RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, KARNATAKA BANGALORE ANNEXURE – II PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
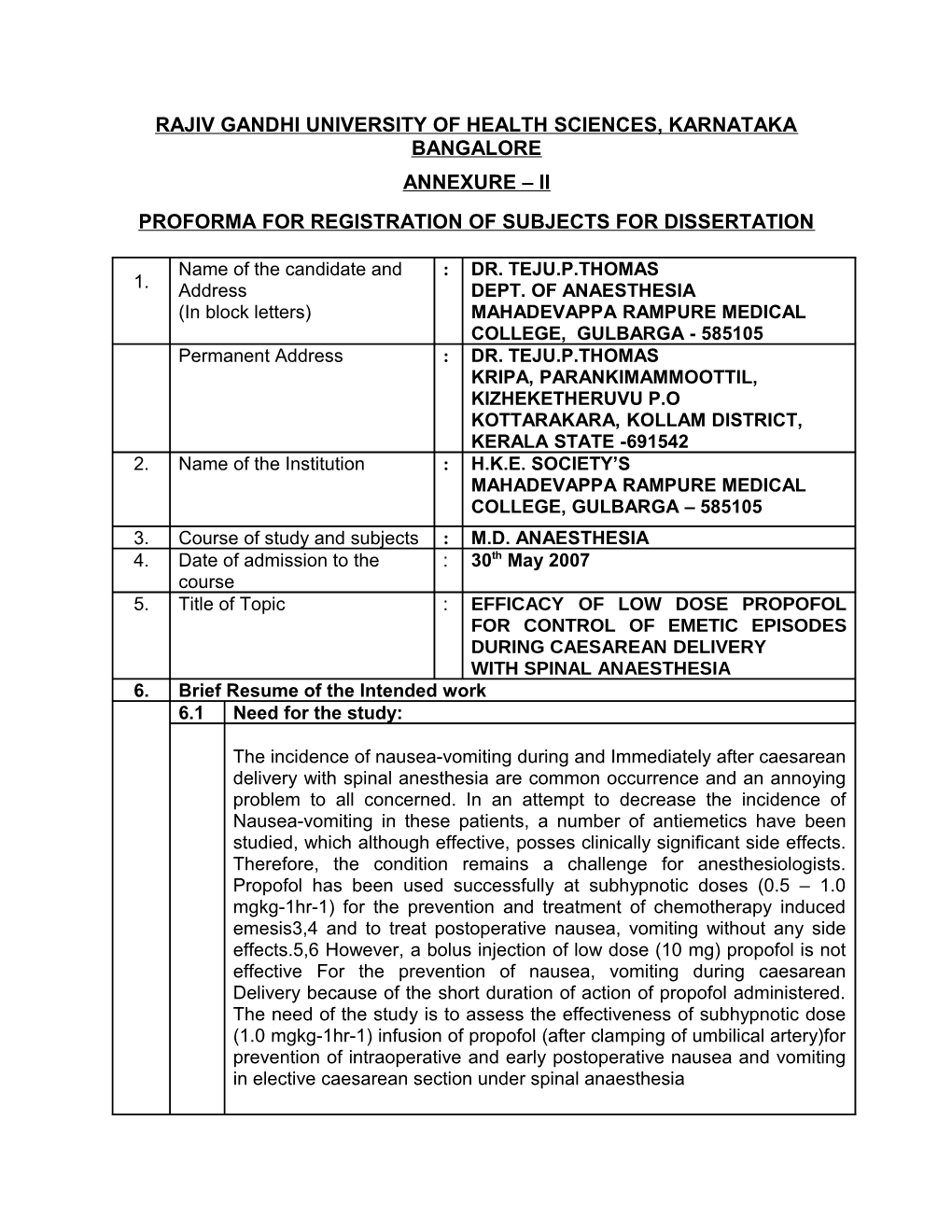
Name of the candidate and : DR. TEJU.P.THOMAS 1. Address DEPT. OF ANAESTHESIA (In block letters) MAHADEVAPPA RAMPURE MEDICAL COLLEGE, GULBARGA - 585105 Permanent Address : DR. TEJU.P.THOMAS KRIPA, PARANKIMAMMOOTTIL, KIZHEKETHERUVU P.O KOTTARAKARA, KOLLAM DISTRICT, KERALA STATE -691542 2. Name of the Institution : H.K.E. SOCIETY’S MAHADEVAPPA RAMPURE MEDICAL COLLEGE, GULBARGA – 585105 3. Course of study and subjects : M.D. ANAESTHESIA 4. Date of admission to the : 30th May 2007 course 5. Title of Topic : EFFICACY OF LOW DOSE PROPOFOL FOR CONTROL OF EMETIC EPISODES DURING CAESAREAN DELIVERY WITH SPINAL ANAESTHESIA 6. Brief Resume of the Intended work 6.1 Need for the study:
The incidence of nausea-vomiting during and Immediately after caesarean delivery with spinal anesthesia are common occurrence and an annoying problem to all concerned. In an attempt to decrease the incidence of Nausea-vomiting in these patients, a number of antiemetics have been studied, which although effective, posses clinically significant side effects. Therefore, the condition remains a challenge for anesthesiologists. Propofol has been used successfully at subhypnotic doses (0.5 – 1.0 mgkg-1hr-1) for the prevention and treatment of chemotherapy induced emesis3,4 and to treat postoperative nausea, vomiting without any side effects.5,6 However, a bolus injection of low dose (10 mg) propofol is not effective For the prevention of nausea, vomiting during caesarean Delivery because of the short duration of action of propofol administered. The need of the study is to assess the effectiveness of subhypnotic dose (1.0 mgkg-1hr-1) infusion of propofol (after clamping of umbilical artery)for prevention of intraoperative and early postoperative nausea and vomiting in elective caesarean section under spinal anaesthesia 6.2 Review of Literature
Rudra A, Halder R, Sen A et al (2004). The aim of this study was to evaluate the efficacy of propofol at subhypnotic dose (1 mgkg-1hr-1) for reducing emetic symptoms in women undergoing caesarean delivery under spinal anaesthesia. In a prospective, randomized, double-blind, placebo controlled manner, we have compared the antiemetic efficacy of propofol with intralipid as placebo (n = 30 in each group) administered immediately after clamping of the umbilical cord. Emetic episodes were noted and safety assessments were performed during spinal anaesthesia for caesarean delivery. The degree of nausea was assessed by the patients using a visual analogue scale. The incidence of patients experiencing no emetic symptoms in the intraoperative, postdelivery period was 86% with propofol and 40% with placebo(P < 0.05). No clinically important adverse events caused by the study agents were observed. We conclude that propofol, given at subhypnotic dose (1.0 mgkg-1hr-1) significantly decreases the incidence of emetic episodes in patients undergoing caesarean delivery with spinal anaesthesia without clinically important adverse events in any of the groups.
Medicine, Tsukuba City, Ibaraki (2003). Participants in this randomized double-blinded study were 100 women aged 23 to 36 yr, all scheduled for elective cesarean delivery. Randomization was to 1 of 4 groups of 25 patients each: placebo (saline) followed by placebo (Intralipid1); placebo (saline) followed by propofol (1.0 mg/ kg/hr); droperidol (1.25 mg) followed by placebo (Intralipid1); or metoclopramide (10 mg) followed by placebo (Intralipid1). Each treatment was administered IV immediately after delivery and clamping of the umbilical cord. Postdelivery emetic episodes were recorded, and patients who experienced nausea rated severity of the episodes on a scale of 0 to 10. Subarachnoid block was initiated with 2.4- 2.8 mL of hyperbaric 0.5% bupivacaine. The 4 treatment groups were similar in maternal demographics and in operative management. Comparable numbers in each group required fentanyl for pain relief and received ephedrine for hypotension. The rate of emesis-free patients (defined as no nausea, retching, or vomiting) in the intraoperative and postdelivery periods was 80% with both propofol and droperidol and 78% with metoclopramide, but only 40% with placebo. Among patients with emetic episodes, severity of nausea was less in those who received propofol than in those given placebo. None of the study drugs caused clinically serious adverse events. Yoshitaka Fujii, Mitsuko Numazaki (2002). In a randomized, double- masked trial, 80 patients received lidocaine intravenously 0.1 mg/kg (for injection pain relief) followed by either placebo or propofol at three different doses (0.5 mg/kg per hour, 1.0 mg/kg per hour, 2.0 mg/kg per hour) (n = 20 in each group) immediately after clamping of the umbilical cord. Emetic episodes and safety assessments were performed during spinal anesthesia for cesarean delivery. To estimate a sufficient sample size, it was calculated that 20 patients per group would be required with = .05 and ß = .2. The rate of patients experiencing no emetic symptoms in an intraoperative, postdelivery period was 45% with propofol 0.5 mg/kg per hour (P = .5), 80% with propofol 1.0 mg/kg per hour (P = .011), and 80% with propofol 2.0 mg/kg per hour (P = .011), compared with placebo (40%). No clinically serious adverse events caused by the study drugs were observed.
Gan TJ, El-Molem H, Ray J, Glass PS (1999). The role of propofol for the management of postoperative nausea and vomiting (PONV) is not well established. This study determines the efficacy of small doses of propofol administered by patient-controlled device for the treatment of PONV. Patients presenting for ambulatory surgery received a standardized general anesthetic. Those who experienced significant nausea or emesis within 1 h of arrival in the recovery room were randomized to receive repeated doses of propofol 20 mg (P-20), propofol 40 mg (P-40), or intralipid (placebo) on demand. Study medications (in equal volumes) were administered with a patient-controlled delivery device for 2 h. A lockout interval of 5 min between doses was used. The following parameters were assessed: nausea, vomiting, rescue antiemetic use, recovery profile, study drug administration history, and satisfaction with treatment. Sixty-nine patients participated in the study. Patient demographics were similar. The average nausea score for a patient in the P-20 and P-40 groups was 25% and 29% less, respectively, compared with placebo during the study period (P < 0.05). This difference was apparent 15 min after initiation of therapy. More placebo patients vomited (P-20, 12%; P-40, 23%; placebo, 56%; P = 0.003) and needed rescue antiemetics (P-20, 17%; P-40, 23%; placebo, 70%; P = 0.001) compared with treatment groups. Sedation scores were similar between groups. Propofol-treated patients had shorter stays in the post-anesthesia care unit (PACU; P-20, 131+/-35 min [mean +/- SD]; P-40, 141+/-34 min; placebo, 191+/-92 min; P = 0.005) and higher satisfaction with their control of PONV than placebo (P < 0.01). Propofol is effective in managing PONV with shorter PACU stay and great degree of patient satisfaction. There were two episodes of oversedation in the P-40 group. Hence, propofol at a demand dose of 20 mg seems more appropriate. Tramer M, Moore A, McQuay H ( ). We have analysed randomized controlled studies which reported the incidence of postoperative nausea and vomiting (PONV) after propofol anaesthesia compared with other anaesthetics (control). Cumulative data of early (0-6 h) and late (0-48 h) PONV were recorded as occurrence or non-occurrence of nausea or vomiting. Combined odds ratio and number- needed-to-treat were calculated for propofol as an induction or maintenance regimen, early or late outcomes, and different emetic events. This was performed for all control event rates and within a range of 20-60% control event rates. We analysed 84 studies involving 6069 patients. The effect of propofol on PONV was dependent mainly on the method of administration, time of measurement and range of control event rates. When all studies were included the number-needed-to-treat to prevent PONV with propofol was more than 9 when used for induction of anaesthesia and at best 6 when used for maintenance. Within the 20- 60% control event rate range, best results were achieved with propofol maintenance to prevent early PONV: the number-needed-to-treat to prevent early nausea was 4.7 (95% confidence interval 3.8-6.3), vomiting 4.9 (4-6.1) and any emetic event 4.9 (3.7-7.1). Within the 20- 60% control event rate, of five patients treated with propofol for maintenance of anaesthesia, one will not vomit or be nauseated in the immediate postoperative period who would otherwise have vomited or been nauseated. This may be clinically relevant. In all other situations the difference between propofol and control may have reached statistical significance but was of doubtful clinical relevance. Treatment efficacy should be established within a defined range of control event rates for meaningful estimates of efficacy and for comparisons
Lacroix G, Lessard MR, Trepanier CA. To compare the efficacy of propofol in a subhypnotic dose (10 mg iv), droperidol (1.25 mg iv), or metoclopramide (10 mg iv) in the treatment of PONV in the post anaesthesia care unit (PACU). In a prospective, randomized, double-blind protocol, over four months, all eligible inpatients and outpatients were asked to give their consent to be included in the study should they suffer PONV in the PACU. They received a standardized general anaesthetic without any prophylactic antiemetic drug. In the recovery room, patients complaining of persistent nausea (lasting more than ten minutes) and/or experiencing at least two episodes of retching or vomiting were given one of the three study drugs. Recurrence of retching or vomiting was recorded for 60 min after administration of the study drug and nausea severity was assessed on a visual analog scale. Patients still complaining of PONV 30 min after administration of the study drug received a rescue medication (dimenhydrinate). Seventy-eight patients received one of the study drugs. The recurrence of retching or vomiting was higher with propofol (58%) than with droperidol (4%) or metoclopramide (24%) (P < 0.001). More patients who received propofol needed the rescue medication (54%) than those who received droperidol (15%) or metoclopramide (28%) (P < 0.02). No difference was observed in nausea severity. A subhypnotic dose of propofol (10 mg iv) is less effective than the conventional antiemetic drugs droperidol and metoclopramide for the treatment of PONV in the PACU.
6.3 Objectives of the study 1. To evaluate the efficacy of propofol at subhypnotic doses for reducing emetic symptoms in parturients undergoing cesarean delivery under spinal anesthesia. 2. To evaluate the safety of propofol at subhypnotic doses for reducing emetic symptoms in parturients undergoing cesarean delivery under spinal anesthesia 7. Materials and Methods 7.1 Source of Data: Patients undergoing elective cesarean section under spinal anesthesia at Basaveshwar Teaching and General Hospital and Sangameshwar Hospital, attached to M.R. Medical College, Gulbarga. 7.2. Methods of collection of Data (Including sampling procedure, if any) Inclusion criteria All patients above 20yrs with ASA physical status I or II, scheduled for Caesarean delivery with spinal anaesthesia, Exclusion criteria Patients with contraindications for regional anesthesia and/or with a history of sensitivity to the drugs used in the study Patients who had gastrointestinal diseases, Patients who had ear diseases, Patients who had liver diseases Patients who had hyperemesis graviderum Patients who had hyperlipidaemia Those who have received drugs with antiemetic properties within 24 hours before surgery were not included in the study Fetal pre-maturity(less than 36 weeks gestation) was also considered a contraindication for the study.
Mode of selection of cases : Random
Allocation of Different Regimens
Group 1: To receive infusion of propofol dose (1.0 mgkg-1hr-1)
Group 2: To receive IV normal saline 1ml/kg/hr
Group-1: 30 cases Group-2: 30 cases
Parameters of comparison
1. Incidence of PONV 2. Episodes of nausea ,retching , vomiting 3. Rescue antiemetics (for severe nausea and vomiting) 4. Monitoring of vitals: BP, pulse rate, respiratory rate, every 10 minutes 5. Side effects like headache, sedation, seizures, extrapyramidal signs (tremors, dystonia). The patient are questioned about any possible of these side effects.
7.3. Does the study require any investigation or intervention to be conducted on patients or other humans or animals? If so, please describe briefly. Yes, Routine investigations like Hb, TC, DC, ESR, Routine urine examinations, RBS, ECG, blood group, blood urea, serum creatinine etc if required 7.4. Has ethical clearance been obtained from your institution incase of 7.3?
Yes. Ethical clearance has been obtained from “Ethical clearance committee of the Institution
8. List of references
1. Rudra A, Halder R, Sen A, et al. Efficacy of low dose propofol for control of emetic episodes during caesarean delivery with spinal anaesthesia. Indian J. Anaesth. 2004; 48 (1) : 31-34. 2. Mitsuko Numazaki and Yoshitaka Fujiis. Reduction of emetic symptoms during cesarean delivery with antsiemetics: propofol at subhypnotic dose versus traditional antiemetics Department of anesthesiology, university of tsukuba institute of clinicals. Medicine, Tsukuba city, Ibaraki, Japan. (J Clin Anesth, s2003;15:423–427. 3. Yoshitaka Fujii, Mitsuko Numazaki. Dose-range effects of propofol for reducing emetic symptoms during cesarean delivery. Obstetrics & Gynecology 2002;99:75-79 4. Scher CS, Amar D, McDowall RH et al. Use of propofol for the prevention of chemotherapy-induced nausea and emesis in oncology patients. Canadian Journal of Anesthesia, 1992; 39: 170-172 5. Kim SI, Han TH, Kil HY et al. Prevention of postoperative nausea and vomiting by continuous infusion of subhypnotic propofol in female patients receiving intravenous patient-controlled analgesia. British Journal of Anaesthesia, 2000; 85 (6): 898-900 6. Gan TJ, El-Molem H, Ray J, et al. Patient-controlled antiemesis: a randomized, double-blind comparison of two doses of propofol versus placebo. Anesthesiology. 1999 Jun;90(6):1564-70. 7. Tramer M, Moore A, McQuay H. Propofol anaesthesia and postoperative nausea and vomiting: quantitative systematic review of randomized controlled studies. Br J Anaesth. 1997 Mar;78(3):247-55
9. Signature of Candidate
10. Remarks of Guide
Name and Designation of the 11. 11.1 (In block letters) DR. AWATI MAHADEV NURANDAPPA M.D (Anaesthesia) Guide PROFESSOR DEPARTMENT OF ANAESTHESIA M.R. MEDICAL COLLEGE, GULBARGA 11.2 Signature
11.3 Co-guide (if any)
11.4 Signature
Dr. BASAVARAJ. V. MODI M.D (Anaesthesia) 11.5 Head of the Department PROFESSOR AND HEAD, DEPARTMENT OF ANAESTHESIA M.R. MEDICAL COLLEGE, GULBARGA
11.6 Signature
Remarks of the 12. 12.1 Chairman and Principal
12. 2 Signature