RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, BANGALORE, KARNATAKA ANNEXURE –II
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
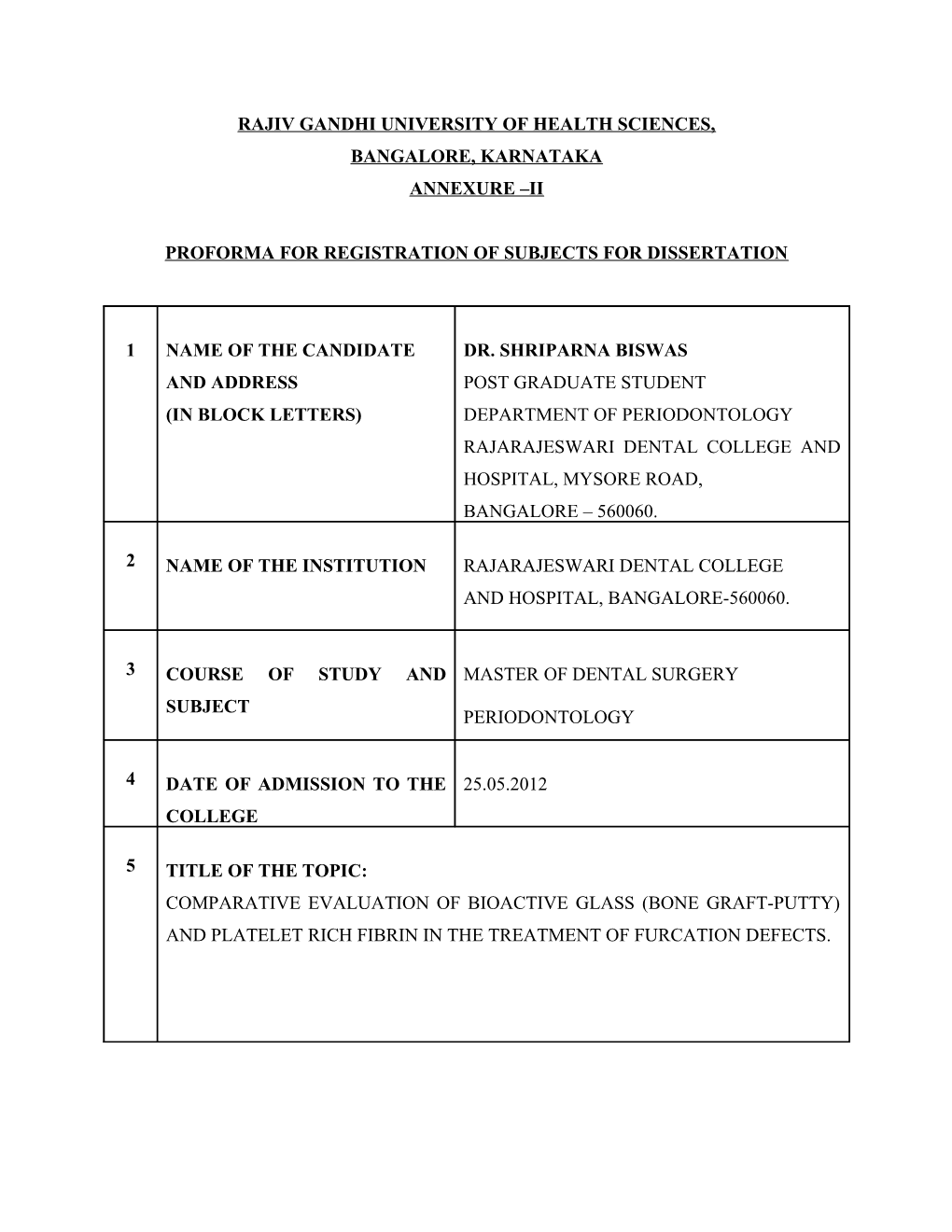
1 NAME OF THE CANDIDATE DR. SHRIPARNA BISWAS AND ADDRESS POST GRADUATE STUDENT (IN BLOCK LETTERS) DEPARTMENT OF PERIODONTOLOGY RAJARAJESWARI DENTAL COLLEGE AND HOSPITAL, MYSORE ROAD, BANGALORE – 560060.
2 NAME OF THE INSTITUTION RAJARAJESWARI DENTAL COLLEGE AND HOSPITAL, BANGALORE-560060.
3 COURSE OF STUDY AND MASTER OF DENTAL SURGERY SUBJECT PERIODONTOLOGY
4 DATE OF ADMISSION TO THE 25.05.2012 COLLEGE
5 TITLE OF THE TOPIC: COMPARATIVE EVALUATION OF BIOACTIVE GLASS (BONE GRAFT-PUTTY) AND PLATELET RICH FIBRIN IN THE TREATMENT OF FURCATION DEFECTS. 6 BRIEF RESUME OF THE INTENDED WORK:
6.1 NEED FOR THE STUDY :
Management of molars with furcation involvement has been one of the most
challenging problems in periodontal therapy. Teeth with furcation involvement undergo more
extensive and rapid clinical attachment loss and are lost with greater frequency than are single
rooted teeth.1
Multiple approaches have been used to resolve furcation defect including autografts,
demineralized freeze-dried bone allografts (DFDBAs), bovine-derived xenografts, barrier
membranes and combinations of membranes and bone grafts.2
An alloplast is a biocompatible, inorganic synthetic bone grafting material. At
present, alloplasts marketed for periodontal regeneration fall into two broad classes: ceramics
and polymers. Among the different alloplastic materials used in periodontal therapy,
hydroxyapatite, calcium phosphates and bioactive glass ceramics have the capacity to form a
carbonated hydroxyapatite layer on their surfaces once exposed to simulated body fluids or
implanted in vivo, hence the concept of “bioactivity.” The material is easy to manipulate and
is hemostatic. Bioglass stimulates osteoblasts to produce more bone tissue than other
synthetic biomaterials which lead to the concept of “osteoproduction” and
“osteostimulation.”.3
Platelet rich fibrin (PRF), first described by Choukron et al in France, is a 2nd
generation platelet concentrate for surgical use. PRF is an autologous leukocyte and platelet
rich fibrin biomaterial. Potential clinical indications of PRF include improvement in soft
tissue healing and bone graft protection and remodeling. Unlike other platelet concentrates,
this technique does not require any anticoagulants or bovine thrombin or any other gelling agent. This open protocol is very simple and inexpensive.4
The purpose of the present study is clinical and radiographical evaluation and comparison of the efficacy of bioactive glass bone graft putty material and PRF in the treatment of furcation defects.
6.2 REVIEW OF LITERATURE: A study was conducted to compare the clinical attachment gain as well as vertical and
horizontal bone fill obtained with open flap debridement (OFD) alone and OFD with
bioactive glass particulate in the treatment of mandibular Class II furcation defects.
Twenty mandibular class II furcation defects were selected in 16 systemically healthy
patients out of which 10 defects were treated with OFD alone (Group I) and other 10
defects were treated with OFD and bioactive glass particulate (Group II). Each defect
was randomly assigned to Group I and Group II. The soft tissue and hard tissue
measurements including vertical probing depth, horizontal probing depth, clinical
attachment level, gingival recession, vertical depth of the furcation defects, and
horizontal depth of the furcation defects were recorded at baseline and six months post
surgery. In conclusion, bioactive glass showed significant improvement in clinical
parameters like vertical and horizontal defect fill in mandibular class II furcation
defects when compared to OFD.1
In one of the studies which was designed to evaluate the effectiveness of
autologous PRF in the treatment of mandibular degree II furcation defects compared
with open flap debridement (OFD) Using a split-mouth design, 18 patients with 36
mandibular degree II furcation defects were randomly allotted and treated either with
autologous PRF and OFD or OFD. Clinical and radiographic measurements were
recorded at baseline and 9 months postoperatively. All clinical and radiographic
parameters showed statistically significant improvement at the sites treated
with PRF and OFD compared to those with OFD alone.2
In a study which was conducted to compare the clinical parameters of probing depth and bleeding on probing using a bioactive glass particulate to open flap debridement
alone in human mandibular class II furcations. 15 patients were included in the study
with moderate to advanced adult periodontitis. Each patient received surgical therapy
consisting of regenerative therapy using bioactive glass compared to open flap
debridement in the furcation defects. The results of therapy were statistically
significant in the defects treated with bioactive glass, regarding the clinical parameters
of probing depth reduction and the reduction in bleeding on probing.5
In this study which was conducted to evaluate the efficacy of a bioactive alloplast,
PerioGlas, in comparison with open flap debridement in intra bony defects. 8
systemically healthy volunteers were chosen, each having 2 collateral sites with ≥6
mm clinical probing depth and radiographic evidence of an intrabony defect.
Randomly, one defect was treated with open flap debridement plus bioactive glass
(test) and the other with open flap debridement alone (control). Measurements were
recorded at baseline, 3, 6, 9 months. Both treatments showed no significant
differences between the two groups at any point of time. However, radiographically,
bioactive glass group showed significant improvement in bone fill over the sites
treated with open flap debridement alone. The alloplastic bone graft material,
PerioGlas, demonstrated clinical advantages beyond that achieved by debridement
alone.6
A study was designed to evaluate the efficacy of bioactive glass in the management of furcation defect associated with an endo perio lesion. A 22 year old patient with an
endo-perio lesion in the right mandibular first molar was treated. The defect was
initially treated with endodontic therapy. Following the endodontic treatment, the
furcation defect was treated using bioactive glass in a putty form. At the end of 9
months, there was gain in clinical attachment level and reduction in probing depth.
Radiographic evidence showed that there was a significant bone fill.7
A study was conducted to investigate the clinical and radiological effectiveness of
autologous PRF in the treatment of intra-bony defects of chronic periodontitis
patients. 32 intrabony defects were treated. By using the image analysis software
intra-bony defect fill was calculated on standardized radiographs (from the baseline
and 9 months). For all clinical and radiographic parameters test group was performed
better than control group, and the difference was found to be statistically significant.
Furthermore, image analysis revealed significantly greater bone fill in the test group
compared with control group. There was greater reduction in PD, more CAL gain and
greater intra-bony defect fill at sites treated with PRF than the open flap debridement
alone.8
6.3 AIMS AND OBJECTIVES OF THE STUDY: To evaluate the clinical and radiographic efficacy of Bioactive glass bone graft putty
material and platelet rich fibrin in the treatment of Grade II furcation defects.
To compare the clinical and radiographic efficacy of Bioactive glass bone graft putty
material and platelet rich fibrin in the treatment of Grade II furcation defects.
7 MATERIALS AND METHODS :
7.1 SOURCE OF DATA
Patients visiting to the Department of Periodontology, Rajarajeswari Dental College and
Hospital, Bangalore.
7.2 METHOD OF COLLECTION OF DATA :
20 mandibular molar furcation defects will be randomly selected from chronic periodontitis
patients belonging to the age group of 20-50 years and will be grouped as follows:
Group I – 10 furcation defects to be treated using Bioactive glass bone graft putty material.
Group II – 10 furcation defects to be treated using platelet rich fibrin.
INCLUSION CRITERIA :
1. Chronic periodontitis patients.
2. Presence of grade II furcation defects in mandibular molars (Glickman’s
classification).9
3. Systemically healthy patients. EXCLUSION CRITERIA
1. Smokers.
2. Patients on any medication taken within the last 6 months which may alter the
periodontal status.
3. Pregnant and lactating mothers.
4. Patients who have undergone periodontal treatment within a period of 1 year.
SCREENING EXAMINATION INCLUDE
Gingival index by Loe H & Silness P, 1963.
Plaque index by Silness P & Loe H, 1964.
Vertical probing depth to be measured using graduated William’s periodontal probe.
Horizontal measurement of the furcation defect using a Naber’s probe and using
customized occlusal stents.
Gingival margin position measured from a fixed reference point to gingival margin
using a customized stent.
Clinical attachment level measured from CEJ to the base of the pocket.
Standardized radiographs of the defect sites will be taken using radiovisiograph
(RVG) and IOPAR film grids to measure the amount and density of bone fill.
DURATION OF THE STUDY: 18 Months PROCEDURE:
Each patient will be informed and signature will be taken on a consent form after explaining the nature of the study. All patients will undergo scaling, root planing, oral hygiene instructions, and occlusal adjustment wherever indicated. Prior to surgery, two customized acrylic stents will be fabricated, one for gingival margin position and other for furcation depth. Measurements for clinical parameters will be recorded from the fixed reference point (stent). All measurements will be recorded by a single investigator. The cases will then be reevaluated. Only when the patient demonstrates adequate plaque control, periodontal surgery will be performed. In each pair of furcation defects, one site will be assigned for treatment with autologous platelet rich fibrin and the other one will be treated with Bioactive glass bone graft putty material. The surgical procedure will be performed under local anesthesia. The postoperative evaluation and data collection will be done at 3, 6 and 9 months. The clinical parameters to be recorded are:
Soft tissue parameters (using stent):
Pocket depth (from gingival margin to base of the pocket)
Clinical attachment level
Hard tissue parameters:
Horizontal probing depth of furcation involvement (using stent)
Radiographic analysis and density measurement of defect site
STATISTICAL ANALYSIS: Following tests of statistics will be used in the present study:
1. Mann-Whitney U test- to compare the result between test site and control site.
2. Wilcoxon sign Rank Sum Test- to compare the results between the various time
intervals.
7.3 Does the study require any investigations or interventions to be conducted on
patients or other human or animals? If so, please describe briefly :
Yes.
The study requires patients to undergo periodontal surgery and radiographic evaluation of
the treated sites pre and post operatively.
7.4 Has ethical clearance been obtained from your institution in case 7.3?
Yes.
Ethical clearance letter has been attached.
LIST OF REFERENCES: 8 1. Manoj H, Dilip GN, Ashita SU. A clinical evaluation of bioactive glass particulate in
the treatment of mandibular class II furcation defects. Braz J Oral Sci 2007;6:1450-
1456.
2. Sharma A, Pradeep AR. Autologous Platelet-Rich Fibrin in the Treatment of
Mandibular Degree II Furcation Defects: A Randomized Clinical Trial. J Periodontol
2011;82:1396-1403.
3. Dumitrescu AL. Bone Grafts and Bone Graft Substitutes. Verlag Berlin
Heidelberg:Springer 2011;9:73-144.
4. David M, Ehrenfest D, Corso DM, Diss A, Mouhyi J, Charrier JB. Three-Dimensional
Architecture and Cell Composition of a Choukroun’s Platelet-Rich Fibrin Clot and
Membrane. J Periodontol 2010;81:546-555.
5. Anderegg CR, Alexander DC, Freidman M. A Bioactive Glass Particulate in the
Treatment of Molar Furcation Invasions. J Periodontol 1999;70:384-387.
6. Subbaiah R, Thomas B. Efficacy of a bioactive alloplast, in the treatment of human
periodontal osseous defects-a clinical study. Med Oral Patol Oral Cir Bucal 2011;16 :
239-244.
7. Narang S, Narang A, Gupta R. A Sequential Approach in treatment of Perio-endo
Lesion. J Indian Soc Periodontol 2011;15:177-180.
8. Thorat MK, Pradeep AR, Pallavi B. Clinical effect of autologous platelet-rich fibrin in
the treatment of intra-bony defects: a controlled clinical trial. J Clin Periodontol 2011;
38: 925–932.
9. Ammons WF, Harrington GW. Furcation, The Problem and Its Management. In Newman, Takei, Carranza, editors:Carranza's Clinical Periodontology 9th Edition.
Philadelphia: W.B. Saunders Co.2002:825-839. 9. SIGNATURE OF CANDIDATE
10. REMARKS OF THE GUIDE
11. 11.1 NAME AND DESIGNATION DR. SAVITA.S M.D.S OF THE GUIDE PROFESSOR AND HEAD
DEPARTMENT OF PERIODONTOLOGY RAJARAJESWARI DENTAL COLLEGE & HOSPITAL, MYSORE ROAD, BANGALORE- 60. 11.2 SIGNATURE
11.3 CO- GUIDE DR. NALINI.M.S MDS READER DEPARTMENT OF PERIODONTOLOGY RAJARAJESWARI DENTAL COLLEGE & HOSPITAL, MYSORE ROAD, BANGALORE- 60.
11.4 SIGNATURE
11.5 HEAD OF THE DR. SAVITA. S M.D.S DEPARTMENT PROFESSOR AND HEAD DEPARTMENT OF PERIODONTOLOGY RAJARAJESWARI DENTAL COLLEGE & HOSPITAL, MYSORE ROAD, BANGALORE- 60. 11.6 SIGNATURE
12. 12.1 REMARKS OF THE CHAIRMAN AND PRINCIPAL
12.2 SIGNATURE