in activities undertaken and identifying ways of minimising those risks. It is about thinking how things could potentially go wrong and what could be done to prevent errors from occurring. Risk assessment can be a useful way of identifying learning needs - and thus, part of the Continuing Professional Development (CPD) cycle. Completing this risk assessment will contribute to your CPD.
Please complete this risk-assessment tool with your pharmacy staff that are directly or indirectly involved in the provision of the service. Try to reach a consensus on the scoring as a team. Try to answer as honestly as you can as this will help you and your pharmacy team to form an action plan to address and improve areas that are weak. This tool is not exhaustive and your pharmacy may have additional safety checks and precautionary steps to further improve the safety of the service. There is no need to submit the completed tool to the PCT unless the PCT specifically requests it. However, it is a Service Level Agreement requirement for the tool to be completed annually and the PCT may seek assurances that this is being done.
Scoring Method
1- Systems are not in place. An area that is weak and needs substantial improvement. 2- Some systems are in place but improvements still needed. Consistency in approach is needed. Approach is reactive rather than proactive. 3- All systems are in place and there is some consistency in the approach. However, there is room for improvement. 4- Effective systems are in place and the approach is consistent in all the team members. 5- Systems in place are effective, well established and well applied in practice. Approach has been consistent within team members for a substantial period.
After completing the risk assessment, formulate an action plan to improve on the weak areas. Generally, areas that have a score of 3 and below will need to be listed in the action plan. Pharmacies may also want to further improve areas that have a score of 4. An example of a completed action plan is included to give you an illustration of what can be included in an action plan.
Name of person leading the completion of the self-assessment
Name and role Signature ______
Date of assessment- ______
Team members involved in the risk assessment – ______Risk Assessment Area 1 2 3 4 5 1 Standard Operating Procedures (SOPs) 1.1 A SOP for the service exists and is written clearly and in a logical manner 1.2 All relevant pharmacy staff have read and familiarised themselves with the SOP and have signed a declaration to that extent 1.3 The SOP is easily accessible and located in a visible manner for easy reference 1.4 Working practices reflect fully what is written on the SOP 1.5 The SOP is reviewed regularly and is up-to-date 2 Changes to CD regulations 2.1 The pharmacy is fully aware and is familiar with all the recent changes to the Misuse of Drugs Regulations 2001 and keeps abreast of changes with the Safer Management of Controlled Drugs guidance issued by the Department of Health. 2.2 The pharmacy is aware of who the PCT CD Accountable Officer is and of their contact details 3 FP10MDA prescriptions 3.1 The pharmacy is fully aware of the home office approved wordings in relation to instalment dispensing and any relevant RPSGB guidance relating to instalment dispensing 3.2 A system is in place to check whether prescriptions have arrived in time and to chase up the relevant Drug prescription services where FP10MDA prescriptions have not arrived in time. (This will allow the pharmacy and prescription services adequate time to sort out a replacement prescription should prescriptions get lost/delayed in the post) 3.3 A system is in place to physically check each FP10MDA prescription (for accuracy, clarity and meeting legal requirements) that have arrived in the pharmacy in a timely manner prior to the start date of the prescriptions. (This will allow the pharmacy and prescription services adequate time to resolve any issues and sort out a replacement prescription if necessary). 3.4 The FP10MDA prescriptions are stored/filed in a safe, secure and organised manner that will minimise any risk of the pharmacy dispensing the wrong prescription, dispensing a prescription prematurely or dispensing a void, invalid or duplicate prescription 3.5 Any FP10MDA prescriptions that are invalid are physically separated from current and valid FP10MDA prescriptions 3.6 FP10MDA prescriptions that are invalid are destroyed immediately and details of the prescription and its destruction recorded to enable a clear audit trail. 4 Preparation and Dispensing of Methadone / Subutex 4.1 A system is in place to ensure that quantities dispensed are double-checked. Wherever possible, all quantities are checked by a second person. 4.2 All pharmacy staff are aware that Methadone oral solution and Subutex come in various strengths and exercises caution when dispensing 4.3 All pharmacy staff are aware that the pharmacy cannot substitute different presentations of Methadone formulation for the other and must dispense exactly what the prescription specifies (e.g. sugar free and non sugar free formulations) 4.4 Where a pharmacy has patients on different strengths and/or formulation of Methadone, additional steps are taken in the pharmacy to prevent confusion and to minimise risks of the wrong strength/formulation being used (e.g. Prescriptions that requests for sugar free formulation are highlighted with a highlighter pen, notes and reminders written on the patient computer records and prescription to remind dispensers and pharmacists that the particular patient/s are on sugar free formulation, the stock bottles of sugar free Methadone are located on a different shelve to normal Methadone and have an additional label attached to it highlighting that it is a sugar free formulation) 4.5 If the pharmacy prepares Methadone extemporaneously, it does so by following the RPSGB requirements. There is a separate SOP for the preparation of extemporaneous Methadone and the pharmacy meets the risk management criteria for this as for SOP (refer to no. 1.1 - 1.5) 4.6 Methadone/Subutex is dispensed from the prescription and not from computer records 4.7 Dispensed Methadone/Subutex awaiting collection and supervision should be stored away in the CD cabinet and not left on the dispensing bench 4.8 Dispensed Methadone/Subutex that are awaiting collection and stored in the CD cabinet are stored in a safe, secure and organised manner to minimise any errors in picking 4.9 The pharmacist verifies the identity of each client each time they present to the pharmacy to collect their dose (e.g. date of birth and/or address checked on each occasion) 4.10 The pharmacist has additional safeguards in place to ensure that the correct dose is presented to the correct client (e.g. performing a final check of the dispensed bottle against the prescription and showing the dispensed bottle to the client prior to supervising their consumption) 5 Communication and Liaison 5.1 The pharmacy has systems and procedures in place to ensure that communication and liaison with the key workers and drug services are effective, improves patient care and delivery of service, maintains patient safety and provides a clear auditable trail. (i.e. communication to and from key workers and drug services should be logged in an organised and auditable manner. Some pharmacies have folders for their clients and each client will have their dedicated section in the folder where notes and communication can be kept and logged) 5.2 The pharmacy has systems and procedures in place to ensure that communication and liaison within the pharmacy are effective, improves patient care and delivery of service, maintains patient safety and provides a clear auditable trail. (this is particularly important where there are staff working in different shifts, part time staff, multiple pharmacists and locum pharmacists) 6 Dispensing errors, significant events and near misses 6.1 The pharmacy records near misses 6.2 The pharmacy analyses near misses periodically and learns from them 6.3 The pharmacy records significant events (including dispensing errors) 6.4 The pharmacy undertakes significant event analysis and learns from them 6.5 The pharmacy has an incident reporting system in place (head office, NPSA) including reporting Controlled Drugs issues to the PCT CD Accountable Officer. 7 RPSGB Controlled Drugs Inspection 7.1 The pharmacy takes into account the RPSGB CD Inspection report and resolves the issues highlighted in the report in a timely manner 8 Education and Training 8.1 There is adequate opportunity for pharmacy staff involved in the service to train in substance misuse and in the delivery and operation of the service 8.2 Pharmacy staff involved in service are adequately trained in substance misuse and in the delivery and operation of the Supervised Consumption Service, 9 Local correspondence, guidance, paperwork relating to the service 9.1 The pharmacy is fully aware of the terms of the service as detailed in the Service Level Agreement 9.2 The pharmacy has a system in place to communicate to all staff any local correspondence and guidance issued by the PCT or Drug Services 9.3 The pharmacy has a system in place to communicate PCT patient safety updates (relevant to the service) to all staff and learn from patient safety incidents shared by the PCT 10 Capacity issues 10.1 The pharmacy has adequate CD cabinet storage, which allows for storage of dispensed product and stock of Methadone/Subutex and other pharmacy Controlled Drugs including patient returns. There are no issues with CD cabinet storage capacity that will pose a risk to patient and pharmacy safety. 10.2 The pharmacy has adequate staffing levels (to allow for peaks and demands of the service and other pharmacy services) in order to maintain the safe and effective delivery of the service. Supervision of consumption is not rushed or compromised and is appropriate to the dose prescribed. 10.3 The pharmacy is able to manage well with the number of clients in the Supervised Consumption Scheme. The client numbers do not compromise the safe and effective delivery of the service and of other pharmacy services Other Risk Assessment areas locally identified by pharmacy
An example of a completed Action plan
Ref. Risk Assessment Area Proposed Actions to be taken by Timescale Lead Comments on completion and date identified as needing pharmacy completed improvement 3.2 A system is in place to check 1) Nominate LH to be in charge of checking that 1 month DH Completed- 23 Jan 08 . LH nominated and SS nominated as whether prescriptions have appropriate prescriptions arrive in time. Nominate (31 Jan 08) deputy arrived in time and to chase up SS to deputise in LH’s absence the Drug prescription services 2) System of checking arrival of FP10MDA DH,LH System in place- 23 Jan 08. Summary of system written down and where FP10MDA prescriptions prescriptions to be developed with LH and SS and and kept at the front of FP10MDA prescription folder have not arrived in time written procedure to be kept with prescription folder SS
3.3 A system is in place to physically 1) Nominate LH to be in charge of this. Nominate 1 month DH Completed– 23 Jan 08. LH nominated and SS nominated as check each FP10MDA SS to deputise in LH’s absence (31 Jan 08) deputy prescription (for accuracy, clarity 2) System of checking each FP10MDA DH,LH System in place– 23 Jan 08. Procedure written down and kept at and meeting legal requirements) prescriptions to be developed with LH and SS and and the front of FP10MDA prescription folder that have arrived in the pharmacy written procedure to be kept with prescription folder SS in a timely manner prior to the start date of the prescriptions. 2.2 The pharmacy is aware of who 1) Call PCT and find out who PCT CD Accountable 1 week DH Completed – 4 Jan 08. Name and contact details of AO obtained the PCT CD Accountable Officer Officer is (7 Jan 08) and written down in SOP is and of their contact details 2) Write down name and contact details of DH Accountable Officer and put together with SOP for Supervised Consumption Scheme 5.1 The pharmacy has systems and 1) Develop a template log/communication sheet and 2 months DH Completed -19 Feb 08. Template sheet produced. All staff briefed procedures in place to ensure place in prescription folder in the front of each (29 Feb 08) on how to use sheets. Communication to and from key workers and that communication and liaison prescription in their relevant pouches. drug services are now recorded using the sheets. Sheets are kept with the key workers and drug 2) Brief all staff on the how to use the DH with the prescription in the relevant pouches. services are effective, improves log/communication sheets patient care and delivery of 3) All log/communication to and from key workers All service, maintains patient safety and drug services to be written down in and provides a clear auditable chronological order trail. Action Plan to improve on weak areas identified in the risk assessment tool
Ref. Risk Assessment Area Proposed Actions to be taken by Timescale Lead Comments on completion and date identified as needing pharmacy completed improvement