Audit Algorithm
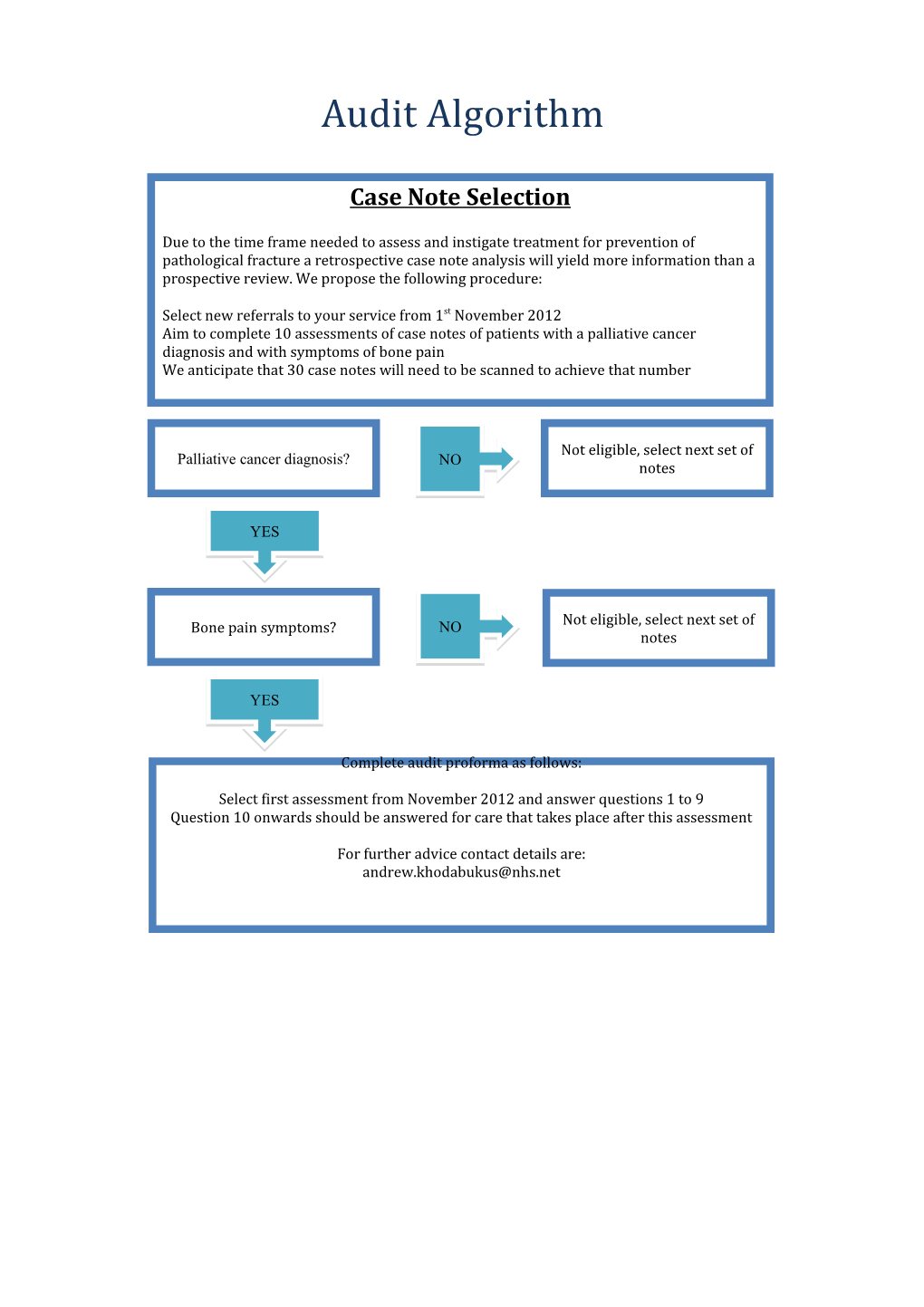
Case Note Selection
Due to the time frame needed to assess and instigate treatment for prevention of pathological fracture a retrospective case note analysis will yield more information than a prospective review. We propose the following procedure:
Select new referrals to your service from 1st November 2012 Aim to complete 10 assessments of case notes of patients with a palliative cancer diagnosis and with symptoms of bone pain We anticipate that 30 case notes will need to be scanned to achieve that number
Not eligible, select next set of Palliative cancer diagnosis? NO NO notes
YES
Not eligible, select next set of Bone pain symptoms? NO notes
YES
Complete audit proforma as follows:
Select first assessment from November 2012 and answer questions 1 to 9 Question 10 onwards should be answered for care that takes place after this assessment
For further advice contact details are: [email protected] Merseyside and Cheshire
Palliative Care Network Audit Group
Prevp Prevention of Pathological Fractures in Palliative Care
Retrospective Case Note Audit
ICN: ( Aintree ( Western Cheshire ( Warrington ( Isle of Man ( Liverpool ( Halton ( St Helens and Knowsley ( West Lancs., Southport & Formby ( Wirral
SETTING: Hospice ( Hospital ( Community (
PROFESSION: Doctor (If so, grade...... Clinical Nurse Specialist ( Other (please specify) ( ……………………………………
The first set of questions relate to the first assessment of a patient with cancer who has bone pain. Please enter the date of this assessment. 1 …………………………………………………………………………………………………… ……………………………………………………………………………… Age 2 (18-20 ( 21-30 ( 31-40 ( 41-50 ( 51-60 ( 61-70 ( 71-80 ( 81-90 ( 91-100( 101+ What is the patient’s primary cancer diagnosis?
( Bladder ( Bowel ( Breast ( Kidney ( Lung ( Melanoma 3 ( Mesothelioma ( Myeloma ( Prostate ( Metastatic cancer of unknown primary ( Other, please specify …………………………………………………………………………………………………… ……………………………………………………………… Is the patient known to have bone metastases? [Please select all that apply]
( No known bone metastases ( Upper arm (humerus) ( Lower arm (ulnar, radius, hand) ( Pelvis and hip (pelvic bones NOT femur) ( Upper leg (femur) ( Lower leg (tibia, fibula, foot) 4 ( Anterior chest wall (ribs, sternum) ( Cervical spine ( Thoracic spine ( Lumbar spine ( Skull ( Other, please specify or add notes …………………………………………………………………………………………………… …………………………………………………………………………………………………… …………………………………………………………………………… 5 Where is the patient experiencing bone pain? Please rank in order of severity (1= most severe), if there is one site you only need to select on answer and so on.
Upper arm including ...... shoulder ...... Lower arm ...... Pelvis and hip ...... Upper leg ...... Lower leg ...... Anterior chest wall ...... Cervical spine ...... Thoracic spine ...... Lumbar spine ...... Skull ...... Other ...
6 What investigations has the patient had up to this point? (Please tick all that apply)
X-ray image Specify anatomical site imaged & date if known or unknown: Please specify …………………………………………………. …………………………………………………………………………………………………… …………………………………
CT scan Specify anatomical site imaged & date if known or unknown: Please specify …………………………………………………. …………………………………………………………………………………………………… …………………………………
MRI scan Specify anatomical site imaged & date if known or unknown: Please specify …………………………………………………. …………………………………………………………………………………………………… …………………………………
Isotope bone scan: Specify anatomical site imaged & date if known or unknown: Please specify …………………………………………………. …………………………………………………………………………………………………… …………………………………
Serum calcium/bone profile: Results: Ca 2+ corrected...... Alkaline Phopshatase ......
Other Please specify …………………………………………………. …………………………………………………………………………………………………… …………………………………
What new investigations were organised/advised at this assessment? [tick all that apply]
X-ray image Specify anatomical site imaged & date if known or unknown: Please specify …………………………………………………. …………………………………………………………………………………………………… ………………………………… CT scan Specify anatomical site imaged & date if known or unknown: Please specify …………………………………………………. …………………………………………………………………………………………………… ………………………………… MRI scan Specify anatomical site imaged & date if known or unknown: Please specify …………………………………………………. …………………………………………………………………………………………………… ………………………………… Isotope bone scan: Specify anatomical site imaged & date if known or unknown: 7 Please specify …………………………………………………. …………………………………………………………………………………………………… ………………………………… Serum calcium/bone profile: Results: Ca 2+ corrected...... Alkaline Phopshatase ...... Other Please specify …………………………………………………. …………………………………………………………………………………………………… …………………………………
No new investigations ordered/advised after assessment because patient too unwell No new investigations ordered/advised after assessment because appropriate tests already ordered prior to palliative care involvement No new investigations - low severity/risk No new investigations - reason unclear What prompted these investigations to be ordered or advised? (Please tick all that apply based on your assessment or other team’s assessment during that episode of care)
Not applicable – none ordered 8 Increased pain Pain on weight-bearing Pain at night Results of other investigations Please specify…………………………………… Other symptoms Please specify …………………………………
Was the risk of new metastatic bone disease assessed? 9 Yes - risk assessed as probable metastatic disease but not graded as one of the options below Yes - risk assessed according to British Association of Surgical Oncology [BASO] Guidelines as "minimal" Yes - risk assessed according to British Association of Surgical Oncology [BASO] Guidelines as "low" Yes - risk assessed according to British Association of Surgical Oncology [BASO] Guidelines as "moderate" Yes - risk assessed according to British Association of Surgical Oncology [BASO] Guidelines as "high"
No/not documented Not applicable - already known to have metastatic disease in that area
The following questions should be answered with information gathered after the initial assessment and investigations.
Please state last date of entry in the notes or computer system/results...... Has new or existing metastatic disease been identified on imaging? 1 Yes 0 No end of survey Was the risk of pathological fracture assessed? Yes - Mirels' score Yes - Harrington's classification Yes - clinical judgement 1 Yes - other system [please add comment below] 1 No or not documented Comments ……………………………. ……………………………………………………………..
Following most recent investigations was the patient discussed with or referred to: Orthopaedic surgeon Please give details & date Oncologist Please give details & date …………………………... 1 ……………………………………………………………. 2 None ……………………………..….……………………………………………………………. Other Please specify & date ……………………………..…. ……………………………………………………… What treatment(s) were considered by the relevant healthcare professionals in view of 1 the results of the above assessment & investigations? Please include any treatments 3 offered to but declined by the patient. If treatments were considered inappropriate please answer accordingly
Radiotherapy Not considered Not appropriate as previously treated: Not appropriate due to poor performance status: Appropriate but declined by patient: Appropriate and planned or administered: Please give details ……………………….………………………………………………
Chemotherapy Not considered Not appropriate clinically: Not appropriate due to poor performance status: Appropriate but declined by patient: Appropriate and planned or administered: Please give details ………………………….……………………………………………
Orthopaedic surgery Not considered Not appropriate technically: Not appropriate due to poor performance status: Appropriate but declined by patient: Appropriate and planned or administered:
Please give details………………………………………………………………………
No change in treatment
Change or increase in analgesia Please give details ……………………………………………………………………
Change in other medication Please specify …………………………….…………………………………………
Other Please give details………………………………………………………………………
Was there a plan for further treatment or other referrals? (e.g interventional pain assessment) 1 4 Yes No N/A Please specify ………………………………………………………………………… ………………………………………………………………………………………….
Please send completed responses to:
Dr Andrew Khodabukus Academic Clinical Fellow & Specialty Registrar in Palliative Medicine Specialist Palliative Care, Linda McCartney Centre, Royal Liverpool University Hospital, Prescot Street, Liverpool, L7 8XP. Tel: 0151 706 2274 Fax: 0151 706 5688 Email: [email protected]
Alternatively, this survey can be completed online at: http://tolu.na/VSrRTG