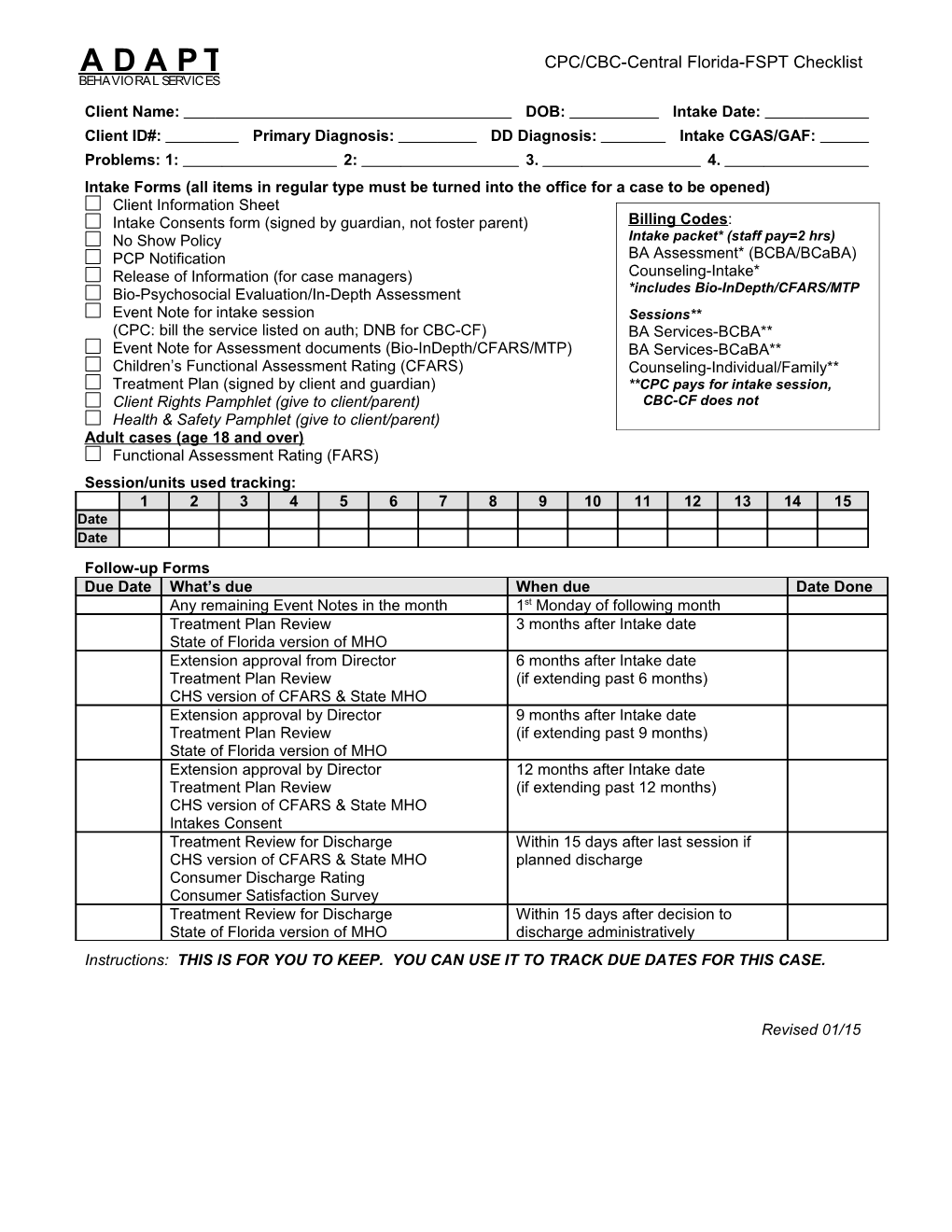
A D A P T CPC/CBC-Central Florida-FSPT Checklist BEHAVIORAL SERVICES
Client Name: DOB: Intake Date: Client ID#: Primary Diagnosis: DD Diagnosis: Intake CGAS/GAF: Problems: 1: 2: 3. 4. Intake Forms (all items in regular type must be turned into the office for a case to be opened) Client Information Sheet Intake Consents form (signed by guardian, not foster parent) Billing Codes: No Show Policy Intake packet* (staff pay=2 hrs) PCP Notification BA Assessment* (BCBA/BCaBA) Release of Information (for case managers) Counseling-Intake* Bio-Psychosocial Evaluation/In-Depth Assessment *includes Bio-InDepth/CFARS/MTP Event Note for intake session Sessions** (CPC: bill the service listed on auth; DNB for CBC-CF) BA Services-BCBA** Event Note for Assessment documents (Bio-InDepth/CFARS/MTP) BA Services-BCaBA** Children’s Functional Assessment Rating (CFARS) Counseling-Individual/Family** Treatment Plan (signed by client and guardian) **CPC pays for intake session, Client Rights Pamphlet (give to client/parent) CBC-CF does not Health & Safety Pamphlet (give to client/parent) Adult cases (age 18 and over) Functional Assessment Rating (FARS) Session/units used tracking: 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Date Date
Follow-up Forms Due Date What’s due When due Date Done Any remaining Event Notes in the month 1st Monday of following month Treatment Plan Review 3 months after Intake date State of Florida version of MHO Extension approval from Director 6 months after Intake date Treatment Plan Review (if extending past 6 months) CHS version of CFARS & State MHO Extension approval by Director 9 months after Intake date Treatment Plan Review (if extending past 9 months) State of Florida version of MHO Extension approval by Director 12 months after Intake date Treatment Plan Review (if extending past 12 months) CHS version of CFARS & State MHO Intakes Consent Treatment Review for Discharge Within 15 days after last session if CHS version of CFARS & State MHO planned discharge Consumer Discharge Rating Consumer Satisfaction Survey Treatment Review for Discharge Within 15 days after decision to State of Florida version of MHO discharge administratively Instructions: THIS IS FOR YOU TO KEEP. YOU CAN USE IT TO TRACK DUE DATES FOR THIS CASE.
Revised 01/15
A D A P T Client Information Sheet BEHAVIORAL SERVICES DEMOGRAPHIC INFORMATION
Client First Name/Last Name: Social Security#: Birth Date: Age: Sex: Male Female Address: County: City: State: FL Zip: Email: Phone: Phone #2: Bilingual needed? no yes: School: Placement: Reg Ed Emotional/Behavioral Other Exceptional Ed Race: White Black Native American/Alaskan Asian Pacific Islander Multi-racial Ethnic: None Puerto Rican Mexican Cuban Other Hispanic Haitian Legal status: Minor Dependent Minor (foster home) Delinquent Minor Competent Adult Incompetent Adult FAMILY COMPOSITION Name Relationship Age Other Information
Other Parent/Guardian: Relationship: Phone: Address: email: OTHER CONTACTS Legal Guardian(s) Name/Relationship*: Phone: Emergency Contact Name/Relationship*: Phone: Referral Source: Name/Agency: Phone: Primary Care Physician: Name/Agency: Phone: Dependency Case Mgr: Name/Agency: Phone: Other Case Manager: Name/Agency: Phone: DJJ Worker/Probation Off: Name/Agency: Phone: Other MH Counseling: Name/Agency: Phone: Psychiatric/Medication: Name/Agency: Phone: School Contact: Name/Agency: Phone: Other: Name/Agency: Phone: *include address of guardian/emergency contact, if different from above: FUNDING Funding Type: Medicaid Healthy Kids Insurance FSPT CMS Other: Funding Agency:: Subscriber #: ADMINISTRATIVE INFORMATION
Primary Clinician Name: Intake Date: Client ID#: Primary Diagnosis Code: Developmental Disability Diagnosis Code: Intake GAF: Prior Adapt record(s) for this client filed in discharge year(s): Updated 06/12
A D A P T Intake Consents & Orientation BEHAVIORAL SERVICES
Client Name: Date of Birth:
______(initial) HEALTH & SAFETY: I received a copy of the Health & Safety pamphlet (red), and it was explained to me, including wellness education; Adapt’s policies on substance use, weapons, abuse reporting, emergency procedures; Adapt’s responsibility to respond to client risk of danger to self/others, and after-hours crisis/emergency phone numbers. ______(initial) CLIENT RIGHTS: I received a copy of the Client Rights pamphlet (yellow), and it was explained to me, including what to expect in the assessment, treatment planning, treatment & discharge process; client rights & responsibilities; agency rights & responsibilities; grievance process; treatment philosophy; Primary Clinician name/phone number; and office hours/phone number. ______(initial) LIMITS TO CONFIDENTIALITY: I understand that information about the above-named client will not be shared with anyone without my consent, except under the following conditions: Adapt is required to report suspicion of child/elder/disabled adults abuse & neglect. Adapt is required to release information for the purpose of abuse/neglect investigations. Adapt is allowed to warn potential victims if we believe that their lives are in danger. Adapt is required to release a copy of records and/or testimony if subpoenaed in court. ______(initial) COMMUNICATION SECURITY: I understand that Adapt staff are required to use encryption when emailing client information, in order to protect its privacy. I understand that cellular phone communication is not secure, however I authorize Adapt staff to use cellular phones to communicate about the above-named client with me and others that I have approved. ______(initial) STATEMENT OF AUTHORITY TO CONSENT: I certify that I have the legal authority to consent to behavioral health treatment, release of information, and all legal issues involving the above- named client. If my status as legal guardian should change, I will immediately notify Adapt Behavioral Services of the name, address, and telephone number of the person who has assumed guardianship of the above-named client. ______(initial) CONSENT FOR TREATMENT AND TREATMENT LOCATION: I consent for the above- named client to participate in assessment and treatment through Adapt Behavioral Services, including sharing relevant confidential information to coordinate care with others involved in services (e.g., client’s family members, school personnel, other service providers) ______(initial) FUNDING AUTHORIZATION: I authorize Adapt Behavioral Services to release relevant confidential information to my current funding source in order to process claims, obtain reimbursement, and comply with the funding source’s auditing requirements. ______(initial) FINANCIAL RESPONSIBILITY: I understand that I will be responsible for any charges that my funding source does not cover, including any services provided after my insurance has lapsed, fees described on the Copayment Agreement, and fees described in the No Show/Cancellation Policy. ______(initial) OTHER INSURANCE: I understand that publicly funded insurance (Medicaid, Healthy Kids) is payor of last resort and that other insurance coverage must be used first. I understand that I will be responisble for 100% of all charges if I fail to disclose other insurance coverage for the above-named client.
I understand that I may revoke consent for the above at anytime, however, I cannot revoke consent for action that has already been taken. A copy of this release shall be valid as the original. THIS CONSENT EXPIRES 1 YEAR FROM THE DATE SIGNED.
______Client/Legal Guardian Signature Date Revised 04/16
A D A P T No Show/Cancellation Policy BEHAVIORAL SERVICES
Client: Date of Birth:
Regular attendance at scheduled appointments is very important. Our services will not be effective in helping you if you do not keep your appointments. Irregular attendance, especially a “no show,” is also inconvenient and costly for the staff assigned to help you. It is therefore your responsibility to attend all scheduled appointments.
CANCELLATION POLICY: If you call your assigned clinician at least an hour before your scheduled appointment, it is considered a “Cancellation,” although 24-hour notice is preferred. 1. After the first cancellation, the staff person will call you to reschedule. 2. After two cancellations in a row, the Director will send you a letter explaining that you must call him/her if you desire to continue services. 3. After the third cancellation in a row, services will be terminated. 4. If you cancel three times, with some attendance in between each cancellation, your therapist will discuss with you some possible solutions to the problem of irregular attendance.
NO SHOW POLICY: If you do not call to cancel at least an hour before the scheduled appointment time, it is considered a “No Show.” 1. If you fail to notify your assigned clinician prior to a missed in-home session, you will be charged a $10 travel fee to cover the staff cost of traveling to your home for the missed appointment. 2. If you fail to notify your assigned clinician prior to an in-office or in-school session, you may be charged a $10 travel fee if the staff traveled to that location specifically for that session. 3. After the first “No Show,” the staff person will call to reschedule the appointment. 4. After the second “No Show,” the Program Manager will send you a letter notifying you that services have been suspended and that you are required to pay the travel fees for both missed sessions in order to reinstate services. 5. After the third “No Show,” your case will be closed.
If these services are mandated or court-ordered, the person responsible for monitoring compliance with the mandate (e.g., dependency case manager, probation officer) will be notified of repeated cancellations/no shows and suspension or termination of services.
I understand Adapt Behavioral Service’s No Show/Cancellation policy and understand that regular attendance is necessary for treatment to be effective. Therefore, I agree to attend all scheduled sessions. If I cannot keep an appointment, I will call the staff 24 hours in advance to reschedule. If I have an emergency that prevents me from attending, I will call the assigned clinician at least one hour before the appointment to cancel.
______Client Signature Date
______Parent/Caregiver Signature Date Revised 11/12
A D A P T Primary Care Physician Notification BEHAVIORAL SERVICES
Client Name: Date of Birth:
This client’s Primary Care Physician is as follows: PCP Name: Mailing Address: City, State, Zip: Phone/Fax: Email address:
Purpose of Document Release: Physician’s office: FOR NOTIFICATION PURPOSES ONLY -- DO NOT SEND RECORDS This document serves as notification to the Primary Care Physician that counseling, behavior analysis, and/or psychiatric services are being provided by Adapt Behavioral Services: Intake date: Clinician name: Clinician phone: Acknowledgement: By signing below, I authorize Adapt Behavioral Services to release a copy of this document to the PCP named above. I further authorize exchange of confidential information between the PCP and Adapt Behavioral Services for the purpose of coordination of care. Contact information for Adapt Behavioral Services is as follows: Orange/Seminole/Lake: 225 S. Swoope Ave. #211, Maitland, FL 32751, (407) 622-0444 Volusia/Flagler/St. John’s: 533 N. Nova Rd. #204, Ormond Beach, FL 32174, (386) 898-5003 Osceola/Polk: 3483 W. Vine St., Kissimmee, FL 34741, (407) 928-0444
. I understand that I may refuse to sign this authorization and that my refusal to sign will not affect my ability to obtain treatment from Adapt Behavioral Services. . I understand that I may revoke this authorization in writing at any time, however I cannot revoke authorization for action that has already been taken. . A copy of this release shall be valid as the original.
THIS CONSENT EXPIRES 1 YEAR FROM THE DATE SIGNED UNLESS OTHERWISE SPECIFIED.
______Client/Legal Guardian Signature Date
Revised 07/16
A D A P T Consent to Release Information BEHAVIORAL SERVICES
Client Name: Date of Birth: I authorize Adapt Behavioral Services Orange/Seminole/Lake Osceola/Polk Volusia/Flagler/St. Johns 225 S. Swoope Ave. #211 3483 W. Vine St. 533 N. Nova Rd. #204 Maitland, FL 32751 Kissimmee, FL 34741 Ormond Beach, FL 32174 (407) 622-0444 (407) 928-0444 (386) 898-5003 (407) 699-0444 fax (407) 518-0808 fax (386) 675-6490 fax to exchange confidential information concerning the above-named client with the following: Agency/Contact: Mailing Address: City, State, Zip: Phone/Fax: Email: I authorize: Informal communication regarding all client information between both parties. AND/OR Copies of the following documents to be mailed/faxed to the agency listed above Copies of the following documents to be mailed/faxed to Adapt Behavioral Services Limited verbal communication (no copies) related only to the following records (Check which documents are authorized to be released) Bio-Psychosocial Evaluation Psychiatric Evaluation Report Cards/Transcripts Licensed Evaluation Medication Management Behavioral Program Treatment Plan/Reviews Medical History & Physical Individual Education Plan Progress Summary Immunization Record Other: Discharge Review Lab Results Other:
Purpose of Release: Assessment Treatment Coordination Other, specify: Notification of compliance with court-ordered treatment (e.g., DCF, DJJ)
. I understand that I may refuse to sign this Authorization and that my refusal to sign will not affect my ability to obtain treatment from Adapt Behavioral Services. . I understand that if I am court-ordered into treatment and refuse to allow Adapt Behavioral Services to share information with those responsible for monitoring my compliance with mandated treatment, this may result in negative consequences imposed by the court. . I understand that I may revoke this authorization in writing at any time, however I cannot revoke authorization for action that has already been taken. . A copy of this release shall be valid as the original. THIS CONSENT EXPIRES 1 YEAR FROM THE DATE SIGNED UNLESS OTHERWISE SPECIFIED.
______Client/Legal Guardian Signature Date
A D A P T Bio-Psychosocial Evaluation In-Depth Assessment BEHAVIORAL SERVICES
Client: Date of Birth: Age: Sex: Race: Primary Clinician: Intake Date: PSYCHOSOCIAL STRESSORS (circle descriptors or, if typing, delete descriptors that do not apply)
Family changes: divorce/remarriage, death/birth, estranged, caregiver changes, other: Family conflict: between siblings, parent-child, couple/marital, extended family, other: Social/Relationships: lack of friends, peer conflict/rejection, death/loss of friend, other: Home Environment: crowded, moves, unsafe, homeless, risk of eviction/foreclosure, other: Educational: school changes, academic delays, poor grades, discipline, other: Financial/Work: low income, unemployed, supervisor conflict, retirement, other: Legal: protective services, arrest, incarceration, probation, litigation, police called, other: Disability/disorder: SSI, injury, chronic illness, physical limitation, developmental, other: Trauma/abuse: sexual abuse, physical abuse, foster care, crime victim, natural disaster, other: Current safety threat (written safety plan required): Other stressor: Describe: ______DEVELOPMENTAL/MEDICAL/PHYSICAL HISTORY *First 3 items required for children only *Developmental history: normal, delays in: crawling, walking, speech, other: *Pregnancy/delivery: *Immunizations up-to-date (children only): yes no, explain: Client’s current & past medical issues (check all that apply & provide details below): none Seizure disorder Hypertension Gross motor problem Headaches Diabetes Heart problem Fine motor problem Stomach aches HIV/AIDS Kidney problem Prenatal drug exposure Bowel problem Brain injury Thyroid problem Life-threatening illness*** Allergies Paraplegia Vision impairment ***(requires safety plan) Asthma Dental problem Hearing impairment Other: Details & medications for above:
______Family medical history: MENTAL HEALTH TREATMENT HISTORY (include treatment type, provider/agency name, dates of treatment) Outpatient: Inpatient/crisis unit: Current psychotropic medications/dosages: Results/side effects of current medications: Prior medications/results/side effects: Prior diagnoses: Family mental health/substance abuse issues: Additional information: Client has psychiatric advance directive? Yes No (if yes, attach a copy of written advance directive)
______
______1 Revised 04/16 ______
A D A P T Bio-Psychosocial Evaluation In-Depth Assessment BEHAVIORAL SERVICES Client: EDUCATIONAL/EMPLOYMENT HISTORY Highest grade completed: Learning/academic delays? Yes No Reading level? School performance: School behavior: Currently employed? Yes No Employer: Work performance/issues: BEHAVIORAL HEALTH/MENTAL STATUS (rating of 4+ requires intervention on MTP or rationale for omission) Severity: 1=no problem; 2-3=slight problem; 4-6=needs treatment; 7-9=may need hospitalization; P=past problem (>3 mo ago) Depression: sad, withdrawn, flat affect, hopeless, apathetic, lethargic, other: Anxiety: worries, fearful, phobic, panic, OCD, PTSD symptoms, sleepless, other: Hyper-manic: inattentive, disruptive, overactive, impulsive, distractible, sleepless, other: Psychosis: hallucinations, delusions, disoriented, loose associations, other: Substance use*: alcohol, tobacco, illegal, prescription, binges, cravings, other: Peer problems: argues, provokes, verbal abuse, physical aggression, rejected, other: Authority problems: defiant, argues, verbal abuse/cursing, physical aggression, other: Family conflict: conflict with sibling, parent, child, partner, extended family, other: Sexuality issues: sexual acting out, sexual preference issues, gender confusion, other: Self-care problems: poor hygiene, needs assistance, daytime enuresis, encopresis, other: Antisocial: breaks societal rules, lies, truant, curfew violations, firesetting, theft, other: Danger to self**: risk-taking, suicidal ideation/plan, self injury, suicide attempt, other: Danger to others**: violent, causes injury, weapons, homicidal ideation/threats, other: Sleep issues: resists bedtime, wakes frequently, wakes early, wets bed, other: Other symptom: Average hours sleep at night: *Rating of 7+ on substance use requires referral to substance abuse assessment/treatment **Rating of 7+ on danger to self or danger to others requires a written safety plan/crisis assessment Details & history of symptoms:
______OBSERVATION/ASSESSMENT OF CLIENT & FAMILY FUNCTIONING Client’s current GAF: ______Affect/Emotionality: calm, restless, happy, sad, anxious, angry, annoyed, apathetic, other: Language: age appropriate, articulation issue, nonverbal, speech delay, echoic, other: Cognitive/developmental: IQ low/average/high, Autism/ASD, learning disability, other: Gross/Fine motor: no issues, difficulties: walking, running, pencil grip, pincer grasp, other: Sensory: no issues, hearing impaired, deaf, hearing aid, vision impaired, blind, glasses. other: Self-care: age-appropriate, verbal prompting, physical assistance, dependent, other: Social functioning: friendly, shy, talkative, guarded, odd behavior, poor eye contact, other: Parent-child relationship: Family communication style: Client strengths: Family strengths: Client: TREATMENT CONSIDERATIONS
2 Revised 04/16
A D A P T Bio-Psychosocial Evaluation In-Depth Assessment BEHAVIORAL SERVICES
Client perception of problems/needs: Client/family treatment goals: Religious/culturally sensitive issues: Gender sensitive issues: Current services/supports: Other desired services/supports: Client/caregiver motivation: Other preferences: In-Depth Assmt criteria: age 0-5 & symptoms atypical for age/development OR “high risk” (check all that apply): EBD school placement reopen w/in 6 months Baker Act/residential in past year 6+ rating on CFARS/FARS INTEGRATED SUMMARY (include significant findings in all areas, relationship between issues, factors affecting outcome) ______Effectiveness of past interventions (include reasons, if low progress): ______Focus of treatment: Services needed: ¼ hr units per for Problems to address: 1. 2. 3. 4. Discharge criteria: Provisional Diagnoses/Clinical Impressions, based on the DSM-5 (include ICD-10 codes before each title):
Discussion of Diagnoses with Licensed Supervisor: Date: I agree with the treatment recommendations and provisional diagnoses contained in this evaluation.
______Primary Clinician/Credentials Date Completed Licensed Supervisor/Credentials Date Discussed
3 Revised 04/16
A D A P T Event Note BEHAVIORAL SERVICES
Instructions: Write note within 24 hours after event. Turn in to office for filing in client record within 1 week.
Client Name: Date: Units of Service: Location: Start Time: am/ pm End: am/ pm SERVICE: TBOS-Therapy (preventing more restrictive placement; Individual & family therapy; collaborative development of the aftercare plan) Individual & Family Therapy (insight oriented, cognitive behavioral, or supportive therapy to an individual or family--not school personnel) 90791 (Ins/HK-Intake) Psychotherapy: 90834 (45min) 90837 (60min) Family Therapy: 90847 (WITH client) 90846 (W/OUT client) Funding ineligibility notification No show Cancellation Week without service Other:
Problem #1: PROGRESS: Problem #2: PROGRESS: Problem #3: PROGRESS: Problem #4: PROGRESS: PARTICIPANTS: Client Other(s): Relationship/Name PRESENTING ISSUES: INTERVENTIONS: 1. Initial session with client and family ______1. Began developing rapport and creating positive expectations ______for treatment success. Oriented client and family to treatment. ______2. ______2. . ______REFERRAL INFORMATION GIVEN FOR: Agency: Service Type: LEVEL OF PARTICIPATION/RESPONSE TO INTERVENTION: Client: Participation/Response by other: Follow through on homework: PLAN: Homework assigned: Focus of next session:
Signature: Name: Credentials: Date: Abbreviation Legend: Clt=client Tch=Teacher =increase =decrease mgmt=management Mx=mother SF=step-father Dx=diagnosis Tx=treatment +=positive wk=week GF=girlfriend Fx=father GM=grandmother Hx=history Bx=behavior x=times w/=with BF=boyfriend
Revised 09/14
A D A P T Event Note BEHAVIORAL SERVICES
Instructions: Write note within 24 hours after event. Turn in to office for filing in client record within 1 week.
Client Name: Date: Units of Service: Location: Start Time: am/ pm End: am/ pm SERVICE: TBOS-Therapy (preventing more restrictive placement; Individual & family therapy; collaborative development of the aftercare plan) Individual & Family Therapy (insight oriented, cognitive behavioral, or supportive therapy to an individual or family--not school personnel) 90791 (Ins/HK-Intake) Psychotherapy: 90834 (45min) 90837 (60min) Family Therapy: 90847 (WITH client) 90846 (W/OUT client) Funding ineligibility notification No show Cancellation Week without service Other:
Problem #1: PROGRESS: Problem #2: PROGRESS: Problem #3: PROGRESS: Problem #4: PROGRESS:
PARTICIPANTS: Client Other(s): Relationship/Name
PRESENTING ISSUES: INTERVENTIONS: ______1. Documented assessment of client and family is needed in ______1. Completed Biopsychosocial Evaluation/In-Depth ______order to formulate an effective plan for treatment. ______Assessment and Children's Functional Assessment Rating ______2. Treatment plan needed to establish goals, objectives, and ______Scale following intake therapy session. ______treatment strategies for course of therapy. ______2. Completed written Treatment Plan, including input from ______client and family. ______REFERRAL INFORMATION GIVEN FOR: Agency: Service Type: ______LEVEL OF PARTICIPATION/RESPONSE TO INTERVENTION: Client: Participation/Response by other: Follow through on homework: PLAN: Homework assigned: Focus of next session:
Signature: Name: Credentials: Date: Abbreviation Legend: Clt=client Tch=Teacher =increase =decrease mgmt=management Mx=mother SF=step-father Dx=diagnosis Tx=treatment +=positive wk=week GF=girlfriend Fx=father GM=grandmother Hx=history Bx=behavior x=times w/=with BF=boyfriend
Revised 09/14
A D A P T Treatment Plan BEHAVIORAL SERVICES
Client: DOB: Intake Date: Primary Clinician: Other Clinician:
DIAGNOSES* (ICD-10 code before each title; evaluation conducted prior to development of treatment plan)
*Based on evaluation by OR consultation with licensed clinician: on CLIENT & SUPPORT SYSTEM STRENGTHS, ABILITIES, NEEDS & PREFERENCES Other professional service needs: Client strengths: Caregiver strengths: Client/caregiver limitations: Client/caregiver preferences: DJJ/Corrections/DCF legal requirements:
SERVICES TO BE PROVIDED (service type/billing code title, frequency & duration)
Individual & Family Therapy ¼ hr units per for TBOS-Therapy (Medicaid/CMS only) ¼ hr units per for ¼ hr units per for TBOS: Intended to prevent more intensive/restrictive behavioral health placement. Justification on problem sheets.
DISCHARGE/TRANSITION PLAN (includes aftercare plan for TBOS services) Client/caregivers will be prepared for independence Client/caregivers will have natural supports Referral will be made for new aftercare services Service intensity will be decreased TBOS aftercare providers/services/activities (e.g., professional services, support grps, religious/athletic/hobbies):
ATTACHMENTS Problem #1 Description Sheet: Problem #2 Description Sheet: Problem #3 Description Sheet: Problem #4 Description Sheet:
This plan is effective as of ______. The following have participated in the development of this Treatment Plan:
______Client Signature Date Primary Clinician Signature/Credentials Date
______Parent Guardian DCM Signature Date Other Participant Signature/Relationship Date The services contained in this treatment plan are medically necessary and appropriate for this client’s diagnosis and
Revised 10/15
A D A P T Treatment Plan BEHAVIORAL SERVICES
Client: Intake Date: PROBLEM #1 TITLE: Problem definition: ______Client desired outcome (in quotes): Guardian desired outcome (in quotes): Baseline level/severity (level at intake, include TBOS justification): ______Measurable discharge criteria: ______Measurable OUTCOME objective to be completed by next review date ( ): O1: Assessment/pattern analysis (trigger situations, family dynamics, other contributing variables, where/when): ______Description of specific treatment strategies (include strategies for integration into community/family): Interventions with client individually: ______Interventions with support system (family/school/others): ______Measurable PROCESS objectives to be completed by next review date ( ): P1:
P2:
P3:
Revised 09/14
A D A P T Treatment Plan BEHAVIORAL SERVICES
Revised 09/14
A D A P T Treatment Plan BEHAVIORAL SERVICES
Client: Intake Date: PROBLEM #2 TITLE: Problem definition: ______Client desired outcome (in quotes): Guardian desired outcome (in quotes): Baseline level/severity (level at intake, include TBOS justification): ______Measurable discharge criteria: ______Measurable OUTCOME objective to be completed by next review date ( ): O1: Assessment/pattern analysis (trigger situations, family dynamics, other contributing variables, where/when): ______Description of specific treatment strategies (include strategies for integration into community/family): Interventions with client individually: ______Interventions with support system (family/school/others): ______Measurable PROCESS objectives to be completed by next review date ( ): P1:
P2:
P3:
Revised 09/14
A D A P T Treatment Plan BEHAVIORAL SERVICES
Revised 09/14
A D A P T Treatment Plan BEHAVIORAL SERVICES
Client: Intake Date: PROBLEM #3 TITLE: Problem definition: ______Client desired outcome (in quotes): Guardian desired outcome (in quotes): Baseline level/severity (level at intake, include TBOS justification): ______Measurable discharge criteria: ______Measurable OUTCOME objective to be completed by next review date ( ): O1: Assessment/pattern analysis (trigger situations, family dynamics, other contributing variables, where/when): ______Description of specific treatment strategies (include strategies for integration into community/family): Interventions with client individually: ______Interventions with support system (family/school/others): ______Measurable PROCESS objectives to be completed by next review date ( ): P1:
P2:
P3:
Revised 09/14
A D A P T Treatment Plan BEHAVIORAL SERVICES
Revised 09/14
A D A P T Treatment Plan BEHAVIORAL SERVICES
Client: Intake Date: PROBLEM #4 TITLE: Problem definition: ______Client desired outcome (in quotes): Guardian desired outcome (in quotes): Baseline level/severity (level at intake, include TBOS justification): ______Measurable discharge criteria: ______Measurable OUTCOME objective to be completed by next review date ( ): O1: Assessment/pattern analysis (trigger situations, family dynamics, other contributing variables, where/when): ______Description of specific treatment strategies (include strategies for integration into community/family): Interventions with client individually: ______Interventions with support system (family/school/others): ______Measurable PROCESS objectives to be completed by next review date ( ): P1:
P2:
P3:
Revised 09/14
A D A P T Treatment Plan BEHAVIORAL SERVICES
Revised 09/14
A D A P T CFARS (age 0-17) BEHAVIORAL SERVICES
Client Name: Error: Reference source not found Client ID#: Error: Reference source not found Intake Date: Age: Error: Reference source not found Instructions: Complete for all clients age 0-17 at admission, every 6 months & planned discharge
Current Evaluation Date: Funder on date of evaluation: Medicaid plans: Healthy Kids plans: Other plans: 13=AHCA 12=PsychCare 23=Amerigroup HK 49=CMS (non-Medicaid) 09=Amerigroup 08=United 114=Cenpatico HK 21=FSPT CBC-CF 70=Cenpatico 100=Wellcare 25=United HK 102=FSPT-CPC 113=CMS-Title 19 104=Wellcare HK 00=Private insurance 111=Magellan Other: Other: Purpose of Evaluation: 1=Admission 2=Every 6 months 3=Planned discharge (within 3 weeks after last session) No Minor Needs Hospitalization Children’s Functional Assessment Rating Scale (CFARS) prob problem outpatient may be treatment needed (for clients age 0-17) 1 2 3 4 5 6 7 8 9 Clinical Domains Depression: Depressed Mood, Sleep Problems, Sad, Hopeless, Withdrawn, Irritable, Lacks Energy/Interest, Anti-Depression Meds Anxiety: Anxious/Tense, Guilt, Phobic, Worried/Fearful, Anti-Anxiety Meds, Obsessive/Compulsive, Panic Hyperactivity: Manic, Inattentive, Agitated, Sleep Deficit, Overactive, Impulsivity, Mood Swings, Pressured Speech, Anti-Manic Meds, ADHD Meds Thought Process: Illogical, Delusional, Hallucinations, Paranoid, Ruminative, Derailed Thinking, Loose Association, Anti-Psychotic Meds, Disoriented Cognitive Performance: Poor Memory, Low Self-Awareness, Slow Processing, Attention/Concentration, Developmental Disability, Concrete Thinking, Impaired Judgment Medical/Physical: Acute Illness, Hypochondria, CNS Disorder Behavior, Chronic Illness, Need of Med/Dental Care, Pregnant, Poor Nutrition, Enuretic/Encoperetic, Eating Disorder, Seizures, Stress Related Illness Traumatic Stress: Acute, Dreams/Nightmares, Chronic, Detached, Avoidance, Repression/Amnesia, Upsetting memories, Hypervigilance Substance Use: Alcohol, Drugs, Dependence, Abuse, Over the Counter Drugs, Craving/Urge, DUI, Medical Control, Interferes with Functioning, IV Drugs Interpersonal Relationships: Poor Social Skills, Overly Shy, Problems with Friends, Difficulty Establishing./Maintaining Relationships Behavior in Home: Defies Authority, Disregards Rules, Conflict with Relative, Conflict with Parent/Caregiver, Conflict with Sibling/Peer ADL Functioning: Handicapped, Permanent Disability, Not Age Appropriate in: Communication, Self-Care, Hygiene, Mobility Socio-Legal: Disregards Rules/Norms, Offense to Property, Offense to Persons, Firesetting, Probation/Parole, Pending Charges, Dishonest/Lying, Gang member, Uses/Cons Others, Incompetent to Proceed, Detention/Commitment Work/School: Absenteeism, Skips Classes, Tardiness, Suspended, Dropped Out, Terminated/Expelled, Poor Performance, Learning Disability, Illiterate, Defies Authority, Disruptive Behaviors, Danger to Self: Suicidal Ideation, Current Plan, Recent Attempt, Past Attempt, Self- Injury, Risk Taking Behaviors, Serious Self-Neglect, Inability to Care for Self Danger to Others: Violent/Physically Aggressive, Threats, Causes Serious Injuries, Homicidal Ideation/Threats/Attempts, Uses Weapons, Cruelty to Animals, Sexual Assault
Security/Management Needs: Suicide Watch, No Harm Contract, Locked Unit, Protection from Others, Seclusion, Home with Supervision, Run/Escape Risk, Restraint, Involuntary Exam, Time-out, Monitored House Arrest, One-to-One Supervision
Clinician Signature: ______Date:______
Revised 08/15
______Signature/Credentials