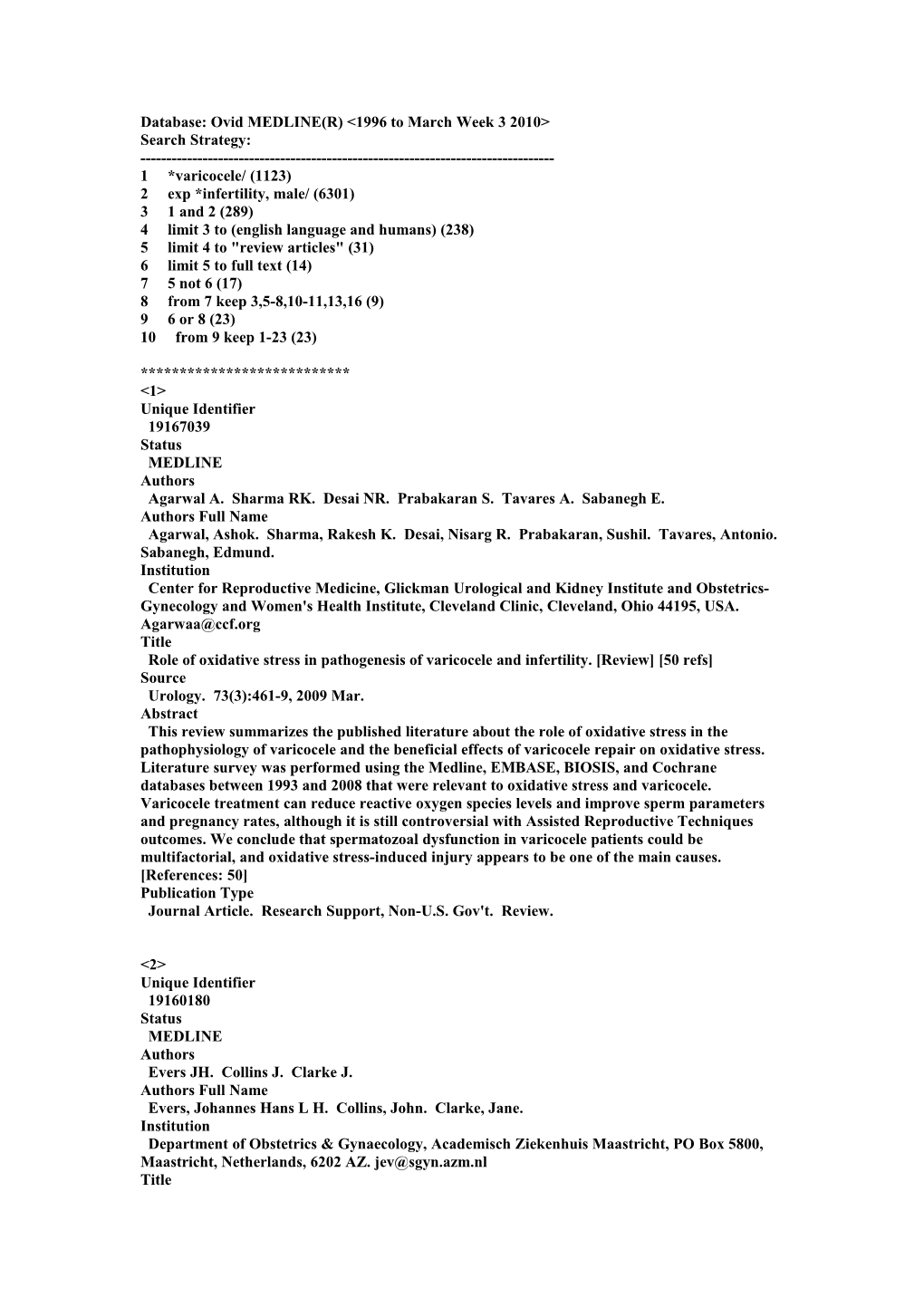
Database: Ovid MEDLINE(R) <1996 to March Week 3 2010> Search Strategy: ------1 *varicocele/ (1123) 2 exp *infertility, male/ (6301) 3 1 and 2 (289) 4 limit 3 to (english language and humans) (238) 5 limit 4 to "review articles" (31) 6 limit 5 to full text (14) 7 5 not 6 (17) 8 from 7 keep 3,5-8,10-11,13,16 (9) 9 6 or 8 (23) 10 from 9 keep 1-23 (23)
*************************** <1> Unique Identifier 19167039 Status MEDLINE Authors Agarwal A. Sharma RK. Desai NR. Prabakaran S. Tavares A. Sabanegh E. Authors Full Name Agarwal, Ashok. Sharma, Rakesh K. Desai, Nisarg R. Prabakaran, Sushil. Tavares, Antonio. Sabanegh, Edmund. Institution Center for Reproductive Medicine, Glickman Urological and Kidney Institute and Obstetrics- Gynecology and Women's Health Institute, Cleveland Clinic, Cleveland, Ohio 44195, USA. [email protected] Title Role of oxidative stress in pathogenesis of varicocele and infertility. [Review] [50 refs] Source Urology. 73(3):461-9, 2009 Mar. Abstract This review summarizes the published literature about the role of oxidative stress in the pathophysiology of varicocele and the beneficial effects of varicocele repair on oxidative stress. Literature survey was performed using the Medline, EMBASE, BIOSIS, and Cochrane databases between 1993 and 2008 that were relevant to oxidative stress and varicocele. Varicocele treatment can reduce reactive oxygen species levels and improve sperm parameters and pregnancy rates, although it is still controversial with Assisted Reproductive Techniques outcomes. We conclude that spermatozoal dysfunction in varicocele patients could be multifactorial, and oxidative stress-induced injury appears to be one of the main causes. [References: 50] Publication Type Journal Article. Research Support, Non-U.S. Gov't. Review.
<2> Unique Identifier 19160180 Status MEDLINE Authors Evers JH. Collins J. Clarke J. Authors Full Name Evers, Johannes Hans L H. Collins, John. Clarke, Jane. Institution Department of Obstetrics & Gynaecology, Academisch Ziekenhuis Maastricht, PO Box 5800, Maastricht, Netherlands, 6202 AZ. [email protected] Title Surgery or embolisation for varicoceles in subfertile men. [Review] [38 refs][Update of Cochrane Database Syst Rev. 2008;(3):CD000479; PMID: 18646066] Source Cochrane Database of Systematic Reviews. (1):CD000479, 2009. Abstract BACKGROUND: A varicoceles is a meshwork of distended blood vessels in the scrotum, usually left-sided, due to dilatation of the spermatic vein. Although the concept that varicoceles causes, and varicocelectomy cures, male subfertility has been around for almost fifty years, the mechanisms by which varicoceles would affect fertility have not yet been satisfactorily explained, and neither have the mechanisms by which varicocelectomy would restore fertility. Furthermore, it has been questioned whether a causal relation exists at all between the distension of the pampiniform plexus and impairment of fertility. OBJECTIVES: To evaluate the effect of varicoceles treatment on pregnancy rate in subfertile couples. SEARCH STRATEGY: We searched the Cochrane Menstrual Disorders and Subfertility Group Trials Register (12 Sept 2003 and October 2007), the Cochrane Central Register of Controlled Trials (The Cochrane Library Issue 1, 2004 and Issue 4, 2007), MEDLINE (January 1966 to October 2007), EMBASE (January 1985 to October 2007) and reference lists of articles. In addition, we handsearched specialist journals in the field from their first issue until 2007. We also checked cross-references, references from review articles and contacted researchers in the field. SELECTION CRITERIA: Randomised controlled trials (RCTs) were included if they were relevant to the clinical question posed, if they reported pregnancy rates as an outcome measure, and if they reported data in treated (surgical ligation or radiological embolisation of the internal spermatic vein) and untreated groups. DATA COLLECTION AND ANALYSIS: Nine studies met the inclusion criteria for the original review. One was an extension of a previously published study, which left eight studies for analysis. All eight only included men from couples with subfertility problems; one excluded men with sperm counts less than 5 million per mL and one men with sperm counts less than 2 million per mL, with or without progressive motility of less than 10%. Two trials involving clinical varicoceles included some men with normal semen analysis. Three studies specifically addressed only men with subclinical varicoceles. Two authors independently screened potentially relevant trials. Any differences of opinion were resolved by consensus (none occurred for this review). Studies were excluded from meta-analysis if they made comparisons other than those specified above. MAIN RESULTS: The combined Peto odds ratio (OR) of the eight studies is 1.10 (95%CI 0.73 to 1.68), indicating no benefit of varicoceles treatment over expectant management in subfertile couples in whom varicoceles in the man is the only abnormal finding. AUTHORS' CONCLUSIONS: There is no evidence that treatment of varicoceles in men from couples with otherwise unexplained subfertility improves the couple's chance of conception. [References: 38] Publication Type Journal Article. Meta-Analysis. Review.
<3> Unique Identifier 18772487 Status MEDLINE Authors Cayan S. Shavakhabov S. Kadioglu A. Authors Full Name Cayan, Selahittin. Shavakhabov, Shavkat. Kadioglu, Ates. Institution University of Mersin School of Medicine, Department of Urology, 33079-Mersin, Turkey. [email protected] Title Treatment of palpable varicocele in infertile men: a meta-analysis to define the best technique. [Review] [59 refs] Source Journal of Andrology. 30(1):33-40, 2009 Jan-Feb. Abstract To date, there have been no randomized, controlled, prospective clinical studies that compare various techniques to describe the best method for the treatment of varicocele in infertile men. This meta-analysis aims to address the best treatment modality for palpable varicocele in infertile men. A MEDLINE search was performed for articles published between January 1980 and April 2008, and we analyzed 36 studies reporting postoperative spontaneous pregnancy rates and/or complication rates after varicocele repair using various techniques in infertile men with palpable unilateral or bilateral varicocele. Spontaneous pregnancy rates and postoperative complications such as hydrocele formation, recurrence, or persistence were compared among the techniques. In addition, interventional failure with radiologic embolization and reported complications with the laparoscopic approach were reviewed. Overall spontaneous pregnancy rates were 37.69% in the Palomo technique series, 41.97% in the microsurgical varicocelectomy techniques, 30.07% in the laparoscopic varicocelectomy techniques, 33.2% in the radiologic embolization, and 36% in the macroscopic inguinal (Ivanissevich) varicocelectomy series, revealing significant differences among the techniques (P = .001). Overall recurrence rates were 14.97% in the Palomo technique series, 1.05% in the microsurgical varicocelectomy techniques, 4.3% in the laparoscopic varicocelectomy techniques, 12.7% in the radiologic embolization, and 2.63% in the macroscopic inguinal (Ivanissevich) or subinguinal varicocelectomy series, revealing significant difference among the techniques (P = .001). Overall hydrocele formation rates were 8.24% in the Palomo technique series, 0.44% in the microsurgical varicocelectomy techniques, 2.84% in the laparoscopic varicocelectomy, and 7.3% in the macroscopic inguinal (Ivanissevich) or subinguinal varicocelectomy series, revealing significant difference among the techniques (P = .001). We conclude that the microsurgical varicocelectomy technique has higher spontaneous pregnancy rates and lower postoperative recurrence and hydrocele formation than conventional varicocelectomy techniques in infertile men. However, prospective, randomized, and comparative studies with large number of patients are needed to compare the efficacy of microsurgical varicocelectomy with that of other treatment modalities in infertile men with varicocele. [References: 59] Publication Type Journal Article. Meta-Analysis. Review.
<4> Unique Identifier 19007639 Status MEDLINE Authors Practice Committee of American Society for Reproductive Medicine. Authors Full Name Practice Committee of American Society for Reproductive Medicine. Title Report on varicocele and infertility. [Review] [18 refs] Source Fertility & Sterility. 90(5 Suppl):S247-9, 2008 Nov. Abstract Controversies regarding diagnosis and treatment of varicoceles in male partners in infertile couples are considered in detail. [References: 18] Publication Type Journal Article. Review.
<5> Unique Identifier 18646066 Status MEDLINE Authors Evers JH. Collins J. Clarke J. Authors Full Name Evers, Johannes Hans L H. Collins, John. Clarke, Jane. Institution Department of Obstetrics & Gynaecology, Academisch Ziekenhuis Maastricht, PO Box 5800, Maastricht, Netherlands, 6202 AZ. [email protected] Title Surgery or embolisation for varicoceles in subfertile men. [Review] [38 refs][Update in Cochrane Database Syst Rev. 2009;(1):CD000479; PMID: 19160180].[Update of Cochrane Database Syst Rev. 2004;(3):CD000479; PMID: 15266431] Source Cochrane Database of Systematic Reviews. (3):CD000479, 2008. Abstract BACKGROUND: A varicoceles is a meshwork of distended blood vessels in the scrotum, usually left-sided, due to dilatation of the spermatic vein. Although the concept that varicoceles causes, and varicocelectomy cures, male subfertility has been around for almost fifty years, the mechanisms by which varicoceles would affect fertility have not yet been satisfactorily explained, and neither have the mechanisms by which varicocelectomy would restore fertility. Furthermore, it has been questioned whether a causal relation exists at all between the distension of the pampiniform plexus and impairment of fertility. OBJECTIVES: To evaluate the effect of varicoceles treatment on pregnancy rate in subfertile couples. SEARCH STRATEGY: We searched the Cochrane Menstrual Disorders and Subfertility Group Trials Register (12 Sept 2003 and October 2007), the Cochrane Central Register of Controlled Trials (The Cochrane Library Issue 1, 2004 and Issue 4, 2007), MEDLINE (January 1966 to October 2007), EMBASE (January 1985 to October 2007) and reference lists of articles. In addition, we handsearched specialist journals in the field from their first issue until 2007. We also checked cross-references, references from review articles and contacted researchers in the field. SELECTION CRITERIA: Randomised controlled trials (RCTs) were included if they were relevant to the clinical question posed, if they reported pregnancy rates as an outcome measure, and if they reported data in treated (surgical ligation or radiological embolisation of the internal spermatic vein) and untreated groups. DATA COLLECTION AND ANALYSIS: Nine studies met the inclusion criteria for the original review. One was an extension of a previously published study, which left eight studies for analysis. All eight only included men from couples with subfertility problems; one excluded men with sperm counts less than 5 million per mL and one men with sperm counts less than 2 million per mL, with or without progressive motility of less than 10%. Two trials involving clinical varicoceles included some men with normal semen analysis. Three studies specifically addressed only men with subclinical varicoceles. Two authors independently screened potentially relevant trials. Any differences of opinion were resolved by consensus (none occurred for this review). Studies were excluded from meta-analysis if they made comparisons other than those specified above. MAIN RESULTS: The combined Peto odds ratio (OR) of the eight studies is 1.10 (95%CI 0.73 to 1.68), indicating no benefit of varicoceles treatment over expectant management in subfertile couples in whom varicoceles in the man is the only abnormal finding. AUTHORS' CONCLUSIONS: There is no evidence that treatment of varicoceles in men from couples with otherwise unexplained subfertility improves the couple's chance of conception. [References: 38] Publication Type Comparative Study. Journal Article. Meta-Analysis. Review.
<6> Unique Identifier 18460942 Status MEDLINE Authors French DB. Desai NR. Agarwal A. Authors Full Name French, Dan B. Desai, Nisarg R. Agarwal, Ashok. Institution Reproductive Research Center, Glickman Urological and Kidney Institute, Cleveland Clinic, Cleveland, Ohio 44195, USA. Title Varicocele repair: does it still have a role in infertility treatment?. [Review] [50 refs] Source Current Opinion in Obstetrics & Gynecology. 20(3):269-74, 2008 Jun. Abstract PURPOSE OF REVIEW: To review the role of varicocele repair in the treatment of male infertility. RECENT FINDINGS: Varicocele is a common finding among men with infertility and its repair has been a mainstay of surgical therapy in these men. Although each year multiple discoveries are made concerning the mechanism of varicocele-induced infertility, the exact pathophysiologic mechanism remains unknown. This study will update significant findings in regard to the pathophysiology of varicocele-induced infertility, such as increased expression of the aquaporin receptor and new findings related to testicular blood flow and vas deferens motility. Recent information concerning the effects of apoptosis and oxidative stress are also reviewed. With regard to the efficacy of varicocele repair, previous meta-analysis of the available data has been misleading due to improper selection criteria. Available clinical data are critically evaluated, with a focus on new meta-analyses that contradict the findings of the Cochrane database review, a study that has been accepted by many as evidence against varicocele repair. SUMMARY: We conclude that varicocele repair not only is an effective treatment for appropriately selected patients but can also be the most cost effective option. [References: 50] Publication Type Journal Article. Research Support, Non-U.S. Gov't. Review.
<7> Unique Identifier 18423240 Status MEDLINE Authors Richardson I. Grotas AB. Nagler HM. Authors Full Name Richardson, Ingride. Grotas, Aaron B. Nagler, Harris M. Institution Sol and Margaret Berger Department of Urology, Beth Israel Medical Center, 10 Union Square East, Suite 3A, New York, NY 10003, USA. Title Outcomes of varicocelectomy treatment: an updated critical analysis. [Review] [76 refs] Source Urologic Clinics of North America. 35(2):191-209, viii, 2008 May. Abstract This article provides an updated analysis of the varicocele literature published since 1994. The present authors have followed the format of the previous review and have included a summary of the results from the 1994 article at the end of each section. [References: 76] Publication Type Journal Article. Review.
<8> Unique Identifier 17822454 Status MEDLINE Authors Cayan S. Woodhouse CR. Authors Full Name Cayan, Settin. Woodhouse, Christopher R J. Institution Department of Urology, University of Mersin School of Medicine, Mersin, Turkey. Title The treatment of adolescents presenting with a varicocele. [Review] [34 refs] Source BJU International. 100(4):744-7, 2007 Oct. Abstract In the last 10 years there have been many reports of children and adolescents with varicocele, but virtually none from the UK. There is an increasing incidence with age, to 19% by the age of 19 years. There is some evidence that a varicocele impairs the development of the affected testis; 9.3% of boys of 19 years old have a small testis as a result. Some aspects of testicular function are compromised. Treatment of the varicocele allows compensatory growth and testicular function. The surgical technique must be meticulous to avoid complications, particularly the formation of a hydrocele. Despite much research, the effect on fertility is unknown. The incidence of varicocele is much higher than that of male factor infertility. It is not known whether varicocele in adolescence impairs fertility or whether surgery restores fertility. At present the main indications for surgery are persistent delay in growth of >20%, bilateral varicocele and impaired spermatogenesis persisting beyond 18 years old. [References: 34] Publication Type Journal Article. Review.
<9> Unique Identifier 17055852 Status MEDLINE Authors Practice Committee of the American Society for Reproductive Medicine. Authors Full Name Practice Committee of the American Society for Reproductive Medicine. Title Report on varicocele and infertility. [Review] [18 refs] Source Fertility & Sterility. 86(5 Suppl 1):S93-5, 2006 Nov. Publication Type Journal Article. Practice Guideline. Review.
<10> Unique Identifier 16426727 Status MEDLINE Authors Ficarra V. Cerruto MA. Liguori G. Mazzoni G. Minucci S. Tracia A. Gentile V. Authors Full Name Ficarra, Vincenzo. Cerruto, Maria Angela. Liguori, Giovanni. Mazzoni, Guglielmo. Minucci, Sergio. Tracia, Angelo. Gentile, Vincenzo. Institution Italian Varicocele Study Group of the Italian Society of Andrology (SIA), Italy. [email protected] Title Treatment of varicocele in subfertile men: The Cochrane Review--a contrary opinion. [Review] [23 refs] Comments Comment in: Eur Urol. 2006 Feb;49(2):217-9; PMID: 16413658] Source European Urology. 49(2):258-63, 2006 Feb. Abstract OBJECTIVE: A recent Cochrane meta-analysis of randomised clinical trials (RCTs) concluded that surgical or radiological treatment of varicocele in men from couples with otherwise unexplained subfertility cannot be recommended. The aim of the present study is to address criticisms of this review carrying out a critical analysis of all available RCTs. MATERIALS AND METHODS: The eight randomised clinical trials selected in the last Cochrane Library systematic review have been evaluated. All RCTs including patients either with normal semen analysis or subclinical varicocele have been excluded. Inclusion criteria, number and clinical characteristics of randomised patients, and outcomes reported in terms of pregnancy rate one year after randomisation have been described in the remaining studies. RESULTS: Only 3/8 RCTs included patients with abnormal semen analysis and palpable varicocele. Overall 120 patients in the treatment group and 117 in the control group were randomised. The studies turned out to be heterogeneous in terms of inclusion criteria and clinical characteristics of the analysed patients. Their methodological quality and statistical power have to be considered poor. Moreover, the "as treated" cumulative analysis showed a significant increase in pregnancy rate in patients who underwent varicocele treatment (36.4%) compared with the control group (20%) (p = 0.009). CONCLUSIONS: The RCTs included in the last Cochrane review concerning the efficacy of varicocele treatment in subfertile couples were heterogeneous and methodologically poor. The pooling of these studies cannot result in a good quality meta-analysis. The Cochrane meta-analysis conclusions should not support guidelines recommendation against varicocele treatment in subfertile patients. Data from ongoing studies should provide more information in this topic. [References: 23] Publication Type Journal Article. Review.
<11> Unique Identifier 15363711 Status MEDLINE Authors Male Infertility Best Practice Policy Committee of the American Urological Association. Practice Committee of the American Society for Reproductive Medicine. Authors Full Name Male Infertility Best Practice Policy Committee of the American Urological Association. Practice Committee of the American Society for Reproductive Medicine. Institution American Urological Association, Baltimore, Maryland, USA. Title Report on varicocele and infertility. [Review] [15 refs] Source Fertility & Sterility. 82 Suppl 1:S142-5, 2004 Sep. Publication Type Guideline. Journal Article. Practice Guideline. Review.
<12> Unique Identifier 14972491 Status MEDLINE Authors Nabi G. Asterlings S. Greene DR. Marsh RL. Authors Full Name Nabi, G. Asterlings, S. Greene, D R. Marsh, R L. Institution Academic Unit of Urology, Department of Surgery, University of Aberdeen, Foresterhill, Scotland, United Kingdom. Title Percutaneous embolization of varicoceles: outcomes and correlation of semen improvement with pregnancy. [Review] [26 refs] Source Urology. 63(2):359-63, 2004 Feb. Abstract OBJECTIVES: To assess the technical feasibility and compare the semen quality in men with or without pregnancy after percutaneous embolization of varicoceles in the management of infertility. METHODS: The records of 102 patients who underwent retrograde varicocele embolization between January 1997 and January 2002 were reviewed through the Hospital Information Support System. Infertility was the indication for embolization in 71 cases. The present study consisted of this group of patients. The size of the varicoceles, the size of the testis, the pre-embolization semen analysis parameters, the technical details of embolization procedure, any anomalous vessels seen on venography, and, if unsuccessful, the reason for failure of the procedure were noted. A record of postembolization semen parameters (at least two) was made. Patients were divided into four groups depending on the pre-embolization semen density, and a correlation of this was assessed with improvements in morphology and motility. Follow-up was performed using a questionnaire to evaluate the success rate of the procedure, complications, and any treatment for infertility by the patient or his partner after the procedure. Patients who had a successful pregnancy were compared with those who did not to determine the correlation between the changes in semen quality and pregnancy rate. RESULTS: Between January 1997 and January 2002, 71 patients underwent retrograde varicocele embolization, using an embolizing coil, for infertility. In 68 (95.7%), it was technically successful. Nineteen patients (26.7%) had various anomalous vessels on venography. A statistically significant improvement (P = 0.002) was noted in the motility parameters in patients with a pre-embolization semen density between 10 and 30 million/mL. All patients were followed up by questionnaire. Follow-up was possible in 51 patients (75%). One patient had varicocele recurrence and underwent open inguinal surgical ligation. Of 45 patients, the partners of 18 (40%) had a successful pregnancy. A comparison of the postembolization semen quality between those with and without a successful pregnancy found no correlation between the changes in the semen parameters and the pregnancy rate. CONCLUSIONS: Varicocele embolization is a technically feasible, minimally invasive, outpatient procedure that improves semen quality significantly in patients with a pre- embolization semen density of 10 to 30 million/mL. However, no correlation was found between the improvements in semen quality and the pregnancy rate. [References: 26] Publication Type Comparative Study. Evaluation Studies. Journal Article. Review.
<13> Unique Identifier 12788571 Status MEDLINE Authors Evers JL. Collins JA. Authors Full Name Evers, Johannes L H. Collins, John A. Institution Department of Obstetrics and Gynaecology, GROW Research Institute, Academisch Ziekenhuis Maastricht, University of Maastricht, Maastricht, Netherlands. [email protected]
<14> Unique Identifier 11866240 Status MEDLINE Authors Redmon JB. Carey P. Pryor JL. Authors Full Name Redmon, J Bruce. Carey, Patrick. Pryor, Jon L. Institution Department of Urologic Surgery, Minneapolis, MN 55455, USA. Title Varicocele--the most common cause of male factor infertility?. [Review] [38 refs] Source Human Reproduction Update. 8(1):53-8, 2002 Jan-Feb. Abstract Varicocele is often cited as the most common cause of male factor infertility. Arguments in support of this statement include reports of increased prevalence of varicocele in populations of infertile men compared with fertile or otherwise unselected men, association of varicocele with abnormal semen parameters, and improvements in semen parameters and/or pregnancy rates after varicocele repair. Logically, there would appear to be three possibilities regarding the relationship between varicocele and fertility: (i) varicocele has no association with or effect on male fertility; (ii) varicocele may be associated with, but is not the cause of, male subfertility; and (iii) varicocele is a direct cause of male subfertility. In the following, we review evidence from the literature for and against these three possibilities: at the current time, available evidence appears inadequate to confirm or deny any of these three possibilities. Since the ultimate goal of infertile couples is to conceive, it seem logical that future varicocele research should focus primarily on adequately powered, controlled clinical trials in well-characterized infertile couples, randomized to intervention or appropriate controlled observation, with pregnancy as the primary outcome. [References: 38] Publication Type Journal Article. Review.
<15> Unique Identifier 12084227 Status MEDLINE Authors Schoor RA. Elhanbly SM. Niederberger C. Authors Full Name Schoor, R A. Elhanbly, S M. Niederberger, C. Institution Department of Urology/Andrology, Division of Andrology, University of Illinois at Chicago, 840 South Wood Street, M/C 955, Chicago, IL 60612-7316, USA. [email protected] Title The pathophysiology of varicocele-associated male infertility. [Review] [48 refs] Source Current Urology Reports. 2(6):432-6, 2001 Dec. Abstract Varicocele is the most commonly identifiable, surgically correctable lesion associated with male- factor infertility. Surgical correction of a varicocele, whether unilateral or bilateral, results in improvement not only in semen parameters but also in spontaneous and assisted pregnancy rates. Varicoceles seem to induce a number of changes in the testicular microenvironment. These alterations in temperature, hemodynamics, and reactive oxidative species and antioxidant concentrations have been demonstrated to produce deleterious effects on spermatogenesis. However, despite current knowledge in the pathophysiology of varicocele-associated male infertility, the exact mechanism--or mechanisms--by which varicoceles impair fertility remains elusive. This review examines scientific evidence regarding the pathophysiology of varicocele- associated male infertility. [References: 48] Publication Type Journal Article. Review.
<16> Unique Identifier 11556494 Status MEDLINE Authors Naughton CK. Nangia AK. Agarwal A. Authors Full Name Naughton, C K. Nangia, A K. Agarwal, A. Institution Center for Advanced Research in Human Reproduction and Infertility, Department of Urology, The Cleveland Clinic Foundation, Ohio 44195, USA. Title Pathophysiology of varicoceles in male infertility. [Review] [124 refs] Source Human Reproduction Update. 7(5):473-81, 2001 Sep-Oct. Abstract Varicoceles are found in 19 to 41% of infertile men, and is one treatable form of male infertility. The mechanism by which varicoceles cause the variable effect on male infertility and spermatogenesis is still unknown. Experimental animal models play a useful (but limited) role due to the sudden and variable iatrogenic nature of the varicoceles and the duration of the studies. Much of the human data are derived by the characterization of associated differences in measurable parameters between men with and without varicoceles. The role of hyperthermia, testicular blood flow and venous pressure changes, reflux of renal/adrenal products, hormonal dysfunction, autoimmunity, defects in acrosome reaction, and oxidative stress, in the pathophysiology of varicocele will be discussed. [References: 124] Publication Type Journal Article. Review.
<17> Unique Identifier 11212078 Status MEDLINE Authors Silber SJ. Authors Full Name Silber, S J. Institution Infertility Center of St Louis, St Luke's Hospital, MO 63017, USA. Title The varicocele dilemma. [Review] [53 refs] Source Human Reproduction Update. 7(1):70-7, 2001 Jan-Feb. Abstract There is probably no subject that is more controversial in the area of male infertility than varicocele. The overwhelming majority of non-urologist infertility specialists in the world are extremely sceptical of the role of varicocele or varicocelectomy in the treatment of male infertility. Directors of most assisted reproductive technologies (ART) programmes view the enthusiasm with which urologists approach varicocelectomy as a potential impediment to the couple that is getting older and do not have much time left to become pregnant using ART. There are many credible, well-controlled studies which show no effect of varicocelectomy on fertility. There are also a few 'controlled' studies that favour varicocelectomy, but all can be criticised on the basis of patient selection bias. Thus the great weight of evidence from controlled studies is against varicocelectomy and the reports supporting varicocelectomy are extremely weak. Finally, the reports that semen parameters are improved by varicocelectomy is flawed by uncontrolled observations and the failure to take into account the variability of semen analysis in infertile men and its regression toward the mean. Many control studies have demonstrated that, because of this variability, men with an initially low sperm count tend later to have higher sperm counts in the absence of any treatment whatsoever. [References: 53] Publication Type Journal Article. Review.
<18> Unique Identifier 11212076 Status MEDLINE Authors Jarow JP. Authors Full Name Jarow, J P. Institution Department of Urology, Johns Hopkins University School of Medicine, Baltimore, MD 21287, USA. [email protected] Title Effects of varicocele on male fertility. [Review] [86 refs] Source Human Reproduction Update. 7(1):59-64, 2001 Jan-Feb. Abstract Varicoceles are vascular lesions of the pampiniform plexus and are the most common identifiable abnormality found in men being evaluated for infertility. Despite the long history associated with varicoceles, there remains much controversy regarding their diagnosis and management. The purpose of this manuscript is to address three of the most pressing controversies: (i) the association of varicoceles with male infertility, (ii) whether varicoceles exert a progressive deleterious effect and (iii) the relationship of varicocele size and outcome following varicocele repair. The current literature is reviewed in an effort to answer these questions. Based upon this analysis, conclusions can be drawn regarding the best management of varicoceles in subfertile men, adolescents, young fertile men and men with subclinical varicoceles. Although there remain many controversies due to a paucity of data, there appears to be a significant difference between adults and adolescents with respect to a progressive deterioration of semen parameters and it is clear that subclinical varicoceles do not play a major role in male infertility. [References: 86] Publication Type Journal Article. Review.
<19> Unique Identifier 11212075 Status MEDLINE Authors Cozzolino DJ. Lipshultz LI. Authors Full Name Cozzolino, D J. Lipshultz, L I. Institution Scott Department of Urology, Baylor College of Medicine, Houston, Texas, USA. Title Varicocele as a progressive lesion: positive effect of varicocele repair. [Review] [42 refs] Source Human Reproduction Update. 7(1):55-8, 2001 Jan-Feb. Abstract Varicoceles are the leading correctable cause of infertility in men who present to an infertility clinic for evaluation. Consequently, the surgical correction of a varicocele, known as a varicocelectomy, is the most commonly performed operation for the treatment of male infertility. The current data suggest that an individual with a varicocele, even with a previously normal semen analysis or documentation of previous fertility, is at risk for subsequent loss of testicular function and infertility. Many of these patients will need to be treated because there is convincing evidence that a varicocele may have a progressive toxic effect on the testes that may ultimately result in irreversible infertility if left untreated. Identifying those individuals with varicoceles that will ultimately cause fertility impairment is still beyond our current clinical capabilities. Current investigative modalities, e.g. semen analysis, testicular measurement, serum gonadotrophin determination, gonadotrophin-releasing hormone (GnRH) stimulation test, and testis biopsy analysis, may be employed to detect early changes in testicular physiology produced by a varicocele. [References: 42] Publication Type Journal Article. Review.
<20> Unique Identifier 11212074 Status MEDLINE Authors Benoff S. Gilbert BR. Authors Full Name Benoff, S. Gilbert, B R. Institution Center for Molecular and Cell Biology, North Shore-Long Island Jewish Research Institute, Manhasset, New York 11030, USA. [email protected] Title Varicocele and male infertility: part I. Preface. [Review] [128 refs] Source Human Reproduction Update. 7(1):47-54, 2001 Jan-Feb. Publication Type Journal Article. Research Support, U.S. Gov't, P.H.S.. Review.
<21> Unique Identifier 10973638 Status MEDLINE Authors Zini A. Defreitas G. Freeman M. Hechter S. Jarvi K. Authors Full Name Zini, A. Defreitas, G. Freeman, M. Hechter, S. Jarvi, K. Institution Division of Urology, Department of Surgery, Mount Sinai Hospital, University of Toronto, Toronto, Ontario, Canada. [email protected] Title Varicocele is associated with abnormal retention of cytoplasmic droplets by human spermatozoa. [Review] [23 refs] Source Fertility & Sterility. 74(3):461-4, 2000 Sep. Abstract OBJECTIVE: To determine whether varicocele is associated with retention of sperm cytoplasmic droplets in infertile men. DESIGN: Retrospective study.Setting: University infertility clinic. PATIENT(S): Nonazoospermic men with idiopathic (n = 69) and varicocele-associated infertility (n = 73), and 20 fertile controls presenting for vasectomy. INTERVENTION(S): None. MAIN OUTCOME MEASURES(S): Standard semen parameters and percentage of spermatozoa with cytoplasmic droplets on Papanicolaou smears. RESULT(S): No statistically significant differences were found between the fertile and infertile groups with respect to semen volume. Fertile controls had significantly greater mean percent sperm motility and normal morphology than infertile men. The mean percentage of sperm with residual cytoplasm was statistically significantly different in all three groups. Infertile men with varicocele had the highest percentage of sperm with cytoplasmic droplets, the next highest level being in men with idiopathic infertility and the lowest level in fertile controls (11.7 +/- 1.0, 8.1 +/- 0.9 and 3.2 +/- 0.4%, respectively, P<.0001). CONCLUSION(S): Our data show that idiopathic and even moreso, varicocele-related male infertility are conditions associated with impaired disposal of residual sperm cytoplasm by the testis and/or epididymis. These data provide a possible mechanism for the observed semen abnormalities and reduced fertility potential associated with varicocele and idiopathic male infertility. [References: 23] Publication Type Journal Article. Review.
<22> Unique Identifier 9646422 Status MEDLINE Authors Hargreave T. Ghosh C. Authors Full Name Hargreave, T. Ghosh, C. Institution Department of Urology, Western General Hospital, Edinburgh. Title Varicocele: does treatment promote male fertility?. [Review] [38 refs] Source Urologe (Ausg. A). 37(3):258-64, 1998 May. Publication Type Clinical Trial. Journal Article. Multicenter Study. Review.
<23> Unique Identifier 9559833 Status MEDLINE Authors Cockett AT. Takihara H. Iwamura M. Koshiba K. Authors Full Name Cockett, A T. Takihara, H. Iwamura, M. Koshiba, K. Institution Department of Urology, University of Rochester Medical Center, New York 14642-8656, USA. Title Pathophysiology of clinical varicoceles in infertile men. [Review] [4 refs] Source International Journal of Urology. 5(2):113-5, 1998 Mar. Abstract In infertile men, clinical varicoceles most often occur bilaterally. In our experience with these patients, both testicles are smaller than normal. We find more than 25% to 35% immature and tapered sperm in in the ejaculum of these men, and the motility of the sperm is usually low. We have found serotonin in the plasma of the varicoceles, and believe this biogenic amine is responsible for the poor sperm motility. We now agree that a subset of neuroendocrine cells in the prostate secrete serotonin. Bilateral varicocele surgery can improve the patient's fertility potential, and we advocate surgical treatment. [References: 4] Publication Type Journal Article. Review.