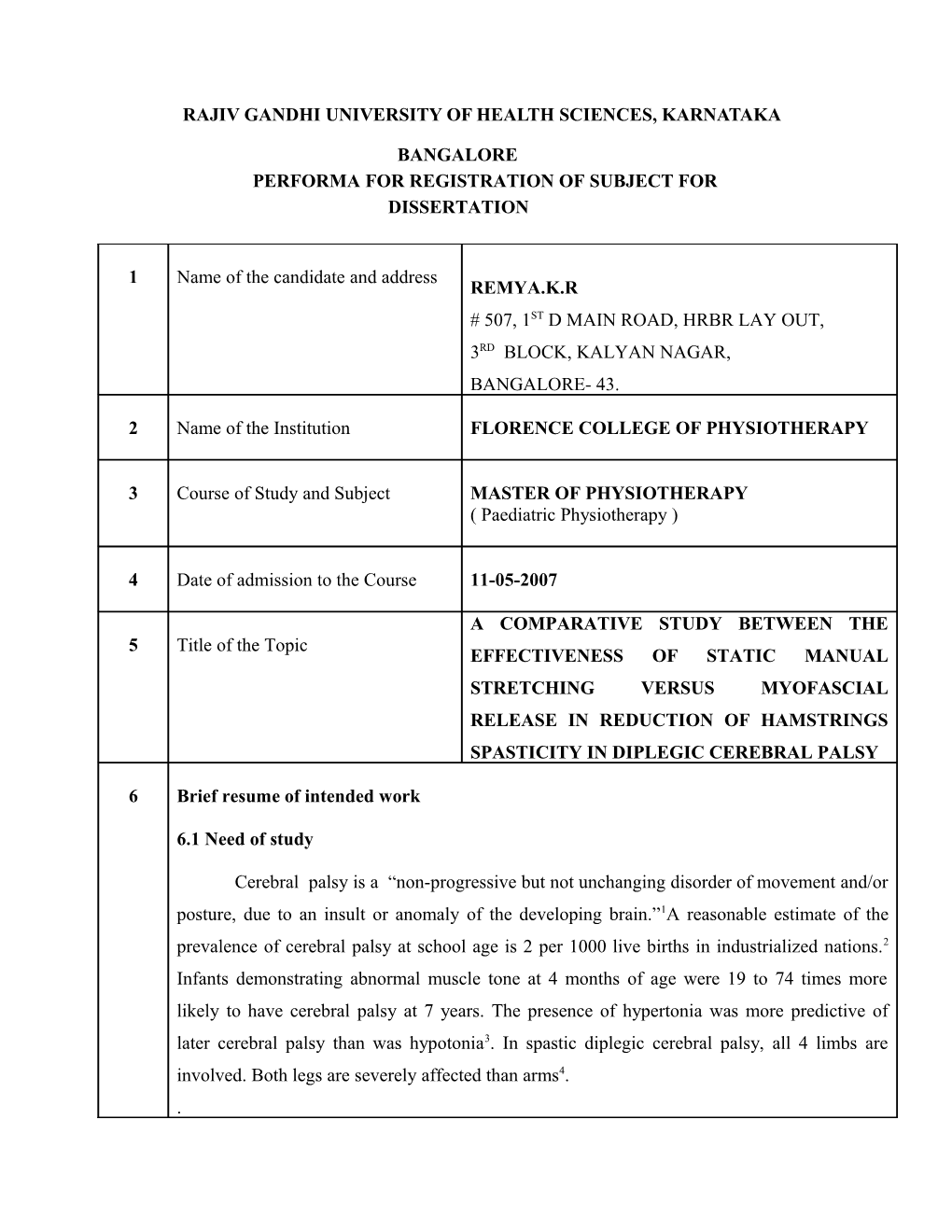
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, KARNATAKA
BANGALORE PERFORMA FOR REGISTRATION OF SUBJECT FOR DISSERTATION
1 Name of the candidate and address REMYA.K.R # 507, 1ST D MAIN ROAD, HRBR LAY OUT, 3RD BLOCK, KALYAN NAGAR, BANGALORE- 43.
2 Name of the Institution FLORENCE COLLEGE OF PHYSIOTHERAPY
3 Course of Study and Subject MASTER OF PHYSIOTHERAPY ( Paediatric Physiotherapy )
4 Date of admission to the Course 11-05-2007
A COMPARATIVE STUDY BETWEEN THE 5 Title of the Topic EFFECTIVENESS OF STATIC MANUAL STRETCHING VERSUS MYOFASCIAL RELEASE IN REDUCTION OF HAMSTRINGS SPASTICITY IN DIPLEGIC CEREBRAL PALSY
6 Brief resume of intended work
6.1 Need of study
Cerebral palsy is a “non-progressive but not unchanging disorder of movement and/or posture, due to an insult or anomaly of the developing brain.”1A reasonable estimate of the prevalence of cerebral palsy at school age is 2 per 1000 live births in industrialized nations.2 Infants demonstrating abnormal muscle tone at 4 months of age were 19 to 74 times more likely to have cerebral palsy at 7 years. The presence of hypertonia was more predictive of later cerebral palsy than was hypotonia3. In spastic diplegic cerebral palsy, all 4 limbs are involved. Both legs are severely affected than arms4. . When muscles are spastic, there is an imbalance of the muscle pull around the joint. This increases the child’s risk of developing a joint deformity or a muscle contracture. When hamstring muscle is spastic in diplegic cerebral palsy child, the normal pattern of sitting and walking is delayed5. It is necessary to relieve spasticity to allow development of normal motor pattern. Both static manual stretching and myofascial release has effects on relieving spasticity6,7.
A comprehensive physical therapy treatment program should be designed to help a child to obtain maximal functional independence to improve gross motor function and maintain joint range of motion to prevent joint deformities and muscle contractures. Spasticity is a factor which restricts to achieve this goal. So, in order to reach the treatment to maximum beneficial level, spasticity should be controlled. Treatment of spasticity consists of certain conventional techniques which include static manual stretching.
Myofascial release is a new approach which produces consistent result in children suffering from hamstring spasticity8. It involves the treatment of the neuromuscular somatic unit as a whole and release of somatic dysfunctional related imbalances, which affect a discrete region, a vertebral level, an entire limb or the whole body. MFR( Myofascial Release ) may act in future as a facilitator and intensifier of treatment for more consistent effectiveness and results of diplegic cerebral palsy children.
Compared to medical and surgical treatment for spasticity, static manual stretching and MFR( Myofascial Release) are less expensive, safe and having very less side effects. So, this study means to compare the effectiveness of these two methods- static manual stretching versus myofascial release- in reducing spasticity and to apply the results in making the treatment of spastic diplegic cerebral palsy children in more effective and affordable way.
6.2 Review of literature
1. Dr. Manisha. C. Desai & Dr. Chhaya. V. Verma (1998): Conducted a study to find out the efficacy of sustained passive stretching to reduce spasticity in 30 subjects and concluded that sustained passive stretching causes reduction in spasticity by the stimulation of the Golgi Tendon Organ which is the length sensitive receptor which causes inhibition of corresponding muscle.
2. Carolyn Kisner (2003) Stated that during static stretching the Golgi Tendon Organ, which monitors tension created by stretch of a muscle tendon unit, may override any facilitative impulses from primary afferents of the muscle spindle ( Ia afferent ) and subsequently may inhibit tension in the contractile units of the muscle being stretched.
3. John. F. Barnes, PT (1995) Myofascial Release techniques are utilized in a wide range of settings and diagnosis: pain, movement restrictions, spasm, spasticity, neurological dysfunction, i.e., cerebral palsy, head and birth injury, pediatrics etc. It is a whole body “hands-on” approach to the evaluation and treatment of the human structure. The therapist is taught to evaluate the fascial system through visual analysis of the human frame three dimensionally in space, by palpating the tissue texture and various fascial layers and observing the symmetry, rate, quality, and intensity of strength of the craniosacral rhythm.
4. Donna. L. Nimec, M.D.(2004) Describes in his book named ‘ Family Guide To Management Of Spasticity’ that treatment options of spasticity in children include different therapy models like Neuro Developmental therapy (NDT), Proprioceptive Neuro- muscular Facilitation (PNF), Conductive education and Manual therapy which include Myofascial Release and Craniosacral therapy.
5. Bandy, WB & Irion JM (1994) Conducted a study on effect of time on static stretch on the flexibility of the hamstring muscle and concluded that 30 second stretching is effective to improve flexibility of hamstrings. Flexibility of the hamstring muscles was determined by measuring knee extension ROM with the femur maintained in 90 degrees of hip flexion.
6. Webright, Randolph & Perrin (1997) Proved that 30 seconds of static stretching twice daily is effective for increasing ROM of knee and flexibility of hamstrings. It is as effective as repetitive active knee extensions 30 repititions, twice daily.
7. Bohannon & Smith (1987) They developed Modified Ashworth Scale for grading spasticity. They also proved that it is having inter rater reliability. The Modified Ashworth Scale includes 6 grades of spasticity.
8. Gogia et al (1987) Studied the reliability and validity of joint ankle measurements using a universal goniometer. Two physical therapists measured knee joint angle between 0 to 120 degrees of flexion on 30 volunteers (13 women & 17 men).Inter-rater reliability and validity were proved as high.
6.3 Objectives of the study
1. To find out the effectiveness of sustained passive stretching in reducing spasticity of hamstring muscles and to increase ROM(Range Of Motion) of knee extension in spastic diplegic cerebral palsy.
2. To find out the effectiveness of Myofascial Release in reducing spasticity of hamstring muscles and to increase ROM of knee extension in spastic diplegic cerebral palsy.
3. To compare the effectiveness of sustained passive stretching over Myofascial Release in reducing spasticity of hamstring muscles and to increase ROM of knee extension in spastic diplegic cerebral palsy.
6.4 Hypothesis
6.4.1. Null hypothesis
Use of myofascial release technique may not have any statistical significance for reducing spasticity in hamstring muscles of spastic diplegic cerebral palsy over manual static stretching.
6.4.2. Alternate Hypothesis Use of myofascial release may have statistical significance for reducing spasticity in hamstring muscles of spastic diplegic cerebral palsy over manual static stretching.
7 Materials and methods 7.1 Source of data
Florence rehabilitation center, Kalyan nagar, Bangalore-43
7.2 Methods of collecting data
7.2.1 Sample & Sampling method Sample size is 30 and samples will be selected by using Simple Random Sampling method.
7.2.2.Research design Comparative in design with pre & post test for both control and experimental groups.
7.2.3. Population
The population for study includes both male and female subjects between the age group of 4 to 10 years, diagnosed as spastic diplegic cerebral palsy .
7.2.4. Selection criteria
Inclusion criteria 1. Subjects diagnosed as spastic diplegic cerebral palsy. 2. Both male and female subjects. 3. Age group between 4 to 6 years. 4. Subjects with spasticity grade 2 as per Modified Ashworth Scale on hamstrings.
Exclusion criteria
1. Subjects who are receiving pharmacologic drugs for reducing spasticity. 2. Subjects with frequent epilepsy. 3. Subjects with mental retardation. 4. Subjects with hypersensitivity of skin
7.2.5. Measurement tool
Modified Ashworth Scale (MAS) Goniometry
7.2.6. Materials used Treatment couch Percussion hammer Pillow Pen, Pencil and Papers Bell Inch tape Weighing machine Goniometer
7.3.Intervention to be conducted
7.3.1.Methodology
Subjects who will report to Florence College of physiotherapy and rehabilitation center and diagnosed as spastic diplegic cerebral palsy will be taken after getting the informed consent from the parent of the subject for being a part of study and later screened for inclusion criteria and exclusion criteria. Those subjects who satisfy the inclusion criteria will be included for the study. Here 30 subjects will be included for the study and subjects will be randomly selected with 15 in each group (group A & group B). All the subjects selected for the study will undergo a pre treatment assessment of spasticity and range of motion using modified Ashworth scale and goniometry.
Patients in group A will receive sustained manual stretching for 30 seconds twice daily for 6 weeks9 on hamstring muscles of both right and left side. Patients in group B will receive myofascial release technique on hamstring muscles of both sides for 3 to 5 min10 twice daily for 6 weeks. Later the subjects who complete the training session successfully will under go post treatment assessment of spasticity and range of motion of knee extension using Modified Ashworth scale and goniometry respectively.
The statistical tools using for this study are Paired and unpaired ‘t’ test, Mc Nemar test and Chi-Squire test.
7.4 Ethical clearance
Ethical clearance has been obtained from the institution. 8 List of references
1. Sivenius J, Heinonen OP, Salonen JT, Riekkinen P. the significance of intensity of rehabilitation of stroke. Stroke. 1985 Nov-Dec;16(6):928-31
2. Van der Lee JH, Snel IA, Beckerman H, Lankhorst GJ, Wagenaar RC, Bouter LM. Exercise therapy for arm function in stroke patients. Clin Rehabil2001; 15: 20-31
3. Feys HM, De Weerdt WJ, Selz BE, Cox-Steck GA, Spichiger R, Vereeck L-E, et al, effect of a therapeutic intervension for the hemiplegic upper limb in acute phase after stroke. Stroke 1998; 29: 785- 792.
4. RY Wang, effect of neuromuscular facilitation on the gait of patients with hemiplegia of long and short duration. Phys Ther Vol. 74, No. 12, December 1994, pp. 1108
5. Brunnstrom S. Movement therapy in hemiplegia: a neurophysiological approach. New York: Harper & Row; 1970
6. Bobath B. Adult hemiplegia: evaluation and treatment. 2nd edn. London: Heineman Medical Book; 1978 7. Bohannon,R, and Smith, M: Interater reliability of a modified Asworth scale of muscle spasticity. Phys Ther 67:206, 1987. 8. Fugl-Meyer, A, et al: The post stroke hemiplegic patient, 1.A method for evaluation of physical performance. Scand J Rehabil Med 7:13, 1976
9. Cristopher Hastellet al. Principles and practice of medicine 19th edition, 2002 pp.1159
10. Susan B. O’Sullivan, Thomas J. Schmitz. Physical rehabilitation assessment and treatment 4th edition, 2001. pp.531