Rhino rescue plan decimates Asian antelopes
19:00 12 February 03
Exclusive from New Scientist Print Edition
An antelope that just a decade ago crammed the steppes of central Asia is this spring on the verge of extinction, victim of an epidemic of poaching. Biologists say it is the most sudden and dramatic population crash of a large mammal ever seen.
In 1993, over a million saiga antelopes roamed the steppes of Russia and Kazakhstan. Today, fewer than 30,000 remain, most of them females. So many males have been shot for Now you see him, soon you won't their horns, which are (Image: NATUREPL.COM) exported to China to be used in traditional fever cures, that the antelope may not be able to recover unaided.
The slaughter is embarrassing for conservationists. In the early 1990s, groups such as WWF actively encouraged the saiga hunt, promoting its horn as an alternative to the horn of the endangered rhino.
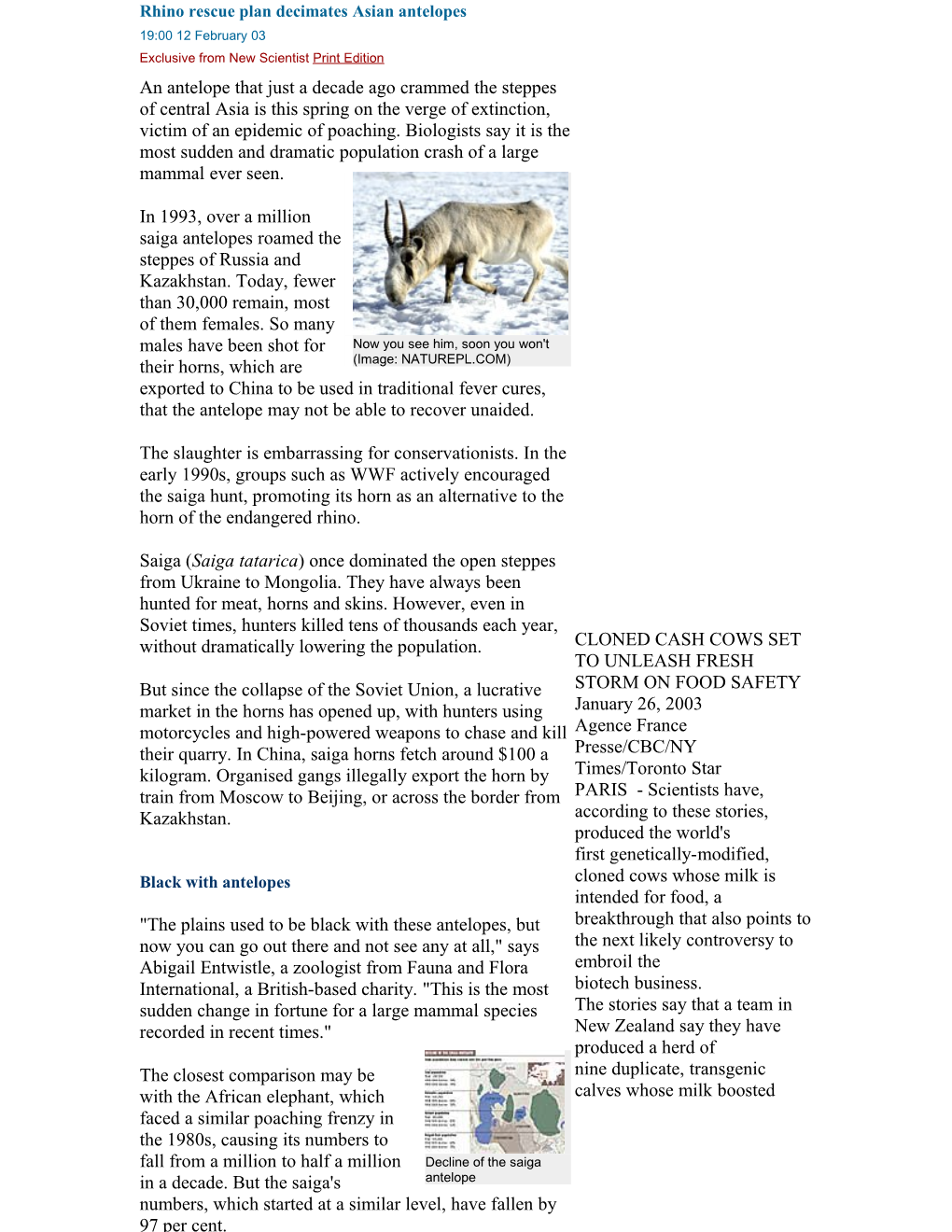
Saiga (Saiga tatarica) once dominated the open steppes from Ukraine to Mongolia. They have always been hunted for meat, horns and skins. However, even in Soviet times, hunters killed tens of thousands each year, without dramatically lowering the population. CLONED CASH COWS SET TO UNLEASH FRESH But since the collapse of the Soviet Union, a lucrative STORM ON FOOD SAFETY market in the horns has opened up, with hunters using January 26, 2003 motorcycles and high-powered weapons to chase and kill Agence France their quarry. In China, saiga horns fetch around $100 a Presse/CBC/NY kilogram. Organised gangs illegally export the horn by Times/Toronto Star train from Moscow to Beijing, or across the border from PARIS - Scientists have, Kazakhstan. according to these stories, produced the world's first genetically-modified, Black with antelopes cloned cows whose milk is intended for food, a "The plains used to be black with these antelopes, but breakthrough that also points to now you can go out there and not see any at all," says the next likely controversy to Abigail Entwistle, a zoologist from Fauna and Flora embroil the International, a British-based charity. "This is the most biotech business. sudden change in fortune for a large mammal species The stories say that a team in recorded in recent times." New Zealand say they have produced a herd of The closest comparison may be nine duplicate, transgenic calves whose milk boosted with the African elephant, which faced a similar poaching frenzy in the 1980s, causing its numbers to fall from a million to half a million Decline of the saiga in a decade. But the saiga's antelope numbers, which started at a similar level, have fallen by 97 per cent. yields of two types of proteins called caseins by up to 100 percent. The two key proteins are a boon to dairy manufacturers because they help liquid cheese to solidify and they also drive off whey, a watery byproduct that is unwanted in the curdling phase of cheese-making. The researchers, led by Goetz Laible at Ruakura Research Centre in Hamilton, on New Zealand's North Island, were cited as saying that the technique, if taken out of the lab and adopted by the dairy industry, offered "substantial economic gains," and could be widened, to "tailor" milk for human consumption. The stories explain that by inserting specific genes in a sheep, for instance, they can produce a valuable protein in its milk which can then be harvested for new drugs. Or, by producing pigs with specifically deleted genes, they may gain tissues for human organ transplants that face less risk of rejection by the patient's immune system. In addition, some pedigree animals have been genetically duplicated for commercial reasons -- research companies hope to sell the clones of livestock that, for instance, are champion producers of milk. But, the stories say, this is the first case in which a cow has been both genetically engineered and cloned to produce an altered milk for human consumption, rather than for medical research. Laible's team did this by inserting into a bovine cell two additional genes responsible for two casein proteins, beta and kappa. The modified cell was then fused with an egg whose core had been removed -- the standard technique in cloning -- and the resulting embryo then implanted into a cow uterus. Out of 126 transgenic, cloned embryos, just 11 (nine percent) survived to become healthy, viable calves. The stories add that whether or not food from cloned animals is safe for humans is being considered by many countries, including Britain and the United States. Governments are treading gingerly, given the angry debate triggered by the the first generation of food that emerged from biotech labs. Sue Meyer, a biologist with the British watchdog group Genewatch, was cited as saying that cloning and genetic manipulation of farm animals was unacceptable on welfare grounds, as many lab studies have shown these creatures are prone to sickness and early death. But there is also concern as to whether food from these animals is safe because of the knock-on effects of genetic tinkering, telling AFP that, "There's going to be enormously important questions about safety and nutritional quality. When you do genetic modification, when you introduce genes that change finely-balanced biochemical pathways, the experience we've got from plants is that you can have unexpected effects, raising or lowering other important components. If you are directing production in the cell down one pathway, increasing the activity of certain enzymes, you can have effects on other pathways." If a company sought to introduce cloned, modified food in Britain, public opposition "would just explode," she predicted. Art Hill, a professor of food science at the University of Guelph, was quoted as saying, "With this breakthrough we're a significant step closer to designer milk," but that it would be at least five years before herds of such transgenic cows produced any designer milk in commercial quantities, adding, "The cows aren't there yet. There still needs to be a lot of work done in studying the properties of this milk." Hill was further cited as saying that protein-enriched milk could give New Zealand an economic edge in selling high-value dairy products in Canada because of the greater yields and lower costs, adding, "They may have their eye on our cheddar cheese market if they could get their costs down enough to ship substantial amounts here." Cheese made from genetically engineered cows is not expected in groceries any time soon. The U.S. Food and Drug Administration has asked that milk or meat from cloned animals not be sold while it develops a policy on such products.
Location summary Sector future
Scandals: ONE DIED, 195 FELL ILL FROM PORK ROLLS IN AUSTRALIA: LAWYERS February 3, 2003 Agence France Presse English SYDNEY - Lawyers in Melbourne, renowned in Australia for its good cuisine, launched court action Monday against a Vietnamese restaurant after a man died and 195 people fell ill allegedly after eating there. Lawyers for the group allege the diners suffered salmonella poisoning after eating pork rolls at the Thanh Phu restaurant in suburban Footscray in early January. They said a 43-year-old man died and 21 people were treated in hospital for food poisoning. The youngest victim was an eight-month-old baby. It is alleged the ingredients of the pork rolls were not properly refrigerated and the restaurant's kitchen was not clean.
AUSTRALIA'S BARRIER REEF POISONED BY CANE FARM RUN-OFF: REPORT January 28, 2003 Agence France Presse English BRISBANE, Australia - Australia's Great Barrier Reef is, according to a scientific report released Tuesday, being poisoned by chemicals draining from sugar cane farms. The story says that the 200-page report by a Queensland state government scientist found that the world's largest coral reef had already suffered significant degradation and recommended restrictions on the sale of fertilisers and pesticides to cane farmers. Cane farmers have previously denied responsibility for problems on the reef, but Queensland premier Peter Beattie said the report was conclusive. "The fact is that there is damage to the reef and we need to take appropriate action," Beattie told reporters. The report found that even though cane farms accounted for only 1.1 percent of the catchment area that drains into the massive coral reef off Australia's east coast, they were responsible for most damage
Politics as usual: USDA: MOST MEAT PLANTS VIOLATE FOOD SAFETY RULES February 4, 2003 Reuters Randy Fabi WASHINGTON - USDA Undersecretary Elsa Murano was cited as telling reporters Tuesday that about 60 percent of the largest U.S. meat plants failed to meet federal food safety regulations for preventing the E. coli bacteria in their products, and that with proposed record level funding for its food safety programs in fiscal 2004, USDA would begin imposing the "next generation of enforcement" on the U.S. meat industry as part of its "war against E. coli," adding, "We are doing everything possible to prevent outbreaks of E. coli in the summer, certainly to prevent these large recalls that we've had." The story explains that in September, the department ordered all U.S. beef slaughter and grinding plants to reexamine their food safety systems after inspectors discovered E. coli was more prevalent in meat than previously thought. A preliminary review of these reassessments found 60 percent of 35 large meat plants not meeting federal food safety regulations. Garry McKee, administrator for USDA's Food Safety and Inspection Service, was quoted as saying, "They were scientific and design issues and not direct food safety issues." USDA said many plants could not verify that their food safety systems were adequate. McKee was further cited as saying the department has notified the plants to fix the problem within 30 days. Meat companies are also being told add at least one safeguard in their food safety systems that will reduce the risk of E. coli. Caroline Smith DeWaal, food safety director for the Center for Science in the Public Interest, was cited as saying USDA's findings proved that companies were not effectively implementing mandated food safety programs.
AMI BOSS RIPS MEDIA OVER SCARE STORIES ON USDA E. COLI HACCP REVIEW February 11, 2003 The Meating Place Dan Murphy www.meatingplace.com Editor's note: The following statement was issued by J. Patrick Boyle, president of the American Meat Institute, following the recent announcement by Agriculture Department officials that its review of industry HACCP plans showed more than half of the nation's biggest plants were deficient in their recordkeeping and/or verification procedures and documentation. "The beef industry benefits by doing everything in its power to ensure the safest possible beef supply. HACCP is the cornerstone of our food safety efforts and is something we take seriously. In fact, it was industry that petitioned USDA in 1994 to make HACCP mandatory. "We know that our HACCP plans and our food safety technologies are working to enhance beef safety. USDA data indicate that bacterial levels on fresh beef have declined since HACCP went into effect five years ago. In addition, Centers for Disease Control data indicate that food-borne illnesses associated with fresh beef are down. These numbers reflect an industry that is committed to HACCP. "Based on our knowledge of the facts, some news media have mischaracterized comments made by USDA [officials] last week regarding reviews of HACCP plans in large beef plants. USDA officials indicated that their reviews showed that HACCP plans in some plants had 'scientific and design issues, not direct food-safety issues.' "USDA so far has reviewed HACCP plans in 35 of the 130 largest beef plants. In 21 of the 130, 'design flaws' were identified. In a clarifying [that] statement, the Food Safety and Inspection Service said" 'The plants have responded to FSIS questions in writing in keeping with FSIS regulatory requirements.' Stories bearing headlines like 'Most Meat Plants Violate Food Safety Rules' are patently false. This type of reporting is inaccurate and counterproductive. "There are no benefits to taking food-safety shortcuts in [the industry's] HACCP plans; to the contrary, [companies] benefit by having the best possible HACCP plans, and that is what beef companies have tried to prepare. The industry will take any comments provided by FSIS seriously and will make appropriate changes to [its] HACCP plans. "Careless reporting of this type of information serves only to alarm consumers about a meat supply that is safe and getting safer every day." MISINTERPRETING THE FACTS February 10, 2003 Lean Trimmings Edited by Kiran Kernellu As any one of 8,000 establishments could attest to, it's difficult to understand the regulatory tools and enforcement processes used by USDA to measure compliance with its myriad rules and regulations. In a separate item in this week's newsletter, we have set forth the regulatory steps to the best of our understanding. Understanding the regulatory system goes a long way to doing what it takes to be in compliance. Unfortunately, Reuters reporter Randy Fabi got it wrong last week. He wrote, under the headline, Most Meat Plants Violate Food Safety Rules, that about 60% of the largest U.S. meat plants failed to meet federal food safety regulations for preventing the E. coli bacteria in their products, and named his source as USDA. He reportedly derived his misinformation from a briefing last Tuesday when Under Secretary Dr. Elsa Murano and FSIS Administrator Dr. Garry McKee briefed interested constituencies with an update about how the industry was meeting the 2002 Directive requiring them to reexamine (re-assess) their plans in light of evidence that E. coli O157:H7 was more prevalent in live animals than was previously thought. As part of the reassessment process, FSIS's Consumer Safety Officers (CSO) are first visiting the 130 largest plants in the industry and examining their HACCP plans. So far 35 plants have been reviewed, and in about 21 of the reviews, the CSOs have asked for further scientific documentation about preventing and eliminating food safety hazards. Dr. Murano and Dr. McKee reportedly restated in response to questions from reporters that the additional questions involved "scientific and design" issues related to HACCP plans. Unfortunately, that was not the message that the Reuters reporter gave, and his misinterpretation has been widely re-stated. We encourage members who find the article in local papers to send it, and the one about regulatory tools, to Reuters and seek clarification.
REGULATORY TOOLS FOR PRODUCTION OF SAFE MEAT & POULTRY February 10, 2003 Herd on the Hill Edited by Kiran Kernellu The USDA is responsible, under the Federal Meat Inspection Act and Poultry Products Inspection Act, of providing "continuous" inspection, including ante and post mortem inspection, to assure that meat and poultry is wholesome and not misbranded or adulterated. That is the law. Pursuant to the Pathogen Reduction HACCP rule of July 1996, USDA required companies to develop Standard Sanitation Operating Systems (SSOPs) and a Hazard Analysis Critical Control Point (HACCP) plan for operations. USDA officials monitor the activities in official establishments to confirm the effectiveness of SSOPs and HACCP plans, and have developed regulatory tools to carry out these responsibilities. The first regulatory tool is the Non-Compliance Record (NR) issued by an Inspector in Charge or off-line Inspector, which identifies a specific non-compliance. It may be accompanied by a regulatory action to retain product if food safety or direct product contamination is at issue. An NR describes the unacceptable condition. Plants may simply accept the NR and take corrective action, or may appeal the NR. Plants are expected to indicate corrective action and what they will do to prevent reoccurrence in writing. After reviewing the SSOP or HACCP plans, inspectors could also issue what is called a 30-day reassessment letter. A 30-day reassessment letter is not considered an enforcement action. Rather, it is issued when there are unclear provisions or questions about the design of the plan that require clarification or resolution. In the event the response to the 30-day reassessment letter is deemed inadequate, FSIS may issue a Notice of Intended Enforcement (NOIE). The next regulatory tool is a NOIE. A NOIE identifies repetitive non-compliance traced to the same root cause, and a failure by the company to prevent the reoccurrence. Plants have 72 hours or 3 business days to respond to an NOIE. If the response to the NOIE is unacceptable, the next regulatory step is a Notice of Suspension, which will be faxed or hand delivered to the plant officials identified on the grant of inspection, and unless there is an imminent food safety risk, a company is usually allowed to complete the shift before the suspension is effective. Inspection is restored when the offending condition is corrected. Also, if appropriate corrective action is taken immediately, then the suspension may be held in abeyance, usually for a designated period of time. In addition to the above, FSIS inspectors have the authority to take immediate action to prevent adulterated or misbranded meat from leaving the plant with the application of a RETAIN tag, or to use this tag to prevent the use of unsanitary equipment or facilities. They would also issue an NR after applying the tag. Plants have the right to appeal at every level by asking the next level of USDA to evaluate and reconsider. The appeal system is lengthy and cumbersome, and often seen as a "rubber stamp" and ineffective. Also, plants may fear retaliation and prefer to stay "under the radar line." Thus, there are relatively few appeals of NRs. FSIS takes the position that retaliation is neither tolerated nor condoned. There are special guidelines to be followed if a company makes such a charge, and NMA recommends that its members consult with it and/or counsel. All regulatory and enforcement actions are recorded and included in the Quarterly Report issued by FSIS and are available on USDA's website at http://fsis.usda.gov/OA/haccp/qer.pdf. The most current one available is April-June 2002. Remember, the fundamental goal of industry, and USDA through its regulatory role, is to ensure the production of food that is safe and wholesome.
EBOLA HEMORRHAGIC FEVER - CONGO REP: SUSPECTED ********************************************** A ProMED-mail post
Date: Weds 5 Feb 2003 From: ProMED-mail
Ebola outbreak feared in Congo ------In the north of Congo-Brazzaville, 16 people have died in a suspected outbreak of Ebola virus infection. The Congolese authorities say they are extremely concerned that the virus might spread. There is no cure for Ebola and little is known about the virus, which causes its victims to die from internal hemorrhaging.
The Congolese Ministry of Health says 16 people are known to have died so far, but communications with the villages of Kele and Mbou, 800 kilometers north of Brazzaville in the Region of Cuvette West, are difficult. Dr Joseph Mboussa, director in the Ministry of Health, says a villager has been dying every few days since the outbreak began on 4 January, and already the death toll could be much higher than 16.
The authorities were first alerted to a possible outbreak when a clan of gorillas in the Cuvette West Region began to die. Tests carried out on the bodies confirmed that the gorillas had died from the Ebola virus, and the disease has now claimed more than 80 per cent of the gorilla clan.
Medical professionals are at great risk of contracting Ebola. The Ebola virus is easily spread just by skin contact with an infected primate or person. Dr Mboussa says this makes the virus particularly difficult to contain, as Congolese funeral rites dictate that the body of a deceased person be washed by the family before burial. The current outbreak is believed to have been caused by villagers eating primates which were already infected with Ebola.
An emergency team of health ministry workers was scheduled to leave for the region on Wednesday to investigate the outbreak and try to contain it, following delays caused by a shortage of petrol and funds for the trip. Ebola experts working for the World Health Organization in Libreville and Geneva also expect to leave soon to investigate the outbreak. Some years ago in the neighboring Democratic Republic of Congo, then President Mobutu Sese Seko adopted a controversial policy of putting an infected village in quarantine. The Ebola virus was contained but the entire village was wiped out. The Congolese health ministry has so far asked local inhabitants not to travel, but the authorities are hopeful they will not have to resort to such drastic measures.
The forestry ministry already has several teams in place trying to make locals aware of the dangers of eating primates, but they admit it is a losing battle in a region where bush meat has formed a staple part of people's diets for centuries.
[byline: Pascale Harter]
-- ProMED-mail
[This is the same general region (Cuvette West) where the last Ebola outbreak in the Congo Rep occurred in 2002. If Ebola is confirmed as the etiology of this outbreak, it will not be the first human outbreak that occurred coincident/following an observed outbreak in primates in this region. As this newswire mentions, primate meat is part of the local diet in this region. The preparation of infected primates for food source is the most likely vehicle for transmission of the Ebola virus to the humans. Given this, the occurrence of primate die-offs in known Ebola regions should trigger increased efforts to alert the local population of the increased risks involved with eating primates. But as the last sentence of the above newswire suggests this is clearly easier said than done. - Mod.MPP]
[see also: Ebola hemorrhagic fever, apes - Congo Rep. 20030124.0207 2002 ---- Unexplained deaths, wildlife - Congo Rep: RFI 20021207.5996 Ebola hemorrhagic fever - Congo Rep: confirmed 20020613.4492 Ebola hemorrhagic fever - Congo Rep: suspected (02) 20020613.4482 Ebola hemorrhagic fever - Gabon/Congo Rep (26) 20020510.4151 Ebola hemorrhagic fever - Gabon: gorilla-to-human? 20020409.3915 Ebola hemorrhagic fever, new diagnostic test 20020228.3647 Ebola hemorrhagic fever - Gabon/Congo Rep 20020102.3149 2001 --- Ebola hemorrhagic fever - Gabon/Congo Rep (04) 20011231.3142 Ebola hemorrhagic fever - Gabon/Congo Rep 20011225.3109 Ebola hemorrhagic fever - Gabon: dead wildlife (03) 20011220.3079 Ebola hemorrhagic fever - Congo Rep. 20011220.3075 Ebola hemorrhagic fever - Gabon (07) 20011220.3074 Ebola hemorrhagic fever - Gabon: dead wildlife 20011216.3041 Ebola hemorrhagic fever - Gabon: WHO confirms 20011211.3002 Viral hemorrhagic fever, suspected - Gabon 20011205.2950]
Location summary Sector general information
Scandals:
Date: Mon 3 Feb 2003 From: Pablo Nart
Sleeping sickness kills 26 people in Uije ------26 people died and 18 others became ill with sleeping sickness in 2002 in Uije and Kitexe districts and at Wamba and "Vale do Loge" resettlement areas, out of the 34 153 people assisted voluntarily in ambulatory consultations.
The person responsible for fighting sleeping sickness in Uije, Kiala Gode, reported that in 2002 there were 3870 traps placed by 304 tse-tse fly capturers who took part in the operation in 177 villages of Uije, Negage, Songo, Mucaba, and Kitexe distritcts. As result of the operation, 156 314 flies were captured in the districts of Uije and Negage under the campaign meant to end the disease. Kiala Gode revealed the lack of economic support for the extension of the operation and control of the sleeping sickness in the rest of the district, as well as for adequate nourishment and sleeping clothes for the 72 inpatients currently at the treatment centres in Uije and Negage.
USA: Biotech pigs may have entered food supply - FDA 06 Feb 2003 Source: just-food.com
Almost 400 pigs that had been used in US bioengineering research may have entered the food supply because they were sold to a livestock dealer instead of being destroyed, the US Food and Drug Administration has said.
The FDA said that researchers at the University of Illinois at Urbana/Champaign released 386 pigs from biotech studies to a livestock dealer between April 2001 and January 2003. Animals involved in this particular study were to have been destroyed by incineration or rendering to prevent their introduction into the human food supply.
The FDA said the pigs did not pose a public health risk, but that the incident, if confirmed, would represent a significant breach of the FDA requirements for this study, warranting strong action against the responsible parties.
“The researchers claim that these pigs, which were the offspring of transgenic animals, did not inherit the inserted genetic material from their parents - that is, they were not themselves transgenic. However, FDA cannot verify this assertion because the researchers did not conduct sufficient evaluation or keep sufficient records to assess whether the offspring inherited the inserted genetic material,” the FDA said in a statement.
Because the pigs were experimental animals, the FDA said it had not yet determined the safety or efficacy of the genetic material they contained but scientific evidence indicates that they would not present a health risk.
“The genes were engineered so that the proteins would be produced primarily, if not exclusively, in the mammary glands of lactating sows. None of the pigs sent to slaughter are believed to have been old enough to lactate. Therefore, FDA does not believe that any product derived from these animals would have to be removed from commerce for public health reasons, and USDA concurs,” the FDA said.
The FDA added that in collaboration with the US Department of Agriculture it was carrying out an investigation into the incident. Politics as usual:
EUROPE WARNS US: HANDS OFF OUR BIOTECH FOOD BAN February 4, 2003 Agence France Presse English/ New York Times/Reuters WASHINGTON - European Union farm chief Franz Fischler was cited as warning Tuesday of a consumer backlash if the United States tried to dismantle its ban on genetically modified foods, adding, "We would strongly advise not to start action in this moment in the WTO. There is a clear risk... our skeptical consumers would take this as an opportunity to make even more difficulties against the use of GM foods than in the past. There is a clear risk that if one starts action now that the European parliament could be reluctant to make the final decision" on the approval process which could come in "three or four months." Peter Allgeier, Deputy U.S. Trade Representative, was cited as telling reporters that Washington was in consultations with potential allies on the timing of any WTO action against the EU's four-year-old moratorium on approval of genetically modified (GM) products, adding, "I am very confident there will be others. I do not think we will be faced with a decision on whether to go it alone."
The Times reported that the Bush administration has decided against antagonizing its European allies and has postponed filing a case against the European Union for its ban on genetically modified food, according to a senior administration official. A senior White House official who asked not to be identified, was quoted as saying, "There is no point in testing Europeans on food while they are being tested on Iraq," A cabinet meeting to consider the suit was canceled this week as European agricultural officials descended on Washington to argue for patience. Even so, the conflict will resurface soon. Mr. Zoellick has said he believes that genetically modified food could help alleviate hunger < as well as open markets for American farmers < and wants the European opposition to be confronted so that developing nations accept food from genetically modified crops. Ann M. Veneman, the United States agriculture secretary, has said that "our patience is just running out." Franz Fischler, the European Union's farm commissioner, said that he met with Ms. Veneman and told her the problem would be resolved within three or four months. They are demanding labels that identify which food has been genetically modified and has passed rigorous testing. The agricultural establishment in the United States is just as strongly opposed, saying that once the food has passed tests there is no need to distinguish it with label that could be seen as a warning. "That implies that there is something wrong with genetically modified food," said Elsa Murano, the Agriculture Department's undersecretary for food safety. "It would be another kind of trade barrier." Industry also complains of the cost. "Labeling is a sham," said Mary Kay Thatcher, lobbyist for American Farm Bureau, a powerful agricultural group. "It would be so expensive, it would shut down our exports." Margaret Beckett, the British minister in charge of food and the environment, said both sides of the argument had to understand the serious cultural differences underlying the disagreement. After the deaths in Europe from mad cow disease and the subsequent killing of herds infected by foot and mouth disease, European consumers are wary of any food that is not clearly labeled and easily traced. The Times story says that while European nations agree on the need for labeling in the face of deep consumer fears, American lawmakers have had a more mixed record. Although it took 12 years of lobbying by farmers, chefs and environmentalists, the agriculture department last year created an official organic label to show consumers what produce has been raised without conventional pesticides or fertilizers, antibiotics or growth hormones. The food is growing in popularity < it is a $4 billion industry < and public response was overwhelmingly in favor of the new label. As industry feared, the cost of the label has proved prohibitive for some of the smallest farmers < averaging $5,000 each year < and the paperwork is time-consuming. Federal officials believe that the process could be streamlined over the years. In last year's farm bill, Congress included a provision opposed by much of agribusiness that required that all meat, fish and produce be labeled with its country of origin within two years. Already, Canada has complained that the new country of origin labeling will restrict its trade with the United States, especially in meat. In a study released last month, Canadian officials complained of the cost and suggested that the new provision should be withdrawn. That is unlikely until the European ban on genetically modified food is lifted and the issue of labeling is confronted head on. Trade and agricultural experts predict that in the end a compromise may have to be reached among competing interests within the United States as well as between the Europeans and the Americans. "The United States is not monolithic," said John Audley of Carnegie Endowment. "Business groups may have to yield on labeling while activists will have to yield on allowing genetically modified food to be sold and let consumers decide what they want." RABIES & VULTURE DIE-OFF - INDIA *****************************
Date: Wed, 5 Feb 2003 From: Pablo Nart
Vulture deaths bring rise in rabies ------The catastrophic decline of the vulture population in India, vital to cleaning the streets of offal and rubbish, has led to an explosion in the number of feral dogs and an increasing human death toll from rabies. An unknown virus has been killing 3 species of the once numerous vultures in the last 10 years. This has led to a crisis.
Habitually, butchers threw offal outside for the vultures, which effectively solved the waste problem. The vulture's niche has now been taken over by feral dogs, the main carriers of rabies. More people now die of rabies in India than anywhere else.
Zoroastrians have had to abandon their traditional practice of placing their dead on Towers of Silence for the vultures to eat.
So alarmed has the government become about the diminished vulture population they have set up a rehabilitation centre to save sick birds and release them into the wild. Britain has donated 145 000 GBP [236 311 USD] for a centre near Delhi, and Elliot Morley, the department of the environment minister for wildlife, will officially open it on Saturday,7 Feb 2003. Mr Morley said "There has been a very high mortality, around 97 per cent of vultures have disappeared."
[byline: Paul Brown]
-- ProMED-mail
[While it may be true that an increase in rabies incidence is being observed in India, the statement "more people now die of rabies in India than anywhere else" was valid before the vulture die-off. The latest available World Survey of Rabies that includes India (WHO, 1998) stated that "the highest incidence continued to be observed in Asia with 33 075 reported human deaths due to rabies. Most of them (estimated 30 000) occurred in India".
[see also: 2002 --- Vulture die-off - India, Pakistan, Nepal (04) 20021018.5590 Vulture die-off - India, Pakistan, Nepal (03) 20021015.5557 Vulture die-off - India, Pakistan, Nepal (02) 20021014.5552 Vulture die-off - India, Pakistan, Nepal: RFI 20021010.5514]
Location summary sector general information
Scandals: MINISTRY SAYS DIOXINS FOUND IN GERMAN ANIMAL FEED February 7, 2003 Reuters BERLIN - Officials were cited as saying on Friday that animal feed produced by a firm in eastern Germany tested positive in January for carcinogenic dioxins, and over 100 tonnes of possibly contaminated feed could have been exported to the Netherlands. Germany's Agriculture Ministry was cited as saying in a statement that the Dutch authorities had been informed. Tests in January had shown animal feed produced by the company in the state of Thuringia contained around 15 times more than the permitted level of dioxin. Dioxin has been linked to several cancers in humans, including lymphomas and lung cancer. Some 300 pigs that had been given the feed had to be slaughtered after tests showed high levels of the poison, according to a statement on Thuringia's Agriculture Ministry Web site
The growing controversy over food irradiation
Friday, January 31, 2003 By Melissa Knopper, E/The Environmental Magazine
Over the past several years, a series of highly publicized recalls have sent panicky consumers running to the fridge to check for tainted meat.
It started in 1998 when Sara Lee recalled millions of pounds of hot dogs and deli meat after 21 people died in a Listeria outbreak from a processing plant in Michigan.
Then, in 2000, a three-year-old Milwaukee girl died after eating watermelon splashed with E. coli 0157:H7 (the most deadly form) at a Sizzler restaurant. Federal investigators traced the E. coli, which made 600 other people sick, to a Colorado Excel meat plant. Most recently — in the second-largest meat recall in U.S. history — ConAgra recalled 19 million pounds of ground beef contaminated with E. coli that made 17 people sick in Colorado.
As these outbreaks continue to generate publicity, people are looking for ways to protect themselves from gaps in the country’s meat inspection system. Food irradiation — an unpopular option in the past — is starting to gain more acceptance. In fact, the federal Food and Drug Administration (FDA) is considering proposals to expand the number of foods that could be irradiated. The food industry already irradiates raw meat and spices; soon, the government may permit irradiated processed meats and imported produce. While it has won some support, food irradiation also generates fiery opposition. As more stores offer irradiated products, the issue is generating nearly as much controversy as genetically engineered foods. Scientific Support
Many scientific organizations, including the U.S. Centers for Disease Control and Prevention, the World Health Organization, and the American Medical Association, endorse food irradiation. The FDA has tested the safety of irradiated foods in both animals and humans, and NASA originally used irradiation to protect the meals astronauts ate in space.
Ricardo Molins, a microbiologist and irradiation expert with the National Academy of Sciences, believes irradiation is a safe and effective way to reduce foodborne illness. "We don’t live in a sterile world; mud and manure could end up in your hamburger," Molins said. "If people don’t like to eat their hamburgers well done, they should buy irradiated meat."
Irradiation prevents food poisoning by killing harmful bacteria such as E. coli, Salmonella, and Listeria. When high-energy beams of radiation pass through the food, it damages the DNA of these microorganisms, reducing the potential for disease. Irradiation will not eliminate viruses and prions, which are the infectious proteins that cause mad cow disease. The process changes some foods, especially those that have a high fat content. Irradiated eggs become runny, and some meats develop an unpleasant odor and taste.
An Industry Cheers
Food industry groups, such as the Grocery Manufacturers of America and the American Meat Institute, are in favor of irradiation. While surveys show consumers tend to be wary of irradiated foods, some stores already sell them. East Coast grocery chain Wegman’s started to aggressively market its own brand of irradiated hamburger last summer.
"E. coli 0157:H7 is especially dangerous to young children, elderly people, and anyone with a compromised immune system," said Wegman’s spokesperson Joanne Colleluori. "This product gives our customers peace of mind."
Irradiation opponents, however, argue it could give the meat industry an excuse to look the other way instead of cleaning up flaws in the system that led to the recent outbreaks of foodborne illnesses. People are getting sick because of the increase in factory farms where cattle are crowded into small pens, sleeping in their own waste, said Patty Lovera, deputy director of Public Citizen’s critical mass energy and environment program.
Instead of grazing on their natural diet of grass, the cows eat grain-based foods, which cause E. coli to flourish in their digestive tracts. The animals move through the slaughter lines so quickly, mistakes cause fecal matter to contaminate the meat, she added. "The meat industry has created a system that makes it difficult to produce a wholesome product," Lovera said. "They see irradiation as a quick fix."
But Matt Baun, a U.S. Department of Agriculture (USDA) spokesperson, said, "There isn’t going to be any lessening of sanitation in these plants as a result of irradiation. We have 7,500 inspectors, and they are in every plant every hour." The USDA will ask meat plants to use additional techniques to kill pathogens, such as steam pasteurization. If consumers want to be sure they’re protected from E. coli, however, Baun said it’s important to make sure they cook beef at 160-degrees Fahrenheit.
What’s in Our Food?
Consumer advocates are also concerned about labeling. Congress recently passed a measure as part of U.S. Senator Tom Harkin’s (D-Iowa) farm bill that would allow grocery stores to label irradiated products as being treated with "electronic pasteurization."
Groups like Public Citizen, the Center for Science in the Public Interest (CSPI), the Organic Consumers Association, and Food and Water feel this term is misleading and confusing. Consumers must be vigilant because the FDA’s labeling rules for irradiated foods have serious loopholes, Lovera said.
For example, restaurants, schools, and hospitals are not required to notify the public if they are serving irradiated foods. Similarly, a company could make applesauce with irradiated apples but would not have to disclose that on the list of ingredients.
"We’re encouraging people to contact big food companies like Tyson, Kraft, and Hormel and tell them they don’t want irradiated foods," said Danila Oder of the Minnesota-based Organic Consumers Union. Several groups are organizing letter- writing campaigns to oppose the FDA labeling changes.
And the Empire State Consumer Association in New York has been meeting with Wegman’s and local school officials to call for a ban on irradiated products. The group encourages consumers to instead buy from local farm markets, community- supported agriculture programs, and food co-ops.
Activists from Public Citizen believe the government needs to do more long-term studies of the potential health risks of a steady diet of irradiated food. They point to the vitamin loss that occurs in some irradiated foods.
Scientists also have identified a new class of chemicals, called cyclobutanones, which only occur in irradiated foods. A German study suggests these compounds could accelerate the growth of cancer in humans. While Public Citizen believes the study has merit, other scientists — including FDA investigators — have not been able to replicate the results.
Meanwhile, activists at the Vermont-based Food and Water are raising questions about the potential for nuclear accidents at irradiation facilities. There already have been injuries and deaths when radioactive materials are mishandled at food irradiation plants, said Executive Director Michael Colby. And the possibility of a terrorist threat at these facilities is even scarier, Colby said. He argues that it’s safer to keep dangerous materials in one guarded storage bunker.
Food and Water’s grassroots campaign also raises awareness about the corporate politics behind the recent push to use irradiation for food safety. "From the beginning, irradiation has been an attempt to use up nuclear waste products and to put a smiley face on all things nuclear," Colby said.
In her new book, Is Our Food Safe? A Consumer’s Guide to Protecting Your Health and the Environment, CSPI Director of Food Safety Caroline Smith DeWaal concluded the benefits of irradiation outweigh the risks, although she agrees on the need for more studies on long-term health effects. As long as packaging is clear and understandable, DeWaal believes consumers should have the opportunity to buy irradiated food if they want it. "The people who prefer natural foods probably are going to avoid irradiated food; it really is an issue of consumer choice," she said. "For many consumers, the ideal solution is to eat less meat and to avoid ground beef because it’s one of the most risky foods."
Melissa Knopper is a Denver-based journalist specializing in health and science topics.
Location summary
Sector irradiation
Politics as usual:
WORLD FOOD EXPERTS STILL DIVIDED OVER IRRADIATION February 9, 2003 Reuters Jeremy Smith BRUSSELS -- International food experts will soon discuss revising -- if not abandoning -- the maximum dose for irradiation, an idea that has, according to this story, stirred opposition from the European Union and infuriated numerous consumer lobby groups. The story says that while most scientists have accepted irradiation as a processing technique, consumers and environmentalists have their doubts about foods that are blasted with high-energy radiation in the form of gamma or X-rays to kill unwanted micro-organisms. Now, the recommended upper limit for absorbed radiation in food may be removed altogether if a committee of the Codex Alimentarius Commission, due to meet in Tanzania in mid-March, can reconcile wide differences of opinion among its members. A Codex official was quoted as saying from the organisation's home base in Rome that, "If they are successful a final text will be submitted to the Codex Alimentarius Commission for formal adoption in June. If they cannot agree, we can expect a two-year delay." The story says that irradiation, endorsed by the World Health Organisation, exposes food to low amounts of electrons or gamma rays to destroy micro-organisms such as E.coli and salmonella. It causes chemical changes but does not leave food radioactive. Codex, which groups officials from the United Nations FAO and World Health Organisation, sets non-binding recommendations for food standards often used as the benchmark in international trade disputes. It has members from more than 160 countries. Since the last major Codex meeting on irradiation, a working group has drafted a compromise proposal that keeps a maximum dose but also inserts a controversial clause saying that high-dose irradiation has no effect on product safety. In a standard dating from 1983, Codex sets the maximum level of absorbed permitted irradiation in food at 10,000 Gray (Gy), which represents 10,000 joules of absorbed energy per kilogram (2.2 lb). Despite the compromise Codex wording, agreement on whether to remove or keep a maximum dose is still a long way off and observers say the debate could still go either way. Merav Shrub at Britain's Food Commission, an independent watchdog group, was quoted as saying, "This document will be discussed and may, or may not, be agreed at that (March) meeting. It may just get postponed with further debate for another year. What they are proposing is a compromise to keep the 10 kGy dose limit but with a comment saying that it's absolutely safe at any dose anyway. It's a bit contradictory." The story notes that several countries, including most EU member states backed by Japan and South Korea, are opposed to removing this maximum dose. In the European Commission, officials are wary about the idea of removing the upper limit, saying the resulting large-scale irradiation might flout good hygiene practices. At present, the EU permits food to be irradiated under only one category: dried aromatic herbs, spices and vegetable seasonings. All irradiated foods must be properly labelled with the words "irradiated" or "treated with ionising radiation." Five EU member states also allow the marketing of certain irradiated foods such as fresh and dried fruits and vegetables, poultry, shrimps, fish or frog legs on their national territory. The United States, Australia, the Philippines and Thailand lie on the other side of the argument and claim that the dose is self-limiting as amounts above 10,000 Gy are only technically feasible for a few dry commodities such as spices.
Scandals:
Pure Water or Pure Peril? Your bottled water is contaminated by pesticides. Gaping holes in regulations and corporate irresponsibility in the fastest growing segment of the beverage industry make a mockery of public health
New Delhi, February 4, 2003: We take it for granted that the bottled water we drink is safe. But a Down To Earth exposé, based on tests conducted by the Pollution Monitoring Laboratory of the Centre for Science and Environment (CSE) shows otherwise.
After analysing 17 brands of packaged drinking water sold in and around Delhi and 13 brands from the Mumbai region, the CSE lab found the samples to contain a deadly cocktail of pesticide residues. Most of the samples contained as much as five different pesticide residues, in levels far exceeding the standards specified as safe for drinking water.
The samples had enough poison to cause in the long term, cancer, liver and kidney damage, disorders of the nervous system, birth defects, and disruption of the immune system. Pesticides do not kill immediately, but can cause irreparable health disorders as they accumulate in the body fat.
The CSE lab tested for two types of pesticides: organochlorine and organophosphorus. The findings were appalling. The four most Click to enlarge commonly found pesticide residues were lindane, DDT, malathion Sunita Narain, CSE director and and chlorpyrifos. Using European Economic Commission norms for Down To Earth editor, fields maximum permissible limits for pesticides in packaged water, the questions from media CSE lab tests of samples from the Delhi region showed that on average, each sample contained 36.4 times more pesticides than the stipulated levels. The Mumbai samples were a shade better, primarily because the source water used by the industry was relatively less contaminated.
CSE used European norms because the standards set for pesticide residues by the Bureau of Indian Standards (BIS) are vague and undefined. The standards say, "pesticide residues shall be below detectable limits". This, one would assume, means that there ought to be no pesticide residues at all in the bottled water. But no, it actually means that one should not be able to find the pesticide residues in the water. The BIS has specified the methodology for detecting pesticide residues and this methodology, which is not very sensitive, does not detect pesticides unless present in extremely high quantities.
Even for drinking water, the BIS norms specify that pesticide residues should be "absent". What is plainly absurd is that if drinking water norms specify that pesticides should not be present, how can packaged drinking water norms be so vague, and use a non-quantifiable phrase, such as "below detectable limits"? Even going by drinking water norms, all the bottled water brands tested by the CSE lab would fail the test of quality.
What was found: Top seller Bisleri was third from the bottom, with pesticide concentration levels 79 times higher than the stipulated limits (see graph). Kinley had concentration levels 14.6 times above the maximum permissible amounts. Aquaplus — favoured by the Indian Railways — topped the dubious list, crossing the limit by 104 times!
Contamination levels were significantly lower in packaged natural mineral water brands Himalayan and Catch from Himachal Pradesh, a state with lower pesticide use. In the Mumbai region, the worst brand was Oxyrich, with 16.7 times higher pesticide concentration levels than the prescribed standards. Bisleri and Kinley fared better in the Mumbai samples – they were ranked 7th and 4th respectively.
The lab also collected raw water from bottling plants to verify its findings. In all cases, tests showed that the pesticides found in the source water matched the toxins found in the bottled water — proof that the source of the pesticide residues is contaminated groundwater. Plants manage to eliminate somewhere between 20 and 80 per cent of the residues. But no regulations exist to ensure that bottled water plants are set up in clean groundwater zones.
The study is important because of the implications for public health. Pesticides ingested in small quantities over time are known to have severe effects on the human immune system. What will it take for regulatory bodies to tighten controls? Should the bottled water industry be allowed to play havoc with public health and breach consumer trust? Scandals:
January 2003 Of birds and bacteria
"Superbugs" that resist the usual antibiotic treatments are nasty, and they could be in your chicken dinner. Here's how to protect yourself.
In the fall of 1997, almost three-fourths of the broilers that Consumer Reports bought in stores nationwide harbored salmonella or campylobacter--the bacteria most likely to give Americans food poisoning. Our new tests revealed contamination in about half of the chickens we analyzed, but there's a dark cloud within that silver lining. Many of the contaminated chickens harbored strains of salmonella and campylobacter that are resistant to antibiotics commonly used against those bugs, which can cause fever, diarrhea, and abdominal cramps. Illustration by Terry Miura As a result, the estimated 1.1 million or more Americans sickened each year by undercooked, tainted chicken, or by food that raw chicken juices have touched, may stay sick longer, possibly with more serious illnesses. Doctors may have to prescribe several antibiotics before finding one that works. And patients may have to pay more to be treated.
For what is, to our knowledge, the largest nationally representative analysis of antibiotic resistance in store-bought chicken, we tested 484 fresh, whole broilers bought at supermarkets and health-food stores in 25 cities nationwide last spring. Represented in our tests were 4 leading brands (Foster Farms, Perdue, Pilgrim's Pride, and Tyson), 14 supermarket brands, 9 premium brands (usually from smaller companies, usually more expensive, labeled as raised without antibiotics, and including free- range and organic brands), and 2 kosher brands.
Our shoppers packed the raw birds in coolers and shipped them overnight to a lab. There, tests determined whether salmonella and campylobacter were present, showed whether those bacteria were resistant to a range of human antibiotics, and measured the chickens' total plate count, an indicator of spoilage. Key findings:
Campylobacter was present in 42 percent of the chickens, salmonella in 12 percent. Five percent of all chickens had both campylobacter and salmonella; 51 percent had neither.
No major brand was less contaminated than others overall. Pilgrim's Pride had an exceptionally low incidence of salmonella but, along with Tyson, a higher incidence of campylobacter than most other brands.
All 12 samples from Ranger, a premium brand sold only in the Northwest, were free of campylobacter and salmonella. Ranger's chickens also had among the fewest bacteria that can cause spoilage. Ranger was the only brand that was clean across the board.
Ninety percent of the campylobacter bacteria tested from our chicken and 34 percent of the salmonella showed resistance to one or more antibiotics.
To see whose chickens harbored bacteria and how many of those bacteria remained unaffected by antibiotics, see How contaminated? How resistant?. We've also deciphered the claims you're likely to find on packages of chicken, including free-range, organic, and natural, in Behind the labels.
HOLES IN THE SAFETY NET
Since 1998, a federally mandated system called HACCP (pronounced hass-ip) has been the consumer's main protection against contaminated poultry, meat, and seafood. The initials stand for Hazard Analysis and Critical Control Points, and the system requires chicken producers to spell out where contamination might occur during processing, then build in procedures to prevent it.
After slaughter, for instance, chickens typically become contaminated with bacteria naturally found in their digestive tract, so processors spray carcasses inside and out with an approved disinfectant. Later, the birds are submerged in an icy wash that must chill them from about 100' F to below 40'.
U.S. Department of Agriculture (USDA) inspectors monitor HACCP plans and sit on production lines, rejecting carcasses that pass by with visible signs of illness or filth. They also test random samples for the presence of salmonella, but, unfortunately, not for campylobacter. Studies that could create a standard for campylobacter testing are under way, a USDA spokesman says, but no time frame has been set for putting tests in place.
According to the Centers for Disease Control and Prevention (CDC), there has been a significant reduction in major foodborne illnesses since HACCP was implemented. Still, the system has shortcomings. USDA inspectors at meat and poultry plants are failing to spot faults in HACCP plans, according to a report issued last August by the General Accounting Office, the government watchdog agency. The agency concluded that inspectors missed problems or, when they found them, didn't require quick corrections. "As a result," the report said, "consumers may be unnecessarily exposed to unsafe foods that can cause foodborne illnesses."
HACCP protections have become even more important with the discovery of chickens harboring antibiotic-resistant strains of campylobacter, salmonella, and enterococcus (a germ linked with deadly hospital-acquired infections).
Antibiotics--which may include, experts say, low doses of human drugs such as penicillin, erythromycin, and tetracycline--are given to chickens to prevent or reduce sickness and to speed growth. That practice is based on studies dating to the 1950s that showed animals given antibiotics reach their market weight faster, though perhaps only a day faster, than untreated animals.
When birds actually get sick, perhaps with respiratory disease from Escherichia coli picked up from their own droppings, they need full-strength antibiotics for a short time. Flocks are too big for veterinarians to treat individual birds, so all birds may receive antibiotics in their drinking water. These drugs kill not only the bacteria that cause chickens to become sick, but also some of the many other types of bacteria that normally live inside chickens. Their routine use in so many birds sets the stage for the evolution of drug-resistant microbes that multiply around chicken coops, each of which can hold up to 20,000 birds. Bacteria that survive drug treatment may eventually contaminate carcasses during slaughtering and processing. And if chicken isn't cooked thoroughly enough to kill those bacteria, they could end up on your dinner plate, then colonize your intestines.
Antibiotic-resistant bacteria can enter your system from an outside source, such as undercooked chicken, but bacteria that normally live inside you can also develop resistance--as a result, for example, of the overuse or misuse of prescription antibiotics.
In either case, once the bacteria are in you, they may stay. Some stay for a short time, causing acute illness; others live peacefully in your digestive tract only to cause hard-to-treat disease when transferred to the bloodstream or urinary tract. Danish researchers recently found that when healthy volunteers ate just one meal contaminated with antibiotic-resistant strains of the bacterium Enterococcus faecium that came from chicken or pork, the bug lingered in the volunteers' intestinal tracts for up to 14 days. Antibiotic-resistant E. faecium does not cause disease if confined to your intestines, but if it escapes into your bloodstream, say during surgery, it can be fatal.
Also disheartening is that resistance can be "catching." Certain bacteria tend to carry their resistance genes on circular strips of DNA, called plasmids, that can move to other bacteria, conferring resistance upon them as well. Antibiotic-resistant bacteria in undercooked chicken, for instance, could pass on their resistance to other bacteria already living in your intestines and make it hard to treat any infection those bacteria might eventually cause.
Although stronger-than-usual or extended doses of antibiotics might eventually kill the bugs in most people, resistant germs can be risky for the very young, the very old, and people with weakened immune systems.
THE ROOTS OF RESISTANCE
What the CDC would later call a growing threat to public health was suspected as early as 1952, when two University of California bacteriologists warned, according to an article in Scientific American, that "chicks raised on antibiotics may develop resistant bacteria and poison people who eat them." The suspicion was confirmed in 1998, when CDC researchers studied salmonella-tainted chickens and stool samples from people sickened by salmonella. They found strains of the bacterium resistant to the human antibiotic gentamicin, a drug routinely injected into chicken eggs to reduce the chance of bacterial contamination.
In May 1999, investigators in Minnesota published findings that revealed the presence of drug-resistant campylobacter in store-bought chicken. They also found that newer fluoroquinolone antibiotics, such as the anthrax drug ciprofloxacin (Cipro), had rapidly lost effectiveness against foodborne campylobacter infections in people.
Food and Drug Administration (FDA) investigators concluded in October 2000 that two fluoroquinolone drugs made specifically for animals had spawned drug-resistant campylobacter in chickens' intestinal tracts. One of the drugs was quickly pulled off the market by its maker. The FDA proposed to withdraw approval of the second drug for treating disease in poultry, but its maker, Bayer, has challenged the proposal. Hearings were ongoing as of last fall.
Last September, the agency announced a proposal that companies submitting animal drugs for FDA approval assess their potential to promote resistance in humans.
The Animal Health Institute, which represents manufacturers of animal drugs, says antibiotic resistance is a top concern. But it maintains that the use of antibiotics in food animals poses an extremely small risk to human health and that the increase of bacterial resistance to antibiotics in humans is largely the result of overreliance on antibiotics in human medicine.
A spokesman for the National Chicken Council, an industry group, notes that "a very large percentage" of antibiotics used in chickens are not closely related to any drugs used in humans. The council also points to data indicating that the overall usage of antibiotics in animals of all kinds has been declining since 1999.
Indeed, four of the biggest U.S. poultry producers recently announced that they have reduced their use of certain antibiotics. Last year, Tyson said it had "chosen to discontinue its previously minimal use" of fluoroquinolone antibiotics in broiler chickens. Perdue says it stopped using fluoroquinolones last year. Foster Farms says it stopped using them approximately five years ago and does not give other important human drugs to chickens except when they're sick. Pilgrim's Pride says it stopped using fluoroquinolones in October 2000.
Margaret Mellon, director of the food and environment program at the Union of Concerned Scientists, a nonprofit environmental group, applauds any cut in antibiotic use. "You don't ever want to use antibiotics where you don't need them," she says. "The rule in antibiotics is, if you use them you lose them." But Mellon points out that industry data don't provide specifics about antibiotic use and production that would be helpful in monitoring ways to prevent drug resistance. The government doesn't collect such data, either. "We know nothing," she says. "We are flying blind."
Moreover, although the use of fluoroquinolones may have tapered off, at least nine other antibiotics are approved for use in both chickens and humans, and some are used in substantial quantities. For example, the Union of Concerned Scientists estimates that more than 380,000 pounds of erythromycin are given to poultry every year to hasten growth and prevent disease.
Our tests support the need for continued concern.
WHAT WE FOUND
Overall, chicken had less bacterial contamination than in our 1997 study, but it was still far from pristine, and there was widespread antibiotic resistance in the bacteria.
Contamination. You need swallow just 15 to 20 salmonella bacteria, or about 500 campylobacter, to become ill. Both bugs can cause intestinal distress. Campylobacter can also cause serious complications, including meningitis, arthritis, and Guillain-Barré syndrome, a severe neurological disorder.
Of all the chickens we tested, 42 percent harbored campylobacter--down from 63 percent in our 1997 tests. Among big brands, incidence ranged from 34 percent, in Perdue, to 56 percent, in Tyson. Supermarket brands as a whole were in the middle of that range.
Twelve percent of all chickens harbored salmonella, as against 16 percent in 1997. Pilgrim's Pride had an extremely low incidence of salmonella: Only 1 percent of its chickens were contaminated. (Pilgrim's Pride was in the news for less laudable reasons last October, when a company it owns recalled more than 27 million pounds of cooked turkey and chicken deli meat. The meat was possibly contaminated with listeria bacteria.)
As a group, the premium chickens were not significantly more free of microbes than others. On average, 33 percent were contaminated with campylobacter; 12 percent with salmonella. That said, the five premium brands labeled organic or free-range had no salmonella, and one of those, the free-range Ranger, also had no campylobacter, at least in the 12 samples we tested. We wondered whether Ranger's birds were treated differently from most others, so, without revealing our results, we checked with Rick Koplowitz, chief executive officer of Draper Valley Farms, which raises Ranger chickens. His answer revealed no unusual HACCP steps that would have made those birds cleaner.
Both kosher brands represented in our tests, Empire and Rubashkin's Aaron's Best, had a relatively high incidence of salmonella: Five of 20 samples of Empire and 1 of 6 samples of Aaron's tested positive. The incidence of campylobacter in Empire's chickens was slightly lower than the average for all chickens. None of Aaron's chickens had campylobacter.
We're still pondering one interesting result from our tests: Of 97 chickens from three processing plants in the Southwest and sold under the Pilgrim's Pride or Tyson name, only one harbored salmonella. That could result, perhaps, from drier weather or different processes in the plants. In any case, a Southwestern origin didn't make a difference when it came to campylobacter.
Spoilage. As a check of freshness, we measured total plate count, testing chickens for a broad class of bacteria whose presence in large numbers can make foods smell or feel slimy, though they generally don't make you sick. Only 12 of the broilers we tested, or 2 percent, had a total plate count high enough to suggest they were almost spoiled. That's a bit better than in our 1997 study, when we found 5 percent of birds had nearly gone bad. The 12 in this study came from 6 different brands. Chickens from the premium brand Bell & Evans were relatively high in spoilage bacteria. It's possible that those birds stayed in the case too long: Some Bell & Evans birds we bought didn't have a sell-by date.
Antibiotic resistance. Despite the chicken producers' announcements and the premium-chicken label claims, antibiotic resistance is still a concern, especially in chickens harboring campylobacter.
Our tests showed that if you are sickened by one of those chickens, two commonly used antibiotics-- tetracycline, an older but still important drug used against germs from pneumonia to chlamydia, and erythromycin, an option for patients allergic to penicillin--may not help. In 66 percent of the campylobacter-contaminated chickens, the bacteria were resistant to tetracycline. In 20 percent, they were resistant to erythromycin.
Your chances of being cured by the usual doses of two fluoroquinolones, ciprofloxacin and ofloxacin, may also be limited. The latest figures from the FDA, reported in 2001, indicate that 11,477 Americans were infected in 1999 by fluoroquinolone-resistant campylobacter in chicken.
Antibiotic-resistant campylobacter appeared even in chickens from the two brands labeled "certified organic," Rosie and Springer Mountain Farms. That isn't as surprising as it might sound. Although antibiotics are not allowed in organic poultry, and farmers must demonstrate to organic certifiers that they have not been used, antibiotic-resistant bacteria are ubiquitous and can persist in the environment for years. In any case, we learned after our tests were finished that Springer Mountain Farms had taken the organic claim off its label.
In 19 percent of the chickens contaminated with salmonella, the bacteria were resistant to ampicillin, used against a dozen or more different bacterial infections. In 17 percent, bacteria were resistant to tetracycline.
Six salmonella-tainted samples from the two kosher-chicken companies showed no antibiotic resistance.
RECOMMENDATIONS Chicken becomes contaminated long before you put it in your shopping cart. For that reason, the first line of attack needs to be a change in food-safety policies. But because consumers are the last line of defense against unsafe food, we've also listed steps you can take.
What policymakers can do:
The government should require companies to monitor data on the use of antibiotics in food animals.
Congress should ban subtherapeutic uses of medically important drugs in poultry and other livestock.
The USDA should extend its food-safety program to include testing for campylobacter in poultry plants, should better train its inspectors to spot deficiencies, and should require speedy fixes.
What you can do:
Make chicken one of the last items you buy before heading to the checkout line.
Pick chicken that is well wrapped and at the bottom of the case, where the temperature should be coolest. Sell-by dates are not a perfect indicator of freshness. We found a few spoiled chickens with sell-by dates as far away as four to six days. If you can find a chicken with a sell-by date seven or more days away, buy it.
Place chicken in a plastic bag like those in the produce department, to keep its juices from leaking.
If you'll be cooking the chicken within a couple of days, store it at below 40' F. Otherwise, freeze it.
Thaw frozen chicken in a refrigerator or microwave oven, never on a counter. Leave it in its packaging and put it on a plate, so juices can't drip.
Separate raw chicken from other foods. Immediately after preparation, use hot, soapy water and paper towels to wash and dry your hands and anything you or raw chicken might have touched.
Cook chicken thoroughly to kill harmful bacteria. Whole chicken should be heated to 180' F, breasts to 170'. Use a thermometer; chicken that is no longer pink can still harbor bacteria.
Don't return cooked meat to the plate that held it raw. And don't use a sauce in which raw chicken has been marinating unless it has been brought to a rolling boil for at least a minute.
Refrigerate or freeze leftovers within two hours of cooking. FLORIDA TODAY Feb 7, 8:50 PM Girl, 14, battles rare illness she may have gotten from kiss By Corey Schubert
TITUSVILLE -- It was New Year's Eve in Fort Lauderdale and, in a festive moment, 14-year-old Shay Eadens shared a kiss with a boy. That innocent moment might have led to her catching a relatively rare disease that caused doctors to amputate three of her fingers, several fingertips and toes, and will keep her bound to a wheelchair for at least the next two years. Shay, who is being treated in a South Florida hospital, is no longer contagious with invasive meningococcal disease, a bacterial infection that restricts blood flow. But with its ability to be spread through kissing, sharing eating utensils or a simple sneeze from an infected carrier, public health officials in Brevard County have looked into the case to ensure there's no threat of a major outbreak on the Space Coast. After investigating the incident, officials found there's no need for residents to worry, said Barry Inman, epidemiologist for the Brevard County Health Department. "There's no likelihood of this becoming a concern in Brevard," he said, noting about two to four cases of the disease are reported in the county each year. Shay, who longs for the day she can return home to sleep in her own bed and spend time with friends, is among about 2,500 people of all ages -- or one in 1,000 people --throughout the nation affected by the disease. About 135 Floridians have the disease, which most often affects people who have deficiencies in their immune system, according to the Florida Bureau of Epidemiology. College students living in dormitories also are at a modestly increased risk. Symptoms usually occur within 2 to 10 days after exposure and can include sudden fever, intense headache, nausea, stiff neck, vomiting and a rash. Invasive meningococcal disease can be life-threatening if not properly treated within about 24 hours after symptoms occur, with a death rate as high as 15 percent, the state bureau said. Shay became seriously ill on Jan. 3 while staying with friends and was taken to Florida Medical Center in Fort Lauderdale, said family friend Linda Linogon of Titusville. The eighth-grader at Jackson Middle School in Titusville then was sent to receive specialized treatment at Joe DiMaggio Children's Hospital in Hollywood, said her mother, Kaisu Bagley, 45, of Titusville. "She flat-lined in the process of transporting her from one hospital to another" and suffered heart damage before being revived, Bagley said. "We're hoping the damage is not permanent." Since then, Shay has clung to her faith in God and her wish to return to school next year. "I'll be home in about a month and I'm looking forward to seeing everybody," said Shay, who plans to become a fashion designer. "My friends help me get through this," she said, adding several friends from Titusville have visited her in the hospital. About 25 percent or more of the nation's population may carry the causative organism for the disease -- neisseria meningitidis -- in their nasal passages and never be affected, Inman said. "Rarely does the disease affect anyone," Inman said. "I may be a carrier and you may be a carrier, but we don't need to run out and get vaccinated or treated for this, unless you know you've been exposed to someone who is affected by the disease." Invasive meningococcal disease is a bacterial infection that releases toxins that can shut down major organs, Inman said. This can lead to the loss of blood flow in fingers, toes and other body parts that may require amputation. Doctors already have removed three of Shay's fingers to the second knuckle, one toe and the tips of other fingers and toes, Bagley said. She has been treated with antibiotics, along with those who have come in contact with her since acquiring the disease, and will need to continue to take heart medication and undergo physical therapy for several years, Bagley said. This week, doctors will remove half of Shay's right foot, Bagley said. No other amputations appear to be needed. Shay's family said her strong will to battle the disease has been an inspiration. "She's my hero. She's a very brave young girl," said her aunt, Liisa Cull of Port St. John. "The doctors told us from the beginning that unless she was a fighter from within, she wouldn't make it." The Fort Lauderdale teen that Shay's family members think carried the disease and transmitted it to her was vaccinated shortly after Shay fell ill, Bagley said. He was not affected by any of the common symptoms, although two other Fort Lauderdale teens who were in contact with him also fell ill and have recovered after being vaccinated, she said. Public health investigators in Brevard informed officials at Shay's school about the incident, but found no related cases of the disease, Inman said. A vaccine is available through most area physicians, and in limited supply through the county's health department, to greatly lower the risk of acquiring invasive meningococcal disease, Inman said. However, the only people who may want to consider being vaccinated are those who soon plan to live in a college dormitory, Inman said. The best way to prevent the disease from occurring is by reducing the chance of direct droplet or saliva exposure through routine hygiene procedures, such as covering one's mouth while sneezing or coughing and by not sharing utensils, drinks and cigarettes, according to the Florida Bureau of Epidemiology. Location summary
Sector general information
Scandals:
U.S. SEIZES MORE HONEY TAINTED WITH ANTIBIOTIC February 5, 2003 Reuters WASHINGTON - The U.S. Food and Drug Administration was cited as saying on Wednesday that nearly 185,000 pounds of honey imports were seized in Texas because of contamination with a human antibiotic banned from U.S. food products. The containers of honey seized from Hoyts Honey Farm Inc. in Baytown, Texas contained traces of chloramphenicol, an antibiotic drug used by physicians as a last resort to treat life-threatening infections. The drug is not widely used because it can cause a disease known as aplastic anemia, in which the body's bone marrow stops making enough healthy blood cells. Chloramphenicol is prohibited in all U.S. food and animal feed products by the FDA. The seized honey was stored in 266 drums, each containing 639 pounds, and five totes, each weighing 3,000 pounds, the FDA said.