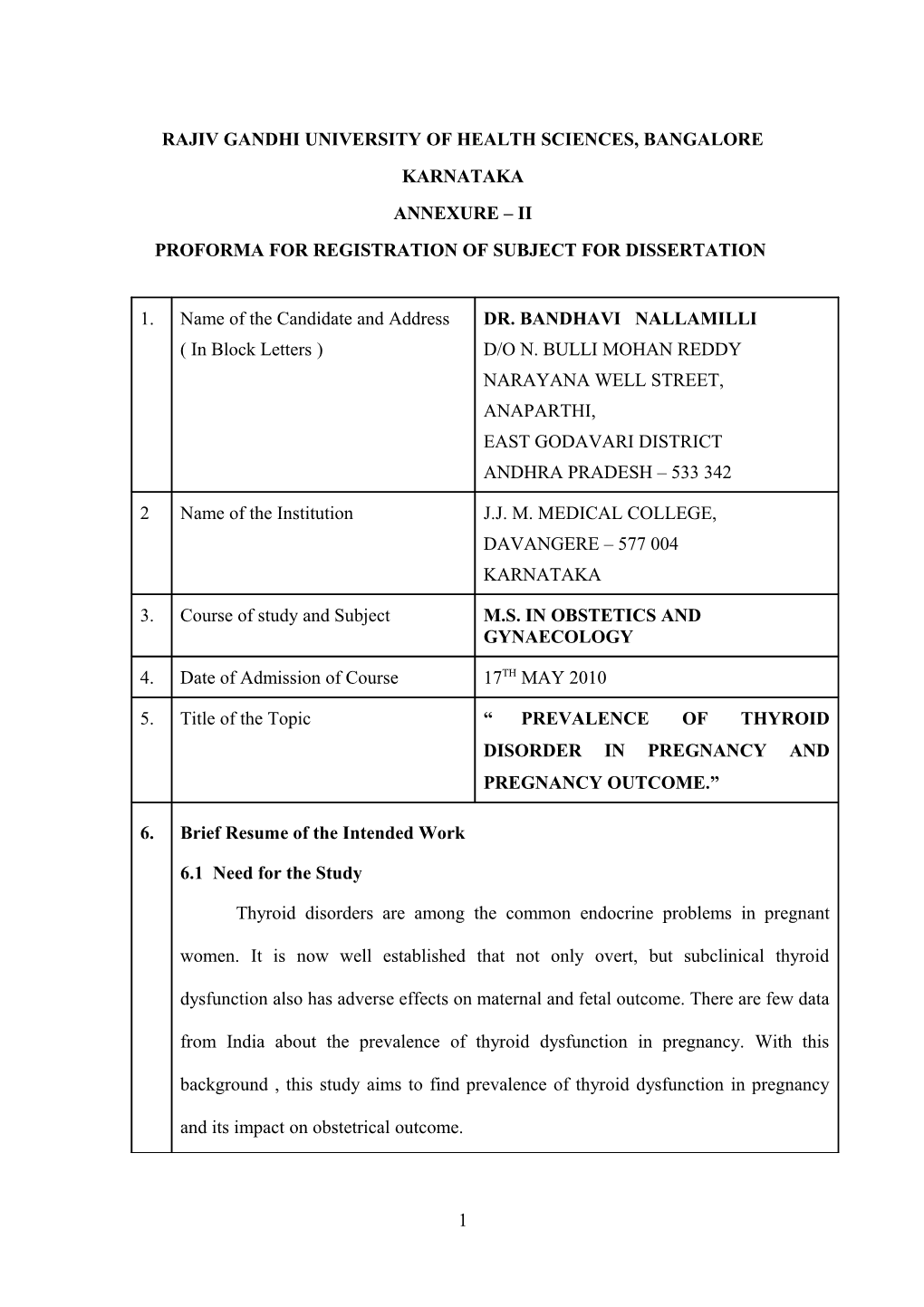
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, BANGALORE KARNATAKA ANNEXURE – II PROFORMA FOR REGISTRATION OF SUBJECT FOR DISSERTATION
1. Name of the Candidate and Address DR. BANDHAVI NALLAMILLI ( In Block Letters ) D/O N. BULLI MOHAN REDDY NARAYANA WELL STREET, ANAPARTHI, EAST GODAVARI DISTRICT ANDHRA PRADESH – 533 342
2 Name of the Institution J.J. M. MEDICAL COLLEGE, DAVANGERE – 577 004 KARNATAKA
3. Course of study and Subject M.S. IN OBSTETICS AND GYNAECOLOGY
4. Date of Admission of Course 17TH MAY 2010
5. Title of the Topic “ PREVALENCE OF THYROID DISORDER IN PREGNANCY AND PREGNANCY OUTCOME.”
6. Brief Resume of the Intended Work
6.1 Need for the Study
Thyroid disorders are among the common endocrine problems in pregnant
women. It is now well established that not only overt, but subclinical thyroid
dysfunction also has adverse effects on maternal and fetal outcome. There are few data
from India about the prevalence of thyroid dysfunction in pregnancy. With this
background , this study aims to find prevalence of thyroid dysfunction in pregnancy
and its impact on obstetrical outcome.
1 6.2 Review of Literature
In 2010 Sahu, Meenakshi Titoria et al, screened 633 pregnant women in second trimester. TSH level estimated . If TSH level was deranged, then free T4 and
Thyroperoxidase antibody level were done. Patients were managed accordingly and followed till delivery. Their obstetrical and perinatal outcomes were noted. Their results showed that prevalence of thyroid dysfunction was high in this study, with subclinical hypothyroidism in 6.47% and overt hypothyroidism in 4.58% women.
Overt hypothyroids were prone to have pregnancy induced hypertension (P =
0.04) . Intrauterine growth restriction (P = 0.01) and intra uterine demise (P = 0.0004) as compared to control. CS rate for fetal distress was significantly higher among pregnant subclinical hypothyroid women. (P = 0.04). Neonatal complications and gestational diabetes were significantly more in overt hyperthyroidism group (P=0.03 and P = 0.04) respectively. They concluded that prevalence of thyroid disorders, especially overt and subclinical hypothyroidism (6.47% ) was high. Significant adverse effect on maternal and fetal outcome were seen emphasizing the importance of routine antenatal thyroid screening.
In 2005, casey BM et al parkland hospital USA, Screened a total of 25,756 women for thyroid who delivered Singelton infants. There were 17298 (67%) women enrolled for prenatal care at 20 weeks gestation or less, and 404 (23%) of these were considered to have subclinical hypothyroidism. Pregnancies in women with subclinical hypothyroidism were 3 times more likely to be complicated by placental abruption
(RR-3.0, 95% confidence interval 1.1 – 8.2). Preterm birth, defined as a delivery at or before 34 weeks of gestation was almost 2- fold higher, in women with subclinical hypothyroidsm (RR 1.8, 95% confidence interval 1.1 – 2.9)
2 In 1998, A study was done by Leung AS et al losangeles. A cohort of 68 hypothyroid patients with no other medical illness were divided in to two groups according to thyroid function tests. The first one had 23 women with overt hypothyroidism and the second 45 women with subclinical hypothyroidism. They sought to identify the pregnancy outcomes. Gestational hypertension – namely eclampsia, preedampsia and pregnancy induced hypertension was significantly more in overt and subclinical hypothyroidism patients in the general population with rates of
22.15 and 7.6% respectively. In addition 36% of the overt, and 25% of the subclinical hypothyroid subjects, who remained hypothyroid at delivery developed gestational hypertension, Except for one still birth and one case of club feet. Hypothyroidism was not associated with adverse fetal and neonatal outcome.
In the year 2006, Bijay Vaidya, Exeter hospital, UK, prospectively analyzed
TSH, FT4 , FT3 in 1560 consecutive pregnant women during their 1st antenatal visit
(Median gestation 9 weeks). They tested thyroperoxidase antibodies in 1327. (85%)
They classified 413 women (26.5%) who had personal h/o thyroid or other autoimmune disorder or a family h/o thyroid disorder as a high risk group. They examined whether testing only such high risk group would pick up most pregnant women with thyroid dysfunction .
The results were forty women (2.6%) had raised TSH (>4.2 IU / ml). The prevalence of raised TSH was higher in the high risk group (6.8 V/s 1% low risk group, PR 65, 95% confidence, interval (CI) 3.3 – 12.6 P < 0.0001) presence of personal h/o thyroid disease (RR 12.2, 95% CI 6.8 – 2.2) P < 0.0001) or other autoimmune disorder (RR 4.8 , 95% CI 1.3 – 18.2, P = 0.0016) . Thyroid peroxidose antibodies (RR 8.4, 95% CI 4.6 – 15.3 P < 0.0001) and family h/o thyroid disorder
3 (RR 3.4, 95% , CI 1.8 – 6.2, P < 0.0001) increased risk of raised TSH. However 12 of
40 women with raised TSH (30%) were in the low risk group.
It concluded that targeted thyroid function testing of only high risk group would
minimum about 1/3rd of pregnant women with overt / subclinical hypothyroidism.
6.3 Objectives of the study
To Know the prevalence of thyroid disorders in Indian Population
To know the obstetric outcomes of the pregnant women suffering from thyroid
disorders.
7 Materials and Methods
7.1 Source of Data
The main source of data for the study are patients from the teaching hospitals
attached to J.J. M. Medical college, Namely
Bapuji Hospital, Davangere
Women and children hospital, Davangere
Chigateri general hospital, Davangere
7.2 Method of Collection of Data (Including Sampling Procedures if any)
Pregnant women coming for routine antenatal checkups.
Inclusion Criteria < 13 Weeks Gestation
4 Singelton Pregnancy
Primigravida / Multigravida
Exclusion Criteria Multifetal gestation
Known chronic disorders Diabetes and HTN
Had previous bad obstetric history with known cause
Who planned to deliver in other hospital.
Procedure : Minimum case to be studies – 1000
All the patients coming to OPD in 1st trimester for regular antenatal visits.
After obtaining the gestational age and informed consent of 1000 patients in 1st trimester were randomly selected from the study. These patients fulfilled all the inclusion criteria.
1) A detailed history was taken regarding the symptoms, and signs of thyroid
disorders. Menstrual history, obstetric history, past history medical history,
family history, personal history
2) A thorough general physical examination with reference to pulse , BP,
Temperature, respiratory rate were noted followed by CVS, CNS , RS, Local
thyroid examination .
3) Per abdomen examination and PV examination done and pregnancy confirmed
4) Patients are sent for TSH testing
5) If TSH comes deranged then FT3 and FT4 levels are checked.
6) If TSH increased and FT4 decreased then it is subclinical / overt
hypothyroidism, Thyroxine 1.6 µg / kg / day is given
5 7) If TSH Decreased and FT4 increased then it is hyperthyroidism, methimazole
is given.
8) Every 8 weeks TSH level will be estimated and the dose of the drug adjusted
9) At the end, the obstetric outcome and perinatal outcome of the pregnancy
noted. 7.3. Does the study require any investigation, or intervention to be conducted
on patients or other humans or animals? If so describe briefly.
No
7.4. Has ethical clearance been obtained from your institution in case of
7.3?
Yes
8 List of References
1. Menakshi Titoria Sahu et al. Overt and subclinical thyroid dysfunction among
Indian pregnant women and its effect on maternal and fetal outcome. Archives
of gynecology and obstetrics. 2010;281(2):215-220.
2. .Casey BM, Dashe JS, Well CE et al. Subclinical hypothyroidism and
pregnancy outcomes. Obstet . Gynecol 2005; 10-5:239-245.
3. Leung AS, Millar L.K, Kooning PP, Montorom, Mestman J. Perinatal
outcomes in hypothyroid pregnancies Obstet Gynecol 1993;81(3):349-353.
4. Vaidya B, Antony S. Bilousm et al. Detection of Thyroid dysfunction in early
pregnancy. Universal screening or high risk targeted case finding ? J Clin
Endocronol. Metab 2007; 92(1): 203-207.
5. Poppex , Glionereg D. Thyroid autoimmunity and hypothyroidism before and
6 during pregnancy . Hum Resport Update 2003;9 (2) : 149-161.
6. Metstman JH. Hyperthyroidism In Pregnancy endocrinol Metal clin North
Am. 1998;27(1): 127-149.
7. Abalovich M, Amino N, Barbons LA, Cobin RH, Degroot LJ, Glinoes D,
Mandel SJ, Stamaro Green A. Management of thyroid dysfunction during
pregnancy and postpartum : an endocrine society. Clinical practice guideline.
Jelin Endocronol. Metab 2007;92.13(5): 547.
7 9 Signature of Candidate
10. Remarks of Guide This study is being done to know the prevalence in our population and its effect on mother and foetus.
11. Name and Designation (In block letters)
11.1. Guide Dr. SHUKLA SHETTY . M.D., , Professor Department of Obstetrics and Gynaecology J.J. M.Medical College, Davangere
11.2 Signature
11.3 Co-Guide (If any) Dr. ANURADHA Reader Department of Obstetrics and Gynaecology JJMMC, Davangere – 577 004
11.4 Signature
11.5 Head of Department Dr. B.R. DAKSHAYINI M.D. Professor and H.O.D. Department of Obstetrics and Gynaecology J.J. M.Medical College, Davangere
11.6 Signature
12. Remarks of the 12.1 Chairman and Principal 12.2 Signature
8