PARTNERSHIP HEALTHPLAN OF CALIFORNIA POLICY/ PROCEDURE
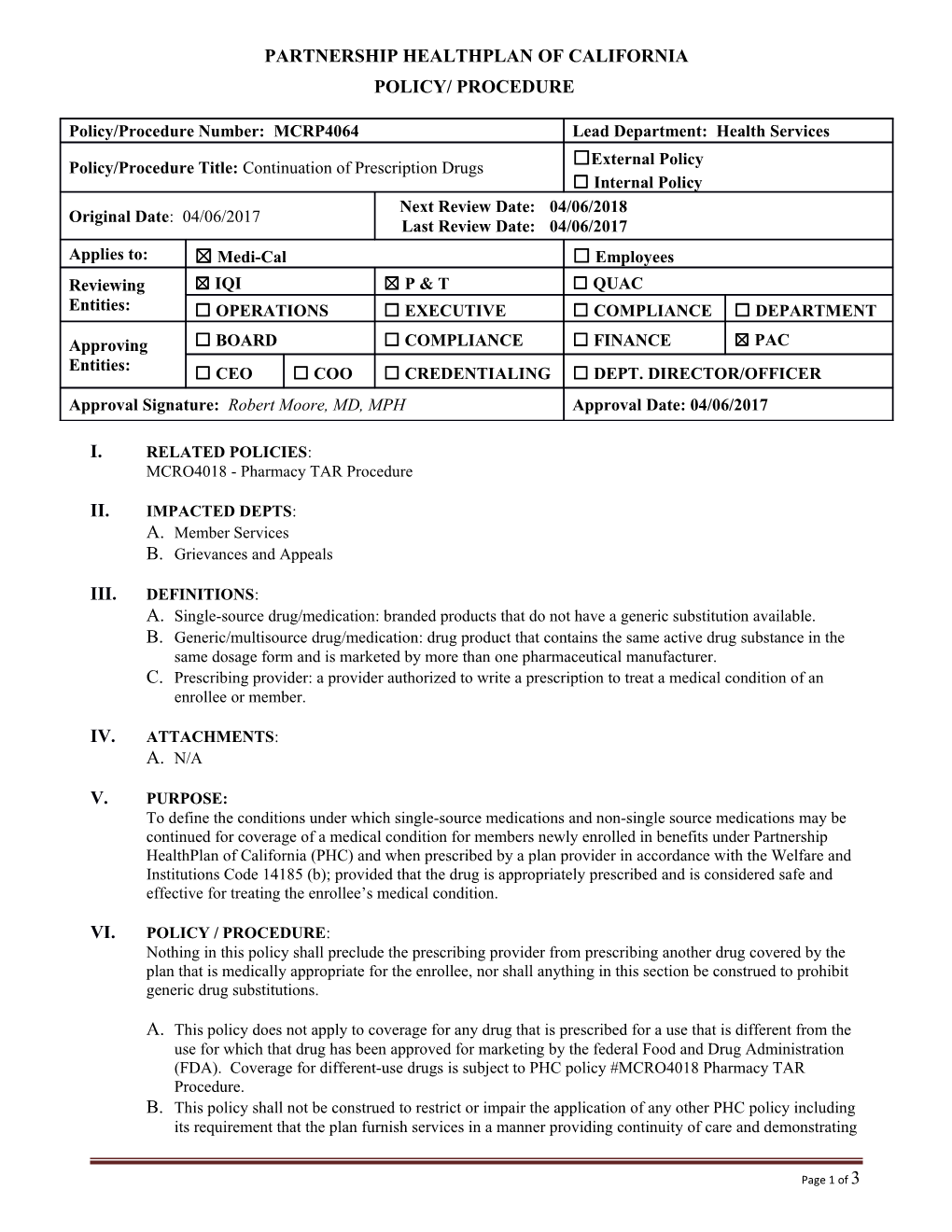
Policy/Procedure Number: MCRP4064 Lead Department: Health Services ☐External Policy Policy/Procedure Title: Continuation of Prescription Drugs ☐ Internal Policy Next Review Date: 04/06/2018 Original Date: 04/06/2017 Last Review Date: 04/06/2017 Applies to: ☒ Medi-Cal ☐ Employees Reviewing ☒ IQI ☒ P & T ☐ QUAC Entities: ☐ OPERATIONS ☐ EXECUTIVE ☐ COMPLIANCE ☐ DEPARTMENT
Approving ☐ BOARD ☐ COMPLIANCE ☐ FINANCE ☒ PAC Entities: ☐ CEO ☐ COO ☐ CREDENTIALING ☐ DEPT. DIRECTOR/OFFICER Approval Signature: Robert Moore, MD, MPH Approval Date: 04/06/2017
I. RELATED POLICIES: MCRO4018 - Pharmacy TAR Procedure
II. IMPACTED DEPTS: A. Member Services B. Grievances and Appeals
III. DEFINITIONS: A. Single-source drug/medication: branded products that do not have a generic substitution available. B. Generic/multisource drug/medication: drug product that contains the same active drug substance in the same dosage form and is marketed by more than one pharmaceutical manufacturer. C. Prescribing provider: a provider authorized to write a prescription to treat a medical condition of an enrollee or member.
IV. ATTACHMENTS: A. N/A
V. PURPOSE: To define the conditions under which single-source medications and non-single source medications may be continued for coverage of a medical condition for members newly enrolled in benefits under Partnership HealthPlan of California (PHC) and when prescribed by a plan provider in accordance with the Welfare and Institutions Code 14185 (b); provided that the drug is appropriately prescribed and is considered safe and effective for treating the enrollee’s medical condition.
VI. POLICY / PROCEDURE: Nothing in this policy shall preclude the prescribing provider from prescribing another drug covered by the plan that is medically appropriate for the enrollee, nor shall anything in this section be construed to prohibit generic drug substitutions.
A. This policy does not apply to coverage for any drug that is prescribed for a use that is different from the use for which that drug has been approved for marketing by the federal Food and Drug Administration (FDA). Coverage for different-use drugs is subject to PHC policy #MCRO4018 Pharmacy TAR Procedure. B. This policy shall not be construed to restrict or impair the application of any other PHC policy including its requirement that the plan furnish services in a manner providing continuity of care and demonstrating
Page 1 of 3 Policy/Procedure Number: MCRP4064 Lead Department: Health Services Policy/Procedure Title: Continuation of Prescription Drugs ☒ External Policy ☐ Internal Policy Original Date: 04/06/2017 Next Review Date: 04/06/2018 Last Review Date: 04/06/2017 Applies to: ☒ Medi-Cal ☐ Employees that medical decisions are rendered by qualified medical providers unhindered by fiscal and administrative management. C. New start designation in Treatment Authorization Request (TAR) Criteria: C.1. A new start is a PHC member who has not previously been on the drug in question. A member who has been previously on a medication but with a significant lapse in treatment may be interpreted as a new start when the duration without the medication indicates the enrollee has not been dependent upon it for treatment and the current request actually represents a restart of treatment rather than continuing treatment. C.2. A new enrollee may also be considered a new start, in the sense that PHC has not previously paid for the medication. Care must be exercised if the enrollee was previously on the drug through a state funded program (Medi-Cal FFS or another Managed Care Medi-Cal/COHS), as it may be prudent to continue a medication the enrollee previously had prior authorization for under a different state payer. If the medication is a single-source medication, PHC will permit the enrollee to continue use of the single-source drug which is part of a prescribed therapy in effect for the enrollee immediately prior to the date of enrollment, whether or not the drug is covered by the plan, until the prescribed therapy is no longer prescribed by the contracted physician. D. New start designation in Treatment Authorization Request (TAR) Criteria: D.1. A new start is a PHC member who has not previously been on the drug in question. A member who has been previously on a medication but with a significant lapse in treatment may be interpreted as a new start when the duration without the medication indicates the enrollee has not been dependent upon it for treatment and the current request actually represents a restart of treatment rather than continuing treatment. D.2. A new enrollee may also be considered a new start, in the sense that PHC has not previously paid for the medication. Care must be exercised if the enrollee was previously on the drug through a state funded program (Medi-Cal FFS or another Managed Care Medi-Cal/COHS), as it may be prudent to continue a medication the enrollee previously had prior authorization for under a different state payer. If the medication is a single-source medication, PHC will permit the enrollee to continue use of the single-source drug which is part of a prescribed therapy in effect for the enrollee immediately prior to the date of enrollment, whether or not the drug is covered by the plan, until the prescribed therapy is no longer prescribed by the contracted physician. E. Continuing care requests for existing PHC members with claim history and previously approved PHC TARs: E.1. Drugs with previous PHC criteria undergoing criteria revision: members with previously approved PHC TARs for ongoing use which have been filled routinely without significant stops/breaks in therapy will be allowed to continue ongoing treatment when indicated (i.e., will not have to meet revised criteria unless treatment is deemed a restart rather than continuation). This will also apply to non-formulary drugs with new TAR criteria, which have always been non-formulary (but without TAR criteria). E.2. Drugs which were previously on formulary and have been removed from formulary, with the addition of TAR criteria: electronic coding will be implemented when the plan and committees approves such for members to continue with the medication without significant stops/breaks in therapy. When electronic coding is not implemented, members receive notification of drugs removed from formulary. Any TARs received for continuing care, and claim of continuing care is supported by the member’s pharmacy claim history, will be considered on a case-by-case basis as to
Page 2 of 3 Policy/Procedure Number: MCRP4064 Lead Department: Health Services Policy/Procedure Title: Continuation of Prescription Drugs ☒ External Policy ☐ Internal Policy Original Date: 04/06/2017 Next Review Date: 04/06/2018 Last Review Date: 04/06/2017 Applies to: ☒ Medi-Cal ☐ Employees whether or not medical justification for continuation warrants such vs transition to formulary alternative (excludes single-source drugs). F. New enrollee without claim history and/or without PHC TAR: F.1. Single-source medication request for continuing care will be allowed; however the plan may suggest formulary alternatives for consideration by the prescriber, without withholding treatment approval. TAR must include documentation that treatment is indeed ongoing from previous state funded payer immediately prior to the date of enrollment (pharmacy dispensing record with last fill date suffices), until the prescribed therapy is no longer prescribed by the contracted physician. F.2. Generic/multisource medication requests for continuing care without a prior PHC approved TAR: continuing care will be considered for generic/multisource drugs based on the medical justification provided with the TAR on a case-by-case basis; however, transition to a formulary alternative may be required.
VII. REFERENCES: N/A
VIII. DISTRIBUTION: N/A
IX. POSITION RESPONSIBLE FOR IMPLEMENTING PROCEDURE: Associate Director, Pharmacy Operations
X. REVISION DATES:
PREVIOUSLY APPLIED TO: N/A
XI. POLICY DISCLAIMER: A. In accordance with the California Health and Safety Code, Section 1363.5, this policy was developed with involvement from actively practicing health care providers and meets these provisions: A.1. Consistent with sound clinical principles and processes; A.2. Evaluated and updated at least annually; A.3. If used as the basis of a decision to modify, delay or deny services in a specific case, the criteria will be disclosed to the provider and/or enrollee upon request. B. The materials provided are guidelines used by PHC to authorize, modify or deny services for persons with similar illnesses or conditions. Specific care and treatment may vary depending on individual need and the benefits covered under PHC.
Page 3 of 3