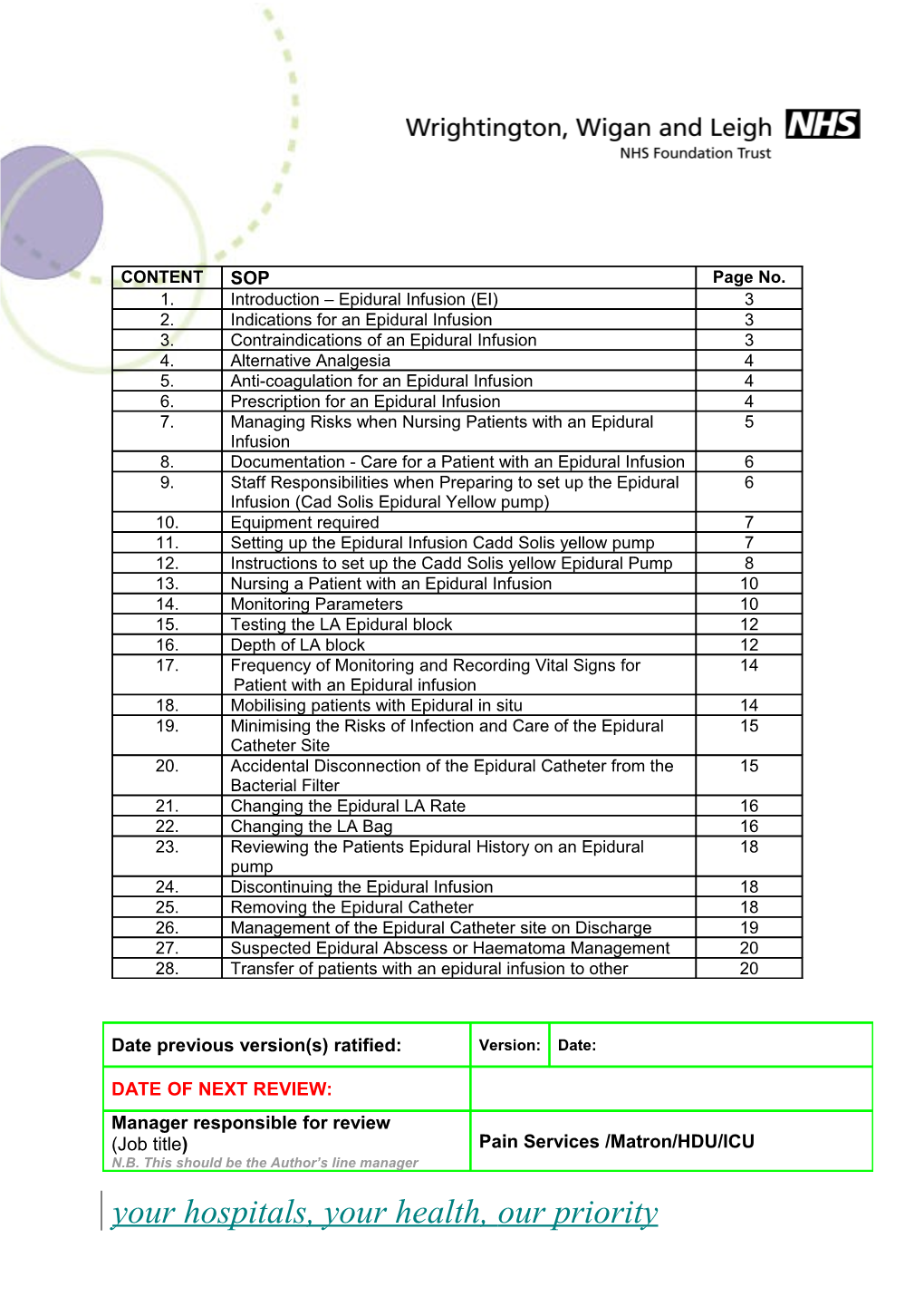
CONTENT SOP Page No. 1. Introduction – Epidural Infusion (EI) 3 2. Indications for an Epidural Infusion 3 3. Contraindications of an Epidural Infusion 3 4. Alternative Analgesia 4 5. Anti-coagulation for an Epidural Infusion 4 6. Prescription for an Epidural Infusion 4 7. Managing Risks when Nursing Patients with an Epidural 5 Infusion 8. Documentation - Care for a Patient with an Epidural Infusion 6 9. Staff Responsibilities when Preparing to set up the Epidural 6 Infusion (Cad Solis Epidural Yellow pump) 10. Equipment required 7 11. Setting up the Epidural Infusion Cadd Solis yellow pump 7 12. Instructions to set up the Cadd Solis yellow Epidural Pump 8 13. Nursing a Patient with an Epidural Infusion 10 14. Monitoring Parameters 10 15. Testing the LA Epidural block 12 16. Depth of LA block 12 17. Frequency of Monitoring and Recording Vital Signs for 14 Patient with an Epidural infusion 18. Mobilising patients with Epidural in situ 14 19. Minimising the Risks of Infection and Care of the Epidural 15 Catheter Site 20. Accidental Disconnection of the Epidural Catheter from the 15 Bacterial Filter 21. Changing the Epidural LA Rate 16 22. Changing the LA Bag 16 23. Reviewing the Patients Epidural History on an Epidural 18 pump 24. Discontinuing the Epidural Infusion 18 25. Removing the Epidural Catheter 18 26. Management of the Epidural Catheter site on Discharge 19 27. Suspected Epidural Abscess or Haematoma Management 20 28. Transfer of patients with an epidural infusion to other 20
Date previous version(s) ratified: Version: Date:
DATE OF NEXT REVIEW: Manager responsible for review (Job title) Pain Services /Matron/HDU/ICU N.B. This should be the Author’s line manager your hospitals, your health, our priority Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date hospital sites 29. Human rights Act 20 30. Accessibility Statement 20 Appendix App 1 Reference 22 App 2 Epidural Infusions Nursed in Side Rooms 23 App 3 Epidural Infusion Care Plan and Nursing Documentation 24 -25 App 4 Epidural Infusion Record 26 -29 App 5 Bromage Scale 30 App 6 Epidural Competence Form 31
1. Introduction - Epidural Infusion (EI)
2 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date 1.1 An epidural infusion is the delivery into the epidural space, of a weak solution of local anaesthetic with/without an opioid to provide segmental (dermatomal) pain relief, ideally without the loss of other sensations or movement to relieve pain. In addition to the continuous epidural infusion there is the facility for the patient to press a patient bolus button to administer a top-up bolus dose if required, at pre- set intervals. This is Patient Controlled Epidural Analgesia (PCEA).
1.2 Any health care professional (HCP) caring for a patient who requires an epidural infusion must have undertaken epidural infusion training by the pain service. This includes epidural pump management and patient monitoring.
2. Indications for an Epidural Infusion 2.1 Analgesia following surgery.
2.2 Thoracic surgery, vascular surgery, upper/lower abdominal surgery and major lower limb surgery.
2.3 Chest trauma i.e. fractured ribs.
2.4 Acute ischemic limb pain.
2.5 Palliative care.
2.6 Pain in Labour.
3. Contraindications of an Epidural Infusion 3.1 Absolute contraindications:
3.1.1 Patient refusal.
3.1.2 Raised intracranial pressure.
3.1.3 Infection at the site of puncture.
3.2 Relative contraindications/caution are:
3.2.1 Hypovolaemia or shock.
3.2.2 Coagulopathy, thrombocytopaenia and full anticoagulation. (Patients with a Platelet count less than 80 need reviewing by senior Anaesthetist, Obstetrician, and possibly haematologist).
3.2 Caution Only 3.2.1 Meticillin-resistant staphylococcus aureus (MRSA.
3.2.2 Pre-existing neurological conditions.
3.2.3 Generalised sepsis.
4. Alternative Analgesia The anaesthetist would normally discuss alternative analgesic methods prior to any procedure.
3 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date 5. Anti-coagulation for an Epidural Infusion 5.1 The patient’s coagulation status must be considered prior to insertion or removal of an epidural catheter. Non Steroid Anti-inflammatory Drugs (NSAID) and Aspirin are not considered significant risk factors for Epidural haematoma.
5.2 Patient on Prophylactic Low Molecular Weight Heparin (Fragmin®, Clexane®): Last dose should be at least 12 hours prior to insertion or removal. Do not recommence heparin until 4 hours after epidural catheter removal or insertion.
5.3 Patient on Treatment Dose Low Molecular Weight Heparin (LMWH) (Fragmin®, Clexane®): Last dose of LMWH should be at least 24 hours prior to insertion or removal. Do not recommence until 4 hours after epidural catheter removal.
5.4 Patients on Intra Venous (IV) Heparin: Stop heparin for 4 hours and measure Activated Partial Thromboplastin Time (APTT). Aim for APPT < 40 prior to insertion or removal. Do not recommence until 4 hours after epidural catheter removal.
5.5 Patients on Clopidogrel and similar potent antiplatelet drugs: Last dose at least 7 days before insertion of epidural. Note:- If patient on drug for coronary artery stenting then risk/benefit analysis on an individual patient basis may result in the 7 day rule being relaxed. Do not recommence until 6 hours after epidural catheter removal.
5.6 Patients on Warfarin: Stop 6 days prior to insertion. Convert to LMWH. International Normalised Rate (INR) should be < 1.5 prior to insertion or removal of epidural catheter.
5.7 Patients on Other Oral Anticoagulants (e.g. Fondaparinux, Dabigatran, Rivaroxaban, Apixaban, Edoxaban): Evidence relatively sparse and renal function critical to timing; last dose at least 48 hrs before insertion of epidural (except dabigatran – up to 96 hrs). Consult with a Haematologist if renally impaired or unsure of specific drug issues. Wait 6 hours after epidural catheter removal before recommencing anticoagulation.
5.8 Patients who have received Thrombolytic Drugs (example:- Altepase, Streptokinase): No epidural for 10 days after administration. Wait for 10 days after epidural catheter removal before administration.
6. Prescribing for an Epidural Infusion 6.1 The anaesthetist must use E-prescribing when requiring an epidural infusion.
6.2 Pre-mixed solution of:
Bupivacaine Fentanyl Bag Size 0.1% 2mcg/ml 250ml and 500ml 0.125% NONE 250MLS 0.15% NONE 500ml
4 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date
6.4 Infusion rates:- 6.4.1 GENERAL Theatre ONLY - Surgical/Trauma patients:
Catheter above T10 0 - 15mls/hour Catheter at or below T10 0 - 20mls/hour Bolus dose/Lockout 2mls /20mins Bolus dose facility for patients recommended. 4 hourly maximum dose limit 100mls
6.4.2 OBSTETRIC patients:
Catheter at or below T10 0 - 10mls/hour Bolus dose/Lockout 5mls /20mins Bolus dose facility for patients recommended. 4 hourly maximum dose limit 100mls
6.5 Fentanyl epidural infusion bags must be kept as per Controlled Drug Trust Procedure (locked cupboard).
6.6 Patient Controlled Epidural Analgesia (PCEA) bolus facility is recommended for this technique, and should not be omitted without justification.
6.7 If the patients pain scoring 2 then infusion rate may be increased in 2ml increments.
6.8 Maximum epidural infusion rate (including bolus) will not exceed 25mls/hr (100ml 4 hours).
6.9 The anaesthetist will prescribe oxygen for patients with an epidural infusion which contains Fentanyl (Oxygen 2L via nasal route) until the epidural is discontinued.
6.10 However, some obstetric patients may not require routine oxygen therapy.
6.11 Oxygen prescription may change if the patient has respiratory disease.
7. Managing Risks when Nursing Patients with an Epidural Infusion 7.1 All patients with an epidural infusion should be nursed on wards/theatre within Wrightington, Wigan and Leigh Foundation Trust (WWL) where full epidural training has been undertaken.
7.2 Patients must always be under the close supervision of a nurse, Operation Department Practitioner (ODP) or midwife competent in the management of continuous epidural infusions and able to be with the patient within seconds of being summoned (BPS 2004). This requires at least one such person is available on the ward at all times throughout the 24-hour period with an increase determined by the number of patients and patient dependency levels. There must be 24-hour availability of staff competent to recognise and manage the more serious complications of a continuous epidural infusion.
5 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date
7.3 It is the nurse/midwife responsibility to change the epidural infusion rates and epidural solutions (bags) as necessary, using Aseptic Not Touch Technique (ANTT).
7.4 It is not advisable routinely to nurse patients in a side-room but should be within a designated bay with appropriate monitoring equipment available.
7.5 If a patient requires a side room due to infection control precautions one to one nursing must be arranged by the ward manger or a Datix completed (Appendix 2).
8. Documentation - Care of a patient with an Epidural Infusion 8.1 Modified Early Warning Score (MEWS) chart - records the patient vital signs.
8.2 This must be used in conjunction with the Epidural Nursing Care Pathway (Appendix 3) and the patient’s Epidural Infusion Record (Appendix 4), to monitor/record the epidural’s effects on the patient’s vital signs, frequency of recordings and local anaesthetic (LA) efficacy. This chart also includes:- Sedation score, Pain score, PONV, Motor/Sensory block level, infusion volume and rate, total MEWs score, Pressure area care, epidural site check.
8.4 The chart also provides the scales used for monitoring patient’s scores and frequency of recording these.
8.5 Two signatures are required on the patient’s epidural infusion care pathway at hand over. This is to ensure that the epidural infusion program/rate/prescription are correct.
9. Staff Responsibilities When Preparing to set up the Epidural Infusion (Cadd Solis Epidural Yellow Pump) 9.1 Prior to setting up a epidural infusion staff must attend the Epidural training course for Epidural pump setup.
9.2 The staff must have an Epidural pump set up competencies form signed (see appendix 6).
9.3 This training must be up dated annually
9.4 The responsible for this training must be on the staff working in that area were epidurals are used regularly.
9.5 Only Anaesthetic/ODP/Recovery/Maternity trained staff to set up epidural yellow Cadd Solis.
9.6 Epidural catheters should ideally be inserted in a clean environment (Theatres, ICU/HDU and Delivery suite) although in exceptional circumstances it may be necessary to perform this technique in other areas.
10. Equipment Required 10.1 Yellow epidural pump, bolus button and pump lock box.
10.2 Batteries x 4 AA and check for any signs of leakage.
6 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date
10.3 Electric designated Power pack cable.
10.4 x1 Yellow Cad Solis epidural giving set.
10.5 LA bag of solution.
10.6 x1 Epidural line labels.
10.7 Prescription label for epidural infusion.
10.8 Sterile gloves.
10.9 Patient’s drug board.
10.10 Epidural care pathway (Epidural pump number to be recorded) and setting up details
10.11 Place batteries in pump and place pump in to the lockable plastic box.
11. Setting up an Epidural Infusion (Cad Solis yellow) pump
Wash and dry hands
Prepare clean area to set up Cadd Solis yellow epidural pump.
This is to reduce risks of infection/contamination of LA and giving set (epidurals may run for longer than 48hrs if required and continue with the closed circuit till discontinued).
1st person wash and dry hands and puts on sterile gloves.
2ND person washes and dries hands using ANTT, opens the sterile yellow epidural pump giving set and places it on sterile glove pack (keep tubing in the sterile field).
2nd person opens LA bag by cleaning the entry port on the LA bag using a sterett pad prior to removal of the foil seal.
1st person with sterile gloves takes the opened epidural giving set and spikes the prescribed LA bag.
1st person loads the epidural cassette in to the yellow epidural pump keeping the end of the giving set in the sterile field.
To lock cassette into position lift the silver lever upwards. Do not lock with key at this stage. Insert the epidural pump into lock box and clip down into place.
Close and Lock, ensuring the tubing is not trapped.
7 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date 12. Instructions to set up Cadd Solis yellow Epidural Pump Turn on epidural yellow PRESS Grey button pump (Check self-test (right side of the pump) is clear on the screen To ensure pump is and information is functioning correctly correct) Screen displays Do you want to start a new PRESS Yes or No patient Screen displays Enter CODE 130 to continue PRESS Accept value Screen displays Select Therapy Options are: WARNING- Z Maternity PRESS- up or down arrows Lumbar epidural configuration different to main to select prescribed therapy Thoracic epidural Theatres patients Scroll up or down arrows to Z Maternity select therapy Screen displays Screen qualifier PRESS - bag volume by Option :250mls or 500mls scrolling up or down (arrows reservoir bags to select LA solution) Screen displays Select drug PRESS - select button by 0.1% Bupivacaine +2mcg scrolling up or down Fentanyl (arrows) to select prescribed 0.125% Bupivacaine LA solution Screen displays Are these correct? PRESS -Yes or No Screen shows the requested therapy qualifier, drug and units Screen displays Programming Screen displays Review programme settings PRESS - Review Screen displays Full configuration of prescribed therapy Continuous rate PCA Dose PCA Lockout 4hourly limit Scroll down to see Reservoir volume Scroll back up to continuous PRESS - select rate( this becomes highlighted using the up and down in white to enable the rate to arrows to adjust the rate) be programmed at the prescribed rate) Don t save or Save PRESS - Save Screen displays Screen displays Green arrow to continuous rate PRESS - Accept value (Pump then automatically scrolls down to the next therapy) Screen displays PCA dose highlights in white PRESS - Accept value box Green tick appears next to 2mls PCA dose (Pump then automatically scrolls down to the next therapy)
8 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date Screen displays PCA lockout highlights in white PRESS - accept value box Green tick appears next to 20minutes the PCA lockout (Pump then automatically scrolls down to the next therapy) Screen displays 4hourly limit highlights in one PRESS - accept value box Green tick appears next to 100mls the 4hourly limit (Pump then automatically scrolls down to the next therapy) Screen displays Reservoir volume highlights in PRESS – accept value the white box Green tick appears next to 250mls/500mls. reservoir volume Screen displays Bottom of screen Review complete PRESS – NEXT highlighted in blue Screen displays Prime tubing? PRESS Yes or No Screen displays Disconnect the tubing from PRESS - Prime patient open clamps Screen displays Amount primed PRESS – STOP PRIMING In blue screen displays TO END Observe for droplets of LA solution at the end of the giving set Screen displays Continue priming PRESS - Yes/No(once priming complete PRESS No) Screen displays Start Pump PRESS Yes/No Screen displays Cassette not locked, Lock PRESS YES (ONLY when cassette with grey key before the ANESTHETIST has starting pump (lock found on connected the epidural right side of pump) giving set to the patient’s epidural catheter.)
Screen displays Epidural patient prescribed Press - YES Epidural pump therapy will automatically start to deliver epidural infusion Screen displays Top line information is highlighted in GREEN Pump running If epidural pump is not PRESS - NO connected to the patient Epidural infusion to be connected only by the ANAESTHETIST in theatre, as soon as possible to reduce risks of error, infection and delayed analgesia. Screen displays Start pump? PRESS - the red and green button (stop and start
9 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date button) on the bottom left side of the epidural pump. The pump will automatically start to deliver Epidural infusion. All epidural catheters All epidural catheters MUST To help prevent must be secured with a be secured (anchored) with disconnection of the filter. suitable dressing which gauze and tape onto the allows visual patient’s chest inspection of the insertion site.
13. Nursing a Patient with an Epidural infusion 13.1 Only epidural trained medical staff administers epidural bolus top-up doses.
13.2 The epidural filter must be securely anchored to the front of the patient’s chest (place a small gauze under the filter to prevent pressure) and tape down. This is to ensure that a closed circuit is maintained and the risk of accidental discontinuation is reduced.
13.3 Intravenous fluids must be maintained until the epidural infusion is no longer required.
13.4 Surgical patients will require a urinary catheter whilst the epidural infusion is in situ.
13.5 However some obstetric patients may not require a urinary catheter.
14. Monitoring Parameters 14.1 Vital signs, Sedation score, Pain score, PONV, Motor/Sensory block levels, Site check, MEWs score and Pressure area care.
14.2 Monitoring parameters.
Monitoring Rationale Value Action parameters Airway Sedation Airway compromised Check airway to ensure due to sedation patent (opioid epidural See further advice below infusion) Breathing Sedation Less 8 Give O2 via facemask at respirations/minute 15L Call ward doctor or maternity doctor or On call Anaesthetist Ensure IV Naloxone is available on the ward Circulation Hypovolemia Systolic BP less Give O2 Via facemask 90mmHg Infuse 500mls Gelofusine Ensure IV Ephedrine available Elevate legs but DO NOT put head down
10 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date Sympathetic effect of Call ward LA blockade doctor/APS/Maternity on call Anaesthetist Give O2 via facemask Ensure IV Atropine available. Call ward doctor/APS/Maternity on (Obstetric Pulse less than call Anaesthetist Foetal heart rate) 45/minute (bradycardia) Nausea and Fentanyl can cause Unpleasant Follow PONV algorithm vomiting emesis experience (See Appendix 4 ) Increased pain and discomfort Slow Recovery, can cause dehydration
Itching Fentanyl may cause Unpleasant Contact ward doctor for histamine release experience Piriton Loss of sleep Slow recovery Dizziness Fentanyl may also Unpleasant sensation Record vital signs ensure cause light headiness, Unsteady mobilisation normal parameters. tiredness, altered gait. Risk of falls Discuss with Pain team to change epidural LA solution
Urinary Motor block may Ensure urinary Contact ward doctor, retention cause urinary catheter is insitu May require addition retention due to LA. Observe patency of fluids the catheter Document urinary out May require a put diuretic/review hydration (minimum 30mls per hour) Motor block Increased motor block Bromage scale is the 1st sign of (see appendix 5 paralysis which may and information be due to intrathecal below) migration of the epidural catheter.
If the block level is higher Motor/Sensory Increased motor block than T6 STOP the block may be due to the epidural infusion, sit the epidural rate of LA too patient up (only if BP at high, or intrathecal normal parameter) migration of the Contact the Pain Team epidural catheter. or ward doctor or On call Paralysis may occur maternity anaesthetist should an epidural (Out of hours 9.00 17.00
11 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date abscess or contact the critical care haematoma develop. service).
Level of block Block level should not Reduce epidural rate by rise above T6 (see Level of block should 2mls per hour dermatome man cover the site of Increase frequency of diagram nursing pain/surgery monitoring block density. monitoring care If density does not pathway appendix 3) reduce in 2 hours contact the pain service or ward doctor (Out of hours contact the On call anaesthetist for theatres or maternity)
Reduced recovery Density of Affect compliance of block Risk of pressure sores physiotherapy Unpleasant sensation Epidural site Risk of Maintain effective 4 hourly inspection of infection/bleeding/leak analgesia epidural dressing/site age or accidental unless clinically indicated dislodgement due to more frequently ineffective dressing
15. Testing the LA Epidural Block 15.1 Sensory block (Afferent function). Pinprick and cold are most commonly used, but mechanical stimuli such as touch, skin pinch, and pressure can be used. Generally, loss of sensation to cold occurs before pinprick, and both of these before touch. Temperature perception is lost before pinprick, this is generally at a higher level, and is usually assessed by the application of ‘cold’ using alcohol skin prep, ice, or ethyl chloride spray.
15.2 Motor or autonomic block (Efferent function). A block which extends to a progressive impairment of motor as well as sensory function. The commonest method of assessment is the modified Bromage scale.
Level Definition 0 No motor block – full flection of knees and feet. 1 Partial block – just able to move knees. 2 Almost complete block – able to move feet only. 3 Complete block – unable to move feet or knees.
15.3 This provides information on both the spread and degree of motor block in the lumbar sacral distribution. Complete inability to straight leg raise (Bromage grade 3) implies the LA block has reached the high lumbar region (Appendix 5).
15.4 Test Method for block level.
15.5 Explain to the patient what and why you are spraying a cold spray on their body. Ask for permission to do this.
12 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date 15.6 The ethyl chloride spray is for use on the skin only. It is applied by a healthcare professional. Do not apply to broken skin or mucous membranes (e.g., inside the nose or mouth). Do not spray into the eyes. Do not inhale the spray.
15.7 This medication is flammable. Do not use near an open flame or near electrical equipment that can spark a fire.
15.8 If using ethyl chloride in an aerosol can, it should be held upright and sprayed onto the area for a few seconds. Your healthcare professional will spray just until the skin starts to turn white, stopping before the skin frosts. The numbing effect of ethyl chloride only lasts for a few seconds to a minute.
15.9 A small spot spray is sprayed first onto the arm to show to the patient how cold it feels and afterwards at different 2-3 levels, starting with one leg and continue to the upper chest to evaluate which dermatomes are affected by the LA.
15.10 Ask the patient each time if it feels as cold as when tested on the arm first (see dermatome diagram in epidural nursing care plan). This test should be done on both sides.
15.11 Upper and lower levels of sensory blocks are tested on conscious, co-operative patients by spraying a small spot spray and asking if they feel cold at the point of contact.
15.12 The patient will not appreciate any temperature change at the level of the epidural block but will appreciate cold above and below this area. The epidural chart provides details of dermatome levels to assist with determining the sensory block height.
15.13 Rationale: Increasing sensory block or an inappropriately high sensory block can indicate that the epidural catheter migration into the subarachnoid space. Sympathetic blockade, T1 – T4 may result in significant hypotension and bradycardia.
16. Depth of LA block 16.1 A good LA epidural block is one which covers both ends of the incision site and does not affect the motor function.
16.2 Provides effective pain relief on movement (so the patient can move around the bed/mobilise/comply with physiotherapy).
16.3 Does not cause the patient to be too sleepy (Fentanyl).
16.4 Does not make the patient nauseated/vomit (Low BP/Fentanyl).
16.5 The patient is asked to tell the nurse what they feel when the cold spray is given.
16.6 If the LA spray cannot be felt the LA block is too heavy and the epidural rate needs to be decreased (x2mls per hour – check patients drug board epidural prescription).
16.7 Document this on the epidural nursing care plan.
13 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date 16.8 Then re-evaluate the LA block level after an hour.
16.9 If the block level does not reduce after turning it down a second time – contact the ward doctor/pain team/On call anaesthetist. (See section 27 - Epidural Haematoma/abscess).
17. Frequency of Monitoring and Recording Vital Signs for Patient with an Epidural Infusion
Monitoring frequency vital signs Record 0 - 24 Hours HOURLY on MEWs chart
After 24h 4 Hourly After an Anaesthetists top up of 1. Every 15 minutes for one hour Local Anaesthetic in to the Epidural catheter 2. Every hour for 4 hours
3. Every 4 hours
If patient’s condition deteriorates Contact ward doctor for urgent review or pain team.
Increase frequency on monitor/recording vital signs if outside patient’s normal parameters.
Continue increased frequency of recording of vital signs until the patient’s condition improves.
Ensure the patient is placed in an observable position on the ward.
18. Mobilising Patients with Epidural in situ 18.1 Bed to chair.
18.2 Patients must be in a stable condition.
18.3 Check BP pre and post transferring.
18.4 Being light- headed, feeling nauseous may occur but is not unusual.
18.5 Return the patient to bed and record the patient’s vital signs.
18.6 If the vital signs are within the normal range encourage the patient to do some deep breathing, leave the patient to recover and try again later to mobilise.
18.7 If the vital signs are not within the patient’s normal parameters contact the ward doctor to review the patient’s condition.
14 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date 18.8 May require Oxygen 2L/min via nasal cannula and ensure the IV line is patent.
18.9 Sit the patient on the edge of bed.
18.10 Two nurses/physiotherapists/midwifes should initially be involved in the move from bed to chair. Postural hypotension or motor block may cause the patient to be unsteady on his/her feet.
18.11 Take care of all lines and attachments.
18.12 Make sure the patients back is not resting on the epidural filter, secure to clavicle/chest to ensure accessibility.
18.13 Elevate feet on a stool – to compensate for venous pooling.
18.14 Patient should be able to mobilise fully with assistance (following Bromage scale assessment).
18.15 Good mobilisation helps to prevent Deep Venous Thrombosis (DVT) or chest infections.
19. Minimise the Risk of Infection and Care of the Epidural Catheter Site. 19.1 Inspection of the epidural catheter site must be undertaken twice per shift and fully documented in the patients nursing plan.
19.2 Observe for any inflammation, tenderness or leakage at the epidural site. Report this to the doctor and/or pain team.
19.3 The epidural dressing covering the site must remain intact; site not to be exposed at any time due to high risk of infection (epidural abscess).
19.4 If the epidural site is exposed contact the on call anaesthetist or pain team to make a risk assessment decision regarding the continuation of the epidural infusion.
19.5 Epidural site must not be immersed in water (e.g. a bath) due to the risk of cross- contamination.
19.6 If an infection is suspected: Refer to procedure for suspected epidural abscess/ haematoma (see section 27).
20. Accidental Disconnection of the Epidural Bacterial Filter. 20.1 Witnessed disconnection from the epidural bacterial filter - contact Anaesthetist and sterile field should be made.
20.2 Free end of the epidural catheter cleaned and sterilised with aqueous chlorhexidine to a length of over 10 cm by the Anaesthetist only.
20.3 The catheter can be cut with sterile scissors or blade half way into the cleaned area and the joint with the filter remade.
20.4 Unwitnessed disconnection from the epidural bacterial filter. If the time of disconnection is unknown - then it would be safer to stop the epidural infusion and commence alternative analgesia.
15 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date
20.5 Remove the epidural catheter according to coagulation guidelines (see section 5).
20.6 Contact the pain team or out hours contact the On-call theatre anaesthetist.
20.7 Document all this in the epidural nursing care plan.
21. Changing the Epidural Infusion Rate.
Look at main screen Screen displays Press - up and down arrows Prescribed infusion settings to highlight continuous rate Highlight continuous rate Once highlighted Press select Screen displays Enter code Press code number (trained staff only) PRESS ACCEPT VALUE Screen displays Continuous rate Press up and down arrows to select appropriate rate Press save Screen displays Home screen displays new Document on the epidural rate nursing care plan
22. Changing the Epidural Bag.
22.1 Epidural trained nurses/OPDs/midwife and the on-call Anaesthetist are the only staff to exchange epidural infusion bags.
22.2 Documentation should be recorded at every change as per WWL procedure regarding controlled drugs on the patient's prescription chart.
22.3 Epidural LA Bag changes must be undertaken using ANTT.
22.4 There is no need to replace the giving set and cartridge until treatment is discontinued (maximum use 5-7 days infection risks increase the longer the epidural catheter is in place).
22.5 Pump screen.
Look at epidural screen Epidural pump will alarm PRESS red/green button to when the bag is nearly stop pump. empty Check patient’s drug board to access correct epidural infusion bag. Check patient’s wristband with 2nd nurse with drug board. Close roller clamp on giving set Epidural trained staff to change infusion bag using ANTT 2nd nurse opens epidural lock box, using gloves
16 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date removes the old infusion bag and passes the infusion spike/giving set to the nurse with sterile gloves on. 2nd nurse then removes the foil/plastic cover from the new epidural bag, and passes this to the 1st nurse who spikes the new bag. The new bag is replaced in the lock box and locked with key. Open roller clamp on giving set and Scroll down using arrows to the bottom therapy. Screen displays Highlighted in white Press select Reservoir Vol. Screen displays Enter code TRAINED STAFF ONLY TO ENTER CODE Screen displays PRESS ACCESS VALUE Screen displays the PRESS SELECT TO reservoir vol. RESET VOL. Press SAVE Screen displays Re vol. show new vol. of Press red/green button to bag restart pump. Screen displays Review pump setting Press review Screen displays Enter code TRAINED STAFF ONLY TO ENTER CODE Accept value Screen displays Full list of therapy’s Accept each value which is highlighted by pressing Accept value Screen will display GREEN Arrow at the side of Press Next each value Review complete Screen displays Start pump Press YES Screen now show new bag volume Screen displays Top of screen now show Document in epidural pump running nursing care plan
23. Reviewing the Patients History on the Epidural Infusion Pump
Main Screen Look at screen bottom Left Show report side of pump Press button below reports Screen displays List of available options PRESS Select Given and PCA Dose Counter is Highlighted
Screen displays Total given since starting
17 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date pump Scroll down to highlight over Using up and down arrows options Screen displays PCA Dose given and PCA Documents reading on Attempts nursing epidural care plan Press back x2 to return to Main screen
24. Discontinuing the Epidural Infusion.
Record all infused volumes and patient bolus totals on the patients epidural nursing care plan.
Stop the epidural pump by pressing the red/green button.
Press the grey button on the right side of the epidural pump.
Screen will display power down - Press – Yes.
Unlock the lock box.
Unlock the epidural pump using key which will allow the silver lever to be pressed down and this will release the cartridge.
The cartridge / giving set and epidural bag must be discarded in to a sharps bin. The epidural pumps must be cleaned as per hospital guidelines (attach green label to highlight the pump has been cleaned).
Remove batteries from pump and place inside case.
Return epidural pump and mains lead to theatre as soon as possible.
25. Removing an Epidural Catheter. 25.1 Before removing the Epidural catheter refer to procedure on anti-coagulation (see section 5).
Equipment for removing the epidural catheter Dressing pack Skin cleaning solution Spot plaster
Inform and prepare the patient what you are about to do. To minimise patient anxiety.
Wash hands with soap and To minimise cross infection. water or hand gel. Open dressing pack. On to clean dressing trolley.
Remove tape and dressing from epidural To allow for full inspection. catheter site.
18 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date
Wash hands again and put on sterile ANTT. gloves. Gently, in one swift movement, remove To ensure the catheter is removed intact. the epidural catheter. Document in the nursing notes:- witness Check that it is intact by observing marks intact epidural catheter tip. along the catheter. If the tip does not have a dark end (visible to x ray). Contact the pain team or On call anaesthetist.
Apply an occlusive dressing and leave in As prophylaxis against infection along situ for 24 hrs. catheter tract and primary healing of the site.
Any evidence to suggest the epidural site is Document this in the nursing notes. infected please send the tip of the epidural An infection may lead to a spinal abscess. catheter for C/S. Continue to observe and record motor and sensory function.
26. Management of the Epidural Catheter Site on Discharge. 26.1 GP discharge letters/district nurse letters/Maternity discharge should include information that the patient has had an epidural infusion.
26.2 Details include any complications as epidural abscesses may occur post discharge.
26.3 All patients must be provided with a patient information leaflet – ‘Discharge Advice following an epidural infusion (see Intranet patient information leaflets – Discharge advice following an epidural infusion information leaflet).
26.4 An explanation regarding this information must be explained to the patient by the nurse/midwife or a member of the pain service regarding the complications and documented in the patients notes.
STOP epidural infusion
Remove catheter within coagulation guidelines ASAP 27. Suspected Epidural Abscess or Haematoma Send Management. tip of epidural catheter for Culture and Sensitivity (C/ S) and swab epidural site and send C/S. Hospital patient - Inform surgical team for Patient has had an epidural infusion insituurgent review for pain management Document findings in patient notes
Consider I.V antibiotic therapy PatientPatient is complaining is complaining of :of : Consider urgent MRI scan WeaknessNew episode of lower of Backachelimbs SensoryDermatome deficit painfor example- Altered SensationTenderness such atas epidural insertion Inform Named Consultant site Pins and Needles or Numbness 19 BladderSwelling or bowel around dysfunction epidural site Community patient - Inform GP or On-call Paralysis doctor for urgent review 999 to A/E
Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date
28. Transfer of patients with an epidural infusion to other hospital sites
28.1 Patients with an epidural infusion/ catheter insitu who require a planned/unplanned transfer must be accompanied by a trained nurse escort with paramedic crew.
28.2 Monday – Friday (Days) the provision of an escorting nurse must be co- ordinated by a matron and/or the first bleep holder who will ensure the release of a nurse whilst maintaining safety of the remaining patients at Wrightington/RAEI site.
28.3 At weekends and nights – if a nurse cannot be sourced by the first bleep holder then the Epidural infusion must be capped off using ANTT following discussion with the on-call anaesthetist.
28.4 An alternative method of providing analgesia must be prescribed and administered as appropriate.
29.5 The receiving hospital must be contacted immediately regarding the transfer and the analgesia plan on arrival. The on call anaesthetist/pain service must be contacted.
29. Human Rights Act Implications of the Human Rights Act have been taken into account in the formulation of this policy and they have, where appropriate, been fully reflected in its wording.
30. Accessibility Statement This document can be made available in a range of alternative formats e.g. large print, Braille and audio CD. For more details, please contact the HR Department on 01942 77 (3766) or email [email protected]
20 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date Appendix 1
References
Smith G, Power I, Cousins MJ.(1999) Acute pain: is there scientific evidence on which to base treatment? Br J Anaesth; 82: 817-819.
Brodner G, Pogatski E, Van Aken H, Buerkle H, Goeters C, Schulzki C, et al. (1998). A multimodal approach to control postoperative pathophysiology and rehabilitation in patients undergoing abdominothoracic oesophagectomy. Anesth Analg; 86: 228-234.
Kehlet H, Werner M, Perkins F. (1999). Balanced analgesia: what is it and what are its advantages in postoperative pain? Drugs. Nov; 58(5): 793-7
Kehlet H. (1999). Acute pain control and accelerated postoperative surgical recovery. Surg Clin North Am. Apr; 79(2): 431-43
Nimmo.S,(2004). Benefit and outcome after epidural analgesia. Continuing Education in Anaesthesia, Critical Care & Pain / Volume 4 No 2.
Phillips J.M.J, Stedeford J.C, Hartsilver E, Roberts C. (2002). Epidural abscess complicating insertion of epidural catheters. Br J Anaesthesia,Vol. 89, No.5 p.778 – 78
Checketts MR, Wildsmith JAW.(2004). Regional Block and DVT Prophylaxis. Continuing Education in Anaesthesia, Critical Care and Pain. Vol. 4 (2).
Good Practice in the management of continuous analgesia in the hospital setting (2004). RCA, RCN, BPS. London.
Harrop-Griffiths W, Cook T, Gill H et al. 92013). Regional anaesthesia and patients with abnormalities of coagulation. Anaesthesia, 68: 966-972
Bromage scale Anesthesia - Analgesia (1993), 77:919 – 24
NICE Guidelines Dec (2014).
21 Epidural Infusion for Pain Management Version No:1 Author(s) Pain Clinical Nurse Specialist Ratified PARC Next Review date Appendix 2
Epidural infusion patients nursed in side rooms.
A. Epidural infusion patients on the Labour ward are nursed in a side room with one- to-one midwife staffing, by midwives who are up-to-date with their epidural training.
B. Side rooms other than those in Labour Ward; any epidural patients nursed in side rooms must have one-to-one staffing by a nurse who is up-to-date with their epidural training. This has been agreed with the WWL anaesthetic department.
Consultant: Dr Nick Flatt.
Date: 03/02/17.
22 Pain Management Care Plan Name: ………………………. DOB: ………………….. Unit no: ……………………… Ward: …………………. Appendix 3 Patient Controlled Epidural Infusion (PCEA) Problem Objective Nursing action Program Program Epi Site Epidural pump program and history are checked as prescribed at the Date Signature Signature Signature Patient has a Ensure patients start of every shift and documented with 2 signatures on every change Patient are nursed in a of nursing personnel responsible for the patients care. Early Controlled safe Epidural environment by Nursed in main ward areas (see appendix 1. for JCW and delivery suit). Late Infusion staff who have . Monitor vital signs including Pain, Sedation Nausea and vomiting score. in situ undertaken . Motor function assessment (signs of spinal complications). Night (PCEA) training in the . Epidural catheter site must be observed and documented each care of patients shift. Early requiring PCEA . IV (access) fluids must be continued until epidural is discontinued (risk of hypotension). Later Provide . Urinary catheter must be in situ until the epidural is discontinued (risk of urine adequate pain retention). Night relief . Pressure areas to be checked regularly (risk of reduced sensation). . Be aware of side effects of Opioid and Bupivacaine administration. Early Recorded as per epidural SOP - hourly first 24 hours – 4 hours until PATIENT DISCHARGE. BP to be recorded pre and post mobilization (risk of vasodilation). Late Patient mobilization . Epidural catheter is secure and insertion site protected. (risk of detachment) moving and . Patients motor function is not restricting mobilization (risk of limb weakness). Night handling. . Anti-coagulation SOP section 5 . Care of epidural catheter tip SOP section 20. Early
your hospitals, your health, our priority Removal of the . Only remove epidural catheter when oral fluids are tolerated and balanced step Late epidural catheter. down analgesia prescribed. Ensure step down analgesia is prescribed and administered following Night cessation of the epidural infusion and Early Information for the REGULARLY EVALUATE treatment plan. care of the patient in The patient's discharge GP/District nurses letter should contain information Late the community. regarding the epidural insertion and any complications. Patient epidural advice leaflet to be given on discharge. Night
24 Appendix 4.
EPIDURAL INFUSION RECORD
Patient Name Date...... Ward………………………. Unit Number Surgery /Maternity
Date of Birth Anaesthetist...... ……
(or paste addressograph label) Anaesthetist comments…………………………….. Dural Tap YES NO No. of attempts…………… Allergies……………………………………………………
Epidural Insertion Details
Catheter Site Depth to Space Catheter in Space
Epidural Prescription Details – Provided at HAND OVER
Epidural Infusion Rate of Infusion CHECKED Date/Time 0.1% Bupivacaine + Fentanyl 2 micrograms/ml 250mls or …………. mls/hr 500mls Bags ………..... mls/hr 0.125% Bupivacaine 250mls bags 0.15% Bupivacaine ……..…… mls/hr 500mls bags
Epidural Pump Set Up, Checked
Pump Set Time and Date Anaesthetist Recovery On hand over P ra Medical Device Ward ct Nurse/O iti DP/Midw ID Number o ife n er
Any patient VITAL signs which are not within normal MEWs/MOEWS scores contact immediately:- 1.DO Ward NOT - OnADMINISTER Call Doctor or ANY IV OR IM OPIOIDS WITHOUT CONSULTING THE 2. In hours,ACUTE Pain PAIN Team, SERVICE Page via switchOR ON-CALL board (9.00 ANAESTHETIST to 17.00) or 25 3. Contact On Call Anaesthetist on Bleep RAEI - 5791 or Wrightington - 8033 or Maternity 5107 4. Critical Care Outreach Team on Ex. 6240 Epidural Monitoring Form( hourly vital signs- on MEWS chart and 4 hourly epidural observations)
Date Time Resp Rate Pain Scale PONV Score (Side Effects) Vital signs - Monitoring 0 - No Pain at rest, no pain on movement. 0 No Nausea or vomiting 0 – 24 Hours Hourly 1 – No Pain at rest, Mild pain on movement. 1 Mild Nausea but no vomit After 24 hours 4 Hourly O2 –2 IntermittentSat% pain at rest, moderate pain on movement 2 Moderate vomittind and/or occasional vomit Sedation3 – Continuous Score pain at rest, severe pain on movement 3 Severe nausea and/or vomiting Sedation Scores Bromage scale (motor block) After top up of Epidural 1. Every 15 minutes for 1 hour Pain Rest 4 hrly Score0 None (FULLY alert) 0 - Full flexion of knees and feet 2. Every hour for 4 hours 1 Mild (EasyMove to rouse). 1 - Just able to move knees 3. Every 4 hours Height2 Moderate of Block (Drowsy or sleepy but can be easily 2 – Able to move feet only If Patient’s condition Increase frequency based on vital wakened). deteriorates signs until condition improves level3 Severe (Somnolent or difficult to rouse). 3 – Unable to move feet or knees Derm Right Level Left
Motor Right Block Left Inf Rate [mls/hr] Total Vol Inf [mls] Patient Bolus (PECA) Tries and Good Site Checked MEWS Score Signature
26 Record all Nursing/Medical Interventions (e.g. Bag/ Rate changes, block changes etc.)
When discontinuing the epidural infusion ensure step down analgesia is prescribed. Date and time when epidural is stopped and catheter removed (see section 5 in SOP).
Check Epidural TIP intact YES /NO Patient information leaflet provided Yes/ No Interventio Date Time n Signature
your hospitals, your health, our priority :
APPENDIX 5- BROMAGE SCALE
28 :
Pain Service
Appendix 6 Assessment for - CADD Solis Epidural Infusion Pump (Adult Patients)
This is a HIGH RISK device – Do not use high risk equipment unless you have been trained and demonstrated competence to a key trainer/assessor Name
Job title
Dept / Division
Participant must demonstrate practical knowledge in the clinical application and management of the above device, You must answer YES to all questions below before being considered competent. If you are not competent you must instigate further learning and repeat the process, It remains the users responsibility to maintain that competence and knowledge (NMC 2006)
Can you the participant: Yes No Completed the epidural training course (access via Pain team or Pain Link Nurse in your area) Carry out all pre operational checks on the above epidural pump? Check for any faults on the epidural pump? List main functions on the epidural pump? Prepare all equipment. Describe what observations should be recorded as per epidural SOP Commence an epidural infusion - Patients Care Pathway Key staff – Anaesthetists, Pain nurse, Recovery staff, ODP staff Demonstrate how to turn on the epidural pump? Correctly programme the pump? (Key staff only) Demonstrate how to purge the epidural line? Demonstrate how to change the epidural infusion bag? Show how to change the epidurals battery? Solve an epidural alarm? Describe how to preview the epidural programme? State how to lookup epidural volume total? State how to lookup epidural bolus history? State how to switch the epidural pump off and recommence the infusion? State how to change the epidural infusion rate? Describe how to clean and store the epidural pump following use? State how you would report an epidural pump fault or breakdown?
Statement of participant: - I am competent to use the above device without further training, I understand that I may be subjected to random assessment without prior notification by an unspecified assessor.
Signature
Date
Signature: Pain Team Specialist Nurse………………………………………………. (or Pain Link Nurse in your clinical area) Date
29