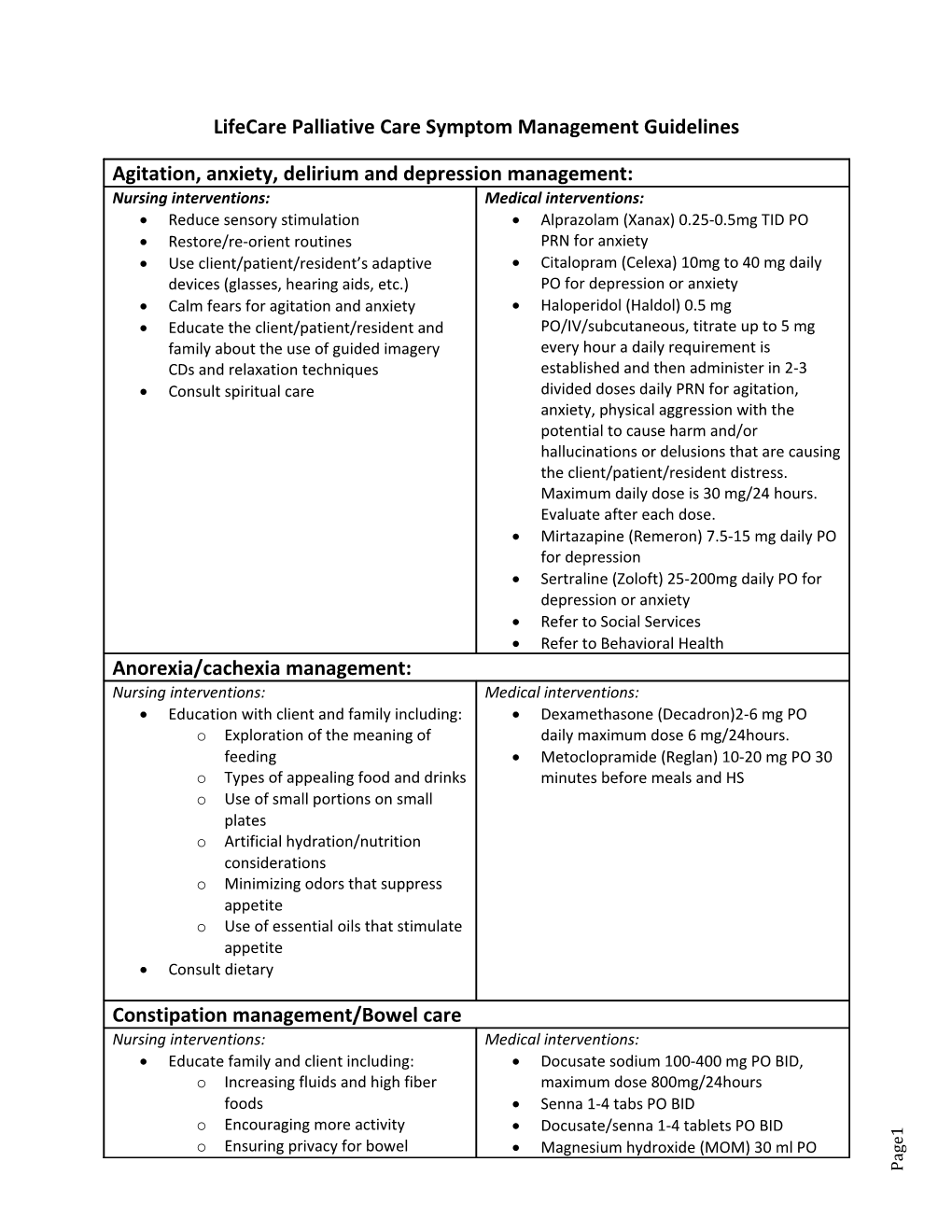
Nursing interventions: care management/Bowel Constipation Nursing interventions: management: Anorexia/cachexia Nursing interventions: management:depression and delirium anxiety, Agitation, Educate family and client including: Consult dietary Education client with and family including: Consult spiritual care CDs and relaxation techniques family about the of use guided imagery Educate the client/patient/resident and Calm fears foragitation and anxiety devices aids,(glasses, hearing etc.) Use client/patient/resident’s adaptive Restore/re-orient routines Reduce stimulation sensory o o o o o o o o o LifeCare Palliative Care Symptom Management Management GuidelinesCareSymptom Palliative LifeCare Ensuring privacy forbowel Encouraging moreactivity foods Increasing and fluids fiber high appetite Use of oilsessential that stimulate appetite Minimizing odors that suppress considerations Artificial hydration/nutrition plates Use of small portions small on Types of appealing food and drinks feeding Exploration of meaning the of Medical interventions: Medical interventions: Medical interventions: Maximum daily is 30dose hours. mg/24 the client/patient/resident distress. hallucinations or delusions that causingare potential cause to and/or harm anxiety, physical aggression with the divided doses PRN daily for agitation, established and then administer in 2-3 every hour a requirement daily is PO/IV/subcutaneous, titrate to up mg 5 Haloperidol (Haldol) 0.5 mg PO anxiety fordepression or Citalopram (Celexa) 10mg40 to daily mg PRN foranxiety Alprazolam (Xanax) 0.25-0.5mg TID PO Magnesium hydroxide (MOM) ml 30 PO Docusate/senna 1-4 tablets BIDPO Senna 1-4 tabs BIDPO maximum dose 800mg/24hours Docusate sodium PO 100-400 mg BID, minutes before meals HS and Metoclopramide (Reglan) mg 10-20 PO 30 daily 6maximum dose mg/24hours. Dexamethasone (Decadron)2-6 PO mg Refer to HealthBehavioral Refer to ServicesSocial depression or anxiety Sertraline (Zoloft)25-200mg daily for PO depressionfor Mirtazapine (Remeron) mg PO 7.5-15 daily Evaluate after dose. each
Page1 Nursing interventions ManagementFatigue Nursing interventions: management Dyspnea Nursing interventions: management Dryeyes/nose Diarrhea management Nursing interventions: Management Cough Educate client and family including: in treatment or therapy plan Pulse oximetery it if will result in a change with clients COPDwith may titrate for up usingcomfort, caution Oxygen 2 at liters nasalvia canulaPRN, Open a window Add a fan roomto clientfor Semi-fowlers positioningas comfortable Add humidification to room Add room humidifier Elevate bed head of 30° to prescribed. constipation/bowel ifcare opioids are Ensure orders havebeen obtained for o o activity Encourage mild exercise and prioritization of activities Promote adaptation and movements Medical interventions: Medical interventions: Medical interventions Medical interventions: Medical interventions: 2 2 after mg each a to loose BM maximum of Loperamide mg (Imodium) 4 initially then hours PRN Guaifenesin with ml codeine5 everyPO 2 PRN (Robitussin DM) ml PO 25 every hours Guaifenesin &dextromethorphan Benzonatate (tessalon) PO 200mg TID PRN daily mixed ozin liquid 8 of PRN Polyethylene Glycol17 (Miralax) grams PO daily PRN Prednisone 7.5-10mg PO daily PRN, evaluate after every dose Oxycodone 2.5-10 mg PO/SL every hour Morphine 0.5 mg IVevery 15 PRNminutes evaluate after dose each Morphine 2.5 mg PO/SLevery hour PRN, dyspneafor and rales Furosemide 5-40mg PO hour every PRN Alprazolam 0.25-0.5mg TIDPO PRN nebulizer everyhours 4 Albuterol/ipratropium (Duoneb) ml inby 3 hours Albuterol nebulizer2.5mg/3ml by every 4 Saline nasal in each spray nostril PRN lidlower BID PRN Eye lubricant (artificial tears) ¼ inch ½ to in Artificial 1-2gtts tears eye each PRN 16 hours mg/24
Page1 Nursing interventions: Oral Care Management Nursing interventions: Vomiting Nausea Management& Nursing interventions: Management Hiccup Nursing interventions: ManagementFever Educate family and client including: Educate client and family Minimal covers forehead Cool clothes to armpits groin, and Tepid sponge baths pharmacological interventions, such as: Educate family and client non-on o o o o o o o o o o o o o o daily daily needed as 15-30 Swish ml. and times spit4 Salt solution, tsp 1 in salt 1 H2O,c moist Lip balm needed as keepto lips spiced, soft foods nothing hot/cold, too mildly Food preparation: lukewarm, How to clean dentures toothette Use of softa toothbrush or Use of oilsessential such as ginger Incorporate techniquesrelaxation nausea Avoidance of smells that trigger Schedule restperiods gag reflex Tongue traction enough trigger to Swallow dry bread Swallow 2 teaspoons of sugar oropharynx Holding ice water in the Soft palate massage Medical interventions: Medical interventions: Candid treatment: Medical interventions: Medical interventions: acetaminophen every 650 4 mg hours PRN May alternate ibuprofen dose with PRN. to Not exceed hours3200mg/24 Ibuprofen everyhours400-800mg 4 PO hours. PO/Rectally PRN. Not exceedto gm/24 4 Acetaminophen 4 1000mg every hours PO/rectally PRN Acetaminophen everyhours 650mg 6 mg for PO then days, reevaluate7 Fluconazole 200 mg initially PO then 100 swallow QID 7 x thendays, reevaluate Nystatin (100 ml 000units/ml) 5 andswish swish swallowand 5 ml every hour and PRN, swish spitor mg/2ml, and 200/200/20 antacid mg/5ml) lidocaine disphenhydramine 2%, 12.5 Miracle wash (equalmouth viscous parts hours PO and PRN, swish spit Topical viscous lidocaine 2% ml every 5 4 Artificial every hour saliva PRN QID 30 before mealsminutes and at hs Metoclopramide (Reglan) mg 10-20 PO/IV Lorazepam 0.5 1.5PO– mg every hours 4 Haloperidol BID mg PRN 2 PO/SQ/IV rectally every 12 hours PRN Prochlorperazine 25 mg suppository given in divided doses, reevaluate days in 7 Dexamethasone 1-20mg daily, PO may be reduce dose forclients with renal Baclofen mg 5 every PO 8 hours PRN, hours PRN Chlorpromazine 25-50 PO mg every 6 dysfunction
Page1 Nursing interventions Management Pain pharmacological interventions including: Educate client and family non-of o o o o o relaxation techniques Social workreferral PRN teach to Massage Diversional techniques ginger Essential oils suchPam as Away, Guided imagery CDs Malignant Bone Pain:Malignant Bone Mild pain Medical interventions: Neuropathic pain: moderateOpioid to for severe medication pain every 4 hours PRN Oxycodone/APAP 5/500mg 1-2 tabs PO every 4 hours PRN Hydrocodone/APAP PO5/500mg 1-2 tabs to 400 mg/24exceed hours) dose in clients renal with not dysfunction; Tramadol 25-100 mg QID (reducePO PRN Naproxen 250 mg BID PO PRN PRN, not exceed to 3200gm/24 hours Ibuprofen PO400-800 mg every hours 4 PRN, not exceed to 4 /24hoursgm Acetaminophen every 650 4 mg hours PO PRN Acetaminophen 6 1000mg every hours PO hours apply for12 hours then remove for 12 Transdermal lidocaine patch patches),(1-3 dysfunction) days (decrease dose forclients with renal Pregabalin 50 PO mg TID, in evaluate 7 then TID 100mg mg daily PO HS, at titrate to up BID100mg Gabapentin ( for elderly population)100 up BID 300mg to , then TID 300mg Gabapentin 100 mg daily PO at titrateHS, (avoid in elderly use clients) Amitriptyline10-25 mg PO daily HS PRN Dexamethasone 3-12mg TID PO Naproxen 250 mg BID PO Ibuprofen PO 400-800mg QID Oxycodone SR 10 PO mg hours every 12 Oxycodone IR 5-10mg every hour PRN 12 hours Morphine SR Contin)15 (MS mg every PO Morphine 10 mg every PO hour PRN Morphine 0.5 mg IVevery 15 PRNminutes minutes PRN Hydromorphone mg IVevery0.1 15 1 hour PRN Hydromorphone 2(Dilaudid) PO mg every :
Page1 Nursing interventions: Management Skin Wound and Nursing intervention: ManagementSeizure Secretion Management dressing dressing change Administer pain PRN med hour ½ prior to Educate family and client including: appropriate pressurerelieving surfaces Evaluate chairs, wheelchairs, etc., for Heel protection available Use of pressure reducing mattress, where skin for itch Lavender oil mixed in carrier oil toapply absorb odor charcoal placed in dishunder bed to Kitty coffeelitter, grounds activated or room, on not ulcer Peppermint oil forodor, bed on linenor in needed for dryskin and discomfort of itch Over the lotioncounter moisturizing as warranted start safety protocol Do Braden a skin risk assessment, if Educate family o o o o o o o o o Wound cleansing and irrigation Techniques odor for control Nutrition and hydration Moisture control skin on Minimizing andfriction sheer Mobilization Causes and risks forpressureareas position. How to in place client recoverya client, especially fingers Not put to anything in mouth of Medical interventions: Medical interventions: Pressure ulcers and wounds: Pressure ulcers and malignant For Pruritus: odor:To control For wound pain: Medical interventions: may repeat one in 4 time hours PRN, Diazepam 0.2 mg/kg for rectally seizures, minutes a to maximum of mg 30 PRN Diazepam 5-10 IV/Buccal/IM mg every 15 maximum 8 mg/ 12 hours in 15 minute if intervals seizure continues, Lorazepam IV/SQPRN, 2-4mg may repeat 72 hours PRN May increase 3 to changed patches every behind ear, change hours every 72 PRN. Scopolamine 1.5transdermal mg patch every 2 hours PRN Atropine 1% ophthalmic solution 1-4gtts wound cleanser Cleanse wound with non-cytotoxic NS or PRN Triamcinolone 0.1% TID cream topically TID PRN Hydrocortisone 1% cream or lotion applied PRN Diphenhydramine 25 every 4 mg hours PO Paroxetine 10-20 mg dailyPO day and evaluate Doxepin 10-25 PO mg HS, daily use for 7 PRN Hydroxyzine 10-25 PO mg every hours 6 wound surface in daily, assess days7 Silver creamsulfadiazine 1% applied to Reassess sprinkled into 7wound x daily days. Metronidazole crushed500mg and reassess Metronidazole 500 mg TID PO days, 7 x to wound surfacecover daily Morphine 1 in mg gram 1 appliedhydrogel Hydromorphone every PO hour 2-4mg PRN every 5 days. maximum of one ofcourse treatment
Page1 Nursing interventions: RetentionManagement and/or Urinary Incontinence Nursing interventions: Management Sleep Disturbance/Insomnia Rectal Rectal exam rule to out impaction fecal Bladder scan PRN confirmto retention Educate client and family including: o o o o & Calm or lavender Use of oilsessential such as Peace caffeine Avoidance of stimulants such as Relaxation therapies Good sleep environment Medical interventions: Medical interventions: To bleeding: prevent For copious exudates: in stage 2-3 ulcers: moderate For of exudatesamounts low to Straight/indwelling catheter PRN bladderfor spasms Oxybutynin 2.5mgPO2-4 daily times PRN Zolpidem 5-10mg HS PO PRN repeat x dose 1 Trazodone 25-100 PO mg HS PRN, may repeat x dose 1 Temazepam 15 PO mg HS at mayPRN in 1-2 hours Alprazolam 0.25 0.5mgmayto repeat dose bleedingTo active manage o o o o o o o o removal Moisten with dressings before NS dressings Use non adherent absorbing drainage from fungating wounds Ostomy appliance contain to days wound borders, change every 2-4 wounds). Apply topically within Alginate (avoid in bleeding days Foam dressing, change every 3-5 every 2-5 days Hydrocolloid dressing; change Apply firm pressure woundto solution of epinephrine Apply gauze saturated with 1:1000 :
Page1