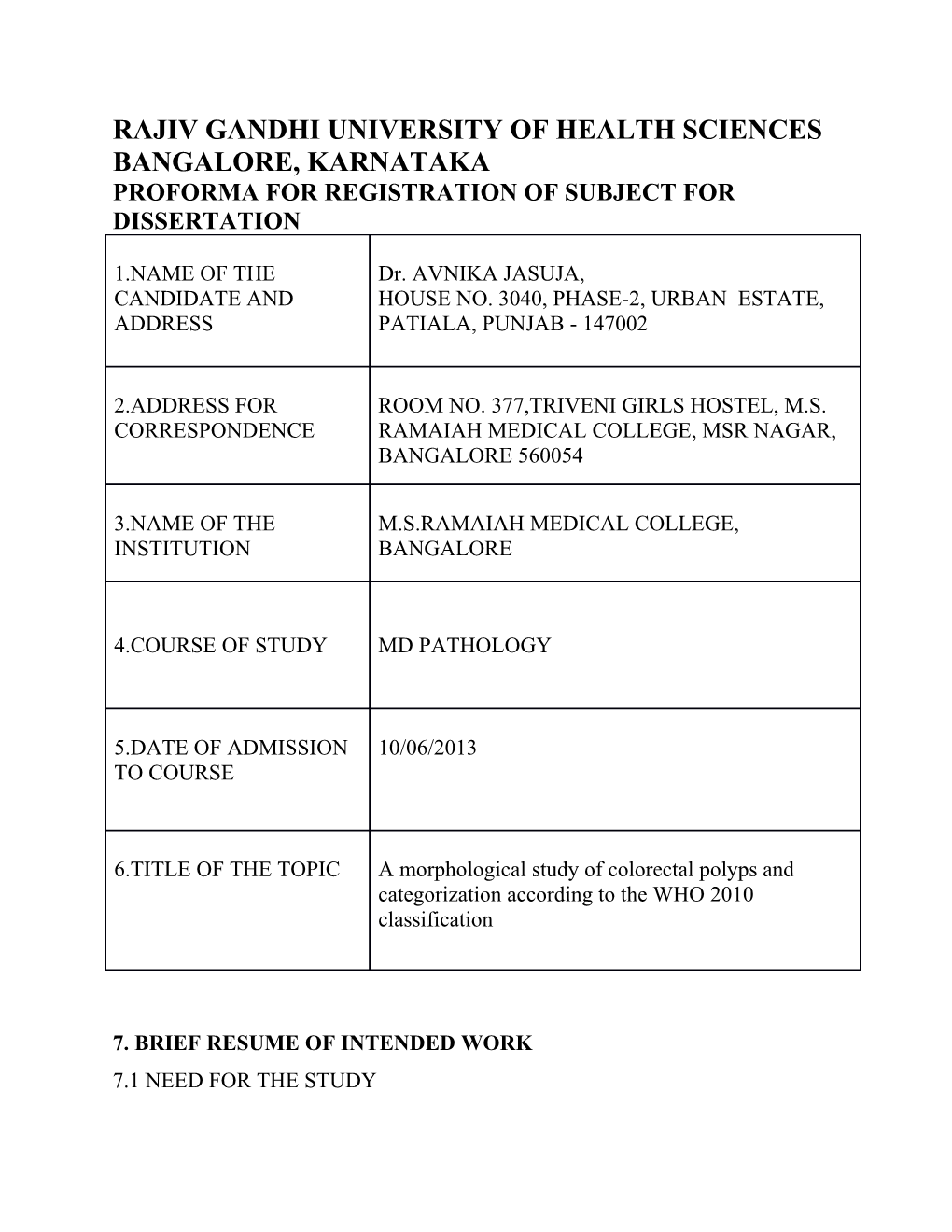
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES BANGALORE, KARNATAKA PROFORMA FOR REGISTRATION OF SUBJECT FOR DISSERTATION
1.NAME OF THE Dr. AVNIKA JASUJA, CANDIDATE AND HOUSE NO. 3040, PHASE-2, URBAN ESTATE, ADDRESS PATIALA, PUNJAB - 147002
2.ADDRESS FOR ROOM NO. 377,TRIVENI GIRLS HOSTEL, M.S. CORRESPONDENCE RAMAIAH MEDICAL COLLEGE, MSR NAGAR, BANGALORE 560054
3.NAME OF THE M.S.RAMAIAH MEDICAL COLLEGE, INSTITUTION BANGALORE
4.COURSE OF STUDY MD PATHOLOGY
5.DATE OF ADMISSION 10/06/2013 TO COURSE
6.TITLE OF THE TOPIC A morphological study of colorectal polyps and categorization according to the WHO 2010 classification
7. BRIEF RESUME OF INTENDED WORK 7.1 NEED FOR THE STUDY Colorectal polyps are common lesions and some of them are known to have malignant potential; therefore correct morphological classification and further studies may help in clinical management of these patients. In the revised WHO classification for colorectal tumors, 2010, the broad classification of adenomatous and non-adenomatous polyps has been maintained. Adenomas are classified into tubular, tubulo-villous or villous, similar to that in the previous classification. However, in the non-adenomatous polyp category, a separate entity of serrated lesions has been described, under which hyperplastic polyps, sessile serrated adenomas and traditional serrated adenomas are included1. Adenomatous polyps are known to progress to malignancy via the APC pathway and standard guidelines exist for management of adenomatous polyps with dysplasia. Recent studies have shown that sessile serrated adenomas with dysplasia also have a premalignant potential, but via the microsatellite instability (MSI) pathway 2, which is distinct from that of the APC and at present there are no standard guidelines for management of these lesions. The demography of colorectal polyps and colorectal cancers differ widely between India and the West and most of the available literature is from the developed nations. There is currently limited data available on the classification of colorectal polyps in India 3and in these the older WHO classification has been followed. We propose to evaluate the morphology of colorectal polyps and reclassify them according to the WHO 2010 classification in which the new category of serrated lesions has been included. 7.2 REVIEW OF LITERATURE Higuchi et al3 in 2005 retrospectively studied all colorectal polyps obtained by colonoscopic polypectomy between 1992 and 1994 at a hospital in Montreal, Canada. Among the 1250 polyps studied, 891 (71.2%) were adenomatous, 298 (23.8%) were hyperplastic and 61 (5%) were serrated lesions including 27 (44%) sessile serrated adenomas. The diagnosis of serrated lesions was based on the criteria established by Longacre and Fenoglio-Preiser. Among the 891 adenomas, 688 (77.2%) tubular adenomas, 190 (21.3%) tubulovillous adenomas and 13 (1.5%) villous adenomas were reported. In a study published by Tony et al4 in 2007 from Calicut Medical College, Kerala, who analyzed colorectal polyps in their institution from 2001 to 2005, a total of 124 colorectal polyps were studied. Of these 99 (79.8%) were adenomatous, 12 (9.8%) were juvenile polyps, 11 (8.8%) were hyperplastic polyps, 1 (0.8%) was inflammatory polyp and 1 (0.8%) was a Peutz Jegher’s polyp. The 99 adenomatous polyps comprised of 61 (62%) tubular adenomas, 24 (24%) tubulovillous adenomas and 14 (14%) villous adenomas. According to WHO Classification of Tumors of Digestive system1, 2010, benign lesions of the large intestine are classified into Adenomas, Serrated lesions and Hamartomatous lesions. Adenomas are further divided into Tubular, Tubulovillous and Villous adenomas. Serrated lesions are Hyperplastic Polyp, Sessile Serrated Adenoma/Polyp and Traditional Serrated Adenoma. Three morphological types of hyperplastic polyp have been described: microvesicular, goblet cell-rich, and mucin poor, although there is no known clinical significance of these variants. Hamartomatous polyps are Cowden- associated, Juvenile and Peutz-Jeghers polyp.
A prospective study done by Buda et al5 in 2012 in Italy studied all colorectal polyps obtained from consecutive average risk asymptomatic individuals undergoing first time colonoscopy between June 2007 and December 2008. A total of 258 polyps were obtained which were classified using the system described by Snover, which has now been included in the WHO 2010 classification. Of the 258 polyps, 155 (60%) were adenomas and 120 (40%) serrated polyps. These serrated lesions included 68 (66.6%) hyperplastic polyps, 28 (27.4%) sessile serrated adenomas and 6 (5.8%) traditional serrated adenomas.
Tadashi Terada6 from Japan in 2013 studied the histopathology of 1022 consecutive benign rectal lesions received over 10 years in their pathology laboratory in Japan. 248 (24%) of these lesions were reported as adenomas, 54 (5%) were hyperplastic polyps and 24 (2%) were serrated adenomas. The 248 adenomas included 182 (73.4%) tubular adenomas, 42 (17%) tubulovillous adenomas and 24 (9.6%) villous adenomas.
7.3 OBJECTIVES OF THE STUDY
1) To study the morphology of colorectal polyps and apply 2010 WHO guidelines to them.
2) To note the percentage of serrated lesions in the polyps studied.
8. MATERIALS AND METHODS
8.1 SOURCE OF DATA All colorectal polyps received for routine histopathological evaluation and any non-malignant polyps identified in colectomy specimens received in Department of Pathology, M.S. Ramaiah Medical College and Hospitals, Bangalore, from June 2011 to May 2015 will be the source of data for the study.
8.2 METHOD OF COLLECTION OF DATA
The detailed clinical history including age, gender and results of relevant investigations done will be collected/abstracted from the patients’ case files. For prospective cases, specimens will be received in the Pathology Department in 10% formalin. In every case the standard protocol for surgical grossing of resected specimens will be followed. After conventional processing, paraffin sections of 5μm thickness will be stained by haematoxylin and eosin (H and E) for histopathological study.
For retrospective cases, slides and paraffin blocks will be retrieved from the archives. Additional sections will be made from the retrieved paraffin blocks. The polyps will be classified according to the WHO 2010 criteria and the relationship between various parameters such as age, gender, anatomic site of polyp, and histologic type will be studied in all biopsy specimens.
8.3 INCLUSION CRITERIA Polypectomy specimens and biopsies from patients with colorectal polyps and non-malignant polyps detected in total colectomy or hemicolectomy specimens. 8.4 EXCLUSION CRITERIA Polyps from patients with familial adenomatous polyposis.
8.5 SAMPLE SIZE DETERMINATION A study carried out by Buda et al (2012) revealed that the proportion of adenomas in all colorectal polyps is 60% and further, among 120 (40%) non adenomatous polyps the proportion of hyperplastic polyps is 66%. Based on the above findings, with a relative precision of 7% and confidence level of 95% (5% alpha error), it is estimated that 188 polyps need to be included for the study. 8.6 STATISTICAL ANALYSIS Descriptive statistics of morphological classification will be analysed and presented in terms of percentage and its 95% confidence interval will be analysed. Chi Square test will be used to find the association between morphological types of polyps and their size and site and the patient’s age and gender.
8.7DOES THE STUDY REQUIRE ANY OTHER INVESTIGATIONS OR INTERVENTIONS TO BE CONDUCTED ON HUMANS OR ANIMALS? Colonoscopic biopsy and histopathological examination will be performed as a part of routine protocol for treatment, pathological assessment and planning further management. No additional investigations or interventions will be done specially for the purpose of the dissertation.
8.8HAS ETHICAL CLEARANCE BEEN OBTAINED FROM YOUR INSTITUTION? Yes (clearance certificate attached)
9.REFERENCES 1. Bosman FT, Carneiro F, Hruban RH, Theise ND, et al. World Health Organization Classification of Tumours of the Digestive System. Fourth Edition. Lyon: International Agency for Research on Cancer Press; 2010. 2. Jass JR. Classification of colorectal cancer based on correlation of clinical, morphological and molecular features. Histopathology 2007; 50: 113-30. 3. Higuchi T, Sugihara K, Jass JR. Demographic and pathological characteristics of serrated polyps of colorectum. Histopathology 2005; 47: 32-40. 4. Tony J, Harish K, Ramachandran TM, Sunilkumar K, Thomas V. Profile of colonic polyps in a southern Indian population. Indian J Gastroenterol. 2007 May-Jun; 26(3): 127-9. 5. Buda A, De Bona M, Dotti I, Piselli P, Zabeo E, Barbazza R et al. Prevalence of different subtypes of serrated polyps and risk of synchronous advanced colorectal neoplasia in average risk population undergoing first time colonoscopy. Clin Transl Gastroenterol. 2012 Jan 5; 3:e6. doi: 10.1038/ctg.2011.5. 6. Terada T. Histopathologic study of the rectum in 1438 consecutive rectal specimens in a single Japanese hospital: 1. benign lesions. Int J Clin Exp Pathol 2013; 6(3):349-57.
10.SIGNATUREOF THE CANDIDATE
Epithelial tumors of the colon and rectum are 11. REMARKS OF THE GUIDE common entities and WHO has revised their classification in 2010. Therefore revised pathological classification of colorectal polyps is being studied which is important for clinical management.
12.(a) NAME AND DESIGNATION OF DR. AARATHI R RAU THE GUIDE PROFESSOR OF PATHOLOGY
(b) SIGNATURE OF THE GUIDE (c) NAME AND DESIGNATION OF THE DR.UMESH JALIHAL, CO-GUIDE SENIOR PROFESSOR OF GASTROENTEROLOGY
(d) SIGNATURE OF THE CO-GUIDE
(e) HEAD OF THE DEPARTMENT DR.K.C.MAHADEVA
(f) SIGNATURE OF THE H.O.D
(g) REMARKS OF CHAIRMAN AND PRINCIPAL
(h) SIGNATURE OF THE PRINCIPAL