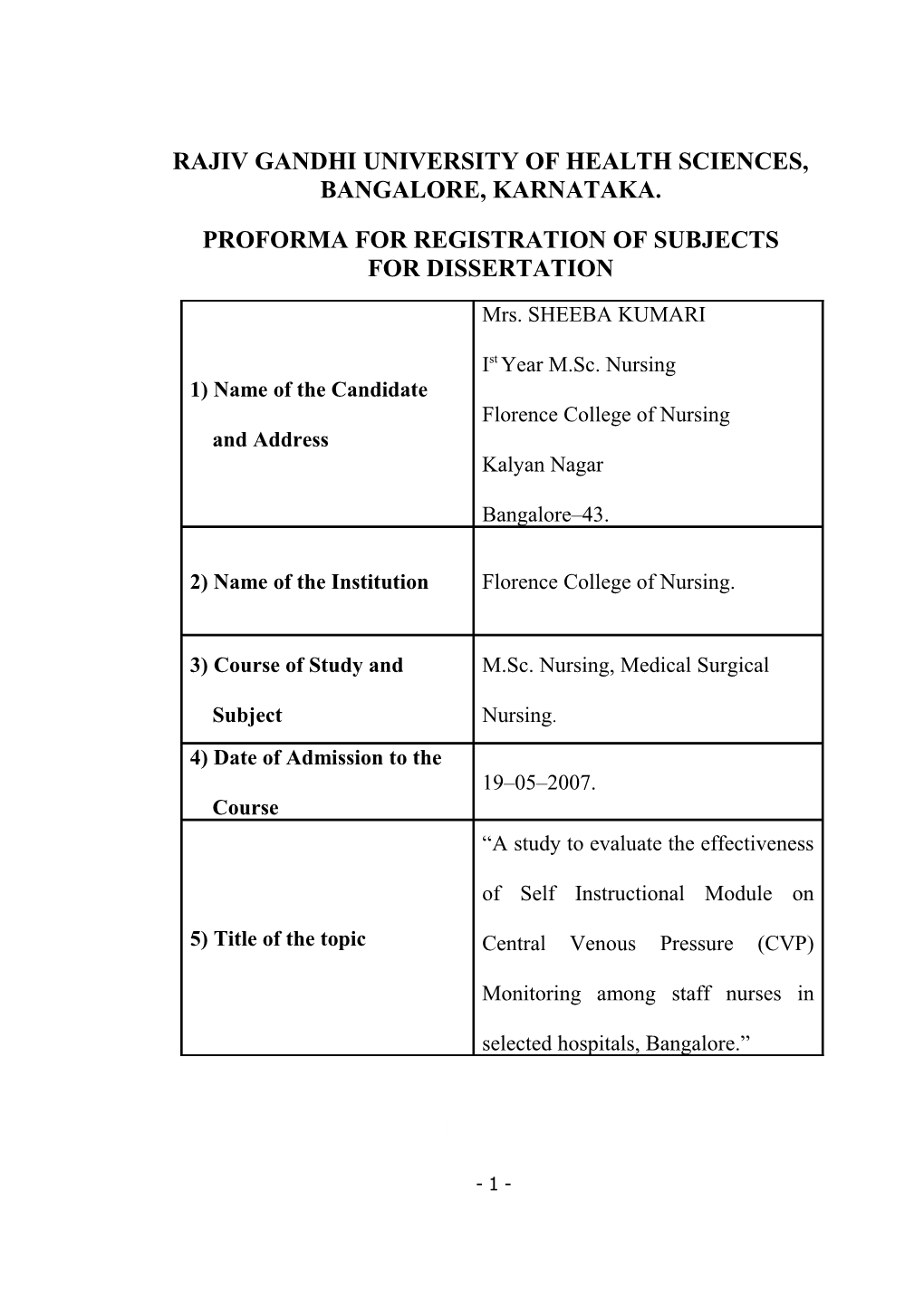
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, BANGALORE, KARNATAKA.
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
Mrs. SHEEBA KUMARI
Ist Year M.Sc. Nursing 1) Name of the Candidate Florence College of Nursing and Address Kalyan Nagar
Bangalore–43.
2) Name of the Institution Florence College of Nursing.
3) Course of Study and M.Sc. Nursing, Medical Surgical
Subject Nursing. 4) Date of Admission to the 19–05–2007. Course “A study to evaluate the effectiveness
of Self Instructional Module on
5) Title of the topic Central Venous Pressure (CVP)
Monitoring among staff nurses in
selected hospitals, Bangalore.”
- 1 - 6) BRIEF RESUME OF THE INTENDED WORK
INTRODUCTION
Critically ill patients require continuous assessment of their cardiovascular system to diagnose and manage their complex medical conditions. This is most commonly achieved by the use of direct pressure monitoring systems, often referred to as hemodynamic monitoring. Central Venous Pressure (CVP), pulmonary artery pressure, and intra arterial BP monitoring are common forms of hemodynamic monitoring. Patients requiring hemodynamic monitoring are cared for in special critical care units. Some critical care step- down units also admits stable patients with
CVP or intra arterial BP monitoring. 1
Hemodynamic monitoring provides quantitative information about vascular capacity, blood volume, pump effectiveness and tissue perfusion. In the early 1970s, hemodynamic monitoring was introduced at the bed side in the critical care unit and in the cardiac catheterization laboratory to permit measurement of several cardiac indices like CVP, Pulmonary Artery Pressure (PAP) and Pulmonary Artery Wedge
Pressure (PAWP) and cardiac out put. 2
Hemodynamic monitoring is the cornerstone of patient management in the intensive care unit. However, to be used effectively its applications and limitations need to be defined and its values applied within the context of proven therapeutic approaches. Most forms of monitoring are used to prevent cardiovascular
- 2 - deterioration or restore cardiovascular wellness. However, little data support the generalized use of aggressive resuscitation protocols in all but the most acutely ill prior to the onset of organ injury. Monitoring should be targeted to meet the specific needs of the patient and it should be used as part of a treatment protocol of proven efficacy. 3
Central Venous Pressure is the pressure within the superior vena cava reflecting the pressure under which the blood is returned to the superior vena cava and right atrium. CVP is determined by vascular tone, blood volume and the ability of the right heart to receive and pump blood. When the tricuspid valve is opened, at the end of diastole, the atrium and ventricle are, in effect, one chamber. At this time the CVP is equal to the pressure in the right ventricle and is a good indicator of right ventricular function. 4
Patient management in the critical care unit consists of a dynamic interaction between resuscitation, support systems, diagnosis, specific therapy, and monitoring.
Monitoring is central to and is inter linked with the all above components forming the basis of the tenets of intensive care, i.e., ‘measure, correct, remeasure’. While sophisticated monitoring devices cannot replace clinical judgment in critically ill patients, clinical judgment may be inadequate and even misleading. Yet, cannot be ignored. The basic clinical parameters include pulse, blood pressure, heart rate and rhythm, depth of respiration, and hourly urinary output. 5
- 3 - 6.1) NEED FOR THE STUDY
The past 20 years has witnessed a tremendous growth in the use of technology associated with central venous access. This growth is evident in both the hospitalized and home care patient populations. Central venous access presents a unique challenge to nurses. Effectively meeting this challenge translates to improved patient care. The ability to recognize and treat complications such as catheter occlusion begins with education. Central venous access provides the nurse a wide range of opportunities for improving patient care. Quality assurance activities provide a systematic method for evaluating problems and managing solutions. Research activities have enhanced patient care and the understanding of vascular access complications. Nurses are in a key position to recognize catheter occlusions and institute appropriate treatments. 6
There is wide variation in the quality of assessment, monitoring and documentation of parameters, due to a range of factors including intra and inter- observer reliability, equipment malfunction and patient preparation. Education of nurses and other health workers in the physiological and technical rationale underpinning the collection of vital signs data and other significant alterations remains as an important challenge. 7
Magder S (2005) cited that Central Venous Pressure is a very common clinical measurement, but it is frequently misunderstood and misused. As with all hemodynamic measurements, it is important to understand its basic principles. Even
- 4 - more important is the use of dynamic measures to interpret the meaning of the central venous pressure. The study concluded that, the clinical application of central venous pressure measurement requires a good understanding of the concept of the interaction of the function of the heart with the function of the return of blood to the heart. 8
Chaturvedi A, Bithal PK, Dash H, Chauhan RS, and Mohanty B (2003) did a prospective study to determine the success rate of correct catheter tip placement during central venous catheterization through antecubital veins in pediatric neurosurgical patients. Basilic or cephalic veins of either arm were selected. The length of insertion was determined from cubital fossa to the right second intercostal space. Correct catheter tip placement was achieved in 98 (49%) patients. The most common unsatisfactory placements were either in the ipsilateral internal jugular vein
(N = 38, 37.2%) or in the ipsilateral subclavian vein (N = 27, 26.4%). 9
Black MJ, Jacob ME cited that Central Venous Pressure is measured with a
Central Venous Line placed in the superior vena cava or a balloon flotation catheter in the Pulmonary Artery (PA). Normal CVP is 2 to 12 mmHg or 3-10 cmH2O. A drop in
CVP pressure indicates a decrease in circulatory volume, which may result from fluid imbalance, hemorrhage, or severe vasodilation and pooling of blood in the extremities with limited venous return. A rise in CVP indicates and increase in blood volume due to a sudden shift in fluid balance, excessive IV fluid infusion, renal failure, or sodium and water retension. 4, 5
- 5 - Dr. Muralidhar KI (2002) stated that, Indications for central venous pressure monitoring are; major operative procedures involving large fluid shifts and / or blood loss, intravascular volume assessment when urine output is not reliable or unavailable
(e.g: renal failure), major trauma, surgical procedures with a high risk of air embolism, such as sitting position craniotomies. In addition to monitoring, the central venous pressure (CVP) catheter may also be used to aspirate intracardiac air, Frequent venous blood sampling, Venous access for vasoactive or irritating drugs, chronic drug administration, inadequate peripheral IV access, Rapid infusion of IV fluids (using large cannulae) and special uses (i) insertion of Pulmonary Artery (PA) catheters (ii) insertion of transvenous pacing wires (iii) haemodialysis / plasmapheresis. 10
A catheter is introduced into the vena cava through the internal jugular, subclavian, basilic or femoral veins. If the canula is connected to a pressure transducer and monitor, the mean CVP can be recorded, which reflects competence of the right heart. A standard reference point is usually the mid axillary line or a point 5 cm below the sternum. The CVP depends on venous return, blood volume, right ventricular compliance, right ventricular contractility, and intrathoracic pressure. 5
Sheela PM (2001) assed the knowledge and practice of nurses in relation to haemodynamic monitoring in cardio-thoracic intensive care units in selected hospitals in Thamil Nadu. She found that, in CVP monitoring (80%) of the nurses closed the stop clock correctly and zeroed the transducer, but only 56.7% maintained the
- 6 - phlebostatic axis. Majority (86.7%) of the subjects turned the stopclock to IV fluids till it fills 20-25 cm level in the tubing of the water manometer, and 90% turned the stopckock to the patient to check the CVP reading. In her study, none of the subjects washed their hands before and after the procedure. Pressure. She concluded that education is necessary for staff nurses regarding CVP monitoring. 11
Gopan A (1999) conducted an evaluative study on nurses performance on hemodynamic monitoring in critical care units. The researcher identified that nurses were carelessly pushing air into arterial and CVP lines which lead to neurological complications. The study also revealed that majority of the nurses were unable to interpret the haemodynamic data with relevant clinical condition which in turn affect the health status of critically ill patients. 12
From the available literature reviewed, it is found that CVP monitoring is one of the major procedures in assessing cardiac function especially in critical care units.
Since nurses are the one, who takes care of the patient for most of the time. So the researcher found if relevant to conduct a study to evaluate the effectiveness of a self- instructional module on Central Venous Pressure (CVP) monitoring among staff nurses in selected hospitals at Bangalore.
6.2) REVIEW OF LITERATURE
The task of reviewing research literature involves the identification, selection, critical analysis and written description of existing information on the topic interest. It
- 7 - is usually advisable to undertake a literature review on a subject before actually conducting a research project. 13
Scott SS, Giuliano KK, Pysznik E, Elliott S, Welsh K, and Delbuono N.
(2005) Conducted a study on measurement of CVP through one of the three ports of centrally placed triple-lumen catheter in order to determine if a difference exist between measurement of Central Venous Pressure obtained via the proximal, medial and distal ports of a triple-lumen. In this study, repeated measures of analyses of variance showed significant differences across port sites. So care should be taken to distinguish whether changes in pressure readings are a result of change in port site rather than in the patients condition. 14
Alzeer A, Arroba S, Ansari Z, Fayed D F, and Nguib M. (2005) conducted a study to determine whether Central Venous Pressure at the common iliac vein reflects right atrial pressure in adult patient’s. In this prospective, non-blinded study 26 mechanically ventilated adult patients were studied. Simultaneous pressure readings were obtained from the right atrium and the common iliac vein. There was a correlation between the right atrium and common iliac vein (r=0.987: P<0.0001).
They concluded that venous pressure recorded from the common iliac vein reflects the pressure in the right atrium. Adopting a femoral route for Central Venous Pressure
Measurement may avoid some of the complications associated with the subclavian route. 15
- 8 - Durbec O, Viviand X, Potie F, Vialet R, Albanese J, and Martin C (2004) conducted a study on prospective evaluation of the use of femoral venous catheters in critically ill adults. Patients were carefully monitored for mechanical, infectious, and thrombotic complications. They concluded that, femoral vein catheterization with a polyurethane catheter is associated with an 8.5% frequency rate of femoral vein thrombosis. Thrombosis in the popliteal vein or posterior tibial vein is higher (25.7%).
They suggested that, femoral venous catheterization offers an attractive alternate site of insertion to the jugular and subclavian veins for central venous access in the critically ill.16
McGee W T, Ackerman BL, Rouben LR , Prasad VM, Bandi V, and Mallori
DL (2004) conducted a study on accurate placement of central venous catheters: a prospective, randomized, multicenter trial. The conclusion of that study was a) catheter tip should not be in the right atrium. b) The average safe insertion depth for a central venous catheter from the left or right internal jugular vein or subclavian vein is
16.5 cm for the majority of adult patients; a central venous catheter should not be routinely inserted to a depth of > 20 cm. c) Recently available, 15- and 16-cm central venous catheters have significant potential to minimize intracardiac placement of central venous catheters by either the internal jugular or subclavian vein route and may become the standard of care. 17
- 9 - Lorente L, Villagas J, Martin MM, Jimenez A, and Mora ML (2004) conducted a study to describe the incidence of catheter related local infection and catheter related blood stream infection caused by central venous catheters and arterial catheters. A prospective observational study was done on 988 patient’s admitted in the ICU. The study findings revealed that central venous catheter insertion at subclavian site was found to have less infection rates when compare to femoral and jugular sites. 18
Mimoz O, Pieroni L, Lawrence C, Edouard A, Costa Y, Samii K et.al.(2003) conducted a study to compare the efficacy of a newly available antiseptic solution
(composed of 0.25% chlorhexidine gluconate, 0.025% benzalkonium chloride, and
4% benzyl alcohol), with 10% povidone iodine, on the prevention of central venous or arterial catheter colonization and infection. They concluded that 4% alcohol-based solution of 0.25% chlorhexidine gluconate and 0.025% benzalkonium chloride was more effective than 10% povidone iodine for insertion site care of short-term central venous and arterial catheters. 19
Loscalzo J, Schafer AI. (2002) Central Venous Catheters are associated with a substantial risk of inducing thrombosis of the great veins. A venographic study of 12 children with indwelling Central lines for long term parenteral nutrition revealed chronic thrombosis in two-thirds of the individuals. Right atrial thrombi were diagnosed by echocardiography in 8.8% of children with Central Venous Line and
Cancer, several of which required surgical atriotomy and thrombectomy because of
- 10 - venous obstruction and a compromise of tricuspid valve in flow. Atrial thrombi were observed to be more likely to form on catheters that had their tips located in the atrium than on catheters with their tips in the superior vena cava. 20
Joynt GM, Kew J, Gomersall CD, Leung VY, and Liu EK (2000) conducted a study to determine the frequency of and potential risk factors for catheter related deep vein thrombosis in critically ill patient’s. A prospective controlled observational cohort study design was used. All adult patient’s undergoing femoral vein catheterization was selected. The result of the study shows that 26% of the patient’s develops iliofemoral deep vein thrombosis. The incidence of catheter related deep vein thrombosis was unrelated to the number of insertion attempt, arterial punchure, hematoma, duration of catheterization and coagulation status. The study conducted that the entire femoral route is convenient and has potential advantage; the use of femoral lines increases the risk of iliofemoral deep vein thrombosis. 21
Fuchs S, Pollak A and Gilon D (1999) reported that thromboembolism is a major complication of long term Central Venous Catheter, usually associated with
Catheter or Venous Occlusion. Intracavitary right atrial thrombosis is considered to result from line tip thrombosis extension. Catheter removal and anticoagulation administration were undertaken with an uneventful clinical course and almost complete disappearance of the thrombi was observed. 22
- 11 - American Association of Critical Care Nurses (1997) conducted an evaluative study on the effect of heparinized and non-heparinized flush solutions on the potency of arterial pressure monitoring lines. Potency checks were performed and recorded every 4 hours until the line was removed. At each potency check period, the following were performed: pressure bag inflation check, square waveform test and backflow test. The study indicated that the arterial pressure monitoring lines containing heparinized flush solutions demonstrated significantly greater (p<0. 00005) potency over time than lines containing non-heparinized flush solution. 23
Rush KL, and Haller LT. (1995) conducted a prospective study to examine the relationship between patient related factors and the development of central venous catheter infection. The study findings revealed that, patient’s who were receiving antibiotics during central line catheterization were at less risk of developing infection than patient’s who were not receiving them. 24
6.3) STATEMENT OF THE PROBLEM
A study to evaluate the effectiveness of a Self Instructional Module on Central
Venous Pressure (CVP) Monitoring among staff nurses in selected hospitals,
Bangalore.
6.4) OBJECTIVES OF THE STUDY
The objectives of the study are to:-
1) assess the knowledge of staff nurses regarding CVP monitoring.
- 12 - 2) evaluate the effectiveness of a self-instructional module on CVP monitoring.
3) identify the relationship between the knowledge of the staff nurses and
selected demographic variables.
6.5) HYPOTHESIS
H1: The mean post test knowledge scores of the staff nurses regarding CVP
monitoring will be significantly higher than the mean pre test knowledge
scores.
H2: There will be a significant positive correlation between the mean pre-test
knowledge scores and selected demographic variables.
6.6) OPERATIONAL DEFINITION OF TERMS
1) Self-instructional module:-
It is a booklet in English prepared by the investigator for the staff
nurses, which covers the purposes, procedure and complications of CVP
monitoring.
2) Effectiveness:-
It refers to the desired change brought about by the self-
instructional module and is measured in terms of significant knowledge
gain in the post-test and graded as adequate knowledge, moderate
knowledge and inadequate knowledge.
- 13 - 3) CVP monitoring:-
It refers to the assessment of pressure recorded by the introduction
of a catheter into the right atrium in order to monitor the condition of the
patient.
4) Staff nurses:-
In this study refers to registered nurses working in Intensive Care
Unit, Coronary Care Unit and post operative wards of selected hospitals,
Bangalore.
5) Evaluation:-
In this study refers to finding the value of the self-instructional
module on increasing knowledge of staff nurses regarding Central Venous
Pressure monitoring.
6.7) ASSUMPTIONS
1) Staff nurses working in critical care areas performs haemodynamic
monitoring.
2) The self-instructional module will enhance the knowledge of staff nurses
regarding Central Venous Pressure Monitoring.
3) Self-instructional module is an accepted strategy of teaching
- 14 - 6.8) DELIMITATIONS
The study is delimited to:-
1) evaluation of knowledge as the correct responses given to the items in the
questionnaire.
2) staff nurses working in the Intensive Care Unit, Coronary Care Units and
Post Operative wards of the selected hospitals.
7) MATERIALS AND METHODS
7.1) Source of data
Staff nurses working in Intensive Care Unit, Coronary Care Units and Post
Operative Wards.
7.2) METHOD OF DATA COLLECTION
Research Method : Quasi Experimental Method
Research Design : One group pre test post test design
Sampling Technique : Convenience Sampling Technique
Sample Size : 60 Staff Nurses
Setting of the study : Study will be conducted at St. Marthas Hospital,
Baptist Hospital and Hosmat Hospital,
- 15 - 7.2.1) CRITERIA FOR SELECTION OF SAMPLE
INCLUSION CRITERIA:-
The study includes ‘Staff Nurses’:-
1) working at selected hospitals at Bangalore
2) working in Intensive Care Unit, Coronary Care Units and postoperative
wards.
3) able to communicate in English.
4) willing to participate in the study.
EXCLUSION CRITERIA:-
The study excludes ‘Staff Nurses’:-
1) who are Auxiliary Nurse Midwives and midwives should be excluded.
2) working at other than the specified areas.
3) not willing to participate in the study.
7.2.2) DATA COLLECTION TOOL
A structured knowledge questionnaire will be prepared to assess the knowledge of the staff nurses regarding Central Venous Pressure (CVP) monitoring.
A self-instructional module will also be prepared on Central Venous Pressure (CVP) monitoring. Content validity of the tool will be ascertained in consultation with guide and experts from various fields like medicine and nursing. Reliability of the tool will be ascertained by “split half method”.
- 16 - Prior to the study, written permission will be obtained from the concerned authority. Further consent will be taken from the Staff Nurses regarding their willingness to participate in the study. The tentative period of data collection will be in July 2008.
7.2.3) DATA ANALYSIS METHOD
Descriptive and inferential statistics will be used for data analysis. Mean,
Standard Deviation, Frequency and percentile distribution will be used. A ‘t’ test will be done to compare the mean pre and post test knowledge scores. Correlation will be done to find out relationship between mean pretest knowledge scores and selected demographic variables.
7.3) DOES THE STUDY REQUIRES ANY INVESTIGATIONS OR
INTERVENTIONS TO BE CONDUCTED ON PATIENTS OR
OTHER HUMAN OR ANIMALS?
YES
Only a self-instructional module regarding Central Venous Pressure (CVP) will be used as an intervention. No other invasive, physical or laboratory procedures will be conducted on the samples.
7.4) HAS ETHICAL CLEARANCE BEEN OBTAINED?
YES
- 17 - a) Confidentiality and anonymity of the subjects will be maintained. b) Consent will be obtained from staff nurses before conducting the study. c) A written permission from institutional authority will also be obtained.
- 18 - 8) LIST OF REFERENCES
1) Smeltzer CS. Brunner and Suddarth’s Textbook of Medical Surgical Nursing.
10th ed. Philadelphia: Lippincott Williams and Wilkins; 2004. P. 677–9.
2) Ignatavicius DD, Bayne VM. Medical Surgical Nursing. 2nd ed. Philadelphia:
WB Saunders Company; 1991. P. 811 – 2.
3) Polanco PM, Pinsky MR. Principles of hemodinamic monitoring. Contrib
nephrol. 2007; 156: 133 – 57.
4) Black MJ, Jacobs ME. Medical Surgical Nursing. 5th ed. Philadelphia: WB
Saunders Company; 1997.p.1233-4.
5) Hai AA, Shivastova BR. Text book of surgery. New Delhi: Tata Mc Graw-
Hill; 2003. p. 184-6.
6) Andris DA, Krzywda EA. Central Venous Catheter Occlusion: Successful
Management Strategies. Med Surg Nursing.1999. Aug; 1-7.
7) Quinn T, Cardiovascular Monitoring Journal of Advanced Nursing; 1998;
27(3) 666.
8) Magder S. How to use Central Venous Pressure Measurements. Curr opin
criti care, 2005 Aug ;11(3) : 264 – 70.
9) Chaturvedi A, Bithal BK, Dash H, Chauhan RS, Mohanty B. Catheter Mal
placement during Central Venous Cannulation through arm veins in pediatric
patients . Journal of Neuo Surgical Anesthesiology, 2003 Jul; 15(3): 170-5.
- 19 - 10) Dr. Muralidhar KI. Central Venous Pressure and Pulmonary Capillary Wedge
Pressure Monitoring. Indian Journal of Anesthesia. 2002 Aug; 46(4): 298-03.
11) Sheela PM(2001) A study of knowledge and practice of nurses in relation to
hemodynamic monitoring patients in cardiothorasic and vascular surgery
intensive care units (CTVS ICU) of selected hospitals in Tamil Nadu.
12) Gopan A (1999) An evaluative study to fid out the effectiveness of planned
audit process on the complaints of nurses performance to audit criteria on
haemodinamic monitoring in a selected critical care unit. Master of
Philosophy in Nursing, Manipal Academy of Higher Education, Deemed
University.
13) Polit DF, Hungler BP. Nursing research: principles and methods. 6th ed
Philadelphia; JB Lppincot company; 1999. p.79.
14) Scott SS, Giuliano KK, Pysznik E, Elliott S, Welsh K, Delbuono N.
Measurement of Central Venous Pressure. American Journal of Critical care.
2005; 7 (1): 60-3.
15) Alzeer A, Arroba S, Ansari Z, Fayed DF, Nguib M. Reflection of right atrial
pressure. Canadian Journal of Anesthesia. 2005; 45(8): 798- 01.
16) Durbec O, Viviand X, Potie F, Vialet R, Albanese J, Martin C. A prospective
evaluation of the use of femoral venous catheters in critically ill adults. Crit
Care Med. 2004 Dec; 25(12): 1943-6.
- 20 - 17) McGee WT, Ackerman BL, Rouben LR, Prasad VM, Bandi V, Mallory DL
Accurate placement of central venous catheters: a prospective, randomized,
multicenter trial. 2004 Aug; 21,( 8):1118-3.
18) Lorente L, Villages J, Martin MM, Jimenez A, Mora ML. Catheter related
infection in critically ill patients. Intensive Care Med, 2004 Aug; 30(8):1681-4.
19) Mimoz O, Pieroni L, Lawrence C, Edouard A, Costa Y, Samii K et.al.
Prospective, Randomised trial of two antiseptic solutions for prevention of
Central Venous or Arterial Catheter colonisation and infection in Intensive
Care Unit patients. Critical Care Medicine. 2003 Nov; 24 (11) : 1818 – 3.
20) Loscalzo. J, Schafer. AI, Thrombosis and Hemorrhage. 2nd ed. Philadelphia:
Williams and Wilkin; 2002. p-1047
21) Joynt GM, Kew J, Gomersall CD, Leung VY, and Liu EK. Deep venous
thrombosis caused by femoral venous catheters in critically ill adult patients.
Chest. 2000 Jan; 117(1) : 178 – 3.
22) Fuchs S, Pollak A, Gilon D. Central Venous Catheter Mechanical Irritation of
the right atrial free wall; A cause for thrombous formation. Cardiology. 1999;
91(3) : 169 – 2.
23) American Association of Critical Care Nurses. Evaluation of the effects of
heparinised and non-heparinised flush solutions on the patency of arterial
pressure monitoring lines. American Journal of Critical Care. 1997; 2(1): 3
24) Rush KL, Haller LT. Patient factors and Central Line Infection. Clinical
Nursing Research. 1995; 4(4) : 397 – 10.
- 21 - SIGNATURE OF THE 9. CANDIDATE
10. REMARKS OF THE GUIDE
NAME AND DESIGNATION
11.1 GUIDE 11.
11.2 SIGNATURE 11.3 CO-GUIDE
11.4 SIGNATURE
11.5 HEAD OF THE DEPARTMENT
11.6 SIGNATURE
12.1 REMARKS OF THE CHAIRMAN & PRINCIPAL
12.
12.2 SIGNATURE
- 22 -