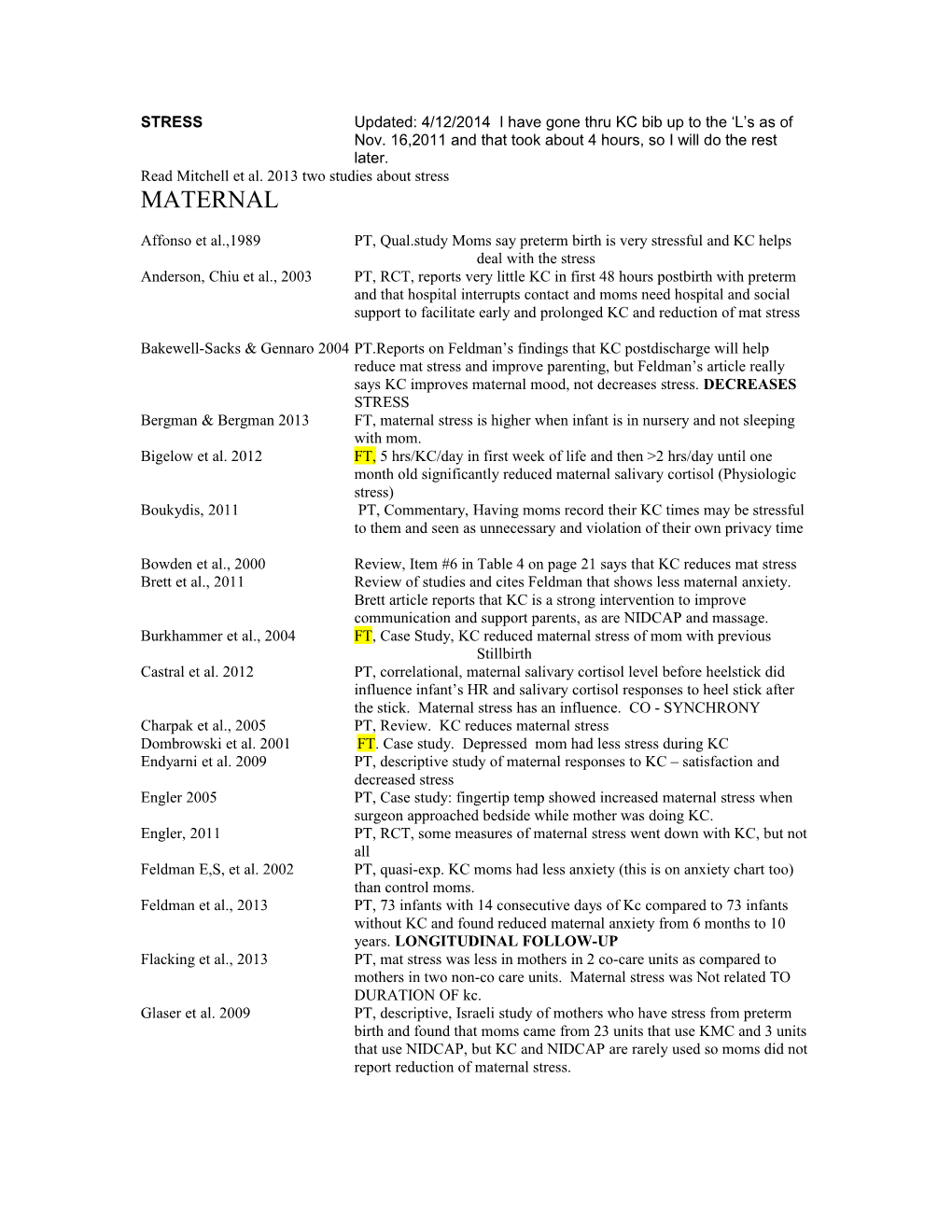
STRESS Updated: 4/12/2014 I have gone thru KC bib up to the ‘L’s as of Nov. 16,2011 and that took about 4 hours, so I will do the rest later. Read Mitchell et al. 2013 two studies about stress MATERNAL
Affonso et al.,1989 PT, Qual.study Moms say preterm birth is very stressful and KC helps deal with the stress Anderson, Chiu et al., 2003 PT, RCT, reports very little KC in first 48 hours postbirth with preterm and that hospital interrupts contact and moms need hospital and social support to facilitate early and prolonged KC and reduction of mat stress
Bakewell-Sacks & Gennaro 2004 PT.Reports on Feldman’s findings that KC postdischarge will help reduce mat stress and improve parenting, but Feldman’s article really says KC improves maternal mood, not decreases stress. DECREASES STRESS Bergman & Bergman 2013 FT, maternal stress is higher when infant is in nursery and not sleeping with mom. Bigelow et al. 2012 FT, 5 hrs/KC/day in first week of life and then >2 hrs/day until one month old significantly reduced maternal salivary cortisol (Physiologic stress) Boukydis, 2011 PT, Commentary, Having moms record their KC times may be stressful to them and seen as unnecessary and violation of their own privacy time
Bowden et al., 2000 Review, Item #6 in Table 4 on page 21 says that KC reduces mat stress Brett et al., 2011 Review of studies and cites Feldman that shows less maternal anxiety. Brett article reports that KC is a strong intervention to improve communication and support parents, as are NIDCAP and massage. Burkhammer et al., 2004 FT, Case Study, KC reduced maternal stress of mom with previous Stillbirth Castral et al. 2012 PT, correlational, maternal salivary cortisol level before heelstick did influence infant’s HR and salivary cortisol responses to heel stick after the stick. Maternal stress has an influence. CO - SYNCHRONY Charpak et al., 2005 PT, Review. KC reduces maternal stress Dombrowski et al. 2001 FT. Case study. Depressed mom had less stress during KC Endyarni et al. 2009 PT, descriptive study of maternal responses to KC – satisfaction and decreased stress Engler 2005 PT, Case study: fingertip temp showed increased maternal stress when surgeon approached bedside while mother was doing KC. Engler, 2011 PT, RCT, some measures of maternal stress went down with KC, but not all Feldman E,S, et al. 2002 PT, quasi-exp. KC moms had less anxiety (this is on anxiety chart too) than control moms. Feldman et al., 2013 PT, 73 infants with 14 consecutive days of Kc compared to 73 infants without KC and found reduced maternal anxiety from 6 months to 10 years. LONGITUDINAL FOLLOW-UP Flacking et al., 2013 PT, mat stress was less in mothers in 2 co-care units as compared to mothers in two non-co care units. Maternal stress was Not related TO DURATION OF kc. Glaser et al. 2009 PT, descriptive, Israeli study of mothers who have stress from preterm birth and found that moms came from 23 units that use KMC and 3 units that use NIDCAP, but KC and NIDCAP are rarely used so moms did not report reduction of maternal stress. Grazel and Hawn, 2001 PT: PSS:NICU stress went down with earphones, more with earphones than without earphones, but both groups decreased stress after 2 sessions of KC. DECREASE Gordon et al., 2010 FT, descriptive. Increases in Central oxytocin help mediate the effects of stress in the first few months of life (p.380) and positive interactions with the baby increase central oxytocin. Handlin et al., 2009 FT, RCT, maternal cortisol decreases more as KC continues. Harrison, 2010 FT, Case study of congenital heart defect baby who got 14 days of 80+mins of KC/day and mom said KC helped with her stress. Heinemann et al., 2013 PT, qualitative study in which parents report that the NICU environment and procedures are very stressful to them. Johnson 2005 PT/FT review and says KC reduces maternal stress as other forms of touch do. Includes some basic touch and mat stress research too. Jones & Spence, 2002 Review of ways to improve Breastfeeding. Says nurse should encourage moms do KC to reduce stress of NICU and preterm birth, which may in turn help milk supply and breastfeeding motivation Lai et al., 2006 PT, RCT, less maternal anxiety each day of 3 days of KMC+music than in mothers of infants who remained in incubator Lasiuk et al., 2013 PT,qualitative. Parents have traumatic psychological distress related to preterm birth. Obstetrical and neonatal healthcare providers need to be educated about the symptoms of Acute Stress Disorder (ASD) and Posttraumatic Stress Disorder (PTSD) to better understand and support parents of preterm birth birth. Breast feeding, kangaroo care, and family centered practices are so meaningful to parents because they help them (re)construct their role as parents, afford parents a sense of agency, moderates (decreases) parental helplessness. Lau et al., 2007 PT, descriptive. Questionnaires every two weeks x 10 weeks after VLBW birth. AA moms had lowest state anxiety, Caucasian moms had lowest scores in social desirability of BF, and stress was similar between AA, Caucasian and Hispanic moms as measured by PSS:NICU. KC was only correlated with milk volume and drive to express milk, not with stress and anxiety. Lee & Shin, 2007 PT, non-equivalent control pretest-postest design in which KC significantly reduced maternal anxiety. Leonard et al., 2008 PT, doing 24/7 KC is stressful for moms. Many sources of stress/discomfort and want to help baby but also want to be home. Lindgren et al., 2011 Adults, human skin-to-skin touch and skin-to-skin massage strongly stimulate the pregenual anterior cingulated cortex area of brain which is area the reduces pain, anxiety, stress when stimulated with opioids and increases senses of well-being. This is mechanism of touch effects. Ludington-Hoe, et al.1995 Overall maternal stress level was lower on day 5 in KC moms than in Control moms. Ludington-Hoe et al., 2006 PT, RCT, Maternal stress only slightly decreased in three scales but maternal comments say KC decreased stress. Separation from infant was most stressful stressor. NO DIFF Mallet et al., 2007 PT, descriptive study of French NICU personnel knowledge and barriers and potential parental stress was a barrier to KC use Miles et al., 2006 PT, RCT, <32 wks. Daily KC for 4 weeks showed no diff in maternal stress at dc 6 and 12 months post-dc. Used PISS-NICU scale. Modi & Glover, 1998 PT, review of studies showing that 20 mins of KC reduced serum and salivary cortisol levels and beta-endorphin. KC reduces stress Montirosa et al., 2013 PT, quasi-exp, maternal stress is related to infant pain Mooncey et al. 1997 PT, descriptive of 15 babies. Cortisol decreased after 20 mins of KC. KC reduces stress Morelius et al., 2005 PT, desdriptive, no pain, but used pain scale over 4 days of KC. Less stress on 4th day than on 1st day of KC. Moriarty 2007 FT, lay article that says KC was done to relieve maternal and infant tension Neu, 1999 PT, qualitative, mothers are apprehensive transferring vented baby Neu, 2004 PT, Qualitative, KC moms had less anxiety than controls. Moms who left KC reported emotional distress after doing so. DECREASE Neu et al., 2009 PT, descriptive, mothers and infant’s stress (cortisol) levels are in sync Neu & Robinson,2010 PT, RCT, Measured state trait anxiety and depression & Still Face Neu et al., 2014 PT, RCT, measured salivary cortisol during one hour of KC after 1hr/dayX8 weeks at home to determine if co-reg of cortisol occurred with infant. IT DID NOT, and concluded that mother and infant may have to be stressed to have co-regulation occur. Both blanket and KC holding were pleasing to moms and babies. Roberts et al.,2000 PT, RCT, KC given for at least 9 hours and up to 4 weeks later at 9 hr/s week, so Range of KC was 9-36 hours. No difference in stress by PSS near discharge between KC and swaddled holding. Roller 2005 PT, Qual. KC was calming and reduced maternal stress. Schwartz et al., 2004. PT, clinical report. Scrap booking helps mothers bond & adapt to NICU And mothers all have first KC session picture taken to write about in scrapbook and may be a support mechanism, but no mention of stress reduction, minimization, or prevention. Tessier et al., 1998 PT, RCT, maternal stress was ???? Uvnas-Moberg, 1999 FT, Review, maternal stress is less with birth KC. Vinall et al. 2013 PT,, This is not a KC study but it talks about maternal stress in NICU and how that affects long term infant pain outcomes and they used several maternal stress measures. This article is reviewed in RELATED LITERATURE on my PAIN Chart. Whitelaw et al., 1988 PT, RCT,6 questions that indirectly reflect maternal stress. No diff between Kcers and nonKcers at discharge. Got KC from 16th –61th day of life, about 36mins perday (total of 30 hours).. Maternal stress can be measured at birth by Hamilton Anxiety Scale and level of stress at birth is related to PT labor, neonatal sepsis and TTN (Romero-Gutierrez, G., Rocha- Morales, D. & Ruiz-Trevino, A.S. (2013). Results of the application of modified Hamilton Scale in the diagnosis of maternal anxiety during immediately puerperium. Ginecol Obstet Mex 81(4), 180-185.
Infant Stress Abdel-Razek et al. 2009 Mother infant interaction is means to reduce infant pain & stress Academy BF Med 2010 PT, KC diminishes infant stress Badr & Purdy, 2007 PT, FT, Review. “measures that reduce infant stress may actually reduce incidence of brain injury” Bakewell-Sachs 2002 PT, Rev of Smith Study. Reiterates Smith’s suggestion that incubator care may be less stressful for intubated infants than Kangaroo Care. Begum et al. 2009 PT, KC reduced cerebral oxygenation because infant was not stressed Bergman, 2010 PT, BOOK, KC reduces stress and article provides neuroscience behind this result. Bulfone et al., 2011 PT/FT. Review of 19 studies. KC had no effect on stress when stress was examined as a short term outcome. Bystrova, 2009 Review of physiology. KC leads to increase in parasympathetic nervous tone and a decrease in central sympathetic tone,so a decrease in stress occurs Bystrova et al., 2003 FT .RCT. KC after birth may be a natural way of reversing stress-related effects on circulation induced during labour because KC babies were more relaxed. Being born is a physiologic stressor, she calls this BIRTH STRESS Bystrova et al., 2009 FT, RCT, first 2-3 hours postbirth are short sensitive period. KC at this time promotes infants’ abilities to handle stress one year post birth. Cadwell et al. 2009 FT, PT, Book on Breastfeeding and in chapter 4 says that KC at birth reduces infant stress Castral et al. 2012 PT, correlational, Infant salivary cortisol levels in response to heel stick were measured and related to maternal salivary cortisol before heel stick. The ability of mothers to regulate their own stress contributed to the infants' responses to pain and stress. PT Chen et al. 2000 PT. Quasi-Exp. BF with KC was less stressful than BF without KC Christensson et al. 1995 FT, RCT. separation from mother causes crying which is sign of stress/distress Clifford et al. 2001 PT, descriptive. 7 infants who got KC had no cold stress CNN 2010 PT, Case study of infant declared dead and came alive during KC after 20 mins of non-productive resuscitation. Theory is that birth placed infant in stressed mode and KC changed brain function to calm, contented mode and he was able to survive. Collados-Gomez,2011 PT, quasi-exper. KC was related to a decrease in all stress variables and produced tranquility in the preterm infants. Dageville et al. 2011 Review. Says that early life maternal-infant separation can alter biological responses to later stress Eichel, 2001 PT. KC with <1000 gm vented infants had stress with transfer but recovered quickly Erlandsson et al. 2007 FT, RCT. Paternal kc at cesarean birth caused infants to relax and demonstrate diminished stress Feldman et al. 2013 PT, quasi-experimental 10 yr follow-up study of 73 infants who got 1 hours of Kc/day for 14 consecutive days in NICU and at 10 years KCers had attenuated stress response Feldman, 2009 PT, quasi-experiment. The decreased cortisol and decreased sympathetic activity seen in first month after birth was still present 10 years later. Feldman et al. 2010 PT, quasi-experimental. The provision of maternal touch during moments of maternal unavailability (still face) reduces infant’s physiological reactivity to stress. Touch, especially KMC touch, reduces stress responses in infants Feldman et al. 2002 PT, Quasi-Exp. KC infant’s stress-reactivity skills were more optimal, as they were more resilient or less sensitive than controls, over 3 months after receiving KC Ferber & Makhoul 2004 FT, RCT, KC reduces infant stress p.861 Ferber & Makhoul 2008 PT, RCT, KC decreased stressful behaviors during heel stick and one hour later. Franck et al. 2002 PT, Descriptive, infant stress is a barrier to its practice. Gale et al., 1993 PT, descriptive study. Transfer of intubated infant was most stressful. Ganatra et al., 2010 PT, FT review of early onset neonatal sepsis and says that KC’s reducing stress effect may be one reason why infants have less infection if given KC Gitau 2002 PT. RCT. 20 minutes of KC reduced salivary cortisol Gray et al. 2000 FT, RCT. KC meets the American Academy of Pediatric’s recommendation to use nonpharmacologic and environmental interventions to reduce or eliminate newborn stress or pain during circumcision Hall & Kirsten 2008 Review, reviews lit that says that KC reduces infant stress Hardy, 2011 PT,Review of L-H’s Developmental Care chapter and reiterates that KC reduces PT infant stress and mother’s stress Harrison, 2001 Review that says that KC reduces infant stress. Harrison et al. 2004 Need to get this report that correlates physiologic and behavioral measures of stress in preterm infants – may have nothing to do with KC afterall, but needs to be checked out. Lindgren et al., 2011 Brain mechanism study showing that human skin to skin contact is a pleasant stimulus and that human skin to skin contact + movement (i.e. massage) is an even stronger pleasant stimulus and that these stimuli activate the pregenual anterior cingulated cortex, center for anxiety, stress & pain reduction and increased well-being when stimulated by opioids like oxytocin. Ludington et al., 1994 Says that KC reduces maternal stress Lyngstad et al. 2014 PT, R cross over of diaper change in incubator with mom present one day and other day diaper change in KC. HR, SaO2, stress (skin conductance) showed diaper change is stressful and much less stress in KC diaper change Odent, 1989 FT. Sustained immediate KC after birth reduces infant stress, so less stress hormone produced, less energy expended and birthwgt loss is stopped. Miles et al., 2006 PT, RCT. Looked at infant stress at dc and during immunization at 6, 12 months post dc and no differences between groups. Modi & Glover 1998 PT Review of studies and starts with statement that preterms have high levels of stress as measured by cortisolemia. Often values exceed 1500nmol/l and in healthy, same GA infants the level is 150 nmol/l. Reducing circulating cortisol levels might have benefit because high levels of cortisol (a glucocorticoid) are neurotoxic, killing hippocampal cells and reducing hippocampal volume. Mooncey et al., 1997 PT. Morelius et al., 2005 PT Morgan et al. 2011 FT, Randomized cross over of one hr sleep in KMC and one hour sleep in cot. Significantly higher LF (sympathetic control) in separation than in KC. This indicates central anxious autonomic arousal during separation (stress). Maternal separation may be a stressor and may not be benign! Neu et al.,2014 PT, RCT, see under maternal above. Roller 2005 PT, Qual. KC calmed infants and reduced infant jitteriness and stress. Shonkoff et al., 2012 FT,PT, talks about biology of stress and maternal influences on stress. This is not a KC study so it is reviewed below in Related Literature. This is the Technical Report article. Sontheimer et al, 2004 PT, FT, descript. No agitation during 31 in and back transports. Stevens et al.,2014 FT, review of KC at C/S and says studies show that this reduces newborns stress. Svenson et al. 2013 FT,RCT of KC+Bf vs BF alone to resolve severe latching on problems and the 53 KC+BF latched on two times sooner than controls and moms had more positive BF success feelings than controls. Says that results were due to “An underlying mechanism may be that skin-to-skin contact with the mother during breastfeeding may calm infants with earlier strong reaction to "hands on latch intervention" and relieve the stress which may have blocked the infant's inborn biological program to find the breast and latch on.” 1st page of article. Takahashi et al., 2010 FT, Birth KC. Having more than 60 mins of KC in first 2 hours postbirth significantly decreases salivary cortisol level compared to < 60 mins of KC Uvnas-Moberg 1998 Physiol review. Oxytocin in brain causes strong anti-stress effect Weller & Feldman, 2003 KC promotes emotional develop and reduces stress through neuropeptide release. Weller, Rozin etal 2002 PT, RCT, Pituitary -thyroid axis and adrenal function in preterm infants raised by KMC. 24 h/day KMC does not compromise maturation of pituitary- thyroid axis and adrenal function in healthy preterm infants. Measured 17-OHP, T4, and TSH. Wiberg et al., 1989 FT, RCT, 3 yr follow up of 15-20 mins of KC in 1st hour after birth. Urine catecholamines were slightly higher in KC group than in routine care group.
SEE ALSO THE MILGROM ET AL 2010 article in Family Friendly file that shows that sensitivity training of parents in NICU improved cerebral white matter micro- structural development in preterm infants. Paternal STRESS Blomqvist et al., 2011 PT, fathers think separation from NICU infant is stressful Heinemann et al. 2013 PT NICU is very stressful for parents, never nighttime, difficult to sleep and procedures on infant are stressful.
Related Lit of infant stress: 1. Diaper change is stressful to full term babies. -Mörelius E, Hellström-Westas L, Carlén C, Norman E, Nelson N.(2006) Is a nappy change stressful to neonates? Early Hum Dev. 2006 Oct;82(10):669-76. - Mörelius E, Nelson N, Gustafsson PA. (2007).Salivary cortisol response in mother-infant dyads at high psychosocial risk. Child Care Health Dev. 2007 Mar;33(2):128-36.Department of Molecular and Clinical Medicine/Division of Paediatrics, Linköping University Hospital, Linköping, Sweden. [email protected] The aim of the present study was to investigate the adrenocortical response to diaper change in mother-infant dyads with psychosocial risk factors. Twenty-two mother-infant pairs with well-defined psychosocial problems were included. The mother-infant pairs were treated for 6 weeks in a daycare programme to improve attachment. Salivary cortisol was measured before and after a diaper change during the first and last weeks of enrollment in the programme. Mothers' sensitivity towards their infants' signals was measured using a scale from 1 (highly insensitive) to 9 (highly sensitive) according to Ainsworth. Median salivary cortisol increased in 15 out of 22 infants after the first diaper change. The increase was most pronounced in the group of infants below 3 months of age (n = 15) where median salivary cortisol increased 170% after the first diaper change (P < 0.05) and decreased 19% after the last diaper change (not significant). Out of these 15 infants, 11 showed an increase in salivary cortisol in response to the first diaper change while four out of 15 did so in response to the last diaper change (P < 0.05). The salivary cortisol response did not change over time in infants aged 3 months or above. A mother's sensitivity to her child increased significantly (P < 0.001) from the first to the last week. In mothers, median salivary cortisol decreased 38% after the first diaper change (P < 0.05) and 57% after the last diaper.A diaper change is normally not perceived as stressful. The stress response caused by a diaper change may illustrate an insufficiency in the mother-infant relationship before treatment. Professional support improved the mothers' sensitivity and stabilized the stress response to diaper change in the youngest infants.
Massage may help stress: Smith, S.L., Lux, R., Haley, S, Slater M, Beechy J. et al., (2013). The effect of massage on heart rate variability in preterm infants. J. Perinatology 33(1), 59-64. Masked RCT of 17 massage and 20 control 29-32 wek medically stable PTs. Licensed massage therapists did the treatment two times per day for 4 weeks. Weekly HRV was analyzed using SPSS GEE (generalized estimating equations). HRV improved in massage infant but not in the control infants. Massaged males had greater improvement than massaged females. HRV in massaged infants was on a trajectory comparable to term-born infants by study completion. Massage may improve infant response to exogenous stressors. Massage improves autonomic nervous system development. STRESS AND IMMUNITY
Carcillo JA, Dean JM, Holubkov R, Berger J, Meert KL, Anand KJ, Zimmerman J, Newth CJ, Harrison R, Burr J, Willson CC, Nicholson C. (2011). The randomized comparative pediatric critical illness stress-induced immune suppression (CRISIS) prevention trial. Pediatr Crit Care Med. 2011 Nov 10. [Epub ahead of print]
BIOLOGY OF STRESS (From Shonkoff, Garner, and AAP Committees, 2012 – the Technical Report.) Genetic variability clearly plays a role in stress reactivity, but early experiences and environmental influences have considerable impact. Beginning as early as prenatal period human studies suggest that fetal exposure to maternal stress can influence later stress responsiveness (Oberlander TF, Weinbereg J et al., 2008 Epigenetics, 3(2): 97-106; Brand SR, Engel SM et al., 2006. NY Acad Sci 1071:454-458.). Epigenetic modifications of DNA appear to be likely to play a role in the biological mechanisms explaining these findings (Murgatroyd C, Patchev AV, Wu Y et al., 2009. Dynamic DNA methylation programs persistent adverse effects of early-life stress. Nat Neurosci, 12(12): 1559-1586). EARLY POSTNATAL EXPERIENCES with ADVERSITY are also thought to affect future reactivity to stress, by altering the developing neural circuits controlling these neuroendocrine responses (Roth TL, Lubin FD, Funk AJ, Sweatt JD. 2009. Lasting epigenetic influence of early life adversity on the BDNF gene. Biol Psychiatry, 65(9); 760-769. Szyf M. 2009. The early life environment and the epigenome, Biochim Biophys Acata, 1790(9): 878-885). STRONG SCIENTIFIC CONSENSUS exists that the ecological context MODULATES the expression of one’s genotype , as if experiences confer a signature on the genome to authorize certain characteristic and behaviors and to prohibit others. This concept underscores the need for determining what external and internal factors can be mobilized to protect against the consequences of activation of stress reactivity. Physiologic responses to stress are well defined: activation of hypothalamic-pituitary-adrenocortical axis and sympathetic-adrenomedullary systems, which result in increased levels of STRESS HORMONES, such as Corticotropin-releasing hormone (CRH), coritsol, norepinephrine, and adrenaline. These changes co-occur with elevated inflammatory cytokines and response of the parasympathetic nervous system, which counterbalances both sympathetic activation and inflammatory responses. Transient increases in stress hormones are protective and essential for survival, excessively high levels or prolonged exposures can be harmful or frankly toxic ( McEwen BS. 2005. Stressed or stressed out: w hat is the difference? J Psychiatry Neurosci 30(5): 315-318; McEwen Bs, Seeman T. 1999. Protective and damagning effects of mediators of stress. Elaborating and testing the concepts of allostasis and allostatic load. Ann NY Acad Sci, 896: 30-47.; McEwen BS,. Protective and damaging effects of stress mediators. N Engl J Med 1998: 338(3): 171-179. McEwen BS. 2006. Protective and damaging effects of stress mediators: central role of the brain. Dialogues Clin Neurosci 2006, 8(4): 367-381; McEwen BS, Gianaros PJ 2011: Stress- and allostatic-induced brain plasticity. Annu Rev Med 62: 431- 445. ) The dysregulation of the network of physiologic mediators (i.e. too much/too little cortisol; too much/too little inflammatory response) can lead to chronic “wear and tear” effect on multiple organ systems, including the brain (McEwen articles listed above – the first three). Allostatic load is the cumulative, stress-induced burden on overall body functioning and the aggregated costs, both physiologic and psychological, required for coping and returning to homeostatic balance (citations 38, 42-44 in Shonkoff & Garner Technical Report). The dynamics of stress-mediating systems when repeated or chronic adversity occurs, leads to alterations in their regulation. There are 3 distinct types of stress responses: positive, tolerable, and toxic and the type depends on their potential to cause enduring physiologic disruptions as a result of the intensity and duration of the response (National Scientific Council on the Developing Child . Excessive stress disrupts the architecture of the developing brain: working paper #3. Available at: developing-child.harvard.edu/resources/reports_and_working _ papers/. And Shonkoff JP. 2010. Building a new biodevelopmental framework to guide the future of early childhood policy. Child Dev. 81(1): 357-367. A POSITIVE stress response refers to a physiologic states that is brief and mild to moderate in magnitude. Central to the notion of positive stress is the availability of a caring and responsive adult who helps the child cope with the stressor, thereby providing a protective effect that facilitates the return of the stress response systems back to baseline status. A TOLERABLE stress response is associated with exposure to nonnormative experiences that present a greater magnitude of adversity or threat. Precipitants may be death of family, serious illness or injury, contentious divorce, a natural disaster, terrorism. When experienced in the context of buffering protection provided by supportive adults, risk of excessive stress reactivity and physiologic harm and long-term consequences is reduced. The essential characteristic that makes this form of stress tolerable is the extent to which protective adult relationships facilitate the child’s adaptive coping and sense of control, thereby reducing the physiologic stress response and promoting a return to baseline. The 3rd form of stress is TOXIC STRESS. It results from strong, frequent or prolonged activation of the body’s stress response systems in the absence of the buffering protection of a supportive adult relationship. Thus, being in the incubator is a source of toxic stress to the infant. “The essential characteristic of toxic stress is the disruption of brain circuitry and other organ and metabolic systems during sensitive developmental periods. Such disruption may result in anatomic changes and/or physiologic dysregulations that are the precursors of later impairments in learning and behavior as well as the roots of chronic, stress-related physical and mental illness….. More important, however, is the need for clinical pediatrics to move beyond the level of risk factor identification and to leverage advances in the biology of adversity to contribute to the critical task of developing, testing, and refining new and more effective strategies for reducing toxic stress and mitigating its effects as early as possible before irrevocable damage is done.” Pg. e236) TOXIC STRESS AND THE BRAIN: “Toxic stress in young children can lead to permanent changes in brain structure and function (McEwen BS. 2005. Stressed or stressed out: what is the difference? J Psychiatry Neurosci 30(5): 315-318; McEwen BS, 2006. Protective and damaging effects of stress mediators: central role of the brain. Dialogues Clin Neurosci 8(4): 367-381.) The plasticity of the fetal, infant, and early childhood brain makes it particularly sensitive to chemical influences, and there is growing evidence from human studies that persistently elevated levels of stress hormones can disrupt the brain’s developing architecture (Natl Scientific Council on Developing Child – cited above). Abundant glucocorticoid receptors are found the AMYGDALA, hippocampus, and prefrontal cortex; exposure to stressful experiences alters the size and neuronal architecture of these areas and leads to functional differences in learning, memory, and aspects of executive functioning” pg. e 236). CHRONIC STRESS is associated with hypertrophy and overactivity of the amygdala and orbitofrontal cortex, and comparable levels of adversity (chronic stress) can lead to loss of neurons and neuronal connection in the hippocampus and medial prefrontal cortex. Functional consequences of these structural changes include more anxiety (2ary to hyperactivation of amygdala (which also leads to atherosclerosis in later life), less top-down control due to prefrontal cortex atrophy as well as impaired memory and mood control as a consequence of hippocampal reduction. “The developing architecture of the brain can be impaired in numerous ways that create a weak foundation for later learning, behavior, and health.”pg. e236
Amygdala mediates fear and anxiety, and also activates physiologic stress response: amygdala’s stimulation activates sympathetic activity and causes neurons in the hypothalamus to release CRH. CRH in turn signals pituitary to release adrenocorticotrophic hormone, which then stimulates adrenal glands to increase serum cortisol concentrations. The amygdala, facilitating the establishment of a positive feedback loop. Significant stress in early childhood can trigger amygdale hypertrophy and results in a hyperresponsive or chronically activated physiologic stress response, along with increased potential for fear and anxiety (Natl Scientific Council on the Developing Child: Persistent fear and anxiety can affect youind children’s learning and development: working paper #9. Available at www.developingchild.net; Tottenham N, Hare TA, Quinn Bt et al. 2010. Prolonged institutional rearing is associated with atypically large amygdale volume and difficulties in emotion regulation. Dev Sci 13(1): 46- 61.) Although the hippocampus can turn off elevated cortisol, chronic stress diminishes its capacity to do so and can lead to impairments in memory and mood-related functions that are located in this brain region. Exposure to chronic stress and high levels of cortisol also inhibit neurogenesis in the hippocampus, which is believed to play important role in encoding of memory and other functions. Toxic stress limits the ability of the hippocampus to promote contextual learning, making it difficult to discriminate danger vs safety conditions. “Altered brain architecture in response to toxic stress could explain in part the strong association between early adverse experiences and subsequent problems in development of linguistic, cognitive, and social-emotional skills, all of which are inextricably intertwined in the wiring of the developing brain (Tottenham above).
Prefrontal cortex also turns off cortisol response and has role in top-down regulation of autonomic balance (sympathetic vs parasympathetic effects), development of executive function (decision making, working memory, behavioral self-regulation, mood and impulse control.) Pfc also suppresses AMYGDALA activity, allowing for more adaptive responses to threatening /stressful experiences, but high levels of cortisol and exposure to stress changes neuronal connectivity in PFC, limiting its ability to inhibit amydala activity and impairing adaptive responses to stress. Thus HIPPOCAMPUS and PFC modulate amygdala’s initiation of stress responses, but chronic or toxic stress changes in the architecture and connectivity within and between these areas accounts for the variability in stress responsiveness (Boyce WT, Ellis BJ. Dev Psychopathol 2005, 17(2): 271-301). The consequences of Adverse Childhood Experiences (ACE) is greater risk for a variety of chronic diseases well into adult years. There is strong link between ACE and health threatingeng behaviors. The extent to swhich cumulative burden of stress over time and timing of specific environmental insults during sensitive developmental periods creates structural and fucnctional disruptions that lead to wide range of physical and mental illnesses later in adult life.Pg. e237. “SIGNIFICANT REDUCTIONS IN CHRONIC DISEASE COULD BE ACHIEVED OVER THE LIFE COURSE BY DECREASING THE NUMBER AND SEVERITY OF ADVERSE EXPERIENCES THAT THREATEN THE WELLBEING OF YOUNG CHILDREN AND BY STRENGTHING THE PROTECTIVE RELATIONSHIP THAT MITIGATES THE HARMFUL EFFECTS OF TOXIC STRESS.” (P. E239)
Feldman R, Gordon I, Zagoory-Sharon O.(2011). Maternal and paternal plasma, salivary, and urinary oxytocin and parent-infant synchrony: considering stress and affiliation components of human bonding. Dev Sci. 2011 Jul;14(4):752-61. doi: 10.1111/j.1467-7687.2010.01021.x. Studies in mammals have implicated the neuropeptide oxytocin (OT) in processes of bond formation and stress modulation, yet the involvement of OT in human bonding throughout life remains poorly understood. We assessed OT in the plasma, saliva, and urine of 112 mothers and fathers interacting with their 4-6-month-old infants. Parent- infant interactions were micro-coded for parent and child's social behaviors and for the temporal coordination of their socio-affective cues. Parents were interviewed regarding their attachment to the infant and reported on bonding to own parents, romantic attachment, and parenting stress. OT in plasma (pOT) and saliva (sOT) were inter-related and were unrelated to OT in urine (uOT). pOT and sOT in mothers and fathers were associated with parent and child's social engagement, affect synchrony, and positive communicative sequences between parent and child. uOT was related to moments of interactive stress among mothers only, indexed by the co-occurrence of infant negative engagement and mother re- -engagement attempts. pOT and sOT were associated with mothers' and fathers' attachment relationships throughout life: to own parents, partner, and infant, whereas uOT correlated with relationship anxiety and parenting stress among mothers only. Similar to other mammals, OT is involved in human attachment and contingent parenting. The dual role of OT in stress and affiliation underscores its complex involvement in processes of social bonding throughout life. Lemyre L, Tessier R(2003). Measuring psychological stress. Concept, model, and measurement instrument in primary care research.Can Fam Physician. 2003 Sep;49:1159- 60, 1166-8
Smith GC, Gutovich J, Smyser C, Pineda R, Newnham C, Tjoeng TH, Vavasseur C, Wallendorf M, Neil J, Inder T.(2011) Neonatal intensive care unit stress is associated with brain development in preterm infants. Ann Neurol. 2011 Oct;70(4):541-9. doi: 10.1002/ana.22545. Epub 2011 Oct 4.
Milgrom J, Newnham C, Anderson PJ, Doyle LW, Gemmill AW, Lee K, Hunt RW, Bear M, Inder T.(2010) Early sensitivity training for parents of preterm infants: impact on the developing brain. Pediatr Res. 2010 Mar;67(3):330-5. doi: 10.1203/PDR.0b013e3181cb8e2f.
**Newnham CA, Inder TE, Milgrom J.(2009). Measuring preterm cumulative stressors within the NICU: the Neonatal Infant Stressor Scale. Early Hum Dev. 2009 Sep;85(9):549-55. doi: 10.1016/j.earlhumdev.2009.05.002. Epub 2009 Jun 10.
MEASURING STRESS
Ng, S.M., Drury, J.A., Turner,M.A, Didi, M., Victor, S., Newland, P., & Weindling, A.M. (2013). A novel method of collection of saliva for estimation of steroid levels in extremently premature infants. Acta Paediatrica 102, 356-359. Doi: 10.1111/apa.12146. Salivary collection is less invasive than blood collection. Previous methods of saliva collection have been poorly tolerated and inaccuaragte. They collected saliva from 23-27 weekers using four standard swabs by placing one commercial SALIVETTE swab at a time in the infnat’s mouth for 1-3 minutes. No salivary stimulants were used. Had 85% success rate in obtaining a mean of 150 microliters of saliva (range 50-350μL) by trained staff. NO AEs..