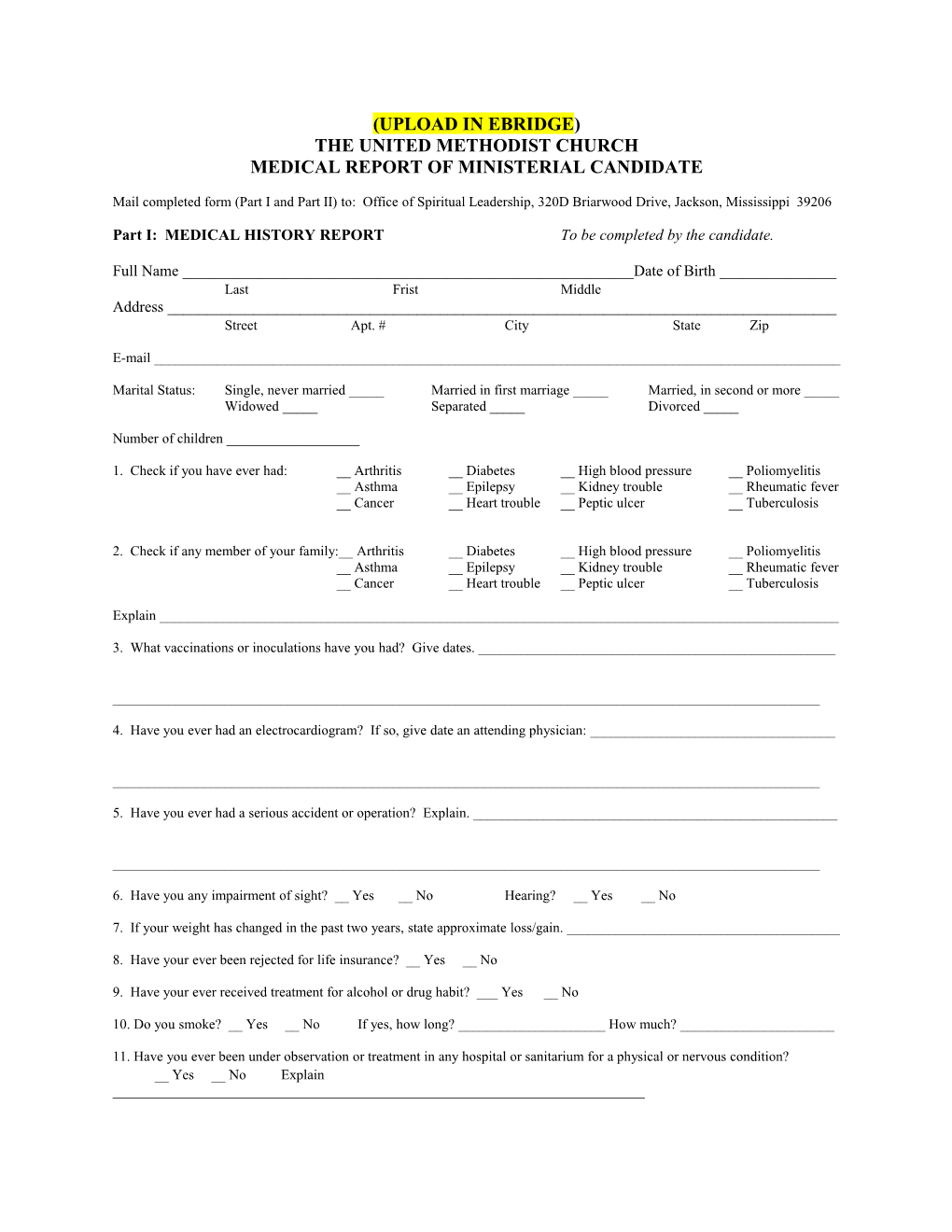
(UPLOAD IN EBRIDGE) THE UNITED METHODIST CHURCH MEDICAL REPORT OF MINISTERIAL CANDIDATE
Mail completed form (Part I and Part II) to: Office of Spiritual Leadership, 320D Briarwood Drive, Jackson, Mississippi 39206
Part I: MEDICAL HISTORY REPORT To be completed by the candidate.
Full Name ______Date of Birth ______Last Frist Middle Address ______Street Apt. # City State Zip
E-mail ______
Marital Status: Single, never married _____ Married in first marriage _____ Married, in second or more _____ Widowed _____ Separated _____ Divorced _____
Number of children ______
1. Check if you have ever had: __ Arthritis __ Diabetes __ High blood pressure __ Poliomyelitis __ Asthma __ Epilepsy __ Kidney trouble __ Rheumatic fever __ Cancer __ Heart trouble __ Peptic ulcer __ Tuberculosis
2. Check if any member of your family:__ Arthritis __ Diabetes __ High blood pressure __ Poliomyelitis __ Asthma __ Epilepsy __ Kidney trouble __ Rheumatic fever __ Cancer __ Heart trouble __ Peptic ulcer __ Tuberculosis
Explain ______
3. What vaccinations or inoculations have you had? Give dates. ______
______
4. Have you ever had an electrocardiogram? If so, give date an attending physician: ______
______
5. Have you ever had a serious accident or operation? Explain. ______
______
6. Have you any impairment of sight? __ Yes __ No Hearing? __ Yes __ No
7. If your weight has changed in the past two years, state approximate loss/gain. ______
8. Have your ever been rejected for life insurance? __ Yes __ No
9. Have your ever received treatment for alcohol or drug habit? ___ Yes __ No
10. Do you smoke? __ Yes __ No If yes, how long? ______How much? ______
11. Have you ever been under observation or treatment in any hospital or sanitarium for a physical or nervous condition? __ Yes __ No Explain ______The above statements are true and accurate to the best of my knowledge.
Signature ______Date ______
PART II: MEDICAL EXAMINER’S REPORT To be completed by the physician.
1. General Appearance ______
2. Personal Hygiene ______
3. Height ______Weight ______
4. Temperature ______Pulse ______Blood pressure ______(Give readings before Temperature ______Pulse ______Blood pressure ______and after exercise)
5. Vision ______
6. Hearing ______
7. Condition of mouth and throat: ______Pharynx ______Tonsils ______Mucous Membranes ______Teeth ______Tongue ______Gum ______
8. Evidence of goiter, enlarged glands, or other tumors ______
______
9. Evidence of varicosity ______Heart ______Lungs ______Thorax ______Spine ______Genitalia ______
10. Evaluate nervous and mental condition ______
______
Laboratory Tests (required) Pap Smear (for all women) ______Mammogram ______PSA (for men over 50) ______Cholesterol ______Fasting Blood Sugar ______
SUMMARY OF FINDINGS AND RECOMMENDATIONS
______
______
______
Name of physician (Type or print) ______
Address ______Street City State Zip
Signature of Physician ______
Form 103