SPECIAL STUDY MODULE
An Introduction to Cytology: Principles and Practice
SE Shirley and CT Escoffery
Introduction
Cytology is a division of Anatomical Pathology in which cells are examined under the microscope to detect a variety of diseases including various types of cancers.
There are 2 main types of cytology specimens - gynaecological and non- gynaecological. Gynaecological specimens are usually Pap (cervical) smears. Non-gynaecological specimens fall into 2 categories – exfoliative and fine needle aspiration samples.
Cytologists, sometimes also known as cytotechnologists, are specially trained personnel who prepare cytology slides and examine them under the microscope to diagnose various types of diseases, including some types of cancers. Most of the abnormalities detected by the cytologist (including all of the cancers) are then examined by a pathologist before a final diagnosis is made.
Pap smears
These are named after Dr. George Papanicolaou who in 1928 presented his findings that cancer cells could be found in the vaginal fluid of women with cancer of the cervix. Nowadays, a Pap smear is done by using a spatula or some other device to scrape cells directly from the cervix. These cells are transferred to a slide and sent to the cytologists for examination.
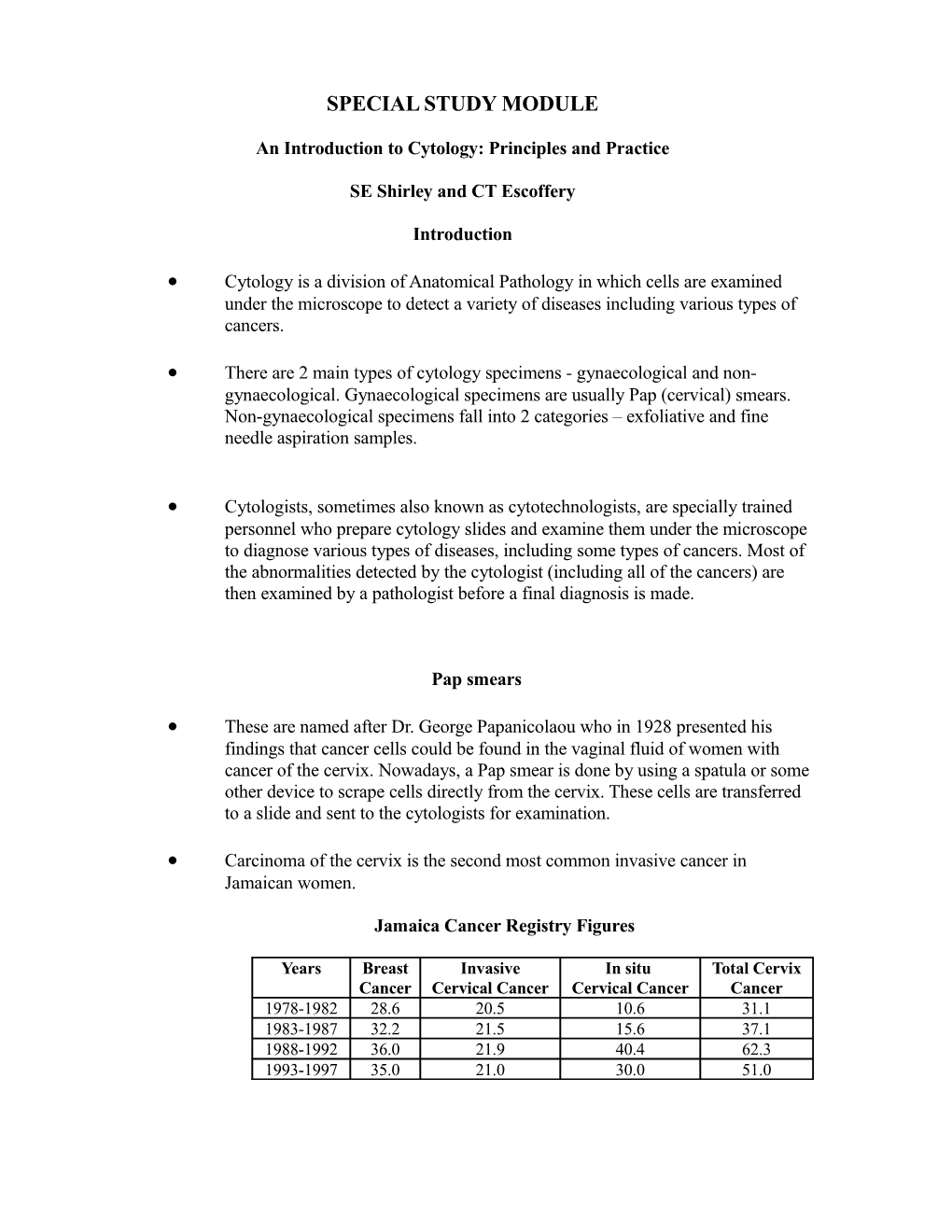
Carcinoma of the cervix is the second most common invasive cancer in Jamaican women.
Jamaica Cancer Registry Figures
Years Breast Invasive In situ Total Cervix Cancer Cervical Cancer Cervical Cancer Cancer 1978-1982 28.6 20.5 10.6 31.1 1983-1987 32.2 21.5 15.6 37.1 1988-1992 36.0 21.9 40.4 62.3 1993-1997 35.0 21.0 30.0 51.0 The Pap smear has been successful worldwide in screening for cervical cancer, reducing morbidity and mortality especially in countries with national screening programmes.
Pre-neoplastic (dysplastic) or early neoplastic changes of the cervix (CIN/SIL) can be detected with the Pap smear and treated appropriately.
Over the past 2 decades, the "dysplasia" classification of premalignant cervical disease fell from favour. The term cervical intraepithelial neoplasia (CIN) was introduced to encompass the whole spectrum of premalignant change in the cervical epithelium. More recently, another classification system was introduced in the USA (The Bethesda System), which uses the term squamous intraepithelial lesion (SIL).
Dysplasia CIN SIL Mild I LSIL Moderate II HSIL Severe/Ca in situ III HSIL
The range of diagnoses that can be made on Pap smears includes: . Normal . Benign cellular changes – infection/inflammation . Epithelial cell abnormalities – Atypical cells of undetermined significance (ASCUS) - (changes fall short of definite CIN/SIL) Squamous (CIN/SIL) Glandular, e.g. adenocarcinoma
ASCUS and LSIL cases can be managed initially with repeat pap smears.
For persistent abnormalities and all higher grades of epithelial abnormalities histological confirmation is required. Biopsies of the cervix are performed under colposcopic guidance by a gynaecologist.
Although the pap smear result usually corresponds to the histologic diagnosis, in some cases, histologic examination may upgrade or downgrade the cytologic impression. Definitive patient management is dependent on the histologic diagnosis from the biopsy and not the screening result of the pap smear. Cytology of HPV/CIN I showing numerous koilocytes (the arrows highlight some good examples)
Histology of HPV/CIN I showing dysplasia confined to the lower third of the epithelium Cytology of CIN II showing moderately dysplastic cells
Histology of CIN II showing dysplasia involving the lower and middle thirds of the epithelium Cytology of CIN III showing severely dysplastic cells
Histology of CIN III showing dysplasia involving the full thickness of the epithelium Exfoliative Cytology
Exfoliative specimens are non-gynaecological specimens from areas of the body where cells are shed (or scraped/brushed) from the lining of organs or tissues into various fluids.
Sites of exfoliative specimens include:
. Lungs – sputum, bronchial washings/brushings etc . Lower urinary tract – urine (voided/catheterized) . Chest and abdominal cavities – pleural, pericardial and peritoneal fluid . Central nervous system – CSF . Gastrointestinal tract – oesophageal, stomach/intestinal brushings
In most cases exfoliative specimens are taken to document the presence or extent of spread of a tumour. Therefore, where the initial cytology is negative, repeat samples are usually advised to increase diagnostic sensitivity.
Fine Needle Aspiration Cytology (FNAC)
FNAC samples are taken from a wide variety of organs and tissues. In the past, FNAC was limited to clinically palpable lesions, but radiologic technology such as CT and ultrasound now allow for access to deep seated impalpable lesions. Common sites sampled by FNAC include breast, thyroid, salivary glands and lymph nodes. A wide range of non-neoplastic and neoplastic diseases can be diagnosed by this technique.
FNAC is a simple, fast, effective and relatively cheap procedure, which can be done in a doctor’s office or the outpatient clinic. Minimal discomfort is involved, similar to that experienced in the taking of blood, and anaesthesia is not usually necessary.
A fine (very thin) needle attached to a syringe is inserted into the relevant tissue in order to extract the cells needed for examination. The cells are smeared on glass slides, stained and examined under the microscope.
FNAC is a valuable primary diagnostic tool, which can be followed by tissue biopsy in cases where the cytology does not permit a definitive diagnosis. The same adjunctive tests used for histology can be used for FNAC, e.g. special stains, immunohistochemistry etc. Cases
Case 1: A 48-year old woman was seen in the Ear, Nose & Throat out-patient clinic with a history of a painless mass in the anterior neck that was slowly increasing in size over the past five years. She was otherwise well, and reported no hoarseness or difficulty in breathing or swallowing. Examination revealed an enlarged, painless thyroid gland, with the right lobe being more prominent than the left. The remainder of the examination was unremarkable. Her thyroid function tests were normal. FNAC of the gland was performed in the clinic.
FNAC of thyroid showing a large group of benign follicular cells with haemosiderin-laden macrophages (plump cells with brown cytoplasmic pigment highlighted by black arrows) and bare nuclei (highlighted by blue arrows) in the background.
Histology of the thyroid gland showing nodules separated by fibrovascular septa (black arrow) with foci of cystic change (blue arrow) and haemorrhage (red arrow.
FINAL DIAGNOSIS: FNAC THYROID, NODULAR GOITRE Case 2:
A 54-year old woman underwent breast ultrasound and mammography as part of her routine annual physical examination. Although clinical examination of the breasts had been normal, a small lump with focal microcalcifications was identified in the upper outer quadrant of the left breast on both the mammogram and ultrasound, and was considered to be suspicious for malignancy by the radiologist. FNAC of the lump was performed by the radiologist under ultrasound guidance.
FNAC breast showing large epithelial cells exhibiting increased nuclear-cytoplasmic ratios, nuclear hyperchromasia and nucleoli.
Histology of breast lump showing invasive ductal carcinoma with foci of necrosis (arrows)
FINAL DIAGNOSIS: FNAC BREAST, INVASIVE DUCTAL CARCINOMA Case 3:
A 65-year old man was referred to the medical out-patient clinic by his general practitioner with a 6 month history of worsening shortness of breath, chronic cough and weight loss. His physical examination and chest x-ray revealed evidence of a right-sided pleural effusion. The chest x-ray also showed a right hilar mass. The fluid was tapped and sent to the microbiology lab for culture, and to the pathology department for cytological evaluation.
Cytology of pleural fluid showing pleomorphic malignant cells.
Cytology of pleural fluid showing vacuolated and multinucleated malignant cells (arrow).
FINAL DIAGNOSIS: PLEURAL FLUID, METASTATIC ADENOCARCINOMA Case 4:
A 68-year old woman presented to the Casualty Department with a two-month history of worsening abdominal distension and discomfort. Ascites was the only significant finding on examination, and no abdominal masses were palpated. She was sent for an abdominal ultrasound, which revealed an ovarian mass that was suspicious for malignancy. She was admitted to the gynaecology ward and some of the ascitic fluid was removed and submitted for cytological assessment.
Cytology of peritoneal fluid showing benign mesothelial cells with eccentric nuclei and abundant cytoplasm (arrows). No malignant cells are present.
FINAL DIAGNOSIS: PERITONEAL FLUID, NEGATIVE FOR MALIGNANCY
Useful internet links: http://medlib.med.utah.edu/WebPath/TUTORIAL/CYTOPATH/CYTOPATH.html http://dpalm.med.uth.tmc.edu/cytopath/