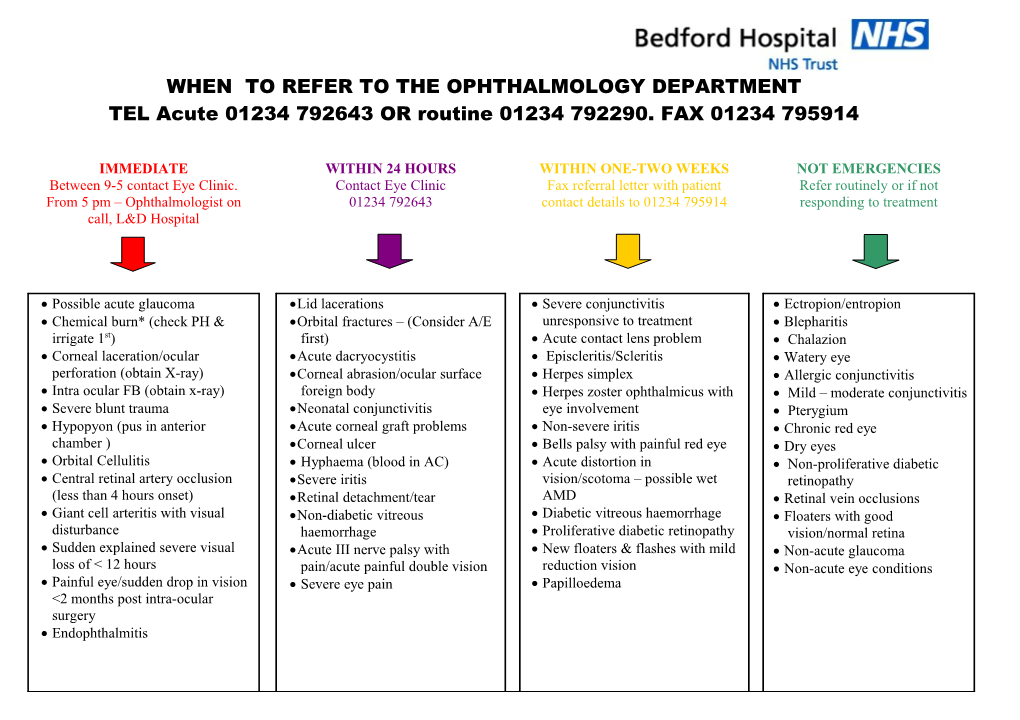
WHEN TO REFER TO THE OPHTHALMOLOGY DEPARTMENT TEL Acute 01234 792643 OR routine 01234 792290. FAX 01234 795914
IMMEDIATE WITHIN 24 HOURS WITHIN ONE-TWO WEEKS NOT EMERGENCIES Between 9-5 contact Eye Clinic. Contact Eye Clinic Fax referral letter with patient Refer routinely or if not From 5 pm – Ophthalmologist on 01234 792643 contact details to 01234 795914 responding to treatment call, L&D Hospital
Possible acute glaucoma Lid lacerations Severe conjunctivitis Ectropion/entropion Chemical burn* (check PH & Orbital fractures – (Consider A/E unresponsive to treatment Blepharitis irrigate 1st) first) Acute contact lens problem Chalazion Corneal laceration/ocular Acute dacryocystitis Episcleritis/Scleritis Watery eye perforation (obtain X-ray) Corneal abrasion/ocular surface Herpes simplex Allergic conjunctivitis Intra ocular FB (obtain x-ray) foreign body Herpes zoster ophthalmicus with Mild – moderate conjunctivitis Severe blunt trauma Neonatal conjunctivitis eye involvement Pterygium Hypopyon (pus in anterior Acute corneal graft problems Non-severe iritis Chronic red eye chamber ) Corneal ulcer Bells palsy with painful red eye Dry eyes Orbital Cellulitis Hyphaema (blood in AC) Acute distortion in Non-proliferative diabetic Central retinal artery occlusion Severe iritis vision/scotoma – possible wet retinopathy (less than 4 hours onset) Retinal detachment/tear AMD Retinal vein occlusions Giant cell arteritis with visual Non-diabetic vitreous Diabetic vitreous haemorrhage Floaters with good disturbance haemorrhage Proliferative diabetic retinopathy vision/normal retina Sudden explained severe visual Acute III nerve palsy with New floaters & flashes with mild Non-acute glaucoma loss of < 12 hours pain/acute painful double vision reduction vision Non-acute eye conditions Painful eye/sudden drop in vision Severe eye pain Papilloedema <2 months post intra-ocular surgery Endophthalmitis