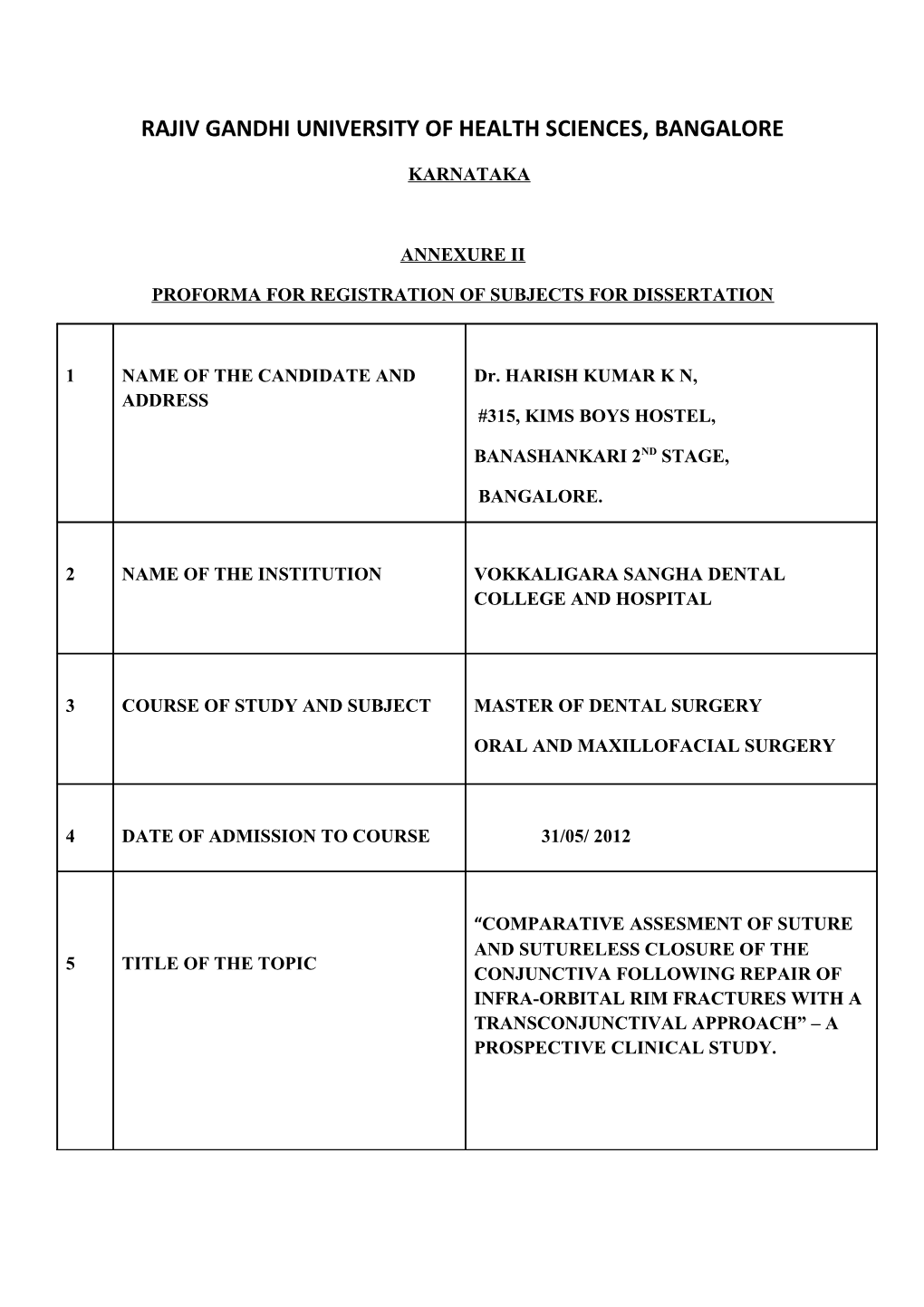
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, BANGALORE
KARNATAKA
ANNEXURE II
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
1 NAME OF THE CANDIDATE AND Dr. HARISH KUMAR K N, ADDRESS #315, KIMS BOYS HOSTEL,
BANASHANKARI 2ND STAGE,
BANGALORE.
2 NAME OF THE INSTITUTION VOKKALIGARA SANGHA DENTAL COLLEGE AND HOSPITAL
3 COURSE OF STUDY AND SUBJECT MASTER OF DENTAL SURGERY
ORAL AND MAXILLOFACIAL SURGERY
4 DATE OF ADMISSION TO COURSE 31/05/ 2012
“COMPARATIVE ASSESMENT OF SUTURE AND SUTURELESS CLOSURE OF THE 5 TITLE OF THE TOPIC CONJUNCTIVA FOLLOWING REPAIR OF INFRA-ORBITAL RIM FRACTURES WITH A TRANSCONJUNCTIVAL APPROACH” – A PROSPECTIVE CLINICAL STUDY. 6 BRIEF RESUME OF THE INTENDED WORK
6.1 NEED FOR STUDY:
In treatment of fractures of the infraorbital rim the choice regarding the approach to the infraorbital rim and the placement of incision is guided by the need to achieve adequate intraoperative visibility, minimal postoperative scar formation and good aesthetic results. A variety of surgical approaches to the infraorbital rim exist and can be conveniently categorized as transcutaneous or transconjunctival.
Although it may seem that the difference lies only at the level of the incision from the ciliary margin, the anatomy of the region and the plane of dissection and closure of the surgical incision also influences the final aesthetic result
The aim of the study is to compare the aesthetic results, and complications in patients treated for infraorbital rim fractures by different closure methods of the transconjunctival approach.
6.2 REVIEW OF LITERATURE:
Katherine A lane et al reported on the surgical outcome of patients who had undergone orbital fracture repair without conjunctival closure. They concluded Forgoing closure of the periorbita and conjunctiva after transconjunctival orbital floor and rim fracture repair was associated with a low incidence of postoperative complications. This technique was applicable in the repair of both isolated floor fractures and complex orbital fractures.1
Ralph E Wesley stated that the transconjunctival approach provides a entire wide access to orbit without surface scars as compared to limitation of producing a noticeable scar associated with lower lid retraction that is often permanent and generally caused by skin approaches.2 Lulz carlos Manganello souza et al, reported on the use of transconjunctival approach in patients who had sustained ZMC fractures. They stated that direct access to orbital floor, zygomatic fractures infraorbital rim and zygomaticofrontal and zygomaticotemporal sutures is better with the transconjunctival approach along with better aesthetic results.3
Rowland et al studied 26 cases of isolated orbital floor fractures repaired by a sutureless closure technique in which Repair of the orbital floor blowout fractures with a nonfixed implant through the transconjunctival approach was done. They concluded that sutureless closure provides an excellent functional and cosmetic result.4
Kakibuchi et al studied 12 cases of fresh blowout fractures involving the orbital floor which were treated with a combined transconjunctival and endonasal – transantral approach. They concluded that endonasal endoscopic repair of the orbital floor combined with a conjunctival incision appears to be safe and effective technique for the treatment of blowout fractures involving the orbital floor.5
Fred G Fedok studied 51 patients of facial fractures necessitating orbital exploration and repair and concluded from his studies that even though commonly reported problems of transconjunctival approach such as ectropion, entropion, scleral show, chemosis, diplopia and eyelids tears/ laceration are there, the complication rate is much lower when compared with a transcutaneous route.6
A Salgerelli, P Bellini et al did a comparative study of different approaches in the treatment of orbital trauma in 274 cases. They concluded that a transconjunctival approach without canthotomy was the most successful surgical approach for the treatment of isolated fracture. Of the orbital floor; however when major surgical exposure is necessary, a subciliary incision is recommended.7 OBJECTIVES OF THE STUDY:
6.3 1. To assess the postoperative complications associated with suture and sutureless closure of the conjunctiva with a transconjunctival approach for treatment of infraorbital rim fractures.
2. To compare the aesthetic outcome of the incision at intervals of 15 days, 1 month and 3 months after surgery using the suture and sutureless method of closure of the conjunctiva.
MATERIALS AND METHODS:
7.0
7.1 SOURCES OF DATA:
The study will be conducted on patients with fractures of infraorbital rim reporting to the department of Oral and Maxillofacial Surgery, Vokkaligara Sangha Dental College and Hospital, Bangalore.
7.2 METHOD OF COLLECTION OF DATA
SAMPLE SIZE : 20 Patients STUDY DESIGN : Randomized Controlled Study STUDY DURATION : One and a half years. 7.3 INCLUSION CRITERIA:
Patients with fractures of the infraorbital rim.
Age group between 15-65 years
7.4 EXCLUSION CRITERIA:
Patients with communited fracture of the infraorbital rim.
Patients with extensive soft tissue injury in the periorbital region
METHODOLOGY :
1. 20 patients with fractures of the infraorbital rim who fulfil the selection criteria are selected.
2. Patients are then informed about the approach and the possible side effects of the approach and a written consent is obtained from them.
3. 20 random numbers are generated from a random sampling table and they are then alternatively assigned into two groups.
Group 1: closure with sutures
Group 2: approximation of conjunctiva and no usage of sutures for closure.
4. The patients are then asked to choose from the 20 random numbers, depending upon the number they choose; they are divided into the above stated groups.
5. Group 1 patients are treated using the transconjunctival approach and closure of surgical site with sutures while in Group 2 patients are treated using the transconjunctival approach but closure is performed with just approximation of the conjunctiva and no usage of sutures. 6. The following will be assessed:
Assessment of Incidence of postoperative complications, including orbital implant exposure, infection, entropion, ectropion and scleral show.
The assessment of aesthetic outcome of the incision site at intervals of 15 days, 1 month and 3 months after surgery.
STATISTICAL ANALYSIS: The data collected will be analyzed statistically by using descriptive statistics like mean, standard deviation and percentage.
The association between the above mentioned complications and the two approaches will be tested using chi-square test.
7.5 DOES THE STUDY REQUIRE ANY INVESTIGATIONS OR OTHER INTERVENTION TO BE CONDUCTED ON PATIENTS OR HUMANS OR ANIMALS? IF SO PLEASE DESCRIBE BRIEFLY.
Yes, investigations are required:
1. Paranasal sinus view & Sub mento vertex radiograph
2. Routine blood investigations
3. Routine investigations needed to get medical clearance for the surgery
7.6 HAS THE ETHICAL CLEARENCE BEEN OBTAINED FROM YOUR
INSTITUTION?
YES
8.0 LIST OF REFERENCES:
1. Katherine A. Lane, Jurij R. Bilyk,, Daniel Taub, Edmund A. Pribitkin: “Sutureless” Repair of Orbital Floor and Rim Fractures.Ophthalmology 2009;116:135–138.
2. Ralph E Wesley Transconjunctival approaches to lid and orbit. JOMS;56:66-69
3. Lulz carlos et al Transconjunctival approach to zygomatic and orbital floor fractures.Int J Oral Maxillofacial Surgery 1997; 26:31-34..
4. Ho VH, Rowland JP Jr, Linder JS, Fleming JC. Sutureless transconjunctival repair of orbital blowout fractures. Ophthal Plast Reconstr Surg 2004; 20:458–60.
5. M. Kakibuchi, K. Fukazawa, K. Fukuda, N. Yamada, K. Matsuda, K. Kawai,S. Tomofuji, M. Sakagami. Combination of transconjunctival and endonasal-transantral approach in the repair of blowout fractures involving the orbital floor. The British Association of Plastic Surgeons 2004; 57: 37–44.
6. Fred G. Fedok .The Transconjunctival Approach in the Trauma Setting: Avoidance of Complications. American journal of otolaryngology 1996; 17:16-21.
7. Salgarelli AC, Bellini P, Landini B, Multinu A, Consolo U. “A Comparative Study of Different Approaches in the Treatment of Orbital Trauma: An Experience Based On 274 Cases”. Oral Maxillofacial Surgery. 2010; 14:23-27. 9 Remarks of the guide
10 Signature of Student
11 Name and Designation of Dr. Keerthi R.
11.1 Guide. Professor Dept. of Oral Maxillofacial Surgery.
11.2 Signature.
11.3 Co –Guide.
11.4 Signature.
Dr. Madan Nanjappa. 11.5 Head of the Department. Professor and H O D. Dept. of Oral Maxillofacial Surgery.
11.6 Signature.
12 12.1 Remarks of the Chairman and Principal.
12.2 Signature. CONSENT FORM
I______son/daughter of______aged resident of______being under the treatment of Dr. Harish Kumar K N, do here by give consent to the performance of drugs / medical /surgical / anesthesia /diagnostic procedure of
______upon myself. The procedure has been explained to me in my own language and also the likely adverse effects of the treatment being used has been explained and I agree that no responsibility will be attached to the surgeon or the hospital staff.
Place:
Date : Signature of the patient / relative