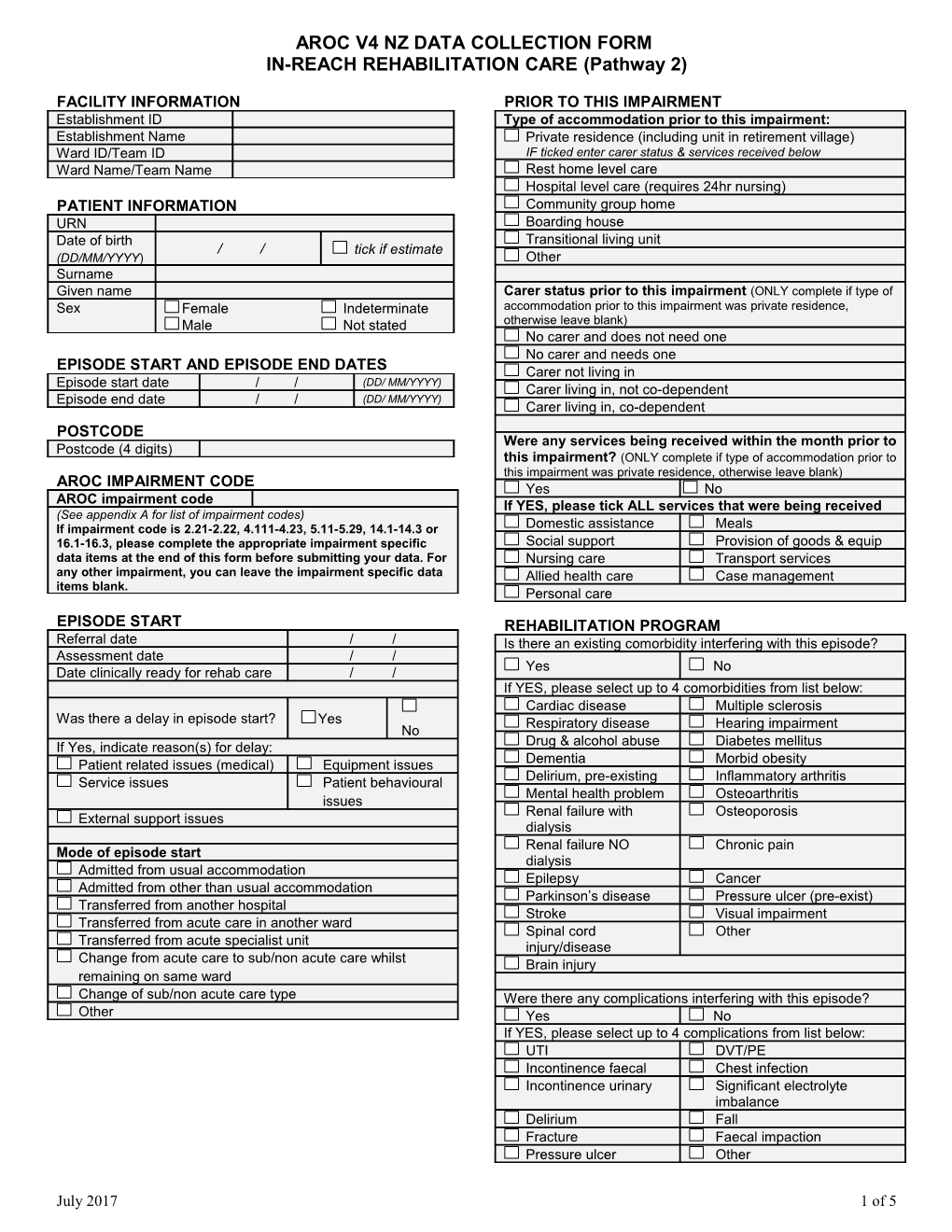
AROC V4 NZ DATA COLLECTION FORM IN-REACH REHABILITATION CARE (Pathway 2)
FACILITY INFORMATION PRIOR TO THIS IMPAIRMENT Establishment ID Type of accommodation prior to this impairment: Establishment Name Private residence (including unit in retirement village) Ward ID/Team ID IF ticked enter carer status & services received below Ward Name/Team Name Rest home level care Hospital level care (requires 24hr nursing) PATIENT INFORMATION Community group home URN Boarding house Date of birth Transitional living unit / / tick if estimate (DD/MM/YYYY) Other Surname Given name Carer status prior to this impairment (ONLY complete if type of Sex Female Indeterminate accommodation prior to this impairment was private residence, Male Not stated otherwise leave blank) No carer and does not need one No carer and needs one EPISODE START AND EPISODE END DATES Carer not living in Episode start date / / (DD/ MM/YYYY) Carer living in, not co-dependent Episode end date / / (DD/ MM/YYYY) Carer living in, co-dependent POSTCODE Were any services being received within the month prior to Postcode (4 digits) this impairment? (ONLY complete if type of accommodation prior to this impairment was private residence, otherwise leave blank) AROC IMPAIRMENT CODE Yes No AROC impairment code If YES, please tick ALL services that were being received (See appendix A for list of impairment codes) If impairment code is 2.21-2.22, 4.111-4.23, 5.11-5.29, 14.1-14.3 or Domestic assistance Meals 16.1-16.3, please complete the appropriate impairment specific Social support Provision of goods & equip data items at the end of this form before submitting your data. For Nursing care Transport services any other impairment, you can leave the impairment specific data Allied health care Case management items blank. Personal care EPISODE START REHABILITATION PROGRAM Referral date / / Is there an existing comorbidity interfering with this episode? Assessment date / / Date clinically ready for rehab care / / Yes No If YES, please select up to 4 comorbidities from list below: Cardiac disease Multiple sclerosis Was there a delay in episode start? Yes Respiratory disease Hearing impairment No If Yes, indicate reason(s) for delay: Drug & alcohol abuse Diabetes mellitus Dementia Morbid obesity Patient related issues (medical) Equipment issues Service issues Patient behavioural Delirium, pre-existing Inflammatory arthritis Mental health problem Osteoarthritis issues Renal failure with Osteoporosis External support issues dialysis Renal failure NO Chronic pain Mode of episode start dialysis Admitted from usual accommodation Epilepsy Cancer Admitted from other than usual accommodation Parkinson’s disease Pressure ulcer (pre-exist) Transferred from another hospital Stroke Visual impairment Transferred from acute care in another ward Spinal cord Other Transferred from acute specialist unit injury/disease Change from acute care to sub/non acute care whilst Brain injury remaining on same ward Change of sub/non acute care type Were there any complications interfering with this episode? Other Yes No If YES, please select up to 4 complications from list below: UTI DVT/PE Incontinence faecal Chest infection Incontinence urinary Significant electrolyte imbalance Delirium Fall Fracture Faecal impaction Pressure ulcer Other
July 2017 1 of 5 AROC V4 NZ DATA COLLECTION FORM IN-REACH REHABILITATION CARE (Pathway 2) Wound infection Boarding house Transitional living unit Hospital REHABILITATION PROGRAM CONTINUED Other Unknown Date MDT rehab plan established / / Final destination (ONLY complete if patient discharged to final or Episode Start (admission) & End (discharge) FIM scores interim destination at episode end, otherwise leave blank) Start End Private residence (including unit in retirement village) IF ticked complete carer status post discharge Date completed / / / / Rest home level care Eating Hospital level care (requires 24hr nursing) Grooming Community group home Bathing Boarding house Dressing upper body Transitional living unit Dressing lower body Other Toileting Unknown Bladder management Bowel management Carer status post discharge (ONLY complete if final destination Transfer at episode end was private residence, otherwise leave blank) bed/chair/wheelchair No carer and does not need one Transfer toilet No carer and needs one Transfer bath/shower Carer not living in Locomotion Carer living in, not co-dependent Stairs Carer living in, co-dependent Comprehension Expression Will any services be received post discharge? (ONLY Social interaction complete if final destination at episode end was private residence, Problem solving otherwise leave blank) Memory Yes No If YES, please tick ALL services that will be received EPISODE END Domestic assistance Meals Date clinically ready for discharge / / Social support Provision of goods & equip (Collection is mandatory if mode of episode end is discharged to final Nursing care Transport services or interim destination, otherwise collection is optional) Allied health care Case management Personal care Was there a delay in discharge? No Yes If YES, indicate reason(s) for delay GENERAL COMMENTS Patient related issues (medical) Equipment issues Patient behaviour Service issues issues External support issues Mode of episode end Discharged to final destination (IF ticked, enter details of final destination in next coloumn) Discharged to interim destination (IF ticked, enter interim destination and final destination in next coloumn) Death Discharged/transferred to other hospital Care type change and transferred to a different ward Care type change and remained on same ward Change of care type within sub/non acute care Discharged at own risk Other and unspecified
EPISODE END CONTINUED Interim destination (ONLY complete if patient discharged to interim destination at episode end, otherwise leave blank) Private residence (including retirement village) Rest home level care Hospital level care (requires 24hr nursing) Community group home
July 2017 2 of 5 AROC V4 NZ DATA COLLECTION FORM IN-REACH REHABILITATION CARE (Pathway 2)
IMPAIRMENT SPECIFIC DATA ITEMS - ONLY Complete data items relevant to patient’s impairment BRAIN DYSFUNCTION Yes No ONLY complete for AROC impairment code 2.21, 2.22, 14.1, 14.2 AMPUTATION OF LIMB (traumatic, open and closed injury) ONLY complete for AROC impairment codes Date patient emerged from PTA / / 5.11, 5.12, 5.13, 5.14, 5.15, 5.16, 5.17, 5.18, 5.19 (non Duration of PTA: traumatic amputation of limb) PTA not recorded 0 days (i.e. never in PTA) 5.21, 5.22, 5.23, 5.24, 5.25, 5.26, 5.27, 5.28, 5.29 (traumatic 1 day (i.e. a couple of mins up 2-7 days amputation of limb) to 24hours) 8-28 days 29-90 days Rockwood Frailty Score (pre-morbid) 91-182 days 183 days or more (chronic Very fit Moderately frail amnesic) Well Severely frail PTA unable to be recorded In PTA at discharge Well, with comorbid disease Terminally ill Apparently vulnerable Unknown or not applicable SPINAL CORD DYSFUNCTION Mildly frail ONLY complete for AROC impairment codes: 4.111, 4.112, 4.1211, 4.1212, 4.1221, 4.1222, 4.13 (NTSCI) Phase of amputee care at EPISODE START 4.211, 4.212, 4.2211, 4.2212, 4.2221, 4.2222, 4.23, 14.1, 14.3 (TSCI) (See Appendix B for explanation of phases of amputee care) ASIA Score (AIS grade) at EPISODE START Pre-operative Prosthetic A B C D E Delayed wound Follow-up Level of SC injury at EPISODE START Pre prosthetic C1 T1 L1 S1 C2 T2 L2 S2 Did the patient pass through the following phases of care C3 T3 L3 S3 DURING their rehabilitation episode? C4 T4 L4 S4 (See Appendix B for explanation of phases of amputee care) Delayed wound? C5 T5 L5 S5 Yes No Pre-prosthetic? C6 T6 Yes No Prosthetic? C7 T7 Yes No C8 T8 Does the patient have a prosthetic device fitted, OR will have one T9 fitted in the future? T10 Yes No (Go to “Outcomes T11 measures at discharge”) T12 Date ready for casting Date known / / ASIA Score (AIS grade) at EPISODE END Date not yet known (please enter 07/07/7777) A B C D E Not suitable for casting (please enter 08/08/8888) Level of SC injury at EPISODE END C1 T1 L1 S1 Date of first prosthetic fitting C2 T2 L2 S2 Date known / / C3 T3 L3 S3 Planned, but date not yet known (please enter 07/07/7777) C4 T4 L4 S4 Has prosthetic device but date unknown (please enter 09/09/9999) C5 T5 L5 S5 C6 T6 Reason for delay in first fitting C7 T7 No delay C8 T8 Issues around wound healing T9 Other issues around the stump T10 Other health issues of the patient T11 Issues around availability of componentry Issues around availability of the service T12 Other issues: Ventilator Dependent at EPISODE END? Yes No Reconditioning– ONLY Complete for AROC impairment Outcome measures at DISCHARGE codes 16.1, 16.2 & 16.3 RECONDITIONING i) Timed up and go (TUG) ONLY complete for AROC Impairment codes 16.1, 16.2 and 16.3 Record time in completed seconds _____ Rockwood Frailty Score (pre-morbid) (RecordRockwood 9999 ifFrailty not applicable Score (pre-morbid) or not appropriate (xxxx) Very fit Moderately frail for episodeVery of fit care) Moderately frail ii) Well 6 minute walk (optional) Severely frail Well Severely frail Record Well,distance with in comorbidmetres disease Terminally ill _____ Well, with comorbid disease Terminally ill (RecordApparently 999.9 if not vulnerableapplicable or not appropriate Unknown or not applicable(xxx.x) Apparently vulnerable Unknown or not applicable for episodeMildly of care)frail Mildly frail iii) 10 metre walk +/- aid (optional) Was patient able to participate in therapy from day 1? Record time in completed seconds _____ Was patient able to participate in therapy from day 1? Yes No (Record 9999 if not applicable or not appropriate (xxxx) Yes No Has patient fallen in the last 12 months? for episode of care) Yes No Has patient fallen in the last 12 months? Has patient lost >10% of their body weight in the last 12 months? Yes No
July 2017 Has patient lost >10% of their body weight in the last 123 months? of 5 Yes No AROC V4 NZ DATA COLLECTION FORM IN-REACH REHABILITATION CARE (Pathway 2) APPENDIX A: AROC Impairment codes V2
Rehabilitation Impairment Code _ _ . _ _ _ _
Use the AROC Impairment Codes to code the impairment which is identified at the beginning of the episode as the major focus of rehabilitation and the primary subject of the rehabilitation plan. Use AROC Impairment Coding Guidelines if unsure.
STROKE AMPUTATION OF LIMB CARDIAC Haemorrhagic Not resulting from trauma 9.1 Following recent onset of new cardiac 1.11 Left body involvement 5.11 Single upper above elbow impairment 1.12 Right body involvement 5.12 Single upper below elbow 9.2 Chronic cardiac insufficiency 1.13 Bilateral involvement 5.13 Single lower above knee (includes 9.3 Heart and heart/lung transplant 1.14 No paresis through knee) 1.19 Other Stroke 5.14 Single lower below knee 5.15 Double lower above knee (includes Ischaemic PULMONARY through knee) 1.21 Left body involvement (right brain) 10.1 Chronic obstructive pulmonary disease 5.16 Double lower above/below knee 1.22 Right body involvement (left brain) 10.2 Lung transplant 5.17 Double lower below knee 1.23 Bilateral involvement 10.9 Other pulmonary 5.18 Partial foot (single or double) 1.24 No paresis 5.19 Other amputation not from trauma 1.29 Other stroke Resulting from trauma BURNS 5.21 Single upper above elbow 11 Burns BRAIN DYSFUNCTION 5.22 Single upper below elbow Non-traumatic 5.23 Single lower above knee (includes 2.11 Sub-arachnoid haemorrhage through knee) CONGENITAL DEFORMITIES 2.12 Anoxic brain damage 5.24 Single lower below knee 12.1 Spina bifida 2.13 Other non-traumatic brain dysfunction 5.25 Double lower above knee (includes 12.9 Other congenital deformity through knee) Traumatic 5.26 Double lower above/below knee 2.21 Open injury 5.27 Double lower below knee OTHER DISABLING IMPAIRMENTS 2.22 Closed injury 5.28 Partial foot (single or double) 13.1 Lymphoedema 5.29 Other amputation from trauma 13.3 Conversion disorder NEUROLOGICAL CONDITIONS 13.9 Other disabling impairments that cannot ARTHRITIS be classified into a specific group 3.1 Multiple Sclerosis 6.1 Rheumatoid arthritis 3.2 Parkinsonism 6.2 Osteoarthritis 3.3 Polyneuropathy 6.9 Other arthritis 3.4 Guillian-Barre MAJOR MULTIPLE TRAUMA 14.1 Brain + spinal cord injury 3.5 Cerebral palsy PAIN SYNDROMES 3.8 Neuromuscular disorders 14.2 Brain + multiple fracture/amputation 7.1 Neck pain 3.9 Other neurological conditions 14.3 Spinal cord + multi fracture/amputation 7.2 Back Pain 14.9 Other multiple trauma 7.3 Extremity pain 7.4 Headache (includes migraine) SPINAL CORD DYSFUNCTION 7.5 Multi-site pain DEVELOPMENTAL DISABILITIES Non traumatic spinal cord dysfunction 7.9 Other pain (includes abdo/chest wall) 4.111 Paraplegia, incomplete 15.1 Developmental disabilities (excludes 4.112 Paraplegia, complete cerebral palsy) 4.1211 Quadriplegia, incomplete C1-4 ORTHOPAEDIC CONDITIONS 4.1212 Quadriplegia, incomplete C5-8 Fractures (includes dislocation) 4.1221 Quadriplegia, complete C1-4 RE-CONDITIONING/RESTORATIVE 8.111 Fracture of hip, unilateral (incl #NOF) 4.1222 Quadriplegia, complete C5-8 16.1 Re-conditioning following surgery 8.112 Fracture of hip, bilateral (incl. #NOF) 4.13 Other non-traumatic spinal cord 16.2 Reconditioning following medical illness 8.12 Fracture of shaft of femur dysfunction 16.3 Cancer rehabilitation 8.13 Fracture of pelvis Traumatic spinal cord dysfunction 8.141 Fracture of knee 4.211 Paraplegia, incomplete 8.142 Fracture of lower leg, ankle, foot 4.212 Paraplegia, complete 8.15 Fracture of upper limb 4.2211 Quadriplegia, incomplete C1-4 8.16 Fracture of spine 4.2212 Quadriplegia, incomplete C5-8 8.17 Fracture of multiple sites 4.2221 Quadriplegia, complete C1-4 8.19 Other orthopaedic fracture 4.2222 Quadriplegia, complete C5-8 Post Orthopaedic Surgery 4.23 Other traumatic spinal cord dysfunction 8.211 Unilateral hip replacement 8.212 Bilateral hip replacement 8.221 Unilateral knee replacement 8.222 Bilateral knee replacement 8.231 Knee and hip replacement, same side 8.232 Knee and hip replacement, diff sides 8.24 Shoulder replacement 8.25 Post spinal surgery 8.26 Other orthopaedic surgery Soft tissue injury 8.3 Soft tissue injury
July 2017 4 of 5 AROC V4 NZ DATA COLLECTION FORM IN-REACH REHABILITATION CARE (Pathway 2)
APPENDIX B: Amputee Phases of Care – Definition Summaries
1 = Pre-operative Clinical decision to perform amputation including assessment of urgency (following trauma or infection). Comprehensive interdisciplinary baseline assessment of patient’s status including medical assessment, functional status including function of contralateral limb, pain control and psychological and cognitive assessment, patient’s goals, social environment and support systems Post-operative care plan should be determined by surgeon and rehabilitation team to address medical, wound or surgical and rehabilitation requirements 2 = Delayed wound Where problems occur with wound healing, consider additional interventions as needed including revision surgery, vascular and infection evaluation, aggressive local wound care and hyperbaric oxygen 3 = Pre prosthetic Patient is discharged from acute care and enters inpatient rehabilitation program or is treated in ambulatory setting Postoperative assessment to review patient’s status including physical and functional assessment; completion of FIM baseline and other relevant assessments Determine rehabilitation goals, establish or update rehabilitation treatment plan and provide patient education Provide physical and functional interventions based on current and potential function Determine whether a prosthesis is appropriate to improve functional status and meet realistic patient goals 4 = Prosthetic Determine functional goals of prosthetic fitting Prescribe prosthesis based on current or potential level of ambulation Interim or permanent prosthetic fitting and training, and early rehabilitation management Provision of prosthetic gait training and patient education on functional use of prosthesis for transfers, balance and safety 5 = Follow-up Scheduled follow-up appointment after discharge from rehabilitation Assessment of patient’s goals, functional assessment, secondary complications, prosthetic assessment (repair, replacement, mechanical adjustment and new technology) and vocational and recreational needs Provide secondary amputation prevention (where relevant) Prosthesis not appropriate: patient is discharged from acute care and enters inpatient rehabilitation program or is treated in ambulatory setting; rehabilitation focus may include transfers, functional mobility, wheelchair mobility, ADL training
July 2017 5 of 5