5 Communicable Disease Nursing
I. EPI DISEASES
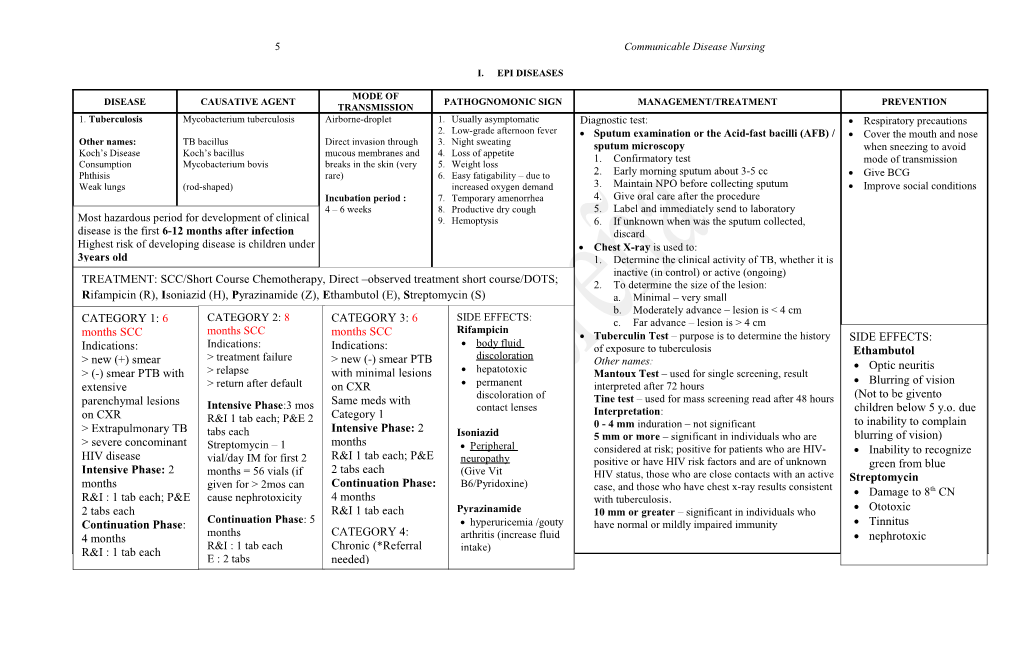
MODE OF DISEASE CAUSATIVE AGENT PATHOGNOMONIC SIGN MANAGEMENT/TREATMENT PREVENTION TRANSMISSION 1. Tuberculosis Mycobacterium tuberculosis Airborne-droplet 1. Usually asymptomatic Diagnostic test: Respiratory precautions 2. Low-grade afternoon fever Sputum examination or the Acid-fast bacilli (AFB) / Cover the mouth and nose Other names: TB bacillus Direct invasion through 3. Night sweating sputum microscopy when sneezing to avoid Koch’s Disease Koch’s bacillus mucous membranes and 4. Loss of appetite 1. Confirmatory test Consumption Mycobacterium bovis breaks in the skin (very 5. Weight loss mode of transmission Phthisis rare) 6. Easy fatigability – due to 2. Early morning sputum about 3-5 cc Give BCG Weak lungs (rod-shaped) increased oxygen demand 3. Maintain NPO before collecting sputum Improve social conditions Incubation period : 7. Temporary amenorrhea 4. Give oral care after the procedure 4 – 6 weeks 8. Productive dry cough 5. Label and immediately send to laboratory Most hazardous period for development of clinical 9. Hemoptysis 6. If unknown when was the sputum collected, disease is the first 6-12 months after infection discard Highest risk of developing disease is children under Chest X-ray is used to: 3years old 1. Determine the clinical activity of TB, whether it is inactive (in control) or active (ongoing) TREATMENT: SCC/Short Course Chemotherapy, Direct –observed treatment short course/DOTS; 2. To determine the size of the lesion: Rifampicin (R), Isoniazid (H), Pyrazinamide (Z), Ethambutol (E), Streptomycin (S) a. Minimal – very small b. Moderately advance – lesion is < 4 cm CATEGORY 1: 6 CATEGORY 2: 8 CATEGORY 3: 6 SIDE EFFECTS: c. Far advance – lesion is > 4 cm months SCC Rifampicin months SCC months SCC Tuberculin Test – purpose is to determine the history SIDE EFFECTS: Indications: body fluid Indications: Indications: of exposure to tuberculosis Ethambutol > treatment failure > new (-) smear PTB discoloration > new (+) smear Other names: Optic neuritis > (-) smear PTB with > relapse with minimal lesions hepatotoxic Mantoux Test – used for single screening, result Blurring of vision extensive > return after default on CXR permanent interpreted after 72 hours discoloration of (Not to be givento parenchymal lesions Same meds with Tine test – used for mass screening read after 48 hours Intensive Phase:3 mos contact lenses children below 5 y.o. due on CXR Category 1 Interpretation: R&I 1 tab each; P&E 2 to inability to complain > Extrapulmonary TB Intensive Phase: 2 0 - 4 mm induration – not significant tabs each Isoniazid blurring of vision) > severe concominant months 5 mm or more – significant in individuals who are Streptomycin – 1 Peripheral considered at risk; positive for patients who are HIV- Inability to recognize HIV disease R&I 1 tab each; P&E vial/day IM for first 2 neuropathy positive or have HIV risk factors and are of unknown green from blue Intensive Phase: 2 months = 56 vials (if 2 tabs each (Give Vit HIV status, those who are close contacts with an active Streptomycin months given for > 2mos can Continuation Phase: B6/Pyridoxine) case, and those who have chest x-ray results consistent Damage to 8th CN R&I : 1 tab each; P&E cause nephrotoxicity 4 months with tuberculosis. 2 tabs each R&I 1 tab each Pyrazinamide 10 mm or greater – significant in individuals who Ototoxic Continuation Phase: Continuation Phase: 5 hyperuricemia /gouty have normal or mildly impaired immunity Tinnitus months CATEGORY 4: 4 months arthritis (increase fluid nephrotoxic R&I : 1 tab each Chronic (*Referral R&I : 1 tab each intake) E : 2 tabs needed) 6 Communicable Disease Nursing
NATIONAL TB CONTROL PROGRAM: MANAGEMENTs OF CHILDREN WITH TUBERCULOSIS - for TB symptomatic children Vision: A country where TB is no longer a public health problem *a TB symptomatic child with either known or Mission: Ensure that TB DOTS Services are available, accessible, and Prevention: BCG immunization to all infants (EPI) unknown exposure to a TB case shall be referred affordable to the communities in collaboration with LGUs and others for tuberculin testing Goal: To reduce prevalence and mortality from TB by half by the year 2015 (Millennium Development Goal) Casefinding: * (+) contact but (-) tuberculin test and unknown Targets: 1. Cure at least 85% of the sputum smear (+) patients discovered - cases of TB in children are reported and identified in 2 contact but (+) tuberculin test shall be referred for 2. Detect at least 70% new sputum smear (+) TB cases instances: (a) patient was screened and was found symptomatic CXR examination Objectives: 1. Improve access to and quality of services of TB after consultaion (b) patient was reported to have been *(-) CXR, repeat tuberculin test after 3 months 2. Enhance stakeholder’s health-seeking behavior exposed to an adult TB patient * INH chemoprophylaxis for three months shall be 3. Increase and sustain support for TB control activities - ALL TB symptomatic children 0-9 y.o, EXCEPT sputum given to children less than 5y.o. with (-) CXR; after 4. Strengthen management of TB control activities at all levels positive child shall be subjected to Tuberculin testing (Note: which tuberculin test shall be repeated KEY POLICIES: Only a trained PHN or main health center midwife shall do *Case finding: tuberculin testing and reading which shall be conducted once a Treatment (Child with TB): - DSSM shall be the primary diagnostic tool in NTP case finding week either on a Monday or Tuesday. Ten children shall be Short course regimen - No TB Dx shall be made based on CXR results alone gathered for testing to avoid wastage. PULMONARY TB - All TB symptomatic shall be asked to undergo DSSM before treatment Intensive: 3 anti-TB drugs (R.I.P.) for 2 months - Only contraindication for sputum collection is hemoptysis - Criteria to be TB symptomatic (any three of the following:) Continuation: 2 anti-TB drugs (R&I) for 4 months - PTB symptomatic shall be asked to undergo other tests (CXR and culture), * cough/wheezing of 2 weeks or more only after three sputum specimens yield negative results in DSSM * unexplained fever of 2 weeks or more EXTRA-PULMONARY TB - Only trained med techs / microscopists shall perform DSSM * loss of appetite/loss of weight/failure to gain weight/weight Intensive: 4 anti-TB drugs (RIP&E/S) for 2 months - Passive case finding shall be implemented in all health stations faltering Continuation: 2 anti-TB drugs (R&I) for 10 months * failure to respond to 2 weeks of appropriate antibiotic therapy *Treatment: Domiciliary treatment – preferred mode of care for lower respiratory tract infection DSSM – basis for treatment of all TB cases * failure to regain previous state of health 2 weeks after a viral *Hospitalization is recommended: massive hemoptysis, pleural effusion, infection or exanthem (e.g. measles) military TB, TB meningitis, TB pneumonia, & surgery is needed or with complications *All patients undergoing treatment shall be supervised -Conditions confirming TB diagnosis (any 3 of the following:) *National & LGUs shall ensure provision of drugs to all smear (+) TB cases * (+) history of exposure to an adult/adolescent TB case *Quality of fixed-dose combination (FDC) must be ensured * (+) signs and symptoms suggestive of TB *Treatment shall be based on recommended category of treatment regimen * (+) tuberculin test * abnormal CXR suggestive of TB DOTS Strategy – internationally-recommended TB control strategy * Lab findings suggestive or indicative of TB Five Elements of DOTS: (RUSAS) Recording & reporting system enabling outcome assessment of all patients - for children with exposure to TB Uninterrupted supply of quality-assured drugs * a child w/ exposure to a TB registered adult patient shall Standardized SCC for all TB cases undergo physical exam and tuberculin testing Access to quality-assured sputum microscopy * a child with productive cough shall be referred for sputum Sustained political commitment exam, for (+) sputum smear child, start treatment immediately * TB asymptomatic but (+) tuberculin test and TB symptomatic but (-) tuberculin test shall be referred for CXR examination 7 Communicable Disease Nursing
2. Diphtheria Corynebacterium diphtheria Droplet especially Pseudomembrane – mycelia of Diagnostic test: DPT immunization secretions from mucous the oral mucosa causing Pasteurization of milk Types: Klebbs-loffler membranes of the nose formation of white membrane on Nose/throat swab Education of parents > nasal and nasopharynx and the oropharynx Moloney’s test – a test for hypersensitivity to diphtheria > pharyngeal – most from skin and other toxin common lesions Bull neck Schick’s test – determines susceptibility to bacteria > laryngeal – most Dysphagia fatal due to proximity Milk has served as a Dyspnea Drug-of-Choice: to epiglottis vehicle Erythromycin 20,000 - 100,000 units IM once only
Incubation Period: Complication: MYOCARDITIS (Encourage bed rest) 2 – 5 days 3. Pertussis Bordetella pertussis Droplet especially from Catarrhal period: 7 days Diagnostic: DPT immunization Hemophilus pertussis laryngeal and bronchial paroxysmal cough followed by Booster: 2 years and 4-5 years Whooping cough Bordet-gengou bacillus secretions continuous nonstop Bordet-gengou agar test Patient should be segregated until Tusperina Pertussis bacillus accompanied by vomiting after 3 weeks from the appearance No day cough Incubation Period: 7 – Management: of paroxysmal cough 10 days but not Complication: abdominal hernia 1. DOC: Erythromycin or Penicillin 20,000 - 100,000 units exceeding 21 days 2. Complete bed rest 3. Avoid pollutants (because if more than 21 4. Abdominal binder to prevent abdominal hernia days, the cough can be Incidence: highest under 7 years of age related to TB or lung Mortality: highest among infants (<6 months) cancer) 4.One Tetanus attack confers definiteClostridium and prolonged tetani – anaerobic Indirect contact – Risus sardonicus (Latin: “devil No specific test, only a history of punctured wound DPT immunization spore-forming heat-resistant and inanimate objects, soil, smile”) – facial spasm; sardonic Otherimmunity. names: Second attacklives occasionally in soil or intestine occurs street dust, animal and grin Treatment: Tetanus toxoid immunization Lock jaw human feces, punctured Antitoxin among pregnant women wound Opisthotonus – arching of back antitetanus serum (ATS) Neonate: umbilical cord tetanus immunoglobulin (TIG) Licensing of midwives Children: dental caries For newborn: Pen G Adult: punctured wound; after 1. Difficulty of sucking Diazepam – for muscle spasms Health education of mothers septic abortion Incubation Period: 2. Excessive crying Varies from 3 days to 1 3. Stiffness of jaw Note: The nurse can give fluid provided that the patient is able month, falling between 7 4. Body malaise to swallow. There is risk of aspiration. Check first for the gag – 14 days reflex 5. Poliomyelitis Legio debilitans Fecal – oral route Paralysis Diagnostic test: OPV vaccination Polio virus Muscular weakness Frequent hand washing Other name: Enterovirus Incubation period: 7 – Uncoordinated body movement CSF analysis / lumbar tap Infantile paralysis 21 days Hoyne’s sign – head lag after 4 Pandy’s test Attacks the anterior horn of the months neuron, motor is affected Management: Man is the only reservoir (!Safety) Rehabilitation involves ROM exercises 8 Communicable Disease Nursing
6. Measles RNA containing paramyxovirus Droplet secretions from 1. Koplik’s spots – No specific diagnostic test Measles vaccine nose and throat whitish/bluish pinpoint patches Disinfection of soiled articles Other names: on the buccal cavity Management: Isolation of cased from diagnosis Morbilli Incubation period: 10 2. cephalocaudal appearance of Supportive and symptomatic until about 5-7 days after onset of Rubeola days – fever maculopapular rashes rash 14 days – rashes appear 3. Stimson’s line – bilateral red line on the lower conjunctiva Period of Communicability: 4 days before and 5 days after the appearance of rash
7. Hepatitis B Hepatitis B virus Blood and body fluids 1. Right-sided Abdominal pain Diagnostic test: -Hepatitis B immunization Placenta 2. Jaundice -Wear protected clothing Other names: 3. Yellow-colored sclera Hepatitis B surface agglutination (HBSAg) test -Hand washing Serum Hepatitis Incubation period: 4. Anorexia -Observe safe-sex 45 – 100 days 5. Nausea and vomiting Management: -Sterilize instruments used in 6. Joint and Muscle pain > Hepatitis B Immunoglobulin minor surgical-dental procedures 7. Steatorrhea -Screening of blood products for 8. Dark-colored urine Diet: high in carbohydrates transfusion 9. Low grade fever Hepatitis A – infectious hepatitis; oral-fecal Hepatitis B – serum hepatitis; blood and body fluids Hepatitis C – non-A non-B, post-transfusion hepatitis; blood and body fluids Hepatitis D – Delta hepatitis or dormant hepatitis; blood and body fluids; needs past history of infection to Hepatitis B Hepatitis E – oral-fecal
II. DISEASES TRANSMITTED THROUGH FOOD AND WATER
MODE OF DISEASE CAUSATIVE AGENT PATHOGNOMONIC SIGN MANAGEMENT/TREATMENT PREVENTION TRANSMISSION 1. Cholera Vibrio cholera Fecal-oral route Rice watery stool Diagnostic Test: Proper handwashing Vibrio coma Stool culture Proper food and water sanitation Other names: Ogawa and Inaba bacteria 5 Fs Period of Communicability: Immunization of Chole-vac El tor 7-14 days after onset, Treatment: Incubation Period: occasionally 2-3 months Oral rehydration solution (ORESOL) Few hours to 5 days; IVF usually 3 days Drug-of-Choice: tetracycline (use straw; can cause staining of teeth) 2. Amoebic Dysentery Entamoeba histolytica Fecal-oral route Abdominal cramping Treatment: Proper handwashing Bloody mucoid stool Proper food and water sanitation Protozoan (slipper-shaped body) Tenesmus - feeling of Metronidazole (Flagyl) incomplete defecation * Avoid alcohol because of its Antabuse effect can cause 9 Communicable Disease Nursing
(Wikipedia) vomiting
3. Shigellosis Shigella bacillus Fecal-oral route Abdominal cramping Drug-of-Choice: Co-trimoxazole Proper handwashing Bloody mucoid stool Proper food and water sanitation Other names: Sh-dysenterae – most infectious 5 Fs: Finger, Foods, Tenesmus - feeling of Diet: Low fiber, plenty of fluids, easily digestible foods Fly control Bacillary dysentery Sh-flesneri – common in the Feces, Flies, Fomites incomplete defecation Philippines (Wikipedia) Sh-connei Incubation Period: Sh-boydii 1 day, usually less than 4 days 4. Typhoid fever Salmonella typhosa (plural, Fecal-oral route Rose Spots in the abdomen – Diagnostic Test: Proper handwashing typhi) due to bleeding caused by Typhi dot – confirmatory test; specimen is feces Proper food and water sanitation 5 Fs perforation of the Peyer’s Widal’s test – agglutination of the patient’s serum patches Incubation Period: Drug-of-Choice: Chloramphenicol Usual range 1 to 3 Ladderlike fever weeks, average 2 weeks 5. Hepatitis A Hepatitis A Virus Fecal-oral route Fever Prophylaxis: “IM” injection of gamma globulin Proper handwashing Headache Hepatitis A vaccine Proper food and water sanitation Other names: 5 Fs Jaundice Hepatitis immunoglobulin Proper disposal of urine and feces Infectious Hepatitis / Clay-colored stool Separate and proper cleaning of Epidemic Hepatitis / Incubation Period: Lymphadenopathy Complete bed rest – to decrease metabolic needs of liver articles used by patient Catarrhal Jaundice 15-50 days, depending Anorexia Low-fat diet; increase carbohydrates (high in sugar) on dose, average 20-30 days 6. Paralytic Shellfish Dinoflagellates Ingestion of raw of Numbness of face especially Treatment: 1. Avoid eating shellfish such as Poisoning (PSP I Red inadequately cooked around the mouth 1. No definite treatment tahong, talaba, halaan, tide poisoning) Phytoplankton seafood usually bivalve Vomiting and dizziness 2. Induce vomiting kabiya, abaniko during red mollusks during red tide Headache 3. Drink pure coconut milk – weakens the toxic effect tide season season Tingling sensation/paresthesia 4. Sodium bicarbonate solution (25 grams in ½ glass of 2. Don’t mix vinegar to shellfish and eventful paralysis of water) it will increase toxic effect 15 Incubation Period: hands Advised only in the early stage of illness because times greater 30 minutes to several Floating sensation and paralysis can lead to aspiration hours after ingestion weakness NOTE: Persons who survived the first 12 hours after ingestion Rapid pulse have a greater chance of survival. Dysphonia Dysphagia Total muscle paralysis leading to respiratory arrest and death
ROBERT C. REÑA, BSN 10 Communicable Disease Nursing
III. SEXUALLY TRANSMITTED DISEASES
MODE OF DISEASE CAUSATIVE AGENT PATHOGNOMONIC SIGN MANAGEMENT/TREATMENT PREVENTION TRANSMISSION 1. Syphilis Treponema pallidum Direct contact Primary stage: painless chancre Diagnostic test: Abstinence (a spirochete) Transplacental at site of entry Dark field illumination test Be faithful Other names: Buboes Fluorescent treponemal antibody absorption test – most Condom Sy Incubation Period: Condylomata reliable and sensitive diagnostic test for Syphilis Bad Blood 10 days to 3 months Gumma VDRL slide test, CSF analysis, Kalm test, The pox (average of 21 days) Wasseman test Lues venereal Morbus gallicus Primary and secondary sores will go even without treatment but the germs continue Treatment: Drug of Choice: Penicillin (Tetracycline if resistant to to spread throughout the body. Latent syphilis may continue 5 to 20+ years with NO Penicillin) 2. Gonorrhea symptoms,Neiserria gonorrheae but the person is NODirect longer contact infectious – genitals, to otherThick people purulent. A pregnantyellowish Diagnostic test: Abstinence mother can transmit the diseaseanus, to her mouth unborn child (congenitaldischarge syphilis). Culture of urethral and cervical smear Be faithful Other names: Burning sensation upon Gram staining Condom GC, Clap, Drip, Incubation Period: urination / dysuria Stain, Gleet, 2 – 10 days Treatment: Flores Blancas Drug of Choice: Penicillin 3. Trichomoniasis Trichomonas vaginalis Direct contact Females: Diagnostic Test: Abstinence white or greenish-yellow Culture Be faithful Other names: Incubation Period: odorous discharge Condom Vaginitis 4 – 20 days; average of 7 vaginal itching and soreness Treatment: Trich days painful urination Drug of Choice: Metronidazole (Flagyl) Personal Hygiene Males: Slight itching of penis Painful urination Clear discharge from penis 4. Chlamydia Chlamydia trachomatis Direct contact Females: Diagnostic Test: Abstinence (a rickettsia) Asymptomatic Culture Be faithful Incubation Period: Dyspareunia Condom 2 to 3 weeks for males; Fishy vaginal discharge Treatment: usually no symptoms for Drug of Choice: Tetracycline females Males: Burning sensation during urination Burning and itching of urethral opening (urethritis) 5. Candidiasis Candida albicans Direct contact White, cheese-like vaginal Diagnostic Test: Abstinence discharges Culture Be faithful Other names: Curd like secretions Gram staining Condom Moniliasis Candidosis Treatment: Nystatin for oral thrush Cotrimazole, fluconazole for mucous membrane and vaginal infection 11 Communicable Disease Nursing
Fluconazole or amphotericin for systemic infection
6. Acquired immune Retrovirus (Human Direct contact 1. Window Phase Diagnostic tests: Abstinence deficiency syndrome T-cell lymphotrophic virus 3 or Blood and body fluids a. initial infection Enzyme-Linked Immuno-Sorbent Assay (ELISA) Be faithful (AIDS) HTLV 3) Transplacental b. lasts 4 weeks to 6 months - presumptive test Condom c. not observed by present Western Blot – confirmatory Attacks the T4 cells: T-helper Incubation period: laboratory test (test should be Sterilize needles, syringes, and cells; T-lymphocytes, and CD4 3-6 months to 8-10 years repeated after 6 months) Treatment: instruments used for cutting lymphocytes 1. Treatment of opportunistic infection operations Variable. Although the 2. Acute Primary HIV 2. Nutritional rehabilitation time from infection to the Infection 3. AZT (Zidovudine) – retards the replication of Proper screening of blood donors development of a. short, symptomatic period retrovirus detectable antibodies is b. flu-like symptoms 4. PK 1614 - mutagen Rigid examination of blood and generally 1-3 months, the c. ideal time to undergo other blood products time from HIV infection screening test (ELISA) to diagnosis of AIDS has Avoid oral, anal contact and an observed range of less 3. Asymptomatic HIV swallowing of semen than 1 year to 15 years or Infection longer. a. with antibodies against HIV Avoid promiscuous sexual (PHN Book) but not protective contact b. lasts for 1-20 years depending upon factors HIV/AIDS Prevention and Control Program: 4. ARC (AIDS Related Complex) Goal: Contain the transmission of a. a group of symptoms HIV /AIDS and other indicating the disease is likely to reproductive tract infections and progress to AIDS mitigate their impact b. fever of unknown origin c. night sweats d. chronic intermittent diarrhea e. lymphadenopathy f. 10% body weight loss
5. AIDS a. manifestation of severe immunosuppression b. CD4 Count: <200/dL c. presence of variety of infections at one time:
oral candidiasis leukoplakia AIDS dementia complex Acute encephalopathy Diarrhea, hepatitis Anorectal disease 12 Communicable Disease Nursing
Cytomegalovirus Pneumonocystis carinii pneumonia (fungal) TB Kaposi’s sarcoma (skin cancer; bilateral purplish patches) Herpes simplex Pseudomonas infection Blindness Deafness
ROBERT C. REÑA, BS IV. ERUPTIVE DISEASES
MODE OF DISEASE CAUSATIVE AGENT PATHOGNOMONIC SIGN MANAGEMENT/TREATMENT PREVENTION TRANSMISSION 1. Chickenpox Human (alpha) herpes virus 3 Droplet spread Vesiculo-pustular rashes No specific diagnostic exam Case over 15 years of age should (varicella-zoster virus), a be investigated to eliminate Other names: member of the Herpesvirus Direct contact Centrifugal appearance of rashes Treatment is supportive and symptomatic; infection viral in possibility of smallpox. Varicella group origin, and therefore is self-limiting Report to local authority Indirect through articles Pruritus Isolation freshly soiled by discharges Drug-of-choice: Concurrent disinfection of throat of infected persons Acyclovir (orally to reduce the number of lesions; topically to and nose discharges Period of Communicability: lessen the pruritus) Exclusion from school for 1 Not more than one day before Incubation Period: week after eruption first appears and more than 6 days after 2-3 weeks, commonly 13 to Avoid contact with susceptibles appearance of the first crop of 17 days vesicles 2. German Measles Rubella virus or RNA- Droplet Forscheimer spots – red Diagnostic Test: MMR vaccine (live attenuated containing Togavirus pinpoint patches on the oral Rubella Titer (Normal value is 1:10) virus) Other Names: Incubation Period: cavity - Derived from chick embryo Rubella German measles is teratogenic Three (3) days Contraindication: Three-day Measles infection. Maculopapular rashes - Allergy to eggs Headache - If necessary, given in divided Low-grade fever Instruct the mother to avoid pregnancy for three months after or fractionated doses and Sore throat receiving MMR vaccine. epinephrine should be at the bedside. 3. Herpes Zoster Herpes zoster virus Droplet Painful vesiculo-pustular lesions Treatment is supportive and symptomatic Avoidance of mode of (dormant varicella zoster virus) Direct contact from secretion on limited portion of the body transmission Other names: (trunk and shoulder) Acyclovir to lessen the pain Shingles Cold sores Low-grade fever 4. Dengue Dengue virus 1, 2, 3, and 4 and Bite of infected mosquito Classification (WHO): Diagnostic Test: 4 o’clock habit Hemorrhagic Fever Chikungunya virus (Aedes Aegypti) Grade I: Torniquet test (Rumpel Leads Test / capillary fragility test) – Chemically treated mosquito net Other names: Period of communicability: Daytime biting a. flu-like symptoms PRESUMPTIVE; positive when 20 or more oetechiae per 2.5 Larva eating fish H-fever Unknown. Presumed to be on Low flying b. Herman’s sign cm square or 1 inch square are observed Environmental sanitation 13 Communicable Disease Nursing
the 1st week of illness up to Stagnant clear water c. (+) tourniquet sign Antimosquito soap when the virus is still present in Urban Platelet count – CONFIRMATORY; (Normal is 150 - 400 x Neem tree (eucalyptus) the blood Grade II: 103 / mL) Incubation Period: a. manifestations of Grade I plus Eliminate vector Occurrence is sporadic Uncertain. Probably 6 days to spontaneous bleeding Treatment: Avoid too many hanging clothes throughout the year 1 week b. e.g. petechiae, ecchymosis Supportive and symptomatic inside the house purpura, gum bleeding Paracetamol for fever Residual spraying with Epidemic usually occur during Manifestations: Analgesic for pain insecticide the rainy seasons (June to Grade III: November) First 4 days: a. manifestations of Grade II Rapid replacement of body fluids – most important treatment Febrile/Invasive Stage plus beginning of circulatory Peak months: September and - starts abruptly as fever failure ORESOL October - abdominal pain b. hypotension, tachycardia, - headache tachypnea Blood tansfusion - vomiting - conjunctival infection Grade IV: Diet: low-fat, low-fiber, non-irritating, non-carbonated. -epistaxis a. manifestations of Grade III Noodle soup may be given. ADCF (Avoid Dark-Colored plus shock (Dengue Shock Foods) 4th – 7th days: Syndome) Toxic/Hemorrhagic Stage ALERT! No Aspirin - decrease in temperature - severe abdominal pain - GIT bleeding - unstable BP (narrowed pulse pressure) - shock - death may occur
7th – 10th days: Recovery/Convalescent Stage - appetite regained - BP stable
ROBERT C. REÑA, BSN V. VECTOR-BORNE DISEASES
MODE OF DISEASE CAUSATIVE AGENT PATHOGNOMONIC SIGN MANAGEMENT/TREATMENT PREVENTION TRANSMISSION 1. Malaria Plasmodium Parasites: Bite of infected anopheles Cold Stage: severe, recurrent Early Diagnosis and Prompt Treatment *CLEAN Technique *Insecticide Vivax mosquito chills (30 minutes to 2 hours) Early diagnosis – identification of a patient with malaria as – treatment of mosquito net Falciparum (most fatal; most soon as he is seen through clinical and/or microscopic method *House Spraying (night time common in the Philippines) Night time biting Hot Stage: fever (4-6 hours) Clinical method – based on signs and symptoms of the patient fumigation) Ovale High-flying and the history of his having visited a malaria-endemic area *On Stream Seeding – Malariae Rural areas Wet Stage: Profuse sweating Microscopic method – based on the examination of the blood construction of bio-ponds for Clear running water smear of patient through microscope (done by the medical fish propagation (2-4 fishes/m2 - intermittent chills and technologist) for immediate impact; 200- 14 Communicable Disease Nursing
sweating 400/ha. for a delayed effect) - anemia / pallor QBC/quantitative Buffy Coat – fastest *On Stream Clearing – cutting of - tea-colored urine Malarial Smear – best time to get the specimen is at height of vegetation overhanging along - malaise fever because the microorganisms are very active and easily stream banks - hepatomegaly identified - splenomegaly *Avoid outdoor night activities - abdominal pain and Chemoprophylaxis (9pm – 3am) enlargement Only chloroquine should be given (taken at weekly intervals *Wearing of clothing that covers - easy fatigability starting from 1-2 weeks before entering the endemic area). In arms and legs in the evening pregnant women, it is given throughout the duration of *Use mosquito repellents pregnancy. *Zooprophylaxis – typing of NURSING CARE: domestic animals like the 1. TSB (Hot Stage) Treatment: carabao, cow, etc near human 2. Keep patent warm (Cold Blood Schizonticides - drugs acting on sexual blood stages of dwellings to deviate mosquito Stage) the parasites which are responsible for clinical manifestations bites from man to these animals 3. Change wet clothing (Wet 1. QUININE – oldest drug used to treat malaria; from Stage) the bark of Cinchona tree; ALERT: Cinchonism – Intensive IEC campaign 4. Encourage fluid intake quinine toxicity 5. Avoid drafts 2. CHLOROQUINE 3. PRIMAQUINE 4. FANSIDAR – combination of pyrimethamine and sulfadoxine 2. Filariasis Wuchereria bancrofti Bite of Aedes poecillus Asymptomatic Stage: Diagnosis CLEAN Technique Brugia malayi (primarily) Presence of microfilariae in the Physical examination, history taking, observation of major and Other names: Brugia timori Aedes flavivostris blood but no clinical signs and minor signs and symptoms Use of mosquito repellents Elephantiasis (secondary) symptoms of disease Anytime fumigation – nematode parasites Laboratory examinations Wear a long sleeves, pants and Endemic in 45 out of Incubation period: Acute Stage: Nocturnal Blood Examination (NBE) – blood are taken from socks 78 provinces 8 – 16 months Lymphadenitis the patient at his residence or in hospital after 8:00 pm Lymphangitis Immunochromatographic Test (ICT) – rapid assessment Highest prevalence Affectation of male genitalia method; an antigen test that can be done at daytime rates: Regions 5, 8, 11 and CARAGA Chronic Stage: (10-15 years Treatment: from onset of first attack) Drug-of-Choice: Diethylcarbamazine Citrate (DEC) or Hydrocele Hetrazan Lymphedema Elephantiasis
3. Shistosomiasis Schistosoma mansoni Contact with the infected Diarrhea Diagnostic Test: Dispose the feces properly not S. haematobium freshwater with cercaria and Bloody stools COPT or cercum ova precipitin test reaching body of water Other Names: S. japonicum (endemic in the penetrates the skin Enlargement of abdomen Use molluscides Snail Fever Philippines) Splenomegaly Treatment: Prevent exposure to Bikharziasis Vector: Oncomelania Hepatomegalu Drug-of-Choice: PRAZIQUANTEL (Biltracide) contaminated water (e.g. use Quadrasi Anemia rubber boots) Endemic in 10 regions weakness Oxamniquine for S. mansoni Apply 70% alcohol immediately and 24 provinces Metrifonate for S. haematobium to skin to kill surface cercariae Allow water to stand 48-72 15 Communicable Disease Nursing
High prevalence: hours before use Regions 5, 8, 11
ROBERT C. REÑA, BSN REFERENCES: THE ROYAL PENTAGON REVIEW SPECIALISTS, INC NOTE-TAKING GUIDE FOR COMMUNICABLE DISEASE NURSING by DANIEL JOSEPH E. BERDIDA, RM, RN CHAPTER VII: COMMUNICABLE DISEASE PREVENTION and CONTROL, PUBLIC HEALTH NURSING IN THE PHILIPPINES, 10th EDITION DEPARTMENT OF HEALTH OFFICIAL WEBSITE: www.doh.gov.ph CENTERS FOR DISEASE CONTROL AND PREVENTION (CDC) OFFICIAL WEBSITE: www.cdc.gov
VI. DISEASES TRANSMITTED BY ANIMALS
MODE OF DISEASE CAUSATIVE AGENT PATHOGNOMONIC SIGN MANAGEMENT/TREATMENT PREVENTION TRANSMISSION 1. Leptospirosis Leptospira interrogans – Through contact of the skin, Leptospiremic Phase Diagnosis Protective clothing, boots and bacterial spirochete especially open wounds with - leptospires are present in Clinical manifestations gloves Other Names: water, moist soil or blood and CSF Culture of organism - Weil’s Disease RAT is the main host. Although vegetation infected with urine - onset of symptoms is abrupt Examination of blood and CSF during the first week of illness Eradication of rats - Mud Fever pig, cattle, rabbits, hare, skunk, of the infected host - fever and urine after the 10th day - Trench Fever and other wild animals can also - headache Leptospira agglutination test Segregation of domestic animals - Flood Fever serve as reservoir Incubation Period: - myalgia - Spirochetal 7-19 days, average of 10 days - nausea Treatment: Awareness and early diagnosis Jaundice Occupational disease affecting - vomiting Penicillins and other related B-lactam antibiotics - Japanese Seven veterinarians, miners, farmers, - cough Tetracycline (Doxycycline) Improved education of people Days fever sewer workers, abattoir workers, - chest pain Erythromycin etc Immune Phase - correlates with the appearance of circulating IgM 2. Rabies Rhabdovirus of the genus Bite or scratch (very rare) of Sense of apprehension Diagnosis: Have pet immunized at 3 lyssavirus rabid animal Headache history of bite of animal months of age and every year Other Names: Fever culture of brain of rabid animal thereafter Lyssa Degeneration and necrosis of Non-bite means: leaking, Sensory change near site of demonstration of negri bodies Hydrophobia brain – formation of negri bodies scratch, organ transplant animal bite Never allow pets to roam the Le Rage (cornea), inhalation/airborne Spasms of muscles of Management: streets Two kinds of Rabies: (bats) deglutition on attempts to *Wash wound with soap immediately. Antiseptics e.g. a. Urban or canine – transmitted Source of infection: saliva of swallow povidone iodine or alcohol may be applied Take care of your pet by dogs infected animal or human Fear of water/hydrophobia *Antibiotics and anti-tetanus immunization Paralysis *Post exposure treatment: local wound treatment, active National Rabies Prevention b. Sylvatic – disease of wild Incubation period: Delirium immunization (vaccination) and passive immunization and Control Program animals and bats which 2 – 8 weeks, can be years Convulsions (administration of rabies immunoglobulin) Goal: Human rabies is sometimes spread to dogs, cats, depending on severity of *Consult a veterinarian or trained personnel to observe the pet eliminated in the Philippines and and livestock wounds, site of wound as “FATAL once signs and for 14 days the country is declared rabies- distance from brain, amount symptoms appear” free of virus introduced, and *Without medical intervention, the rabies victim would protection provided by usually last only for 2 to 6 days. Death is often due to 16 Communicable Disease Nursing
clothing respiratory paralysis. 3. Bubonic Plague Bacteria (Yersinia pestis) Direct contact with the Fever and lyphadenitis Streptomycin, tetracycline, chloramphenicol Environmental Sanitation infected tissues of rodents Vector: rat flea
VII. DISEASES OF THE SKIN
MODE OF DISEASE CAUSATIVE AGENT PATHOGNOMONIC SIGN MANAGEMENT/TREATMENT PREVENTION TRANSMISSION 1. Leprosy Mycobacterium leprae Airborne-droplet Early signs: Diagnostic Test: Avoid prolonged skin-to-skin Change in skin color – either reddish or Slit Skin Smear - determines the presence of M. leprae; contact Other names: Prolonged skin-to-skin white optional and done only if clinical diagnosis is doubtful to BCG vaccination – practical Hansenosis contact Loss of sensation on the skin lesion prevent misclassification and wrong treatment and effective preventive Hansen’s disease Loss of sweating and hair growth Lepromin Test – determines susceptibility to leprosy measure against leprosy Thickened and painful nerves Good personal hygiene -an ancient disease Muscle weakness or paralysis or Treatment: Adequate nutrition and is a leading cause extremities Ambulatory chemotherapy through use of MDT Health education of permanent physical Pin and redness of the eyes Domiciliary treatment as embodied in RA 4073 which disability among the Nasal obstruction or bleeding advocates home treatment communicable Ulcers that do not heal diseases PAUCIBACILLARY (tuberculoid and indeterminate); Late Signs: noninfectious type Madarosis Duration of treatment: 6 to 9 months Loss of eyebrows Procedure: Inability to close eyelids Supervised: Rifampicin and Dapsone once a month on the (lagophthalmos) health center supervised by the rural health midwife Clawing of fingers and toes Self-administered: Dapsone everyday at the client’s house Contractures Chronic ulcers MULTIBACILLARY (lepromatous and borderline); infectious Sinking of the nosebridge type Enlargement of the breast Duration of treatment: 24-30 months (gynecomastia) Procedure: Supervised: Rifampicin, Dapsone, and Lamprene (Clofazimine) once a month on the health center supervised by the rural health midwife Self-administered: Dapsone and Lamprene everyday at the client’s house 17 Communicable Disease Nursing
2. Anthrax Bacillus anthracis Contact with 1. Cutaneous form – most common Treatment: Penicillin Proper handwahing a. tissues of animals - itchiness on exposed part Other names: (cattle, sheep, goats, - papule on inoculation site Immunize with cell-free Malignant pustule horses, pigs, etc.) dying - papule to vesicle to eschar vaccine prepared from culture Malignant edema Incubation period: of the disease - painless lesion filtrate containing the protection Woolsorter disease few hours to 7 days most b. biting flies that had antigen Ragpicker disease cases occur within 48 hours partially fed on such 2. Pulmonary form – contracted from Charbon of exposure animals inhalation of B. anthracis spores Control dust and proper c. contaminated hair, - at onset, resembles common URTI ventilation wool, hides or products - after 3-5 days, symptoms become made from them e.g. acute, with fever, shock, and death drums and brushes d. soil associated with 3. Gastrointestinal anthrax – infected animals or contracted from ingestion of meat from contaminated bone meal infected animal used in gardening - violent gastroenteritis - vomiting - bloody stools
3. Scabies Sarcoptes scabiei Direct contact with Itching Diagnosis: Personal hygiene - An itch mite infected individuals Appearance of the lesion Avoid playing with dogs parasite When secondarily infected: Intense itching Laundry all clothes and iron Incubation Period: Skin feels hot and burning Finding of causative mite Maintain the house clean 24 hours Environmental sanitation When large and severe: fever, headache, Treatment: (limited entirely to the skin) Eat the right kind of food and malaise Examine the whole family before undertaking treatment Regular changing of clean Benzyl benzoate emulsion (Burroughs, Welcome) – cleaner to clothing, beddings and towels use and has more rapid effect Kwell ointment
4. Pediculosis Pediculosis Direct contact Itchiness of the scalp Kwell shampoo (twice a week) Proper hygiene Capitis (head lice) Other name: Corporis (body lice) Common in school age One tbsp water + one tbsp vinegar Phthipiasis Pubis (crab lice)
VIII. INTESTINAL PARASITISM 18 Communicable Disease Nursing
MODE OF DISEASE CAUSATIVE AGENT PATHOGNOMONIC SIGN MANAGEMENT/TREATMENT PREVENTION TRANSMISSION 1. Ascariasis Ascaris lumbricoides Fecal-oral route Pot-bellied Diagnostic Test: Fecalysis Proper handwahing Voracious eater Other names: (nematode) 5 Fs: Finger, Foods, Feces, Thin extremities Treatment: Roundworm Flies, Fomites Antihelminthic: Mebendazole / Pyrantel Pamoate Giant worms 2. Taeniasis Taenia solium – pork Eating inadequately cooked Muscle soreness Diagnostic Test: Fecalysis Proper handwahing Taenia saginata – beef pork or beef Scleral hemorrhage Other name: Dyphyllobotruim latum – fish Treatment: Cook pork and beef adequately Tape worm 5 Fs: Finger, Foods, Feces, Antihelminthic: Mebendazole / Pyrantel Pamoate Flies, Fomites
3. Capillariasis Trichuris trichuria Eating inadequately cooked Abdominal pain Diagnostic Test: Fecalysis Proper handwahing seafood Diarrhea Other name: Capillararia Philippinensis borborygmi Treatment: Cook seafoods adequately Whip worm 5 Fs: Finger, Foods, Feces, Antihelminthic: Mebendazole / Pyrantel pamoate Flies, Fomites 4. Enterobiasis Enterobium vermicularis Inhalation of ova Nocturnal anal itchiness Diagnostic Test: Fecalysis / tape test Proper handwahing Toilet seat Other name: Infected bedsheets Treatment: Proper disinfection of beddings Pinworm Antihelminthic: Mebendazole / Pyrantel pamoate 5 Fs: Finger, Foods, Feces, Flies, Fomites 5. Ancyloclos- Ancyclostoma duodenal Walking barefooted Dermatitis Diagnostic Test: Fecalysis Proper handwahing tomiasis Necatur americanus 5 Fs: Finger, Foods, Feces, Anemia Treatment: Avoid walking barefooted Other name: Flies, Fomites Antihelminthic: Mebendazole / Pyrantel pamoate Hookworm Black fishy stool ROBERT C. REÑA, BSN
IX. OTHER COMMUNICABLE DISEASES
MODE OF DISEASE CAUSATIVE AGENT PATHOGNOMONIC SIGN MANAGEMENT/TREATMENT PREVENTION TRANSMISSION 1. Pneumonia Bacteria: Droplet Rusty sputum Diagnosis: Avoid mode of transmission Pneumococcus, streptococcus Fever and chills Based on signs and symptoms Types: pneumoniae, staphylococcus Incubation Period: Chest pain Dull percussion on affected lung Build resistance a. Community aureus, Klebsiella pneumonia 2 – 3 days Chest indrawing Sputum examination – confirmatory Acquired Pneumonia (Friedlander’s bacilli) Rhinitis/common cold Chest x-ray Turn to sides (CAP) Productive cough b. Hospital / Virus: Fast respiration Management: Proper care of influenza cases Nosocomial Haemophilus influenzae Vomiting at times Bedrest c. Atypical Convulsions may occur Adequate salt, fluid, calorie, and vitamin intake Fungi: Pneumonocystis carinii Flushed face Tepid sponge bath for fever pneumonia Dilated pupils Frequent turning from side to side 19 Communicable Disease Nursing
Highly colored urine with Antibiotics based on CARI of the DOH reduced chlorides and increased urates Oxygen inhalation Suctioning Expectorants / mucolytics Bronchodilators Oral/IV fluids CPT 2. Mumps Mumps virus, a member of Direct contact Painful swelling in front of the Supportive and symptomatic MMR vaccine family Paramyxoviridae ear, angle of the jaws and down Other name: Source of infection: the neck Sedatives – to relieve pain from orchitis Isolate mumps cases Epidemic Parotitis Secretions of mouth and nose Fever Cortisone – for inflammation Malaise Incubation Period: Loss of appetite Diet: Soft or liquid as tolerated 12 to 26 days, usually 18 days Swelling of one or both testicles (orchitis) in some boys Support the scrotum to avoid orchitis, edema, and atrophy
Dark glasses for photophobia 3. Influenza Influenza virus Direct contact Sudden onset Supportive and symptomatic Avoid use of common towels, A – most common Droplet infection or by Fever with chills glasses, and eating utensils Other name: B – less severe articles freshly soiled with Headache Keep patient warm and free from drafts Cover mouth and nose during La Grippe C – rare nasopharyngeal discharges Myalgia / arthralgia TSB for fever cough and sneeze Airborne Boil soiled clothing for 30 minutes before laundering Period of Communicability: Probably limited to 3 days from Incubation Period: clinical onset Short, usually 24 – 72 hours 4. Streptococcal sore Group A beta hemolytic Droplet Sudden onset Diagnosis: Avoid mode of transmission throat streptococcus High grade fever with chills Throat swab and culture Complication: Enlarged and tender cervical Other name: Other diseases: Rheumatic Heart Disease lymph nodes Treatment: erythromycin Pharyngitis Scarlet fever Inflamed tonsils with Tonsillitis St. Anthony fire mucopurulent exudates Care: Puerperal sepsis Headache Bed rest Imoetigo dysphagia Oral hygiene with oral antiseptic or with saline gargle (1 glass Acute glumerulonephritis of warm water + 1 tsp rock salt) Rheumatic Heart Disease Ice collar 5. Meningitis Meningococcus Direct (Droplet) A. Sudden Onset Diagnostic Test: Respiratory Isolation Neisseria meningitides - high fever accompanied by Other name: Incubation Period: chills Lumbar puncture or Lumbar tap - reveals CSF WBC and Cerebrospinal fever 2 - 10 days - sore throat, headache, protein, low glucose; contraindicated for increased ICP for prostration (collapse) danger of cranial herniation
B. entrance into the bloodstream Hemoculture – to rule out meningococcemia leading to septicemia (meningococcemia) Treatment: a. rash, petchiae, purpura Osmotic diuretic (Mannitol) – to reduce ICP and relieve cerebral edema; Alert: fastdrip to prevent crystallization 20 Communicable Disease Nursing
C. Symptoms of menigeal Anti-inflammatory (Dexamethasone) – to relieve cerebral irritation edema - nuchal rigidity (stiff neck) – Antimicrobial (Penicillin) earliest sign Anticonvulsany (Diazepam / Valium) - Kernig’s sign – when knees are flexed, it cannot be extended - Brudzinski signs – pain on Complications: neck flexion with automatoc Hydrocephalus flexion of the knees Deafness (Refer the child for audiology testing) and mutism - convulsion Blindness - poker soine (poker face / flat affect) - Increased ICP (Cushing’s triad: hypertension, bradycardia, bradypnea) and widening pulse pressure
IX. KILLER DISEASES OF THE NEW MILLENNIUM
MODE OF DISEASE CAUSATIVE AGENT PATHOGNOMONIC SIGN MANAGEMENT/TREATMENT PREVENTION TRANSMISSION 1. Meningococcemia Neisseria meningitides Direct contact with High grade fever in the first Respiratory isolation within 24 hours Universal precaution respiratory droplet from 24 hours Chemoprophylaxis nose and throat of infected Hemorrhagic rash – Drug-of-Choice: Penicillin Proper hand washing individuals petechiae nuchal rigidity Incubation Period: Kernig’s sign 2 – 10 days Brudzinski sign Shock Death 2. Severe Acute Coronavirus Close contact with Prodromal Phase: No specific treatment Utilize personal protective Respiratory Syndrome respiratory droplet Fever (>38 0C) equipment (N95 mask) / SARS secretion from patient Chills PREVENTIVE MEASURES and CONTROL Malaise 1. Establishment of triage Handwashing Earliest case: Incubation Period: Myalgia 2. Identification of patient Guangdong Province, 2 – 10 days Headache 3. Isolation of suspected probable case Universal Precaution China in November Infectivity is none to low 4. Tracing and monitoring of close contact The patient wears mask 2002 5. Barrier nursing technique for suspected and Isolation Respiratory Phase: probable case Global outbreak: March Within 2-7 days, dry 12, 2003 nonproductive cough progressing to respiratory First case in the distress Philippines: 21 Communicable Disease Nursing
April 11, 2003
3. Bird Flu Influenza Virus H5N1 Contact with infected birds Fever Control in birds: Isolation technique Body weakness and body 1. Rapid destruction (culling or stamping out of all Vaccination Other Name: Incubation Period: malaise infected or exposed birds) proper disposal of carcasses Proper cooking of poultry Avian Flu 3 days, ranges from 2 – 4 Cough and quarantining and rigorous disinfection of farms days Sore throat 2. Restriction of movement of live poultry Dyspnea Sore eyes In humans: 1. Influenza vaccination 2. Avoid contact with poultry animals or migratory birds 4. Influenza A (H1N1) Influenza Virus A H1N1 Exposure to droplets from - similar to the symptoms of Diagnostic: - Cover your nose and mouth the cough and sneeze of regular flu such as Nasopharyngeal (throat) swab when coughing and sneezing Other Name: This new virus was first the infected person Fever Immunofluorescent antibody testing – to distinguish - Always wash hands with Swine Flu detected in people in Headache influenza A and B soap and water April 2009 in the United Influenza A (H1N1) is not Fatigue - Use alcohol- based hand May 21, 2009 – first States. transmitted by eating Lack of appetite sanitizers confirmed case in the thoroughly cooked pork. Runny nose Treatment: - Avoid close contact with Philippines Influenza A (H1N1) is Sore throat Antiviral medications may reduce the severity and sick people fatal to humans The virus is killed by Cough duration of symptoms in some cases: - Increase your body's June 11, 2009 - The cooking temperatures of - Vomiting or nausea Oseltamivir (Tamiflu) resistance WHO raises its 160 F/70 C. - Diarrhea or zanamivir - Have at least 8 hours of Pandemic Alert Level to sleep Phase 6, citing Incubation Period: - Be physically active significant transmission 7 to 10 days - Manage your stress of the virus. - Drink plenty of fluids - Eat nutritious food
ROBERT C. REÑA, BSN