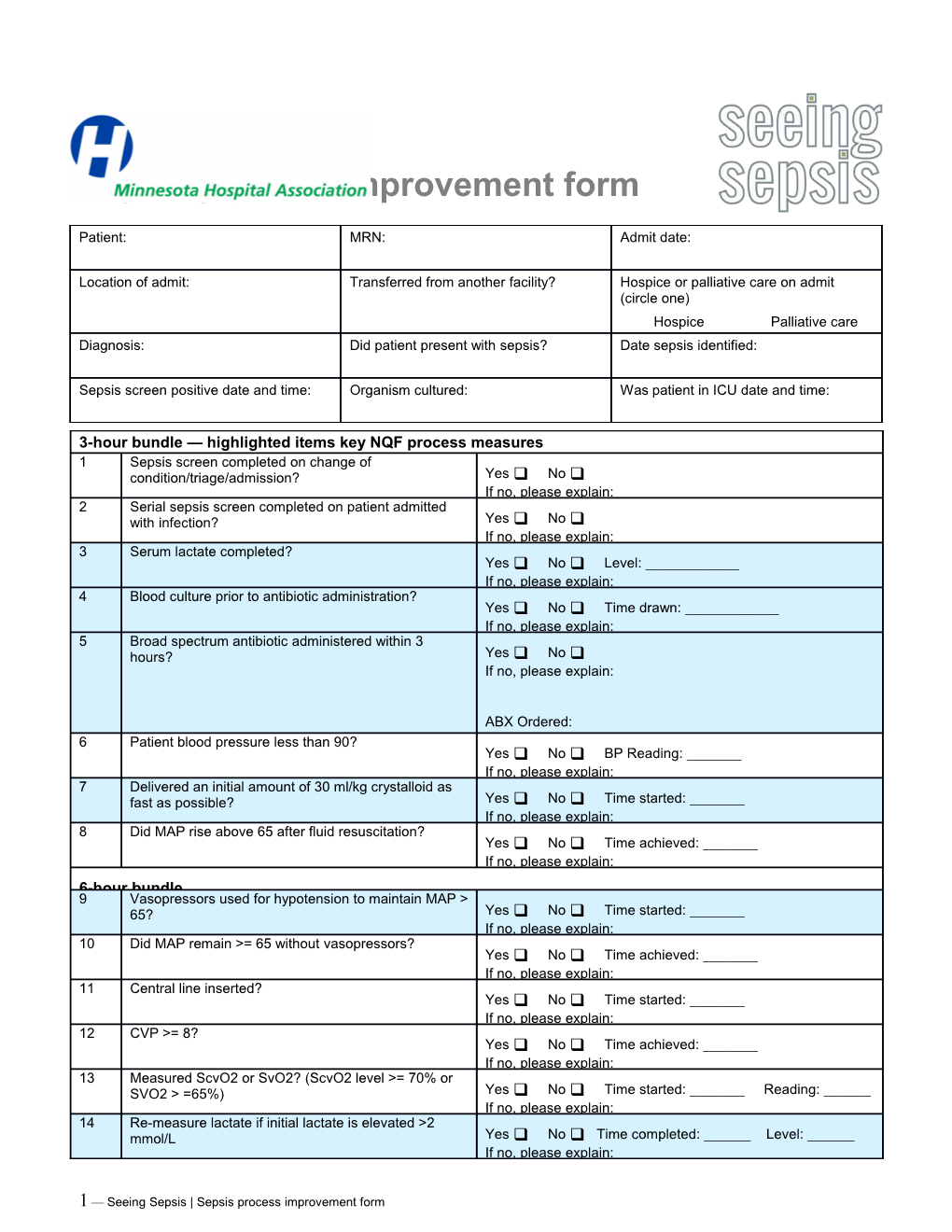
Sepsis process improvement form
Patient: MRN: Admit date:
Location of admit: Transferred from another facility? Hospice or palliative care on admit (circle one) Hospice Palliative care Diagnosis: Did patient present with sepsis? Date sepsis identified:
Sepsis screen positive date and time: Organism cultured: Was patient in ICU date and time:
3-hour bundle — highlighted items key NQF process measures 1 Sepsis screen completed on change of condition/triage/admission? Yes No If no, please explain: 2 Serial sepsis screen completed on patient admitted with infection? Yes No If no, please explain: 3 Serum lactate completed? Yes No Level: ______If no, please explain: 4 Blood culture prior to antibiotic administration? Yes No Time drawn: ______If no, please explain: 5 Broad spectrum antibiotic administered within 3 hours? Yes No If no, please explain:
ABX Ordered: 6 Patient blood pressure less than 90? If no, please explain: Yes No BP Reading: ______If no, please explain: 7 Delivered an initial amount of 30 ml/kg crystalloid as fast as possible? Yes No Time started: ______If no, please explain: 8 Did MAP rise above 65 after fluid resuscitation? Yes No Time achieved: ______If no, please explain: 6-hour bundle 9 Vasopressors used for hypotension to maintain MAP > 65? Yes No Time started: ______If no, please explain: 10 Did MAP remain >= 65 without vasopressors? Yes No Time achieved: ______If no, please explain: 11 Central line inserted? Yes No Time started: ______If no, please explain: 12 CVP >= 8? Yes No Time achieved: ______If no, please explain: 13 Measured ScvO2 or SvO2? (ScvO2 level >= 70% or SVO2 > =65%) Yes No Time started: ______Reading: ______If no, please explain: 14 Re-measure lactate if initial lactate is elevated >2 mmol/L Yes No Time completed: ______Level: ______If no, please explain:
1 — Seeing Sepsis | Sepsis process improvement form 15 Critical Care Unit discharge Yes No Date/Time: ______If no, please explain: RCA factors 16 Was equipment availability a factor? Yes No If yes, please explain: 17 Was staff training a factor? Yes No If yes, please explain: 18 Was the correct laboratory testing available? Yes No If no, please explain: 19 Were antibiotics available at the proper time? Yes No If no, please explain: 20 Was central-line insertion available within 3 hours of identification? Yes No If no, please explain: 21 Was there a delay in diagnosis? Yes No If yes, please explain: 22 Was communication a factor? Yes No If yes, please explain: Comments:
Conclusions:
Issue Plan of Action Completion Deadline/Person Progress Summary Responsible
Reviewing staff (please list): ______
Completed by: ______Name Date Time Surviving sepsis campaign bundles: 3-hour bundle and 6-hour bundle from: Dellinger RP, Levy MM, Rhodes MB et al: Surviving Sepsis Campaign: International Guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 2013; 41 (2) “Reproduced with permission of the publisher. Copyright 2012 Society of Critical Care Medicine and European Society of Intensive Care Medicine.”
Surviving sepsis campaign bundles: 3-hour bundle and 6-hour bundle from: Dellinger RP, Levy MM, Rhodes MB et al: Surviving Sepsis Campaign: International Guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 2013; 41 (2) “Reproduced with permission of the publisher. Copyright 2012 Society of Critical Care Medicine and European Society of Intensive Care Medicine.”