Bree Collaborative Meeting
March 27, 2013
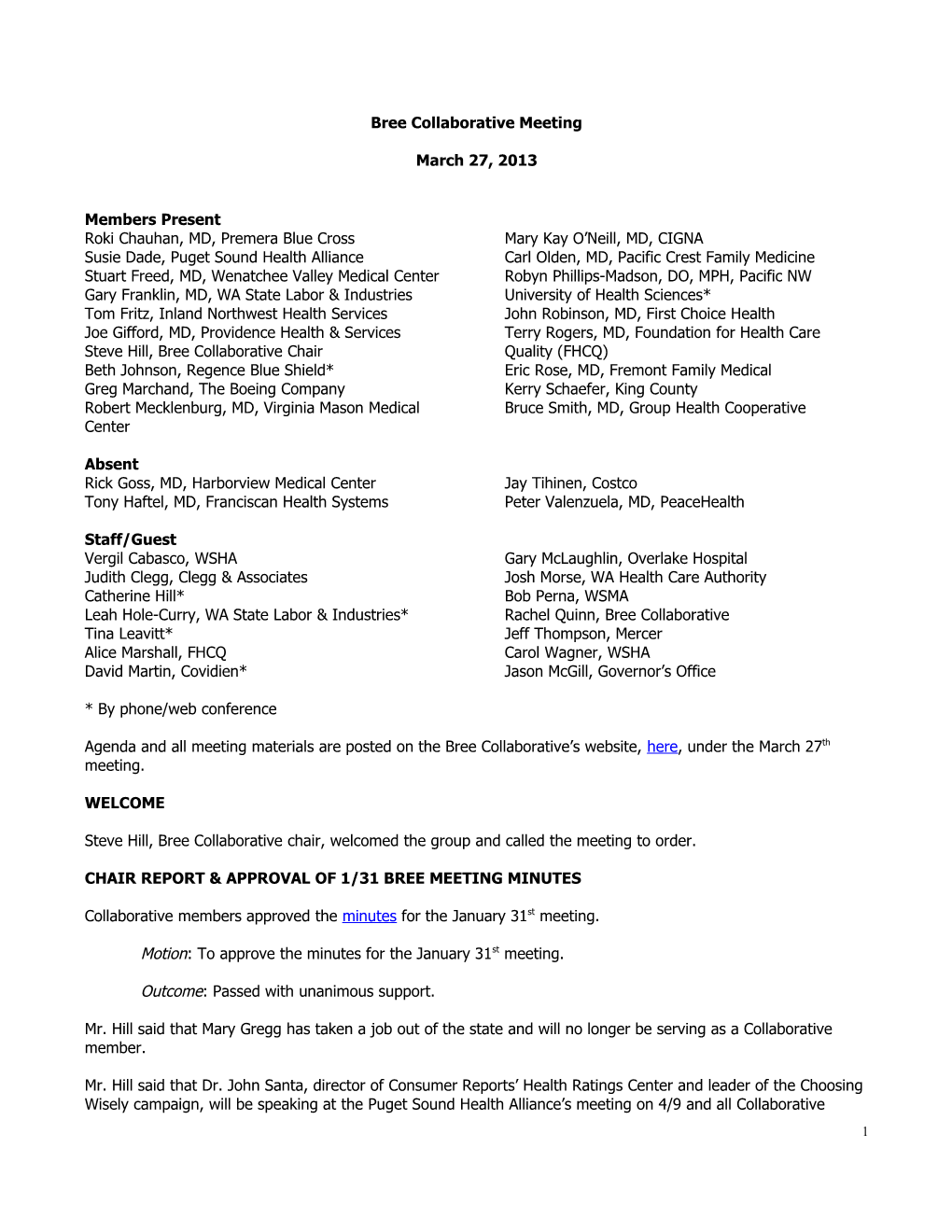
Members Present Roki Chauhan, MD, Premera Blue Cross Mary Kay O’Neill, MD, CIGNA Susie Dade, Puget Sound Health Alliance Carl Olden, MD, Pacific Crest Family Medicine Stuart Freed, MD, Wenatchee Valley Medical Center Robyn Phillips-Madson, DO, MPH, Pacific NW Gary Franklin, MD, WA State Labor & Industries University of Health Sciences* Tom Fritz, Inland Northwest Health Services John Robinson, MD, First Choice Health Joe Gifford, MD, Providence Health & Services Terry Rogers, MD, Foundation for Health Care Steve Hill, Bree Collaborative Chair Quality (FHCQ) Beth Johnson, Regence Blue Shield* Eric Rose, MD, Fremont Family Medical Greg Marchand, The Boeing Company Kerry Schaefer, King County Robert Mecklenburg, MD, Virginia Mason Medical Bruce Smith, MD, Group Health Cooperative Center
Absent Rick Goss, MD, Harborview Medical Center Jay Tihinen, Costco Tony Haftel, MD, Franciscan Health Systems Peter Valenzuela, MD, PeaceHealth
Staff/Guest Vergil Cabasco, WSHA Gary McLaughlin, Overlake Hospital Judith Clegg, Clegg & Associates Josh Morse, WA Health Care Authority Catherine Hill* Bob Perna, WSMA Leah Hole-Curry, WA State Labor & Industries* Rachel Quinn, Bree Collaborative Tina Leavitt* Jeff Thompson, Mercer Alice Marshall, FHCQ Carol Wagner, WSHA David Martin, Covidien* Jason McGill, Governor’s Office
* By phone/web conference
Agenda and all meeting materials are posted on the Bree Collaborative’s website, here, under the March 27th meeting.
WELCOME
Steve Hill, Bree Collaborative chair, welcomed the group and called the meeting to order.
CHAIR REPORT & APPROVAL OF 1/31 BREE MEETING MINUTES
Collaborative members approved the minutes for the January 31st meeting.
Motion: To approve the minutes for the January 31st meeting.
Outcome: Passed with unanimous support.
Mr. Hill said that Mary Gregg has taken a job out of the state and will no longer be serving as a Collaborative member.
Mr. Hill said that Dr. John Santa, director of Consumer Reports’ Health Ratings Center and leader of the Choosing Wisely campaign, will be speaking at the Puget Sound Health Alliance’s meeting on 4/9 and all Collaborative 1 members are welcome to attend. Susie Dade, Collaborative member, said that the Alliance and WSMA both received grants to promote the Choosing Wisely guidelines in the community and will coordinate their efforts.
A member said that there was an interesting article in Health Affairs about the difficulty of administering shared decisionmaking aids. Action item: Rachel Quinn, project manager for the Collaborative, will distribute the article to the group.
AVOIDABLE READMISSIONS WORKGROUP UPDATE
Ms. Quinn provided an update on the Potentially Avoidable Readmissions (PAR) workgroup.
Request to WSHA and Qualis to Publish 30-Day, All-Cause Readmissions Data
Ms. Quinn discussed the status of the Collaborative’s request to WSHA and Qualis to publish 30-day, all-cause readmissions data. Ms. Dade clarified that the Puget Sound Health Alliance has not decided how it will share results with Alliance members and/or the general public once its new measure is developed.
Carol Wagner, WSHA, explained the rationale for WSHA’s decision not to make its 30-day, all-cause readmissions data publicly available. Ms. Wagner said that different patient populations have different readmission rates, which makes it hard to compare rates that aren’t risk-adjusted across hospitals; currently, this data is being used to help individual hospitals track their own changes over time and do “drilldowns” to support improvement efforts (e.g. stratify by time period to figure out when follow-up calls should be made). CMS is going to come out with two new risk-adjusted measures in July and there are three existing measures that can guide payment decisions.
Members had the following comments and questions: Is there good data about how much of a difference risk adjustment makes in the results? Do we know that risk-adjusted measures are more valid? If so, how much more? (Ms. Wagner said that she can ask people at CMS about these questions.) We don’t want to wait for perfect data, but real harm can be done by throwing around garbage data. We need to know what the reality is today. If the numbers are bad, then we can talk about the reasons. The Collaborative needs to plow ahead with transparency. The data may not need to be on a public website, but it should be shared with the buyers and sellers of health care to allow for informed dialogue. Access to this information should not be restricted to WSHA’s members. This data could allow us to look at outliers, give accolades, and identify opportunities for improvement. I agree that risk-stratification is too complicated, but am still interested in the percentage of government payers since that is pretty solid information and could help set benchmarks.
Ms. Wagner said that WSHA is willing to share this data with members of the Collaborative and Alliance in efforts to improve quality but is not sure how much WSHA is able to move forward with making data publicly available before July. Ms. Wagner agreed to present WSHA’s current, unblinded data at the next Collaborative meeting (end of May) for further discussion. Mr. Hill asked that WSHA also present the data at the next PAR workgroup meeting in April.
The group briefly discussed getting data from health plans. A member said that would only be helpful if all of the plans used the same measure, and another said that all of the plans measure readmissions slightly differently.
Endorsement of the WSHA Tool Kit
Ms. Quinn summarized efforts by staff to promote the Collaborative’s endorsement of the concept of the tool kit.
2 Summary of Stakeholder Interviews and Discussion of Bree’s Future Role
Ms. Quinn presented key findings from interviews that she conducted with workgroup members and community stakeholders. The group discussed areas where the Collaborative could add value to existing readmission efforts. Comments included: Several initiatives have good evidence of effectiveness. Why can’t the Collaborative make one of those a community standard? Why aren’t we looking at how we can rapidly mobilize this work in communities? Successful strategies are included in the tool kit, which is currently being pilot tested in two communities. The point of the pilot is to figure out how to operationalize these strategies in communities that are completely fragmented. After the tool kit is finished, the next step is motivating its dissemination and implementation. A literature review would be helpful to identify low hanging fruit and refine our focus. WSHA and Qualis have already done literature reviews, and the tool kit is being built based on those reviews. The question is not what we should do, it’s how do we get people to do it. A recent article said that its is problematic to focus only on readmissions because they are all related to larger problems – is the Collaborative looking at this too narrowly? Improving end of life care could be a good area of focus because it cuts across many diagnoses and could avoid a lot of unnecessary care. It would be great to see data about how often PCPs are able to engage in the activities that are essential to reducing readmissions. The Hospital Assessment is moving ahead in legislature, and the group could consider talking to Representative Cody about creating incentives for hospitals to meet goals, as was done in the past. We’ve identified some root causes and issues, like not being able to pay for a visit within 24 hours or providing with a week’s worth of meds. There’s a lot we could do as a group to push these things out. The tendency is for each place to want to do things their own way, but the only way the tool kit will make a difference if it is spread in a fairly uniform way across the state because people are mobile. I foresee a future role for this group (when the tool kit is done) to go out with the hardline message across the state and create accountability for engaging communities and implementing the tool kit in a standardized way. Reducing variability should be the first goal, and that would be consistent with what we did for OB.
Consensus: The PAR workgroup should pursue two tracks. The first track is to wait for the tool kit to be finalized, and then work on operationalizing it and developing incentives to encourage standardized implementation of it across the state. The second track is payment reform, which will continue to be carried out by the APM subgroup. No members opposed this plan.
ACCOUNTABLE PAYMENT MODEL SUBGROUP UPDATE
Dr. Bob Mecklenburg, Collaborative member and chair of the Accountable Payment Model (APM) subgroup, presented an update on the subgroup’s work. The subgroup has completed a draft warranty for total knee and hip replacements and is seeking clinical input. Dr. Mecklenburg reviewed the warranty components and discussed some of the references that the group relied upon for its development.
Mr. Hill reminded the group that the Collaborative will not be setting any prices. A member suggested that providers for patients who go through the initial screening stages and then decide that they don’t need the surgery may deserve compensation for more than just a regular office visit due to the complexity involved.
Dr. Mecklenburg said that the marketplace will decide whether any patients will have TKR/THR surgery outside of the bundle, but the bundle will serve as a vehicle for reducing variation in care.
3 SPINE/LOW BACK PAIN TOPIC UPDATE
Spine SCOAP Recommendation
Ms. Quinn presented an update on the Spine SCOAP recommendation that was sent to the Health Care Authority (HCA) in January. Josh Morse from the HCA explained the rationale behind HCA’s response to the recommendation, which is that the HCA supports the recommendation but is concerned about the phrase “community standard”; reviewers concluded that establishing a community standard exceeds the authority of the Collaborative and creates possible legal and regulatory issues.
A member remarked that WA State Labor and Industries (L&I) has concerns about the process of establishing participation in Spine SCOAP as a requirement. It still supports the Spine SCOAP recommendation, but believes that is separate from the question of whether a public agency would make hospitals do this.
Members had the following comments: The Collaborative does not have any regulatory authority, so it is essentially a bully pulpit. If saying that participation in a registry should be a community standard isn’t within our purview, then I don’t know what is. The HCA could use its bully pulpit to support the recommendation, even if it can’t build it into any contracts. “Community standard” may not be a problem if the language is that the Collaborative strongly recommends participation. This would maintain the strength of the message without going beyond our purview. Anything other than “community standard” really waters down the recommendation. The Collaborative could move beyond the bully pulpit by educating the public about best practices and identifying which hospitals are participating in registries that strive for the highest quality of care. It is premature to comment on Spine SCOAP’s outcomes data because there is an intense effort underway to expand data collection. The composition of the Collaborative makes it the ideal body to determine community standards. “Community standard” means different things to different people.
Mr. Hill emphasized that it was not the intent of the Collaborative to have the HCA mandate participation in Spine SCOAP. Mr. Hill asked that representatives from state agencies come back to the Collaborative with ideas about possible strategies for increasing participation in Spine SCOAP (short of changing contracts). Mr. Hill said that the Collaborative will resubmit the request with the following language: “To approve…that the Collaborative strongly recommend participation in Spine SCOAP as a community standard”. The HCA will review this new language.
Spine/Low Back Pain Workgroup Update
Dr. Mary Kay O’Neill, Collaborative member and chair of the Spine/Low Back Pain workgroup, and Ms. Quinn summarized the workgroup’s progress. The workgroup has adopted criteria and reviewed guidelines, over-used modalities, and best practices. The workgroup plans to present an outline or draft report at the next Collaborative meeting. Dr. O’Neill said that the workgroup is trying to work through the flow of patient care so that tools are in place to make the right decision at all of the steps along the care pathway, and the workgroup plans to consult primary care providers to focus on operationalizing best practices.
Members had the following comments: L&I is heavily invested in a Functional Recovery Questionnaire. The screening recommendation should allow for the use of tools that are equivalent to the STarT Back tool. The group should consider adding modality-based physical therapy to the list of over-used modalities. The report should not say that screening should be conducted at the very first visit. 4 For doctors who do not see a lot of back pain patients, it may make sense for screening to be administered in a centralized manner. The group should consider options for different types of practices.
OTHER TOPIC UPDATES
Cardiology/PCI
Ms. Quinn presented an update on the cardiology report adopted at the January Collaborative meeting. No response has been received from the HCA yet on the cardiology report. The target dates for public reporting of appropriateness of PCI have been pushed back. COAP will send hospitals an updated appropriate use insufficient information report (based on 4th Quarter 2012 data only) for their hospital to review by May 15, 2013 (original target date was April 15th), and data will be publically available June 1st (original target date was May 1st). A member asked about moving beyond appropriateness, and Dr. Terry Rogers said that COAP will explore options at the national level.
OB Implementation
Ms. Quinn summarized efforts to spread the word about the OB report and work with HCA to implement the HCA Administrator’s decision to adopt the recommendations. The group discussed potential roles for other purchasers and payers in the implementation of the recommendations.
RETREAT PLANNING DISCUSSION
Ms. Quinn presented initial planning efforts for a Bree Collaborative retreat. She introduced Judy Clegg, who will be helping with planning and serving as the facilitator at the retreat. Members had the following comments: The agenda should include a discussion about how the Collaborative can: 1) link quality improvement efforts to all three of the stakeholder groups rather than focusing on providers, and 2) translate evidence into actionable work processes. Other recommended topics: succession planning, sustaining membership, managing tension (not avoiding tension). Recommend that people attend the retreat in person, if possible. This sounds more like a strategic planning meeting, which is different from a retreat focused on “getting away” and social networking; it would be good to include some time for socializing. The retreat should be held at a different location so it doesn’t just feel like another meeting. There was a lot more divisiveness and a sense that we are not aligned in this meeting, which we haven’t had at past meetings. We really need to think about why we are here – to serve patients in this state. Having tension at meetings is appropriate and sometimes necessary because we are dealing with hard issues; it’s important to be careful about letting conflicts become personal rather than about the issues. Members should be invited to submit anonymous feedback before the retreat for members who are not comfortable expressing provocative thoughts at meetings.
PUBLIC COMMENT/NEXT STEPS
Mr. Hill thanked everyone for attending the meeting.
5