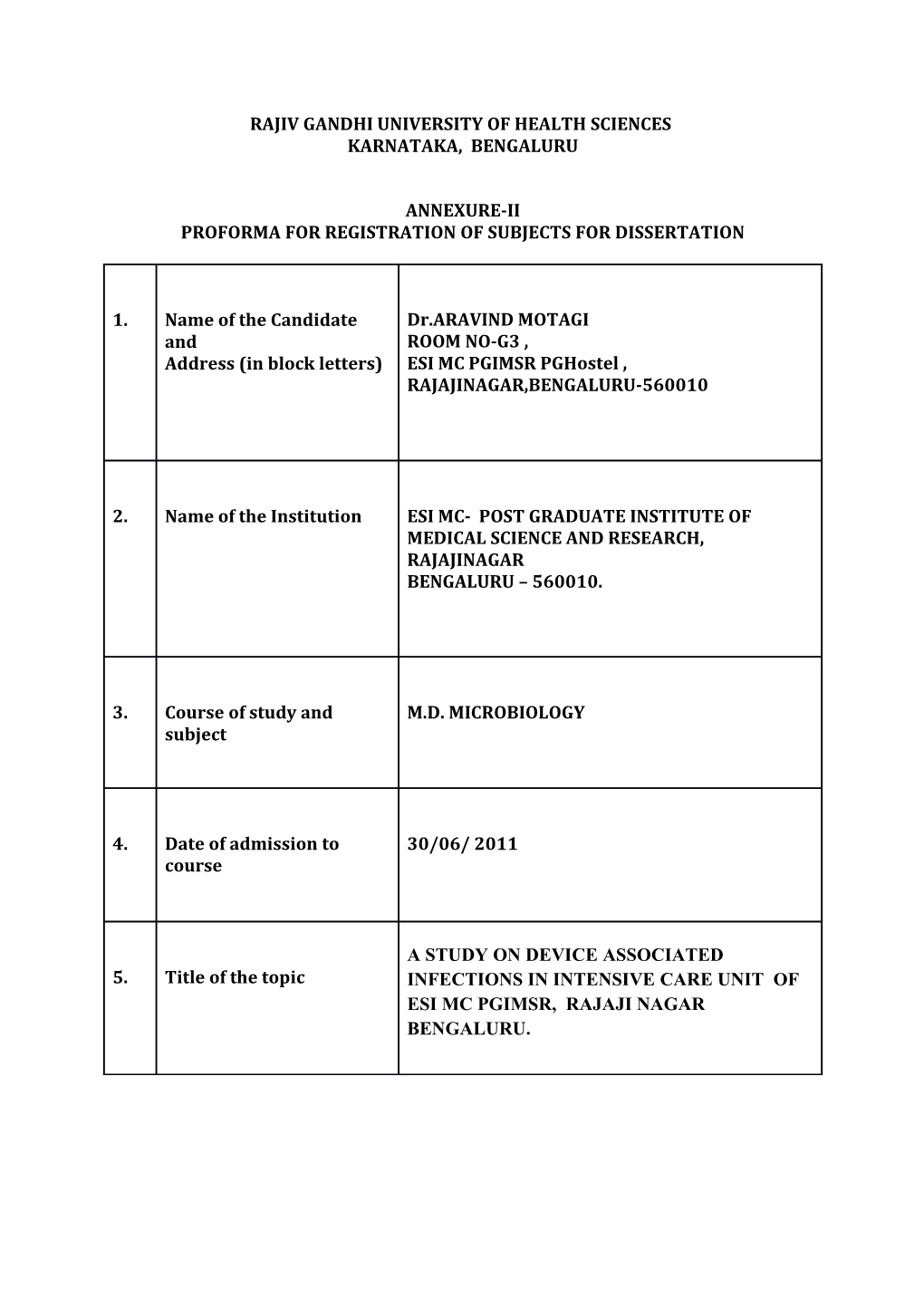
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES KARNATAKA, BENGALURU
ANNEXURE-II PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
1. Name of the Candidate Dr.ARAVIND MOTAGI and ROOM NO-G3 , Address (in block letters) ESI MC PGIMSR PGHostel , RAJAJINAGAR,BENGALURU-560010
2. Name of the Institution ESI MC- POST GRADUATE INSTITUTE OF MEDICAL SCIENCE AND RESEARCH, RAJAJINAGAR BENGALURU – 560010.
3. Course of study and M.D. MICROBIOLOGY subject
4. Date of admission to 30/06/ 2011 course
A STUDY ON DEVICE ASSOCIATED 5. Title of the topic INFECTIONS IN INTENSIVE CARE UNIT OF ESI MC PGIMSR, RAJAJI NAGAR BENGALURU. 6. BRIEF RESUME OF THE INTENDED WORK: 6.1 NEED FOR THE STUDY: Nosocomial Infection(NI) is defined as infection that is acquired in a hospital (i.e., the infection was not present/ incubatory at the time of admission). For most bacterial infections, an onset of symptoms more than 48 hrs after admission is evidence of nosocomial acquisition. [1] Nosocomial infection rates are one of the most important indicators of the quality of health services.[2] NIs are frequently encountered in Intensive Care Units (ICUs) because of severity of underlying diseases, the frequency of invasive interventions, and the frequent use of wide spectrum antibiotics.[3] It has been reported that ICUs account for 25% of NIs, even though they occupy only approximately 10% of the bed capacity of a hospital.[4] The vast majority of NIs are related to devices (e.g., urinary tract catheters, endotracheal tubes in ventilated patient and central venous catheter). The premise upon which infection control programs operate is that many of these life threatening and costly NIs are preventable.[1] Surveillance of Device associated infections (DAIs) can reduce the incidence of NIs by as much as 32% & lead to reduced health care costs. DAIs such as Ventilator Associated Pneumonia (VAP), Central Line Associated Blood Stream Infections (CLA-BSI) & Catheter Associated Urinary Tract Infections (CA-UTI) have greatest challenge to hospital safety & quality health care in ICU patients.[5] The frequency of such infections, particularly in ICUs , the agents & their resistance rates should be identified in order to better control infections.[2] There is a limited data available on DAIs in the present hospital & also there is a need to create a baseline antibiotic susceptibility pattern to various organisms isolated from device associated infections in ICU so as to provide information to assist in effective infection control program of the hospital. Hence the present study. 6.2 REVIEW OF LITERATURE: The early twentieth century, the discovery of pathogenic bacteria provided a new basis for the study of hospital infection. Though Dukes (1929) recognized the importance of the indwelling urinary catheter, as a means of introducing infection into the bladder; this was forgotten. Later; this idea was reviewed with introduction of closed drainage systems by Gillespie, 1956 & Kunin & Mc Conmack, 1966. Antibiotic treatment & hospital infection control are intimately entwined. The use of antibiotics although not the only influence, has altered the prevailing pathogens in hospital infection. S. pyogenes was almost banished & later, resistant gram negative bacteria replaced S. aureus. Then gram positive bacteria, S.aureus, Coagulase Negative Staphylococcus (CONS), Entercocci & Clostridium difficile re-emerges. The emergence of gram negative bacteria such as Pseudomonas aeruginosa, Klebsiella spp with Extended Spectrum beta-lactamases (ESBLs), Stenotrophomonas maltophilia & Acinetobacter baumanni has occupied much attention recently. The development of multiple resistance in hospital pathogens, without the prospect of new antibiotics to deal with them is alarming.[6] Antimicrobial resistance poses a particular challenge to developing countries where 45% of deaths are due to infectious diseases. Targeted surveillance & calculation of DAI rates per 1000 invasive device – days allows bench marking with other different institutions in the same/even different countries and facilitates detection & improvement of institutional problems because specific risk factor is included in the rate calculation.[5] The Centers for Disease Control Prevention(CDC) definition of DAI is an infection in patient with a device (e.g. ventilator/central line/urinary tract catheters) that was used within 48 hour period before onset of infection. If the interval is longer than 48hrs, there must be compelling 7. evidence that the infection was associated with device used CA-UTI is defined as urinary tract infection in a patient who had an indwelling urinary catheter at the time of or within 48 hours before onset of the event.[7] Most health care associated infection of urinary tract is associated with urethral catheterization. Even the single passage of a catheter is associated with a definite, though usually low infection risk. Inspite of closed drainage, bladder colonization nevertheless occurs. It may reach about 10% of patients/day. The root of infection is not via the lumen of catheter, but between catheter & the urethral wall. Early infection caused by local commensals & late infection caused by more resistant hospital associated gram negative bacteria. Bladder bacteriuria is benign & symptomless in many patients. It prolongs hospital stay & worsen prognosis.[6] VAP is defined as pneumonia in a patient who was intubated & ventilated at the time of, or within 48 hours before, the onset of the event.[7] It is categorised as early onset VAP, which occurs within 4 days & late onset VAP, which occurs after 4 days of endo-tracheal intubation. This classification also helps in predicting the implicated pathogens & guides us in the initial empiric therapy with antibiotics.[8] CLA-BS is defined as blood stream infection in a patient who had a central line at the time of, or within 48 hours before, onset of the event.[7] Blood stream infections related to central line associated constitute one of the major nosocomial device associated infections.[9] 6.3 OBJECTIVES OF THE STUDY: 1. To know the occurrence of device associated infection rate in ICU. 2. To know the bacterial profile of various device associated infections. 3. To know the antibiotic resistance pattern & common resistance mechanisms of the iso- lates from these infections. MATERIALS & METHODS: 7.1 SOURCE OF DATA: Data will be collected from the patient’s case sheets admitted to 6 bedded recently established intensive care unit of ESI MC PGIMSR Teaching Hospital, Rajajinagar, Bengaluru. STUDY PERIOD: One year SAMPLE SIZE: Minimum of 1000 devices will be screened for device associated infections according to CDC criteria. INCLUSION CRITERIA: According to CDC definitions[7] 1) Ventilator Associated Pneumonia (VAP) : Adult patient on mechanical ventilation at the time of or within 48 hours before onset of the event and showing radiological evidence of pneumonia and Any 2 of the following: Temperature ≥ 380C or ≤350C WBC >12000/mm3 or <4000/mm3 Purulent sputum Pathogenic bacteria isolated from endo tracheal aspirate. 2) Catheter Associated Urinary Tract Infection( CA-UTI ): Adult patient with an indwelling urinary catheter at the time of or within 48 hours before onset of the event & 8. microorganisms seen on Gram stain of unspun urine and a positive urine culture of ≥103 and <105 CFU/ml with no more than 2 species of microorganisms. 3) Central Line Associated-Blood Stream Infection (CLA– BSI ): Adult patient with central line at the time of, or within 48 hours before onset of event, must meet any one of the criteria : Fever (≥380C) or chills or hypotension (systolic <90) and Signs & symptoms & positive lab results not related to infection at another site Minimum of 2 blood culture samples taken from different sites at separate occasions showing same organism & same antibiotic susceptibility patterns. EXCLUSION CRITERIA: Patients not on any device. Pediatric patients. 7.2 METHODS OF COLLECTION OF DATA: Clinical specimens (endotracheal secretions, catheterized specimen urine and intravenous blood) will be collected, transported & processed in the diagnostic Microbiology laboratory according to standard procedures.[10] The organisms isolated will be identified by standard techniques [10] and their Antibiotic Sensitivity Test (AST) will be formed by Kirby-Bauer’s disc diffusion method using panel of antibiotics[11]. COMMON ANTIBIOTIC RESISTANCE MECHANISMS DEMONSTRATED BY FOLLOWING TESTS: Screening for Methicillin Resistance Staphylococcal aureus( MRSA), Inducible Clindamycin Resistance, Extended Spectrum β-Lactamase(ESBL), Inducible AmpC β-Lactamase, Plasmid- mediated AmpC production, and Metallo-βLactamase(MBL) will also be performed by Cefoxitin disc diffusion[12], D-test[13], Combined disc diffusion method[14], Disk antagonism[15], Amp C disk test[16] and Modified three-dimensional test[17], and EDTA disk synergy test & Modified Hodge Test[18] respectively.
STATISTICAL ANALYSIS: Simple statistics for detection of infection rate.
7.3 Does the study require any investigation or interventions to be conducted on patients or other humans or animals? If so, please describe briefly. Culture and sensitivity of various samples will be done. No special investigations or interventions to be conducted on patients or animal experiments required.
7.4 Has ethical clearance been obtained from your institution in case of 7.3?
References 1) Diekema DJ, Pealler MA. Infection control, epidemiology& Clinical Microbiology. In Manual of Clinical Microbiology. 9th ed. Washigton: ASMPress,Washington DC; 2007. p.118(volume 1).
2) Dogru A , Sargin F, Celik M, Sagiroglu AE, Goksel MM and Sayhan H. The rate of De- vice Associated Nosocomial Infections in a Medical-Surgical Intensive Care Unit of a training & research hospital in Turkey: One Year Outcomes. Jpn J Infect Dis [serial online]2010Jan19[cited2011Oct1];63:95-98. Available- from:http://www.nih.go.jp/JJID/63/95.pdf.
3) Vincent JL. Nosocomial infection in adult intensive care units. Lancet 2003;361:2068- 2077.
4) Fridkin SK, Welbel SF &Weinstein RA. Magnitude & prevention of nosocomial infections in the intensive care unit. Infect Dis Clin North Am 1997;11:479-496.
5) Lynch P, Rosenthal VD, Borg MA and Eremin SR. Infection Control A Global View. In Bennett & Brachman’s Hospital Infections. 5th ed. California: Lippincott Williams & Wilkins, a Wolter Kluwer business; 2007. p.255.
6) Wilcox MK and Spencer RC. Health Care Associated Infections. In Topley Wilson’s Mi- crobiology and Microbial Infections. 10th ed. GreatBritain: Hodder Arnold; 2005. p.371 and 388.(Bacteriology; Volume 1).
7) Garner JS, Jarvis WR, Emori TG, Horan TC , Hughes JM. CDC definition for Nosocomial infections. In: Olmsted RN, ed.: APIC Infection Control & Applied Epidemiology: Princi- ples and Practise. St Louis, Mosby; 1996:p A1-A20.
8) Dandagi GL. Nosocomial Pneumonia in critically ill patients. Lung India Journal[serial on- line]2010Aug10[cited2011Oct1]27(3):149-153. Available from: www.lungindia.com.
9) Chopdekar K, Chande C, Chavan S, Veer P, Wabale V, Vishwarama K, Joshi A. Central venous catheter-related blood stream infection rate in critical care units in a tertiary care teaching hospital in Mumbai. Indian J Med Microbiol 2011;29(2):169-171.
10) Koneman EW, Allen SD, Janda WM, Schreckenberger PC, Win WC. The Enterobacteri- aceae. In Color atlas and textbook of diagnostic microbiology. 5th ed. Philadelphia: JB Lip- pincott Co;2006. p.211-302.
11) Bauer AW, Kirby WN, Sherris JC, Truck H. Antibiotic suspectibilty testing by a standard- ized single disk method. Am J Clin Pathol 1966;45:493-496.
12) Shorman MA, Atoom AM, Abuharfeil NM, Al-Majali AM.Identification of Methicillin Resistant Staphylococcus aureus (MRSA) & Methicillin Resistant Coagulase Negative Staphylococcus (CONS) in clinical settings. Am J Infect Dis 2008;4(2):156-161.
13) Deotale V, Mendiratta DK , Raut U, Narang P. Inducible clindamycin resistance in Staphy- lococcus aureus isolated from clinical samples. Indian J Med Microbiol 2010;28(2):124- 126.
14) Agrawal P, Ghosh AN, Kumar S, Basu B, Kapila K. Prevalence of extended-spectrum β- lactamases among Escherichia coli & Klebsiella pneumonia isolates in a tertiary care hos- pital. Indian J Patho and Microbiol 2008;51(1):139-142.
15) Sanders CC, Sanders WE, Goering HV. In vitro antagonism of β-lactam antibiotics by ce- foxitin. J Antimicrob Chemother 1982;21:968-975.
16) Black JA, Moland ES, Thomson KS. Amp C Disk Test for detection of Plasmid-mediated Amp C β-lactamases. J Clin Microbiol 2005;43(7):3110-3113.
17) Manchanda V, Singh NP. Occurence and detection of AmpC β-lactamases among Gram negative clinical isolates using a modified three-dimensional test at Guru Tegh Bahadur Hospital,Delhi,India. J Antimicrob Chemother 2003;51:415-418.
18) Lee K, Chong Y,Shin HB, Kim YA, Yong D and Yum JH. Modified Hodge test & EDTA Disc Synergy tests to screen metallo-β-lactamase producing strains of Pseudomonas & Acinetobacter species. Eur Soc of Clinic Microbiol Infect Dis, CMI[serial online]2001 Dec20[cited 2011Oct3];7:88-91. Available from : online library.wiley.com. 1)SCREENING FOR MRSA: By CEFOXITIN DISC METHOD: Using 0.5 McFarland standard, a Mueller Hinton Agar (MHA)plate supplemented with NaCl will be inoculated with the strain to be screened & Cefoxitin 30 microgram disc on plain MHA plate will be kept in situ along with a control strain of MRSA. The plate will be incubated between 25-350C & observed after 18-24 hours .Depending on zone of inhibition, if the strains are resistant to cefoxitin ,then considered as MRSA as per CLSI guidelines.[12] 2)DETECTION OF INDUCIBLE CLINDAMYCIN RESISTANCE BY D-TEST: After inoculating the S.aureus strain on to MHA plate , an Erythromycin disc (15µg) will be placed 15mm apart from clindamycin disc(2µg).Inducible resistance to clindamycin is manifested by flattening of the clindamycin zone of inhibition adjacent to the erythromycin disc,giving a D-shape to zone of inhibited growth. Interpretation : MS Phenotype- Strains resistance to erythromycin & sensitive to clindamycin & giving circular zone of inhibition around clindamycin.
Inducible MLSB Phenotype-Strains resistance to erythromycin & sensitive to clindamycin & giving D shaped zone of inhibition around clindamycin.
Constitutive MLSB Phenotype-Strains resistance to both erythromycin & clindamycin with circular zone inhibition.[13] 3)DETECTION OF ESBL: By COMBINED DISC DIFFUSION METHOD: A disc of Ceftazidime alone & a disc of Ceftazidime +Clavulanic acid will be placed at distance of 25mm apart on a lawn culture of the test isolate on MHA plate and incubated overnight at 370C. Interpretation: When there is an increase of >5mm in inhibition zone diameter around combination disk of Ceftazidime+clavulanic acid versus ceftazidime disk alone.[14] 4)DETECTION OF INDUCIBLE AMP C BETALACTAMASE : By DISC ANTAGONISM TEST : A disc of Cefoxitin and other beta-lactam discs(cefotaxime, ceftriaxone or ceftriaxone) will be placed at distance of 25mm apart on a lawn culture of the test isolate on MHA plate and incubated overnight at 370C. If radius will be smaller by 4mm or more, then antagonism will be considered.[15]
5)DETECTION OF PLASMID-MEDIATED AMP C PRODUCTION: By AMP C DISK TEST: Briefly,0.5 McFarland suspension of ATCC E.coli will be inoculated on the surface of MHA plate.A 30µg cefoxitin disk & a sterile plain disk inoculated with several colonies of the test organism will be placed just beside the cefoxitin disk almost touching it,with inoculated disk face in contact with the agar surface.After overnight incubation at 370C, the plates will be examined for either an indentation or a flattening of the zone of inhibition,indicating enzymatic inactivation of cefoxitin(positive result), or absence of a distortion (negative result).[16] By MODIFIED THREE DIMENSIONAL TEST: Briefly, fresh overnight growth of test organism from Mueller Hinton Agar plate was taken in a micro centrifuge tube. Peptone water will be added & centrifuged at 3000rpm for 15 min. Crude enzyme extract will be prepared by repeated freeze thawing in -800C for seven times.A lawn culture of E.coli ATCC will be made on MHA plate & cefoxitin(30µg)disc will be placed on the plate.Linear slits will be cut using a sterile surgical blade 3mm away from the cefoxitin disc; 30 to 40 µl of the enzyme extract will be added to a well made at the outer edge of the slit, without overflowing. The plates will be kept upright for 5-10 min until liquid dried & will be incubated at 370C for overnight. Clear distortion of zone of inhibition of cefoxitin is taken as Amp C beta-lactamase producer.[17]
6)DETECTION OF METALLOBETALACTAMASE : i. By EDTA DISC SYNERGY TEST: Overnight culture of the test strain was suspended to the turbidity of a McFarland no 0.5 tube & used to swab inoculate a MHA plate. After drying, a 10µg Imipenem disk & a EDTA disk (1.5mg) placed at a distance of 10mm from it .After overnight incubation, the presence of an enlarged zone of inhibition will be interpreted as EDTA synergy test positive.[18] ii. MODIFIED HODGE TEST: The surface of a MHA plate was inoculated evenly using a cotton swab with an overnight culture suspension of E.coli, which will be adjusted to one-tenth turbidity of McFarland no 0.5 tube.After brief drying an imipenem disk will be placed at the center of plate,& imipenem resistant test strains from overnight cultured plates will be streaked heavily from the edge of the disk to the periphery of the plate.The presence of a distorted inhibition zone after overnight incubation will be interpreted as Modified Hodge Test.[18]
9. Signature of candidate
10. Remarks of the guide
11. Name and designation of (in block letters ) 11.1 Guide Dr.B.V.NAVANEETH PROFESSOR & HOD, DEPARTMENT OF MICROBIOLOGY
11.2 Signature
11.3 Co-guide Dr.CHANDRASHEKAR.E ICU INCHARGE, DEPARTMENT OF ANAESTHESIA. 11.4 Signature
11.5 Head of department Dr.B.V.NAVANEETH PROFESSOR & HOD, DEPARTMENT OF MICROBIOLOGY
11.6 Signature
12. 12.1 Remarks of the Chairman and Principal/Dean
12.2 Signature