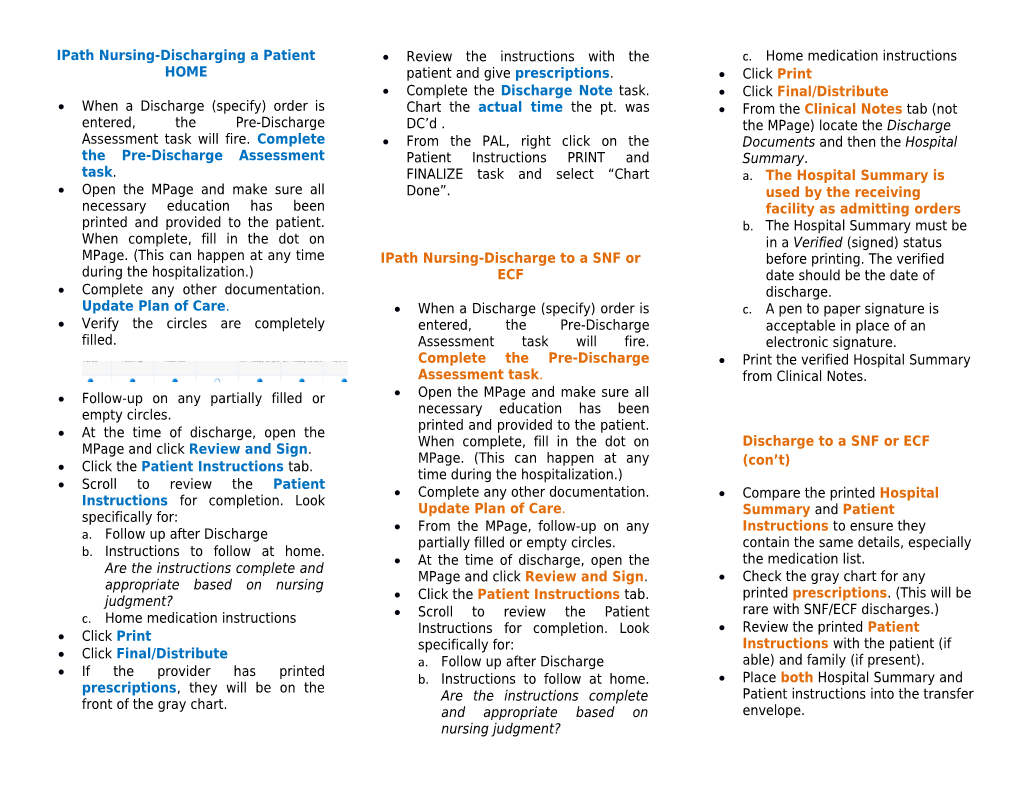
IPath Nursing-Discharging a Patient Review the instructions with the c. Home medication instructions HOME patient and give prescriptions. Click Print Complete the Discharge Note task. Click Final/Distribute When a Discharge (specify) order is Chart the actual time the pt. was From the Clinical Notes tab (not entered, the Pre-Discharge DC’d . the MPage) locate the Discharge Assessment task will fire. Complete From the PAL, right click on the Documents and then the Hospital the Pre-Discharge Assessment Patient Instructions PRINT and Summary. task. FINALIZE task and select “Chart a. The Hospital Summary is Open the MPage and make sure all Done”. used by the receiving necessary education has been facility as admitting orders printed and provided to the patient. b. The Hospital Summary must be When complete, fill in the dot on in a Verified (signed) status MPage. (This can happen at any time IPath Nursing-Discharge to a SNF or before printing. The verified during the hospitalization.) ECF date should be the date of Complete any other documentation. discharge. Update Plan of Care. When a Discharge (specify) order is c. A pen to paper signature is Verify the circles are completely entered, the Pre-Discharge acceptable in place of an filled. Assessment task will fire. electronic signature. Complete the Pre-Discharge Print the verified Hospital Summary Assessment task. from Clinical Notes. Follow-up on any partially filled or Open the MPage and make sure all empty circles. necessary education has been printed and provided to the patient. At the time of discharge, open the When complete, fill in the dot on Discharge to a SNF or ECF MPage and click Review and Sign. MPage. (This can happen at any Click the Patient Instructions tab. (con’t) time during the hospitalization.) Scroll to review the Patient Complete any other documentation. Compare the printed Hospital Instructions for completion. Look Update Plan of Care. Summary and Patient specifically for: From the MPage, follow-up on any Instructions to ensure they a. Follow up after Discharge partially filled or empty circles. contain the same details, especially b. Instructions to follow at home. At the time of discharge, open the the medication list. Are the instructions complete and MPage and click Review and Sign. Check the gray chart for any appropriate based on nursing printed prescriptions. (This will be judgment? Click the Patient Instructions tab. rare with SNF/ECF discharges.) c. Home medication instructions Scroll to review the Patient Instructions for completion. Look Review the printed Patient Click Print specifically for: Instructions with the patient (if Click Final/Distribute a. Follow up after Discharge able) and family (if present). If the provider has printed b. Instructions to follow at home. Place both Hospital Summary and prescriptions, they will be on the Are the instructions complete Patient instructions into the transfer front of the gray chart. and appropriate based on envelope. nursing judgment? Use the appropriate checklist (MMC and provided to the patient. When Form 1917- ECF) to ensure all items complete, fill in the dot on MPage. (This are completed. can happen at any time during the Phone report to the receiving hospitalization.) facility. Complete any other documentation. Complete the Discharge Note Update Plan of Care. task. Chart the actual time the pt. On the MPage, verify the circles are is leaving completely filled. From the PAL, right click on the Patient Instructions PRINT and FINALIZE task and select “Chart Follow-up on any partially filled or Done”. empty circles. The Patient Instructions do NOT have to be finalized (signed) or printed for these patients. Using the appropriate checklist (Form 2160), ensure all pertinent documentation is collected and sent with the patient. Phone report to the receiving facility. The provider can dictate a Hospital Course using dictation service. This document can be printed from Clinical Notes to accompany the patient, if available. Complete the Discharge Note at the actual time the pt. is leaving o It is important to document the correct facility that the patient is discharge to because this determines where Transfer IPATH Nursing-Transfer to Acute Care of Care documentation is Facility distributed. o Documentation that is When a Discharge (specify) order is erroneous (ie. Wrong DC time or entered, the Pre-Discharge Assessment facility) must be corrected as task will fire. Complete the Pre- soon as the error is discovered. Discharge Assessment task. From the PAL, right click on the Patient Open the MPage and make sure all Instructions PRINT and FINALIZE task necessary education has been printed and select “Chart Done”. October 20, 2014
Discharge Process Pocket Guide for Nursing
Discharge to home
Discharge to SNF or ECF
Transfer to Acute Care Facility