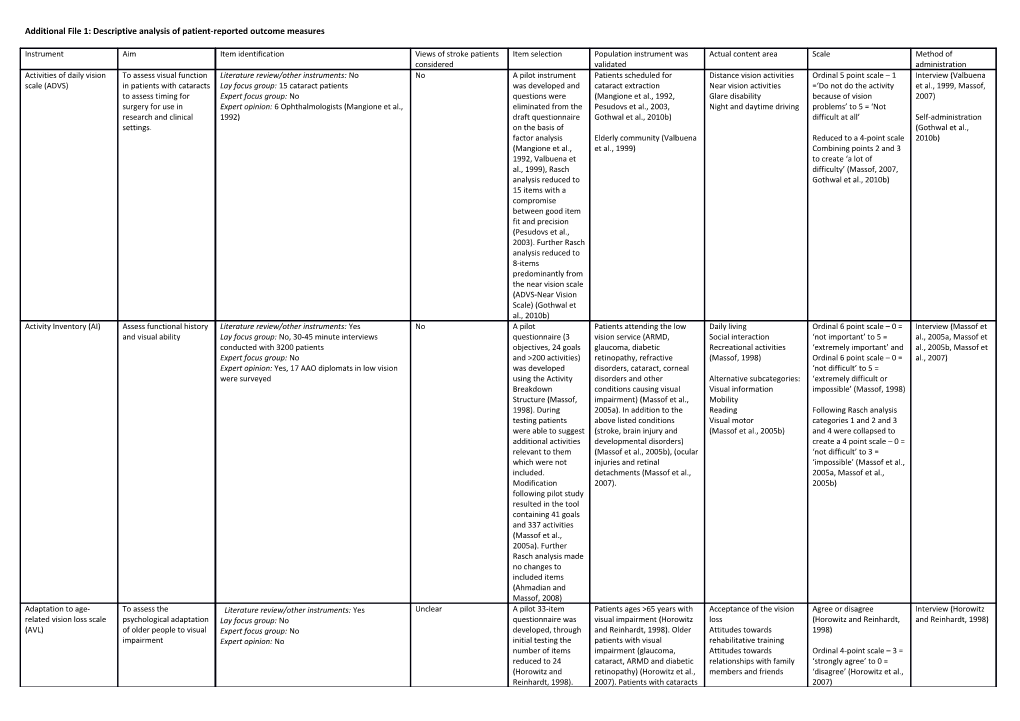
Additional File 1: Descriptive analysis of patient-reported outcome measures
Instrument Aim Item identification Views of stroke patients Item selection Population instrument was Actual content area Scale Method of considered validated administration Activities of daily vision To assess visual function Literature review/other instruments: No No A pilot instrument Patients scheduled for Distance vision activities Ordinal 5 point scale – 1 Interview (Valbuena scale (ADVS) in patients with cataracts Lay focus group: 15 cataract patients was developed and cataract extraction Near vision activities =‘Do not do the activity et al., 1999, Massof, to assess timing for Expert focus group: No questions were (Mangione et al., 1992, Glare disability because of vision 2007) surgery for use in Expert opinion: 6 Ophthalmologists (Mangione et al., eliminated from the Pesudovs et al., 2003, Night and daytime driving problems’ to 5 = ‘Not research and clinical 1992) draft questionnaire Gothwal et al., 2010b) difficult at all’ Self-administration settings. on the basis of (Gothwal et al., factor analysis Elderly community (Valbuena Reduced to a 4-point scale 2010b) (Mangione et al., et al., 1999) Combining points 2 and 3 1992, Valbuena et to create ‘a lot of al., 1999), Rasch difficulty’ (Massof, 2007, analysis reduced to Gothwal et al., 2010b) 15 items with a compromise between good item fit and precision (Pesudovs et al., 2003). Further Rasch analysis reduced to 8-items predominantly from the near vision scale (ADVS-Near Vision Scale) (Gothwal et al., 2010b) Activity Inventory (AI) Assess functional history Literature review/other instruments: Yes No A pilot Patients attending the low Daily living Ordinal 6 point scale – 0 = Interview (Massof et and visual ability Lay focus group: No, 30-45 minute interviews questionnaire (3 vision service (ARMD, Social interaction ‘not important’ to 5 = al., 2005a, Massof et conducted with 3200 patients objectives, 24 goals glaucoma, diabetic Recreational activities ‘extremely important’ and al., 2005b, Massof et Expert focus group: No and >200 activities) retinopathy, refractive (Massof, 1998) Ordinal 6 point scale – 0 = al., 2007) Expert opinion: Yes, 17 AAO diplomats in low vision was developed disorders, cataract, corneal ‘not difficult’ to 5 = were surveyed using the Activity disorders and other Alternative subcategories: ‘extremely difficult or Breakdown conditions causing visual Visual information impossible’ (Massof, 1998) Structure (Massof, impairment) (Massof et al., Mobility 1998). During 2005a). In addition to the Reading Following Rasch analysis testing patients above listed conditions Visual motor categories 1 and 2 and 3 were able to suggest (stroke, brain injury and (Massof et al., 2005b) and 4 were collapsed to additional activities developmental disorders) create a 4 point scale – 0 = relevant to them (Massof et al., 2005b), (ocular ‘not difficult’ to 3 = which were not injuries and retinal ‘impossible’ (Massof et al., included. detachments (Massof et al., 2005a, Massof et al., Modification 2007). 2005b) following pilot study resulted in the tool containing 41 goals and 337 activities (Massof et al., 2005a). Further Rasch analysis made no changes to included items (Ahmadian and Massof, 2008) Adaptation to age- To assess the Literature review/other instruments: Yes Unclear A pilot 33-item Patients ages >65 years with Acceptance of the vision Agree or disagree Interview (Horowitz related vision loss scale psychological adaptation Lay focus group: No questionnaire was visual impairment (Horowitz loss (Horowitz and Reinhardt, and Reinhardt, 1998) (AVL) of older people to visual Expert focus group: No developed, through and Reinhardt, 1998). Older Attitudes towards 1998) impairment Expert opinion: No initial testing the patients with visual rehabilitative training number of items impairment (glaucoma, Attitudes towards Ordinal 4-point scale – 3 = reduced to 24 cataract, ARMD and diabetic relationships with family ‘strongly agree’ to 0 = (Horowitz and retinopathy) (Horowitz et al., members and friends ‘disagree’ (Horowitz et al., Reinhardt, 1998). 2007). Patients with cataracts 2007) The number of (Gothwal et al., 2009a) items was reduced again to develop a short-form of the questionnaire. The decisions to remove 10 items were based on skewness, interviewer feedback, missing data and low correlations. A further 2 items were removed through factor analysis resulting in the AVL- 12 (Horowitz et al., 2007). Rasch analysis was performed on the original AVL-24, in order to achieve unidimensionality 5 items were deleted and a further 3 misfitting items were removed (Gothwal et al., 2009a). Adult Strabismus Quality Evaluate health related Literature review/other instruments: No Unclear The draft Patients with childhood and Psychosocial Ordinal 5-point scale – 100 Self-administration of Life questionnaire (AS- quality of life in adults Lay focus group: No – 30 individual interview with questionnaire acquired strabismus (Hatt et Function = ‘never’ to 0 = ‘always’ (Hatt et al., 2009, 20) with strabismus patients developed al., 2009). plus a ‘not applicable’ Leske et al., 2012) Expert focus group: No contained 181 items Subscales were divided option Expert opinion: No from unique following Rasch analysis: statements from the Self-perception Rasch analysis indicated to patient interviews. Interactions collapse never and rarely This was reduced to Reading function in the function subscale 20 items using General function (Leske et al., 2012) factor analysis (Hatt (Leske et al., 2012) et al., 2009). Rasch analysis reduced the questionnaire by two items (hobbies and depth perception) to 18 items (Leske et al., 2012) Amblyopia and Evaluate health related Literature review/other instruments: Existing No A pilot Patients with strabismus with Fear of losing the better Ordinal 5-point scale – 1 = Self-administration strabismus questionnaire quality of life in patients questionnaires questionnaire was or without amblyopia (van de eye ‘None of the time’ to 5 = (Felius et al., 2007, (ASQE) with amblyopia and Lay focus group: Yes developed using Graaf et al., 2004, Felius et al., Distance estimation ‘All of the time’ (van de Vianya-Estopa et al., strabismus Expert focus group: No themes from the 2007, Vianya-Estopa et al., Visual disorientation Graaf et al., 2004) 2010) Expert opinion: No patient focus group 2010) Double vision (van de Graaf et al., Social contact and Rasch analysis suggested 2004). Translation of appearance the collapse of categories Dutch version (26 4 (some of the time) and 5 items) to English (all of the time) (Vianya- (Felius et al., 2007). Estopa et al., 2010) Rasch analysis highlighted problems with testing non- strabismic amblyopes, a reduction of 3 items was required to improve fit (Vianya- Estopa et al., 2010) Catquest Assess benefits of Literature review/other instruments: Yes No The questionnaire Patients awaiting cataract Frequency of performing Ordinal 5-point scale – 1 = Interview (Lundstrom cataract surgery Lay focus group: No, 139 patients were interviewed started with 37 surgery (Lundstrom et al., activities ‘No difficulty’ to 5 = et al., 1997) Expert focus group: No items, this was 1997, Lundstrom and Perceived difficulty in ‘Cannot perform the Expert opinion: No reduced using Pesudovs, 2009) performing activities activity because of bad results from patient Difficulties in general and vision’ plus a ‘cannot say’ interviews to 6 satisfaction with vision option (Lundstrom et al., activities which Cataract symptoms 1997) were deemed to be important plus a Following Rasch analysis, question about the categories 3 and 4 in the persons preferred frequency scale were activity, creating an collapsed (Lundstrom and 18 item Pesudovs, 2009). questionnaire. (Lundstrom et al., 1994). Rasch analysis suggested the removal of frequency and symptom items. The remaining disability and global items were combined to create a 9-item short form measure (Catquest-9SF) (Lundstrom and Pesudovs, 2009). Another Rasch analysis agreed with the removal of the frequency items, however, also kept two symptom items and one driving item – creating a 12 item questionnaire (Gothwal et al., 2009b). Daily living tasks Evaluate an individual’s Literature review/other instruments: No No A pilot question was Patients with ARMD or The domains are not Ordinal 4-point scale – 1 = Interview (Hart et al., dependent on vision visual status Lay focus group: Yes – list activities which cause developed using the awaiting cataract surgery with named (Hart et al., 2005) ‘Cannot see to do’ to 4 = 2005) (DLTV) difficulties activities suggested a control group from an ‘No difficulty’ (Hart et al., Self-administration Expert focus group: No by patients and elderly population (Hart et al., 1999) (Schmier et al., 2006) Expert opinion: Yes – asked for comment on patients health care 1999). Patients with ARMD lists professionals, it (Hart et al., 2005, Schmier et Rasch adjusted 4-point consisted of 22 al., 2006). scale was found to be items plus 2 overall Patients with visual optimal (Denny et al., visual function impairment following stroke 2007) rating scales (Hart et (Rowe et al., 2013) al., 1999). Item response theory analysis found two redundant items (reading correspondence and identifying money), therefore these were removed (Hart et al., 2005). Rasch analysis was performed on the original 22 item questionnaire, resulted in the removal of 5 items (adjusting to dark, objects off to one side, seeing and using steps and pouring a drink) reducing the overall questionnaire to 17 items (Denny et al., 2007) Diplopia questionnaire To assess the frequency Literature review/other instruments: No Unclear A short Patients with acquired - Ordinal 3-point scale – Interview (Holmes et of diplopia Lay focus group: No questionnaire was diplopia (Holmes et al., 2005) ‘always’ to ‘never’, al., 2005) Expert focus group: No developed with 8 weighted scores to Expert opinion: Yes items, one for each primary and reading position of gaze position (Holmes et al., (Holmes et al., 2005) 2005). The questionnaire ‘Rarely’ and ‘Often’ were was revised, which added creating a 5-point resulted in the scale (Holmes et al., 2013) removal of one item (Holmes et al., 2013) Glaucoma quality of life Assess the impact of Literature review/other instruments: Yes – existing No A pilot Patients with glaucoma Outdoor mobility and Ordinal 5 point scale – 1 = Self-administration -15 questionnaire common disabilities questionnaires for glaucoma and other visual questionnaire navigation ‘no difficulty’ to 5 = (Nelson et al., 1999) (GQL-15) suffered by patients with conditions underwent item Lighting and glare ‘severe difficulty’ plus a glaucoma Lay focus group: No reduction to 15 Activities demanding ‘not relevant’ option Combination of self- Expert focus group: No items using factor functional peripheral (Khadka et al., 2011). administration and Expert opinion: No analysis (Nelson et vision interview (Gothwal et al., 1999). Household tasks and al., 2012b) The GQL-15 was personal care assessed using Interview (Wang et Rasch analysis. al., 2013) Items were removed to eliminate multidimensionality (reading newspaper, tripping, crossing the road, bumping into objects, recognising faces and adjusting to bright lights). The re-engineered instrument was named the Glaucoma Activity Limitation-9 (GAL-9) (Khadka et al., 2011). A second Rasch analysis of the GQL- 15 was completed and Items were reduced to 10 and renamed Glaucoma Activity Limitation- 10 (GAL-10) (Gothwal et al., 2012b). A more recent Rasch analysis found 2 misfit items, however, removal did not improve fit statistics and concluded the original GQL-15 is valid (Wang et al., 2013) Houston vision Aid the decision making Literature review/other instruments: No No A pilot Patients awaiting cataract Cooking Part A - Ordinal 5 point Self-administration assessment test (HVAT) process when Lay focus group: Yes questionnaire was surgery (Prager et al., 2000) Night driving scale – 0 = ‘not at all (Gothwal et al., considering cataract Expert focus group: No developed Day driving limited’ to 4 = ‘severely 2011b) surgery Expert opinion: No containing 11 items. Housework limited’ plus a ‘not For each item both Leisure activities relevant’ option. physical and visual Outdoor activities Part B - Ordinal 6 point impairment is Reading scale – 0 = ‘I have no visual estimated (Prager et Taking medication or other physical al., 2000). Watching television limitations’ to 5 = ‘all due Rasch analysis was Writing to eyesight’ (Prager et al., not conducted as 2000) the rating scale could not be fixed Rasch analysis of scales (Gothwal et al., Part B – reduced to a 4- 2011b) point scale 0 = ‘none due to eyesight’ to 3 = ‘all due to eyesight’, categories 2 and 3 were collapsed. Reanalysed indicated more adjustment to the scales were required but it could not be isolated which categories needed to be collapsed (Gothwal et al., 2011b) Impact of vision To assess the impact of Literature review/other instruments: Existing QoL No A draft People with visual Emotional reaction to Ordinal 6 point scale – 0 = Interview (Keeffe et impairment (IVI) vision impairment on a questionnaires, VF-14, NEI-VFQ, VQOL and VCM1. questionnaire (76 impairment including ARMD, vision loss Not at all to 5 = all the al., 1999, Weih et al., visually impaired Lay focus group: 53 patients with visual impairment items) based on a retinopathies, glaucoma, Household care time (14 items) 2002, Lamoureux et patient’s ability to (diabetic retinopathy, glaucoma, ARMD, cataracts, combination of the other conditions and cataract Personal care Ordinal 7 point scale – 0 = al., 2007a, participate in daily life retinitis pigmentosa and congenital visual VQOL and VCM1, (Keeffe et al., 1999, Weih et Leisure and work Not at all to 5 = Can’t do Lamoureux et al., activities impairments) excluding items on al., 2002, Lamoureux et al., Mobility this because of eyesight 2007b) Expert focus group: No ocular symptoms 2006, Lamoureux et al., Social and consumer plus 8 = Don’t do this for Expert opinion: No and disability, with 2007a, Lamoureux et al., interactions other reasons (19 items). Combination of (Keeffe et al., 1998) the addition of focus 2007b, Lamoureux et al., (Hassell et al., 2000) interview and self- group suggestions. A 2008b) Emotional well being administration reduction in items Patients awaiting cataract Reading and accessing Rasch 4 point scale – 0 = (Lamoureux et al., to 45 due to high surgery (Pesudovs et al., information low participation to 3 = 2006, Lamoureux et correlation (Keeffe 2008) Mobility and high participation (26 al., 2007c, Pesudovs et al., 1999). A independence items) et al., 2008) further 13 items (Lamoureux et al., 2007c) Rasch 3 point scale – 0 = were excluded due low participation to 2 = to redundancy high participation (2 items (items in emotional – reading ordinary sized domain) and floor print and getting needed and ceiling effects information) (Lamoureux (eating and driving); et al., 2006) factor analysis was unable to highlight items for exclusion (Hassell et al., 2000). The items were reduced further by Rasch analysis to 28 due to irrelevance (work and sporting events) and ceiling effects (hobbies and reading street signs) (Lamoureux et al., 2006). Further Rasch analysis suggested the removal of ‘worry about your eyesight getting worse’ due to misfit (Pesudovs et al., 2008) Indian visual function To develop a patient Literature review/other instruments: No No The initial pilot Patients with cataract, Visual symptoms Ordinal 5 point scale – 1 = Interview (Gupta et questionnaire defined vision function Lay focus group: 10 patients per group, 40 specific to questionnaire (103 glaucoma, diabetic Psychosocial impact ‘not at all’ to 4 = ‘a lot’ al., 2005, Gothwal et (IND-VFQ) questionnaire in a diagnosis (cataracts, glaucoma, ARMD, diabetic items) was tested retinopathy, ARMD and no General functioning plus x = ‘unable to carry al., 2012a) population of visually retinopathy) and 6 mixed groups. with the aim of item visual condition (Gupta et al., (Gupta et al., 2005) out because of vision impaired and blind Expert focus group: No reduction. Pre- 2005) impairment’ (Gupta et al., people living in a low Expert opinion: No (Murthy et al., 2005) designed exclusion Rasch analysis altered 2005) income country criteria for items – subscales: not relevant >10% Mobility Rasch scale 4 point scale – of patients (18 items Activity limitation or visual 1 = ‘not at all’ to 3 = ‘a lot’ excluded) and no functioning plus x = ‘unable to carry difficulty reported Visual symptoms out because of vision by >30% of patients Psychosocial impact impairment’ (Finger et al., (40 items excluded). (Finger et al., 2011, 2011). Resulting in a 45 Gothwal et al., 2012a) item questionnaire. Rasch analysis approved Further item original rating scale reduction using (Gothwal et al., 2012a) missing data, redundancy and item convergent/discrimi nant validity producing the 33 item questionnaire (Gupta et al., 2005). Rasch analysis resulted in a further 5 item reduction (Finger et al., 2011). Another Rasch analysis excluded one item from the visual functioning scale or activity limitation subscale (Gothwal et al., 2012a) Low vision quality of life To assess the quality of Literature review/other instruments: Yes – existing No A pilot Patients with low vision General vision Ordinal 6-point scale – 5 = RCT comparison of questionnaire (LVQoL) life in patient with low questionnaires assessed questionnaire was diagnosed with a variety of Mobility ‘no difficulty’ to 0 = ‘could postal, telephone or vision and allow Lay focus group: No but opinion of patients with low developed using conditions Lighting issues no longer performed interview (Wolffsohn evaluation of vision sort with MDT. questions from Psychological adjustment because of vision’ plus a et al., 2000). rehabilitation strategies Expert focus group: No existing Reading and fine work ‘no longer perform Self-administration Expert opinion: MDT (ophthalmologists, questionnaires Activities of daily living because of vision’ and a (de Boer et al., 2006) optometrists, orthoptists, occupational therapists, found in literature ‘not relevant’ option welfare officiers, audiologists and patients with low review resulting in (Wolffsohn and Cochrane, vision). 74 items. Pre- 2000) (Wolffsohn and Cochrane, 2000) designed exclusion criteria for items – not relevant >33% of patients, little or great difficulty by >65% of patients and reliability of items <0.60 – resulted in a reduction to 25 items (Wolffsohn and Cochrane, 2000) Melbourne low vision Assess ability to perform Literature review/other instruments: Yes Unclear A pilot tool was Adults with ocular disease Ordinal 5-point scale – 0 = Clinical assessment ADL index (MLVAI) activities of daily living Lay focus group: No developed which and stable visual impairment ‘very unsatisfactory’ to 4 = (Haymes et al., Expert focus group: No consisted of nine (Haymes et al., 2001a). ‘very satisfactory’ (Haymes 2001b, Haymes et al., Expert opinion: No self-reported items Patients with ARMD (Haymes et al., 2001a) 2001c) and 18 observed et al., 2001b). items. Factor analysis resulted in two items (shirt buttoning, naming colours) being eliminated. Rasch analysis was also performed which highlighted redundant items, however, further item reduction did not occur at this stage due to a small sample size (Haymes et al., 2001a). A weighted version of the tool was created to produce personal impact estimates by completing a personal importance scale(Haymes et al., 2001c) Mobility questionnaire To assess subjective Literature review/other instruments: Critical review – No Forty seven items Patients with retinitis Mobility 5-point scale – 1 = ‘no Self-administered reporting of mobility no details published were chosen and pigmentosa (Turano et al., Mobility related behaviour difficulty’ to 5 = ‘extreme (Turano et al., 1999) function in patient with Lay focus group: No split into two parts. 1999) and open-angle difficulty’ plus ‘not Interview (Turano et retinitis pigmentosa Expert focus group: No Validity glaucoma (Turano et al., applicable’ (Turano et al., al., 2002) Expert opinion: One experience mobility instructor demonstrated by 2002) 1999) Rasch analysis, no resulting item reduction (Turano et al., 1999)
National Eye Institute To assess vision-targeted Literature review/other instruments: Yes No A pilot Patients requiring refractive Clarity of vision Sixteen options of Self-administered Refractive Error health-related quality of Lay focus group: Yes, 52 groups with a mean of 8 questionnaire (94 correction and emmetropes Expectations response scale depending (Hays et al., 2003, Correction quality of life life for persons with well patients per group items) created using (Hays et al., 2003). Near vision on item, varying between McAlinden et al., Questionnaire corrected refractive Expert focus group: No focus groups were Patients awaiting refractive Far vision dichotomous and 6-point 2011a) (NEI RQL) error Expert opinion: No reduced during surgery (McAlinden et al., Diurnal fluctuations ordinal scale (Hays et al., testing to a 42-item 2011a) Activity limitations 2003) questionnaire (Hays Glare et al., 2003). Rasch Symptoms Rasch analysis highlighted analysis highlighted Dependence on the need to remove 13 misfitting items corrections categories 2 and 3 in the and suggested the Worry 6-point scales to create a removal of these Suboptimal correction 4-point scale (McAlinden items (McAlinden et Appearance et al., 2011a) al., 2011a) (Hays et al., 2003) National Eye Institute To assess the impact of Literature review/other instruments: Existing NEI-VFQ: Unclear Focus group analysis Multi-condition population General health Ordinal 5-point scale – 1 = Interview (Mangione Visual Functioning visual impairment on questionnaires resulted in the 51- (cataracts, ARMD, diabetic General vision ‘all of the time’ to 5 = et al., 1998b, Questionnaire health related quality of Lay focus group: 246 eye clinic patients with various Neuro-10: Yes item pilot version of retinopathy, glaucoma and Near visual activities ‘none of the time’ or 1 = Mangione et al., (NEI VFQ) life across various eye ophthalmic diagnoses the NEI-VFQ low vision) (Mangione et al., Distance visual activities ‘no difficulty at all’ to 5 = 2001, Globe et al., conditions Expert focus group: No (Mangione et al., 1998b, Mangione et al., 2001, Ocular pain ‘stopped doing because of 2003, Marella et al., and Expert opinion: No 1998a). Clemons et al., 2003). Vision specific social your eyesight’ plus a 2010, Lloyd et al., The pilot version Optic neuritis (Cole et al., function ‘stopped doing for other 2013) Long form visual underwent item 2000). Vision specific role reasons or not interested functioning scale (LFVFS- reduction by Multi-condition and visually difficulties in doing this option’ Self-administered 39) qualitative criteria normal population (Globe et Vision specific mental (Cole et al., 2000, and linear al., 2003). health Rasch analysis Raphael et al., 2006, regression to Multiple sclerosis and other Vision specific dependency recommended the Ryan et al., 2008, resulting in 25-items neuro-ophthalmic disorders Driving collapse of categories 1 Pesudovs et al., (Mangione et al., with Neuro-10 supplement Colour vision and 2 to create a 4-point 2010a) 1998b). (Raphael et al., 2006). Peripheral vision scale (Massof, 2007) A 10-item Neuro- Patients with cataracts Ophthalmic (Pesudovs et al., 2010a). Reduced to four subscales Rasch analysis suggested Supplement (Neuro- Age-related macular using Rasch analysis: collapsing options: no 10) to the NEI-VFQ degeneration (Orr et al., General health difficulty = 0 and a little 25 was developed 2011) . Uveitis (Naik et al., Near activities difficulty = 1 (Ryan et al., using survey and 2013) Distance activities 2008) focus group Role difficulties methods. A decision (Pesudovs et al., 2010a) Rasch analysis suggested to delay item collapsing middle options reduction (possibly An alternative subscale to create a dichotomous – ‘eye/eyelid structure was suggested: scale: 1 = always and 2 = appearance is Visual functioning never , 1 = true and 2 = unusual’ and Socioemotional false plus the not sure ‘ptosis’) until further (Marella et al., 2010) option (Marella et al., testing has taken 2010) place (Ma et al., 2002, Raphael et al., 2006). Ceiling effects were found in three subscales: general vision, ocular pain and vision-specific mental health. Rasch analysis was performed on a 7- item version of the questionnaire created by author’s choice (Ryan et al., 2008). The NEI VFQ was re- engineered using Rasch analysis and renamed Long-Form Visual Functioning Scale (LFVFS) with the number items being reduced to 8 and Short-Form Visual Functioning Scale (SFVFS) with 6 items (Pesudovs et al., 2010a). Rasch analysis of the 25 item version suggested item reduction resulting in a 19-item version (Marella et al., 2010). Rasch analysis has also been used to create a 6-item utility index (Kowalski et al., 2012) Nursing home vision Evaluate vision-targeted Literature review/other instruments: Yes Unclear A pilot Residents of nursing homes Reading 5-point scale – ‘no Interview (Dreer et targeted health related health-related quality of Lay focus group: No Structured interviews questionnaire with (Dreer et al., 2007, Ocular symptoms difficulty at all’ to ‘stopped al., 2007, Lamoureux quality of life life in older adults who Expert focus group: No 57 items was Lamoureux et al., 2009a) General vision doing this because of your et al., 2009a, Elliott questionnaire (NHVQoL) live in nursing homes Expert opinion: No developed using ADLs eyesight’ or ‘none of the et al., 2010) themes which Mobility time’ to ‘all of the time’ or emerged from Social activities/hobbies ‘definitely true’ to interviews (Dreer et Psychological distress ‘definitely false’ plus many al., 2007). Adaptation/coping items had additional An adapted version Social interaction options of ‘not sure’, of the questionnaire ‘stopped doing this for was created to During Rasch analysis the other reasons or not produce personal adaptation/coping interested in doing this’ impact by the subscale was added to and ‘could do this but not addition of bother psychological distress given the opportunity’ subscales as a part B (Lamoureux et al., 2009a) (Dreer et al., 2007) to the original version (Elliott et al., 2010) QoL and visual function To evaluate self-reported Literature review/other instruments: Yes No A pilot Patients with cataract, Overall self-assessment of 3-point scale – 1 = ‘not at Interview (Carta et questionnaire visual satisfaction Lay focus group: No questionnaire was glaucoma, ARMD, branch visual satisfaction all’ to 3 = ‘very much’ al., 1998) (QoL-VFQ) Expert focus group: No developed retinal vein occlusion, minor Self-assessment of visual (Carta et al., 1998) Expert opinion: No consisting of 17 refractive error or presbyopia field Self-administration questions selected (Carta et al., 1998) Self-assessment of Rasch analysis confirmed (Gothwal et al., by consensus of the Patients awaiting cataract distance visual acuity optimal use of the scale 2009c) authors (Carta et al., surgery (Gothwal et al., Self-assessment of near (Gothwal et al., 2009c) 1998). Rasch 2009c) visual acuity analysis required Self-assessment of sensory the reduction of two adaptation items (lights of Self-assessment of colour oncoming cars and vision recognising colour) resulting in a 15- Rasch analysis revealed item questionnaire poor performance of the (Gothwal et al., subscales and 2009c) recommended addition of items to subscales or that the subscales not be used (Gothwal et al., 2009c) Quality of vision (QoV) Evaluate quality of vision Literature review/other instruments: Yes No A 23 items Patients with or without Frequency 4-point scale Self-administration Lay focus group: Yes x3 (5 non-experts) plus 15 underwent refractive correction and Severity Frequency 0 = ‘Never’ to 3 (Piermarocchi et al., subject interviews discussion within a patients with cataracts Bothersomeness = ‘Very often’ 2011) Expert focus group: Yes x3 (5 experts) focus group for item (McAlinden et al., 2010). Severity 0 = ‘Not at all’ to Expert opinion: No redundancy, Patients awaiting refractive Further analysis of the 3 = ‘ Severe’ representation and surgery (McAlinden et al., subscales recommended Bothersomeness 0 = ‘Not face validity to 2011b) continuing using all three at all’ to 3 = ‘Very’ reduce items to (McAlinden et al., 2013) (McAlinden et al., 2010) create a 30-item questionnaire focused on 10 symptoms. The pilot questionnaire developed was tested using conventional statistics and Rasch analysis (McAlinden et al., 2010) Self-report assessment Measure the Literature review/other instruments: No No A group of experts Patients with homonymous Reading 5-point scale – 1 = ‘unable’ Interview (Mennem of functional visual performance of vision Lay focus group: No developed a list of hemianopia (Mennem et al., Writing to 5 = ‘independent’ plus a et al., 2012, Velozo et performance dependant ADLs in older Expert focus group: No common ADLs and a 2012). Money management ‘not applicable’ option al., 2013) (SRA-VFA) adults with low vision Expert opinion: Yes five-point rating Telephone usage scale. A separate Reading a timepiece Rasch analysis suggested panel of experts Personal care the need to collapse the reviewed the list Clothing care middle ratings (2, 3 and 4) and rating scale. The Meal Preparation to create: a 3-point scale – pilot questionnaire Leisure 1 = ‘unable: dependant on consisted of 39 Functional mobility other to perform task, items (Gilbert and would perform task if able’ Baker, 2011) Reading to 3 = ‘independent: Writing experiences no difficulty Communication performing task safely, Financial and health accurately and efficiently’ management (Velozo et al., 2013) Feeding Personal hygiene Dressing Clothing care Meal Preparation Shopping Functional mobility Community or social and leisure participation Severity of visual field To assess subjective Literature review/other instruments: No No The original Patients with glaucoma (Mills - Ordinal 3-point scale 1 = Interview (Mills and damage disability associated with Lay focus group: Yes - interviews question consisted and Drance, 1986, no, 2 = uncertain and 3 = Drance, 1986, visual field loss Expert focus group: No of 15 items Viswanathan et al., 1999) yes (Mills and Drance, Viswanathan et al., Expert opinion: Yes – physicians and visual field developed from 1986) 1999) technicians expert and patient input (Mills and Drance, 1986). The questionnaire was modified, rewording of questions and the removal of items resulted in a 10-item questionnaire (Viswanathan et al., 1999) Veterans affairs low To measure functional Literature review/other instruments: Yes – clinical No The second round of Patients with low vision Visual ability Identical response scales Interview (Stelmack vision visual functioning ability of low vision guidelines modified Delphi (ARMD, glaucoma, diabetic Mobility for all items: 5-point scale et al., 2004a, questionnaire patients and measure Lay focus group: No – structure interviews with analysis selected 48 retinopathy and other) Reading – 1 = ‘not difficult’ to 5 = Stelmack et al., (VA LV VFQ) patient-centred patients items for the pilot (Stelmack et al., 2004a, Visual motor ‘impossible’ 2004b, Szlyk et al., outcomes of low vision Expert focus group: No questionnaire Stelmack et al., 2004b, Szlyk Visual information 2004) rehabilitation Expert opinion: Yes – consensus panel (Stelmack et al., et al., 2004). Rasch analysis indicated recommendations 2004a). The Patient with macular disease the collapse of categories questionnaire was (Stelmack and Massof, 2007). 2 ‘slightly difficult’ and 3 tested using Rasch Patients with homonymous ‘moderately difficult’ analysis (Szlyk et al., hemianopia (George et al., resulting in a 4-point scale 2004). Some items 2011) (Stelmack et al., 2004b) were identified as poor fit during Rasch analysis, however, any item change was deferred (Stelmack et al., 2004b). A short form of the questionnaire was developed by reducing items based on Rasch analysis and clinical relevance, resulting in a 20 item questionnaire (Stelmack et al., 2006, Stelmack and Massof, 2007) Vision and quality of life Economic evaluation of Literature review/other instruments: Yes No An item bank of 33 Patients with visual Physical well-being Range of between 5 and 7- Self-administration index (VisQoL) eye care and Lay focus group: Yes – 3 groups with 8-9 patients was created from impairment (Misajon et al., Independence point scales, different for (Misajon et al., 2005) rehabilitation programs Expert focus group: No the results of the 2005) Social well-being each item (Misajon et al., Expert opinion: No focus groups. Item Emotional well-being 2005) reduction was Self-actualisation achieved through Planning and organisation factor analysis and item response theory. A pilot study was then conducted using this item bank. Factor analysis retained 13 items. The final version contained 6 items following iterative structural equation modelling (Misajon et al., 2005) Vision function and To assess improvement Literature review/other instruments: Yes No Two pilot Patients with cataract, Overall visual function Ordinal 4 point scale – 1 = Interview (Fletcher et quality of life in functioning following Lay focus group: No questionnaires VF glaucoma, iritis, ARMD or Visual perception ‘not at all’ to = ‘a lot’ al., 1997) questionnaires cataract surgery Expert focus group: No (13 items) and QOL corneal disease (Fletcher et Limitation in everyday (Fletcher et al., 1997). Self-administration (VF and QOL) Expert opinion: Yes – 3 ophthalmologists and 2 social (12 items) were al., 1997). activities and visual acuity (Gothwal et al., workers developed and Patients with cataracts Peripheral vision 2009d) tested (Fletcher et (Gothwal et al., 2009d) Sensory adaptation, light al., 1997) (Fletcher dark adaptation, visual et al., 1997). search, colour Rasch analysis found discrimination and glare the VF disability questionnaire to be Depth perception valid. However, Self-care despite removal of Mobility items the QOL Social questionnaire was Mental found to be limiting (Fletcher et al., 1997). precision and could Rasch analysis not be deemed valid recommended these (Gothwal et al., subscales not to be used 2009d) (Gothwal et al., 2009d) Vision related quality of To assess vision related Literature review/other instruments: Yes No Pre-testing finalised Patients with cataract, ARMD, Overall vision Ordinal 6 point scale – 0 = Self-administered (de life (VQoL) quality of life Lay focus group: No – semi structured interviews the ‘parent’ version Glaucoma, Aphakia, Visual symptoms ‘not at all’ to 5 = ‘can’t do Boer et al., 2006) or with 38 patients with of the Amblyopia, Corneal lesions, Self esteem because of eye-sight’ plus Vision-related quality of Expert focus group: No - 11 interviews with support questionnaire Diabetic retinopathy, Thyroid Emotion a ‘don’t do for other life core measure workers and professionals containing 139 eye disease, Retinal Safety reasons’ option (VCM1) Expert opinion: Consultation with 26 professionals items. The selection detachment, Iritis, Ocular General Ordinal 5 point scale – 0 = of items took a hypertension, Ocular trauma, Self-care ‘not at all’ to 5 = ‘all the modular approach ocular tumour, Optic Domestic time’ – the latter used by to enable to neuropathy, RP, Retinal Financial all VCM1 items (Frost et questionnaire to vascular occlusions and no Reading al., 1998) meet the pathology (Frost et al., 1998). Miscellaneous information requirements of Patients awaiting cataract Mobility Rasch analysis indicated different groups of surgery Social interaction the need to collapse patients. Ten items (Lamoureux et al., 2008c) Leisure categories 4 ‘very rarely’ were identified as and 5 ‘all the time’ core items and resulting in a 4-point scale named VCM1(Frost (Lamoureux et al., 2008c) et al., 1998). Rasch analysis did not change any included items of the VCM1 (Lamoureux et al., 2008c) Visual activity To assess individual’s Literature review/other instruments: No No The pilot Adults aged 17 to 89. Glare disability Ordinal 5 point scale – 1 = Self-administration questionnaire (VAQ) problems in performing Lay focus group: No questionnaire Drivers aged 55 and over. Light and dark adaptation ‘never’ to 5 = ‘always’ (Gothwal et al., visual activities typical of Expert focus group: No contained 100 items (Sloane et al., 1992) Acuity and spatial vision (Sloane et al., 1992) 2009e) everyday life Expert opinion: No spilt into 10 areas. Visual search Items were reduced Patients with cataract Visual processing speed Rasch analysis by removing those (Gothwal et al., 2009e) Depth perception recommended the that did not provide Colour discrimination collapse of categories 2 further information Peripheral vision and 3 resulting in a 4-point and items with scale (Massof, 2007) unclear wording. Reduced to in the 13-item Factor analysis version: resulted in Visual search reduction of items Visual processing speed to 33 (Sloane et al., Depth perception 1992). Peripheral vision Rasch analysis (Gothwal et al., 2009e) reduced the number of items to 13 due to multidimensionality. This reduction in items results in floor-effects (Gothwal et al., 2009e) Visual disability Assess subjective visual Literature review/other instruments: Yes No A pilot Patients with cataracts Mobility 4 point scale – 1 =’Not at Self-administration assessment (VDA) disability Lay focus group: No questionnaire of 37 (Pesudovs and Coster, 1998, Distance/Lighting/Reading all’ to 4 = ‘A lot’ (Pesudovs (Pesudovs et al., Expert focus group: No items was Pesudovs et al., 2010b) Near and related tasks and Coster, 1998) 2010b) Expert opinion: No developed. Item (Pesudovs and Coster, reduction was 1998) performed by eliminating In order to achieve redundant items, unidimensionality Rasch resulting in an 18 analysis suggested the item questionnaire segregation of the (Pesudovs and mobility subscale and Coster, 1998) activity limitation subscale (Pesudovs et al., 2010b)
Visual disability Aid with prioritising Literature review/other instruments: Yes No A pilot Patients with retinitis - Ordinal 5 point scale – 0 = Interview (Marella et questionnaire (VDQ) rehabilitation goals Lay focus group: Yes – 3 groups (8 participants per questionnaire (28 pigmentosa, macular ‘not important’ to 4 = al., 2009) group) items) was created. degeneration, diabetic ‘extremely important’ and Expert focus group: No The pilot testing retinopathy, glaucoma, optic ordinal 5 point scale – 0 = Expert opinion: Yes resulted in removal atrophy, refractive error, ‘not difficult’ to 4 = unnecessary items corneal disorders, ‘impossible’ and addition of new developmental disorders, items (Marella et al., albinism and other diseases Rasch analysis suggested 2009) the collapse of categories 1 and 2 resulting in a 4- point scale (Marella et al., 2009) Visual function index Evaluate the amount of Literature review/other instruments: No No Items were chosen Patients awaiting cataracts Direct visual limitations Dichotomous – ‘yes/no’ or Self-administration (VFI) improvement obtained Lay focus group: No from those used to surgery (Bernth-Petersen, Mobility limitations ‘sufficient/insufficient’ (Gothwal et al., by cataract surgery Expert focus group: No routinely interview 1985, Gothwal et al., 2010a) Social role limitations Only two items use an 2010a) Expert opinion: Yes cataract patients (Bernth-Petersen, 1985) ordinal 3-point scale. but with the aim of (Bernth-Petersen, 1985) standardisation an 11-item questionnaire was created (Bernth- Petersen, 1985). Rasch analysis found this questionnaire not valid for use in a modern cataract population in a developed country (Gothwal et al., 2010a)
Visual functioning 14 To measure functional Literature review/other instruments: Existing vision No A pilot instrument Patients awaiting cataract Seeing steps Ordinal 5 point scale – 0 Interview (Cassard et items (VF-14) impairment caused by related questionnaires was developed surgery (Steinberg et al., Writing cheques =’Unable to perform al., 1995, Lamoureux cataract Lay focus group: No – individual interviews with following the expert 1994) Playing table games activity’ to 4 = ‘No et al., 2008a, patients were conducted focus group. Factor Taking part in sports difficulty’ (Steinberg et al., Lamoureux et al., Expert focus group: 11 members of National Advisory analysis divided Patients with retinal disease Cooking 1994, Massof, 2007) 2009b) Panel of ophthalmologists and optometrists items into 4 factors (Linder et al., 1999) Reading small print Self-administration Expert opinion: Three ophthalmologists (Steinberg et al., Doing fine handwork Reduced to a 4-point scale (Gothwal et al., 1994). Various Population based study Reading a newspaper Combining points 2 and 3 2010c) shortened versions (Lamoureux et al., 2008a) Daytime driving (Lamoureux et al., 2009b) have been proposed Night-time driving (Uusitalo et al., Reading street signs 1999, Friedman et Reading large print al., 2002, Pager, Recognising people 2004, Moghimi et Watching television al., 2007). A reduction in items (large print, fine handwork, and taking part in sports) created the VF-11, this was examined using Rasch analysis (Lamoureux et al., 2008a). Further Rasch analysis reduced items (driving at night and driving in daytime) to the VF-9 with a change of scale (Lamoureux et al., 2009b). Additional revision (eliminating large print, recognising people, sports, cooking and driving) created the VF-8R using a Rasch scale (Gothwal et al., 2010c). Visual symptom and To assess the outcome Literature review/other instruments: Yes No A 32-item draft Patients awaiting cataract Visual symptoms/disability Ordinal 4 or 5 point scale – Self-administration quality of life following second-eye Lay focus group: No – individual interviews with 40 questionnaire was surgery or recently Vision-specific quality of 13 formats (Donovan et (Gothwal et al., questionnaire (VSQ) cataract surgery patients were conducted devised using the undergone cataract surgery life al., 2003) 2011a) Expert focus group: No data obtained from (Donovan et al., 2003, Expert opinion: Yes – 6 ophthalmologists, 6 clinical experts and Gothwal et al., 2011a) Rasch analysis indicated ophthalmic nurses, 4 optometrists, 1 social worker patients. Results the collapse of options 3 and 1 OT from pilot testing and 4 for the question ‘do resulted in some you have difficulty reorganisation and recognising people’s faces’ rewording of items, (Gothwal et al., 2011a) most commonly clarifying the question with ‘in the past month’ and ‘because of trouble with your eyesight’. Factor analysis resulted in the removal of four items (perception of colour, diplopia, blinkered vision and watering eyes). A short (14-item) and a long (26-item) final version were created (Donovan et al., 2003). Rasch analysis was performed on the 26-item version, due to lack of unidimensionality all items from the subscales visual symptoms and vision-specific quality of life were removed. Two further items were removed from the remaining subscale due to misfit, creating a 14-item questionnaire (Gothwal et al., 2011a) AHMADIAN, L. & MASSOF, R. 2008. Impact of general health status on validity of visual impairment measurement. Ophthalmic Epidemiology, 15, 345-55. BERNTH-PETERSEN, P. 1985. Visual functioning in cataract patients. Methods of measuring and results. Acta Ophthalmologica, 59, 198-205. CARTA, A., BRACCIO, L., BELPOLITI, L., SOLIANI, L., SARTORE, F., GANDOLFI, S. A. & MARAINI, G. 1998. Self-assessment of the quality of vision: association of questionnaire score with objective clinical tests. Current Eye Research, 17, 506-512. CASSARD, S. D., PATRICK, D. L., DAMIANO, A. M. & ET AL. 1995. Reproducibility and responsiveness of the vf-14: An index of functional impairment in patients with cataracts. Archives of Ophthalmology, 113, 1508-1513. CLEMONS, T. E., CHEW, E. Y., BRESSLER, S. B., MCBEE, W. & AGE-RELATED EYE DISEASE STUDY RESEARCH, G. 2003. National Eye Institute Visual Function Questionnaire in the Age-Related Eye Disease Study (AREDS): AREDS Report No. 10. Archives of Ophthalmology, 121, 211-7. COLE, S. R., BECK, R. W., MOKE, P. S., GAL, R. L. & LONG, D. T. 2000. The National Eye Institute Visual Function Questionnaire: experience of the ONTT. Optic Neuritis Treatment Trial. Investigative Ophthalmology & Visual Science, 41, 1017-21. DE BOER, M. R., TERWEE, C. B., DE VET, H. C., MOLL, A. C., VOLKER-DIEBEN, H. J. M. & VAN RENS, G. H. M. B. 2006. Evaluation of cross-sectional and longitudinal construct validity of two vision-related quality of life questionnaires: The LVQOL and VCM1. Quality of Life Research, 15, 233-248. DENNY, F., MARSHALL, A. H., STEVENSON, M. R., HART, P. M. & CHAKRAVARTHY, U. 2007. Rasch analysis of the daily living tasks dependent on vision (DLTV). Investigative Ophthalmology & Visual Science, 48, 1976-82. DONOVAN, J. L., BROOKES, S. T., LAIDLAW, D. A., HOPPER, C. D., SPARROW, J. M. & PETERS, T. J. 2003. The development and validation of a questionnaire to assess visual symptoms/dysfunction and impact on quality of life in cataract patients: the Visual Symptoms and Quality of life (VSQ) Questionnaire. Ophthalmic Epidemiology, 10, 49-65. DREER, L. E., MCGWIN, G., JR., SCILLEY, K., MEEK, G. C., DYER, A., SEKER, D. & OWSLEY, C. 2007. Development of a nursing home vision-targeted health-related quality of life questionnaire for older adults. Aging & Mental Health, 11, 722-33. ELLIOTT, A. F., DREER, L. E., MCGWIN, G., JR., SCILLEY, K. & OWSLEY, C. 2010. The personal burden of decreased vision-targeted health-related quality of life in nursing home residents. Journal of Aging & Health, 22, 504-521. FELIUS, J., BEAUCHAMP, G. R., STAGER, D. R., SR., VAN DE GRAAF, E. S. & SIMONSZ, H. J. 2007. The Amblyopia and Strabismus Questionnaire: English translation, validation, and subscales. American Journal of Ophthalmology, 143, 305-310. FINGER, R. P., KUPITZ, D. G., HOLZ, F. G., BALASUBRAMANIAM, B., RAMANI, R. V., LAMOUREUX, E. L. & FENWICK, E. 2011. The impact of the severity of vision loss on vision-related quality of life in India: an evaluation of the IND-VFQ-33. Investigative Ophthalmology & Visual Science, 52, 6081-8. FLETCHER, A. E., ELLWEIN, L. B., SELVARAJ, S., VIJAYKUMAR, V., RAHMATHULLAH, R. & THULASIRAJ, R. D. 1997. Measurements of vision function and quality of life in patients with cataracts in southern India. Report of instrument development. Archives of Ophthalmology, 115, 767-74. FRIEDMAN, D. S., TIELSCH, J. M., VITALE, S., BASS, E. B., SCHEIN, O. D. & STEINBERG, E. P. 2002. VF-14 item specific responses in patients undergoing first eye cataract surgery: can the length of the VF-14 be reduced? British Journal of Ophthalmology, 86, 885-891. FROST, N. A., SPARROW, J. M., DURANT, J. S., DONOVAN, J. L., PETERS, T. J. & BROOKES, S. T. 1998. Development of a questionnaire for measurement of vision-related quality of life. Ophthalmic Epidemiology, 5, 185-210. GEORGE, S., HAYES, A., CHEN, C. & CROTTY, M. 2011. Are vision-specific quality of life questionnaires important in assessing rehabilitation for patients with hemianopia post stroke? Topics in Stroke Rehabilitation, 18, 394-401. GILBERT, M. P. & BAKER, S. S. 2011. Evaluation and intervention for basic and instrumental activities of daily living. In: WARREN, M. (ed.) Occupational therapy interventions for adults with low vision. Bethesda, Maryland: AOTA Press. GLOBE, D., VARMA, R., AZEN, S. P., PAZ, S., YU, E., PRESTON-MARTIN, S. & LOS ANGELES LATINO EYE STUDY, G. 2003. Psychometric performance of the NEI VFQ-25 in visually normal Latinos: the Los Angeles Latino Eye Study. Investigative Ophthalmology & Visual Science, 44, 1470-8. GOTHWAL, V. K., BAGGA, D. K. & SUMALINI, R. 2012a. Rasch analysis of the Indian vision function questionnaire. British Journal of Ophthalmology, 96, 619-23. GOTHWAL, V. K., REDDY, S. P., BHARANI, S., BAGGA, D. K., SUMALINI, R., GARUDADRI, C. S., RAO, H. L., SENTHIL, S., PATHAK-RAY, V. & MANDAL, A. K. 2012b. Impact of glaucoma on visual functioning in Indians. Investigative Ophthalmology & Visual Science, 53, 6081-92. GOTHWAL, V. K., WRIGHT, B. D., LAMOUREUX, E. L. & PESUDOVS, K. 2009a. Validity of the adaptation to age-related vision loss scale in an Australian cataract population. Journal of Optometry, 2, 142-147. GOTHWAL, V. K., WRIGHT, T., LAMOUREUX, E. L. & PESUDOVS, K. 2010a. Psychometric properties of visual functioning index using Rasch analysis. Acta Opthalmologica, 88, 797-803. GOTHWAL, V. K., WRIGHT, T. A., LAMOUREUX, E. L., KHADKA, J., MCALINDEN, C. & PESUDOVS, K. 2011a. Improvements in visual ability with first-eye, second-eye, and bilateral cataract surgery measured with the visual symptoms and quality of life questionnaire. Journal of Cataract & Refractive Surgery, 37, 1208-16. GOTHWAL, V. K., WRIGHT, T. A., LAMOUREUX, E. L., LUNDSTROM, M. & PESUDOVS, K. 2009b. Catquest questionnaire: re-validation in an Australian cataract population. Clinical & Experimental Ophthalmology, 37, 785-94. GOTHWAL, V. K., WRIGHT, T. A., LAMOUREUX, E. L. & PESUDOVS, K. 2009c. Rasch analysis of the quality of life and vision function questionnaire. Optometry & Vision Science, 86, E836-44. GOTHWAL, V. K., WRIGHT, T. A., LAMOUREUX, E. L. & PESUDOVS, K. 2009d. Rasch analysis of visual function and quality of life questionnaires. Optometry & Vision Science, 86, 1160-8. GOTHWAL, V. K., WRIGHT, T. A., LAMOUREUX, E. L. & PESUDOVS, K. 2009e. Visual Activities Questionnaire: assessment of subscale validity for cataract surgery outcomes. Journal of Cataract & Refractive Surgery, 35, 1961-9. GOTHWAL, V. K., WRIGHT, T. A., LAMOUREUX, E. L. & PESUDOVS, K. 2010b. Activities of Daily Vision Scale: what do the subscales measure? Investigative Ophthalmology & Visual Science, 51, 694-700. GOTHWAL, V. K., WRIGHT, T. A., LAMOUREUX, E. L. & PESUDOVS, K. 2010c. Measuring outcomes of cataract surgery using the Visual Function Index-14. Journal of Cataract & Refractive Surgery, 36, 1181-8. GOTHWAL, V. K., WRIGHT, T. A., LAMOUREUX, E. L. & PESUDOVS, K. 2011b. Multiplicative rating scales do not enable measurement of vision-related quality of life. Clinical & Experimental Optometry, 94, 52-62. GUPTA, S. K., VISWANATH, K., THULASIRAJ, R. D., MURTHY, G. V., LAMPING, D. L., SMITH, S. C., DONOGHUE, M. & FLETCHER, A. E. 2005. The development of the Indian vision function questionnaire: field testing and psychometric evaluation. British Journal of Ophthalmology, 89, 621-7. HART, P. M., CHAKRAVARTHY, U., STEVENSON, M. R. & JAMISON, J. Q. 1999. A vision specific functional index for use in patients with age related macular degeneration. British Journal of Ophthalmology, 83. HART, P. M., STEVENSON, M. R., MONTGOMERY, A. M., MULDREW, K. A. & CHAKRAVARTHY, U. 2005. Further validation of the Daily Living Tasks Dependent on Vision: identification of domains. British Journal of Ophthalmology, 89, 1127-30. HASSELL, J. B., WEIH, L. M. & KEEFFE, J. E. 2000. A measure of handicap for low vision rehabilitation: the impact of vision impairment profile. Clinical & Experimental Ophthalmology, 28, 156-61. HATT, S. R., LESKE, D. A., BRADLEY, E. A., COLE, S. R. & HOLMES, J. M. 2009. Development of a quality-of-life questionnaire for adults with strabismus. Ophthalmology, 116, 139-144.e5. HAYMES, S. A., JOHNSTON, A. W. & HEYES, A. D. 2001a. The development of the Melbourne low-vision ADL index: a measure of vision disability. Investigative Ophthalmology & Visual Science, 42, 1215-25. HAYMES, S. A., JOHNSTON, A. W. & HEYES, A. D. 2001b. Preliminary investigation of the responsiveness of the Melbourne Low Vision ADL index to low-vision rehabilitation. Optometry & Vision Science, 78, 373-80. HAYMES, S. A., JOHNSTON, A. W. & HEYES, A. D. 2001c. A weighted version of the Melbourne Low-Vision ADL Index: a measure of disability impact. Optometry & Vision Science, 78, 565-79. HAYS, R. D., MANGIONE, C. M., ELLWEIN, L., LINDBLAD, A. S., SPRITZER, K. L. & MCDONNELL, P. J. 2003. Psychometric properties of the National Eye Institute-Refractive Error Quality of Life instrument. Ophthalmology, 110, 2292-301. HOLMES, J. M., LESKE, D. A. & KUPERSMITH, M. J. 2005. New methods for quantifying diplopia. Ophthalmology, 112, 2035-9. HOLMES, J. M., LIEBERMANN, L., HATT, S. R., SMITH, S. J. & LESKE, D. A. 2013. Quantifying diplopia with a questionnaire. Ophthalmology, 120, 1492-6. HOROWITZ, A. & REINHARDT, J. P. 1998. Development of the adaptation to age-realted vision loss scale. Journal of Visual Impairment and Blindness, 92, 30-41. HOROWITZ, A., REINHARDT, J. P. & RAYKOV, T. 2007. Development and validation of a short-form adaptation of the age-related vision loss scale: The AVL12. Journal of Visual Impairment and Blindness, 101, 146-159. KEEFFE, J. E., LAM, D., CHEUNG, A., DINH, T. & MCCARTY, C. A. 1998. Impact of vision impairment on functioning. Australian & New Zealand Journal of Ophthalmology, 26, S16-S18. KEEFFE, J. E., MCCARTY, C. A., HASSELL, J. B. & GILBERT, A. G. 1999. Description and measurement of handicap caused by vision impairment. Australian & New Zealand Journal of Ophthalmology, 27, 184-6. KHADKA, J., PESUDOVS, K., MCALINDEN, C., VOGEL, M., KERNT, M. & HIRNEISS, C. 2011. Reengineering the glaucoma quality of life-15 questionnaire with rasch analysis. Investigative Ophthalmology & Visual Science, 52, 6971-7. KOWALSKI, J. W., RENTZ, A. M., WALT, J. G., LLOYD, A., LEE, J., YOUNG, T. A., CHEN, W. H., BRESSLER, N. M., LEE, P., BRAZIER, J. E., HAYS, R. D. & REVICKI, D. A. 2012. Rasch analysis in the development of a simplified version of the National Eye Institute Visual-Function Questionnaire-25 for utility estimation. Quality of Life Research, 21, 323-34.