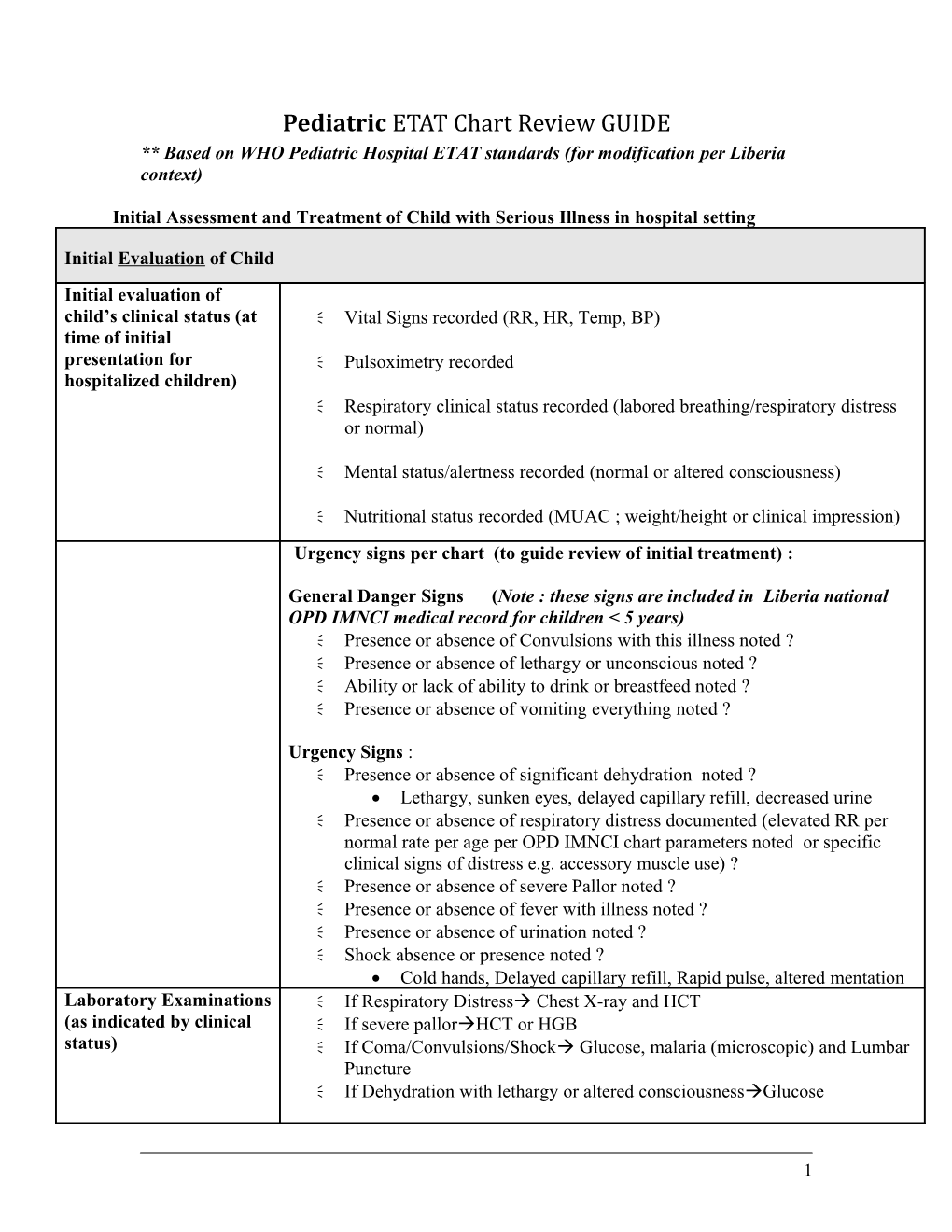
Pediatric ETAT Chart Review GUIDE ** Based on WHO Pediatric Hospital ETAT standards (for modification per Liberia context)
Initial Assessment and Treatment of Child with Serious Illness in hospital setting
Initial Evaluation of Child Initial evaluation of child’s clinical status (at Vital Signs recorded (RR, HR, Temp, BP) time of initial presentation for Pulsoximetry recorded hospitalized children) Respiratory clinical status recorded (labored breathing/respiratory distress or normal)
Mental status/alertness recorded (normal or altered consciousness)
Nutritional status recorded (MUAC ; weight/height or clinical impression) Urgency signs per chart (to guide review of initial treatment) :
General Danger Signs (Note : these signs are included in Liberia national OPD IMNCI medical record for children < 5 years) Presence or absence of Convulsions with this illness noted ? Presence or absence of lethargy or unconscious noted ? Ability or lack of ability to drink or breastfeed noted ? Presence or absence of vomiting everything noted ?
Urgency Signs : Presence or absence of significant dehydration noted ? Lethargy, sunken eyes, delayed capillary refill, decreased urine Presence or absence of respiratory distress documented (elevated RR per normal rate per age per OPD IMNCI chart parameters noted or specific clinical signs of distress e.g. accessory muscle use) ? Presence or absence of severe Pallor noted ? Presence or absence of fever with illness noted ? Presence or absence of urination noted ? Shock absence or presence noted ? Cold hands, Delayed capillary refill, Rapid pulse, altered mentation Laboratory Examinations If Respiratory Distress Chest X-ray and HCT (as indicated by clinical If severe pallorHCT or HGB status) If Coma/Convulsions/Shock Glucose, malaria (microscopic) and Lumbar Puncture If Dehydration with lethargy or altered consciousnessGlucose
1 Presumptive admission Initial admission diagnosis recorded and appropriate treatment initiated for diagnosis recorded & admission diagnosis (e.g. artesunate for malaria) treatment initiated Stabilization Measures in Children with Serious Urgency Signs (in addition to treatment for initial presumptive diagnosis—e.g. malaria) Oxygen : infants < 1 an : 0,5 L/min; infants > =1 year 1 L/min (unless Respiratory Distress normal pulsoximetry > 95% recorded) If severe anemia (Hct < 15) : Transfuse 10-15 ml/Kg packed red blood cells
Shock Oxygen : infants < 1 an : 0,5 L/min; infants > =1 an 1 L/min Rehydratation : If normally nourished child : Ringer lactate or normal saline IV bolus 20ml/kg ; repeat x 2 if not improving. If malnourished child : IV Ringer lactate or normal saline 15 ml/Kg over 1 heure. If no improvement, repeat x 1 over 2nd hour. If no improvement presumptive treatment for septic shock (ampicillin + gentamycin) Coma Secure airway if trauma Correct hypoglycemia if present : If <2,5 mmol/l (0,45 g/l) in normally nourished child or <3 mmol/l (0,55 g/l) in a malnourished child, give D 50% glucose solution bolus (1-5ml/kg) If serum glucose not available, give 10% glucose bolus (5 cc/kg) Convulsions Stabilize/secure airway Administer diazepam 0.5 mg/kg per rectum (if diarrhea administer IV or IM, 0.3 mg/kg slow bolus IV) Correct hypoglycemia if present : If <2,5 mmol/l (0,45 g/l) in normally nourished child or <3 mmol/l (0,55 g/l) in a malnourished child, give 10% glucose solution bolus (5ml/kg) If serum glucose not known, give 10% glucose bolus (5 cc/kg) Severe Dehydration If NO severe malnutrition and unable to drink: Age < 1 year : Ringer Lactate 30ml/kg 1st hour 70ml/kg over 5 following hours Age > 1 year: 30ml/kg pendant les premières 30 minutes 70ml/kg dans les 2h1/2 qui suivent Once child able to drink : 5ml/kg ORS every hour IF severe malnutrition : NO IV fluids Oral rehydration or via NG tube : 5ml/kg ReSoMal or ORS (diluted by half) every 30 minutes, then 5 to 10 cc/kg once stabilizing Systematic sugar water or 10% gluose 5 ml/kg Initial Monitoring of child with urgency signs (1st 2 hours or until stabilizing)
2 Respiratory distress RR every 30 minutes Shock Pulse every 30 minutes Convulsions /Coma Glucose upon arrival and repeat until normalizing Severe Dehydration Pulse and RR every 30 minutes until stabilizing
3