Will Advances in Reproductive Technology Affect Future Generations?
Emily Cook, Angela Riley, Stephanie Lloyd ?? Laws, Technology and Public Belief Laws, technology and public belief play an important role in initiating and sustaining certain behaviours in people that are deemed acceptable (and legal) in society. When a particular action or event becomes legalised, this often has the effect of changing peoples’ beliefs and attitudes towards it. A situation that may have previously been considered as dangerous or unethical may now be viewed with acceptance and approval once it becomes legalised.
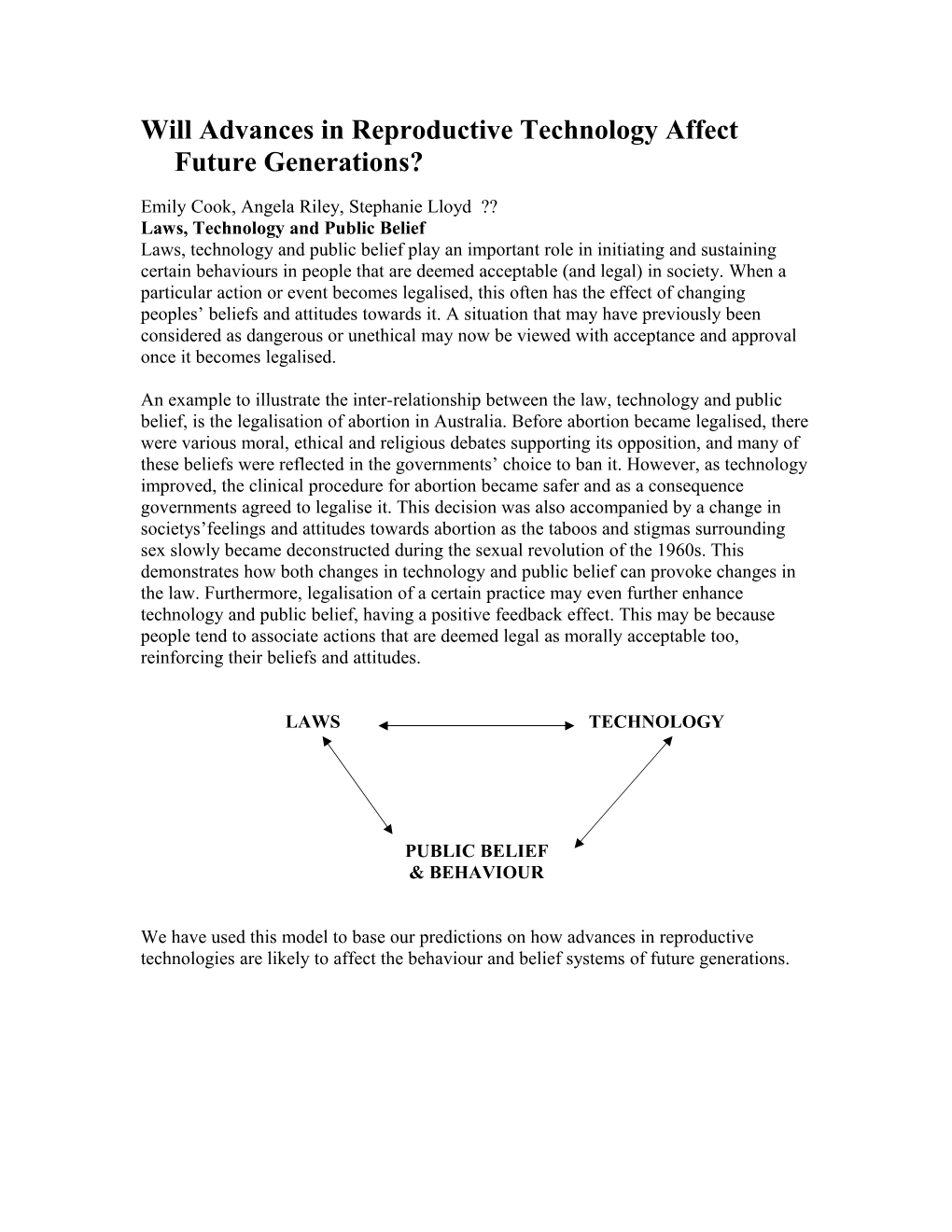
An example to illustrate the inter-relationship between the law, technology and public belief, is the legalisation of abortion in Australia. Before abortion became legalised, there were various moral, ethical and religious debates supporting its opposition, and many of these beliefs were reflected in the governments’ choice to ban it. However, as technology improved, the clinical procedure for abortion became safer and as a consequence governments agreed to legalise it. This decision was also accompanied by a change in societys’feelings and attitudes towards abortion as the taboos and stigmas surrounding sex slowly became deconstructed during the sexual revolution of the 1960s. This demonstrates how both changes in technology and public belief can provoke changes in the law. Furthermore, legalisation of a certain practice may even further enhance technology and public belief, having a positive feedback effect. This may be because people tend to associate actions that are deemed legal as morally acceptable too, reinforcing their beliefs and attitudes.
LAWS TECHNOLOGY
PUBLIC BELIEF & BEHAVIOUR
We have used this model to base our predictions on how advances in reproductive technologies are likely to affect the behaviour and belief systems of future generations. CLONING Angela Riley
What Is Cloning? Cloning is the process in which the DNA of an oocyte is removed and replaced with a different set of DNA from another cell. This technique is also referred to as somatic cell nuclear transfer. Scientists transfer genetic material from the nucleus of a donor adult cell to an egg whose nucleus, and thus its genetic material, has been removed. The reconstructed egg containing the DNA from a donor cell must be treated with chemicals or electric current in order to stimulate cell division. Once the cloned embryo reaches a suitable stage, it is transferred to the uterus of a female host where it continues to develop until birth.
Types of Cloning There are two types of cloning: reproductive and therapeutic. Reproductive cloning uses the cloning procedure to produce a clonal embryo which is implanted in a woman's womb with intent to create a fully formed living child. Therapeutic cloning uses the cloning procedure to produce a clonal embryo, but instead of being implanted in a womb and brought to term it is used to generate stem cells. The purpose of using clonal embryos to generate stem cells is to allow creation of tissues or organs that the clonal donor can use without having these tissues or organs rejected by their body's immune system.
The Current Law in Australia Laws are generally not made unless a certain situation is creating a problem that needs to be regulated, or if a situation poses a problem that can be reasonably foreseen and hence requires the law to cease it or place limitations on it. The birth of Dolly the sheep in 1997 was a pivotal moment in the history of cloning because it inspired the creation of cloning laws in many nations including Australia. Human cloning was not considered feasible until Dolly, and when it was suggested that the same method used for Dolly could be used to clone humans, governments around the world gave their full attention to cloning, setting in motion a series of laws.
The current law in Australia governing the cloning of humans prohibits any somatic cell nuclear transfer, either for reproductive or therapeutic purposes. According to the Commonwealth Prohibition of Human Cloning Act 2002, a person commits an offence if the person intentionally creates a human embryo clone. It further states that it is an offence to create a human embryo for a purpose other than achieving pregnancy in a woman. The objective of this Act is to address concerns, including ethical concerns, about scientific developments in relation to human reproduction, and the utilization of human embryos by prohibiting certain practices.
If Reproductive Cloning Were To Be Legalised If reproductive cloning was legalised, this technology could help infertile couples. 1 in 12 couples are unable to conceive naturally, and of those that resort to assisted reproductive technology (‘ART’), roughly 30% result in a live birth. Therefore, cloning would be suitable for couples who have failed repeatedly with current ART and are intent upon having genetically related offspring. This would provide an alternative to surrogacy (which is illegal in Australia), adoption or sperm/oocyte donation. But what would be the implications for future generations if reproductive cloning were to become legalised?
The legalisation of reproductive cloning is likely to have a profound impact on future generations. One major concern is the negative impact cloning may have on the psychological welfare of future ‘cloned’ children. A human clone is essentially a time- delayed identical twin of an already-existing person. There is a fear that by having the same genome as someone else, this will lead to a lack of individual identity. Clones may also be subject to strong parental expectations to behave in a manner similar to the person from whom they are cloned, rather than being given the autonomy to express and develop their own individuality and identity.
It is very likely that a person will be cloned based on some quality or qualities they possess, which is hoped the duplicate clone will also possess. This may create the potential for a loss of uniqueness of the clone as an individual. If they have knowledge of facts about his or her origin, they may be feel paralysed from being spontaneous in becoming himself or herself due to this expectation.
As well as depriving children from a sense of individual identity, cloning may also result in the commodification of children. If parents have complete control over the genome of their children, this may lead them and society to view children as commodities, or objects which exist to satisfy adult desires, rather than ends in themselves. This may the deprive the child from being recognised for qualities that they uniquely possess.
Reproductive cloning may set in the motion the revival of a eugenic society, whereby children are selected on the basis of certain genetic characteristics, breeding out unfavourable characteristics in the process. Therefore, cloning may well provide the means by which society can improve the quality of their race by controlling what characteristics are inherited by future generations. The selection of children based on the presence or absence of certain qualities may not only affect the cloned children, but also affect people already in existence who possess undesirable characteristics and are intentionally not chosen to be cloned. This may lead to a sense of rejection, feeling of insecurity and subsequent marginalisation.
Cloning may potentially pose a threat to genetic diversity, affecting society aa a whole and not just at an individual level. If the widespread use of cloning became legalised and available to all people, this could mimic the action of a “controlled evolution”, allowing for the development of only those qualities that humans desire. While variety in the world may be important for providing originality and fascination it may also be necessary for the biological environment. If too many cloned people are selected and certain traits are bred out, this may cause inbreeding, resulting in substantial risks to the gene pool.
If Therapeutic Cloning Were To Be Legalised The legalisation of therapeutic cloning could open the doorway to a myriad of medical breakthroughs, having a profound impact on the health of future generations. The goal of therapeutic cloning is not to create cloned human beings, but rather to harvest stem cells that can be used to study human development and to treat disease. Stem cells are important to biomedical researchers because they can be used to generate virtually any type of specialized cell in the human body. This would be extremely beneficial to people suffering degenerative diseases that cannot be treated pharmaceutically and require the replacement of damaged cells. For example, stem cells could be cultured to grow into nerve cells for spinal cord injuries, skin cells to provide grafts for burns victims or bone marrow for cancer (leukaemia) sufferers.
Stem cells could also be specialised to grow into specific tissues and organs to be transplanted. Organ transplantation often fails as a result of the patient’s immune system recognising the new organ as foreign and rejecting it. Cloned organs would be a genetic match to the host individual, therefore this could eliminate the problem of rejection by extracting stem cells from an embryo created by the fusion of the patient’s own somatic cell with an enucleated egg. The stem cells derived could then grow into a specific tissues or organs to be transplanted back into the patient without fear of rejection. An example of this is the extraction of cells from a person’s healthy kidney and fuse them with embryonic stem cells to then grow a second kidney for transplantation. This would also provide a way around the serious shortage of organs and tissues needed for transplantation.
As a whole, therapeutic cloning would enhance basic research aimed at understanding matters such as cell division and early human development. This may provide important clues into the origins of birth defects, the way alterations in cell division are involved in producing cancer, and the ageing process. Research on embryonic stem cells would be more accurate since current research on animals can often have differences, making the transfer of results into humans difficult or speculative. DESIGNER BABIES Stephanie Lloyd
“Designing babies” is mainly a combination of two areas of assisted reproductive technology (ART). The first is pre-implantation genetic testing (PGT) which is either the testing of embryos for chromosomal abnormalities and pre-implantation genetic screening (PGS); or pre-implantation genetic diagnosis (PGD) which is testing for known genetic disorders. (Preimplantation Genetic Testing, n.d.), The second is germ line therapy (Biotechnology latest news: Special focus Designer Babies, n.d.), which will most probably change a lot and become very controversial in the future. It is already raising many ethical issues but it is really more a fabrication by the media than a reality as many of the techniques needed for “designing babies” are no more than ideas at the present. As has happened in history, the way in which “designer babies” will have an influence on future generations and the public opinion will be based on the advancements of the technologies involved. This is because with the advancements of technologies comes a change in public opinion and belief and then in turn changes occur to the laws that govern these technologies. There are six different techniques that come under the term “designing babies”; screening embryos for high-risk diseases, screening embryos for unknown diseases, selecting the sex of a baby, picking an embryo for its specific traits, genetic manipulation for therapeutic reasons and genetic manipulation for cosmetic reasons (Biotechnology latest news: Special focus Designer Babies, n.d.). Each of these techniques is likely to change in the future and so influencing public belief and therefore the laws relating to “designer babies”.
1. SCREENING EMBRYOS FOR HIGH-RISK DISEASES
The technique of screening embryos for high-risk diseases comes under the widely used term “designer babies” because by finding out which embryos have the genes for diseases that are at a high risk of being passed on from the parents and which do not, a choice would then be made not to use the unhealthy embryos, and so one is in a way choosing or “designing” their child. The ART used here is pre-implantation genetic diagnosis (PGD) which involves four stages. The first is embryo biopsy where a cell or blastomere is taken from the embryo after an opening is made in the outside coating or zona of the embryo using a laser. The second is cell fixation, the third is genetic analysis which is done using polymerase chain reaction (PCR) and the fourth stage is embryo transfer. This technique is very useful in the early detection of many inherited genetic disorders such as Cystic Fibrosis, Huntington’s disease, Myotonic Dystrophy, Haemophilia and many other conditions, including rare familial ones (Preimplantation Genetic Testing, n.d., Biotechnology latest news: Special focus Designer Babies, n.d.).
Current public opinion The public opinion on the technique of screening embryos for high-risk diseases is generally that it is quite a useful technique that is morally sound. People reason that if one is to spend so much time, effort and money on an ART procedure and there is a high risk of the parents passing on specific genetic disorders to their children, then it is plausible to diagnose the embryos before implantation in order to ensure a healthy embryo is chosen (Biotechnology latest news: Special focus Designer Babies, n.d.). If a couple does not require the aid of ART to get pregnant but there is high-risk of the child inheriting specific genetic disorders from the parents, PGD can still be done but only with the aid of ART. This is slightly more controversial as some people, in particular religious groups, believe that this is “playing God” too much, because no reproductive assistance was needed in the first place. In general though the public opinion is again that this is plausible as there is a known high risk for the child and it is almost morally wrong to put a person through a debilitating disorder when it was not necessary (“Screening picks ‘best chance’ embryos”, 2000, “Science screens out defective genes”, 2000).
Future public opinion In the future, the technology of PGD will most probably improve in the way that even more genetic disorders can be diagnosed and with greater ease and less time. With these improvements in the technology will come a change in public opinion on the technique, which will probably also be an improvement. People will become more accepting of the procedure as it will become more and more common as a result of the improving technology. Also, people are steering away from religious type beliefs and starting to be influenced by more scientific and general moral views even now, and this will most probably develop even more in the future. Another reason why public opinion on this technique will become more relaxed is because of with the improvements in the technology will come a safer procedure.
Current Laws The laws on this particular technique of screening embryos for high-risk diseases have only just changed to make it legal in Western Australia. The Human Reproductive Technology Act 1991 (WA) and the Amendment Act 1996 says that treatment for infertile de facto and legally married couples and single women and the prevention of the transfer of genetic diseases is allowed (Reproductive Technology: Legislation around Australia, n.d.). The Human Reproductive Technology Amendment Act 2004 and the Acts Amendment (Prohibition of Human Cloning and Other Practices) Act 2004 were passed through both houses of parliament in 2004 and brought the WA legislation into consistency with the nationally agreed legislation (Reproductive Technology Council, Government Response to the Report from the House of Commons Science and Technology Committee, n.d.). This permits the Reproductive Technology Council to approve PGD which was previously prohibited in WA. This is only on the basis of there being scientific and medical knowledge that indicates it is unlikely that the embryo will be left unfit for implantation after the procedure and that there is a significant risk of a serious genetic abnormality or disease being present in the embryo. Also PGD can only be approved for people eligible for IVF under the HRT Act or when there is a high risk of a genetic disorder being passed on from the parents to the child (Reproductive Technology Council).
Future Laws In the future the laws on screening embryos for high-risk diseases will most probably stay very similar to what they are today. This technique is quite a plausible and moral one and public opinion towards it will only get more relaxed, which will in turn influence the laws also to become more relaxed. With the law now allowing this procedure to be performed in WA, in both the case of embryos in an IVF procedure and embryos not in an IVF procedure, the only way the law could become more relaxed is to make it legal without the approval of the Reproductive Technology Council. There would however still need to be assurance that the embryo would not be harmed and that there is definite need for the genetic diagnosis.
2. SCREENING EMBRYOS FOR UNKNOWN DISEASES
The second technique of “designing babies” is the screening of embryos for unknown diseases which uses the same technologies as PGD. However, other unpredictable chromosomal disorders can be screened using pre-implantation genetic screening (PGS), which come under the same technique name. These disorders cause things like birth defects, miscarriage and diseases like Down’s syndrome. PGS is recommended for couples who have an increased risk of producing embryos with the wrong number of chromosomes (aneuploidy) which is a high risk in women over 35, women who have had more than two miscarriages or women who have more than two failed IVF attempts. The technique of PGS has the same stages as PGD but the genetic analysis stage is different. Fluorescent in situ hybridization (FISH) is used which involves five probes for five chromosomes each with a different fluorescent tag being mixed with the fixated cell. Each tag is known to be for a specific chromosome and there should be two copies of every chromosome in every cell. By this the screener can identify which chromosomes are present and if there are any abnormalities in them. Also the correct number of chromosomes can be checked (Preimplantation Genetic Testing, n.d.).
Current Public Opinion The public opinion for the technique of screening embryos for unknown diseases is very similar to that of the technique of screening embryos for high-risk diseases, that in general, it is okay. The procedure is again more moral than immoral and it is argued that if the technology is available to prevent genetic diseases, you should be able to access it. Also there is the argument that if a couple is to go through IVF and spend all that time, money and effort then they should be entitled to a procedure to check that the embryo they are using is healthy. PGS is only used for couples that are undergoing some kind of ART, making the screening even more acceptable, especially when the technique is usually used as a last resort when previous IVF attempts have failed or there is a high risk of miscarriage. Another argument is that the body rejects most defective embryos in natural pregnancies anyway there should not be a problem with screening for defective embryos with PGS (Biotechnology latest news: Special focus Designer Babies, n.d.). Of course there will always be arguments against procedures involving screening embryos for unknown diseases one being that first there will be attempts to prevent diseases, but then the technology will progress and eventually embryos will be able to be screened for intelligence or athleticism, all with the argument that it will be better for the child (Deneen, n.d., Cookson, 2001). This is more a minority argument though, as the general public opinion is that this procedure is plausible. Future Public Opinion The public opinion on screening embryos for unknown diseases will most probably become more relaxed in the future because it is already generally accepted and the procedure is a moral one. Also, with improvements to the technology the procedure is most likely to become safer towards the embryo and the mother and this always makes people’s opinions on the area relax.
Current Laws There are no laws on the technique of screening embryos for unknown diseases but the Human Reproductive Technology Amendment Act 2004 and the Acts Amendment (Prohibition of Human Cloning and Other Practices) Act 2004 (Reproductive Technology Council), which permit the Reproductive Technology Council to approve PGD, only do so on the basis of there being a significant risk of passing on a genetic disorder from the parents to their children. This means that the screening of embryos for unknown diseases is not yet legal in WA, as there would not be significant risk. This even goes for IVF couples. The PGS technique used in an attempt to prevent birth defects, miscarriage and other disorders caused by aneuploidy is legal, as it is already being used in fertility clinics for patients of IVF and who are at risk of these things. However, legality would only be for couples that are eligible to use IVF under the HRT Act.
Future Laws In the future the laws on this technique could well change to include the screening of unknown diseases as well as high-risk diseases. It seems plausible and as public opinion gets more relaxed on this subject the laws should also be influenced. The law on PGS could also become more relaxed in that it could become legal for non-IVF couples to access the procedure.
3. SELECTING SEX OF A BABY
The third technique of “designing babies” is selecting the sex of a baby. This can be done in three different ways; by selecting the sperm that are more likely to produce males or females which ever the case may be (there have been recent advances in this technology), by using PGS and by determining the sex several weeks into pregnancy in which case an abortion can be given if the sex is wrong (Biotechnology latest news: Special focus Designer Babies, n.d.). PGS is the best way of selecting sex as it is more reliable and easier than selecting sperm before fertilization and it is less emotional than finding out once pregnancy has begun and then needing an abortion. PGS was explained in the previous technique discussed, the only difference is that at the genetic analysis stage the sex chromosomes must be tagged. This means two tags have to be used, one for the X chromosome and one for the Y chromosome so the sex can be identified, where XX is a girl and XY is a boy. This is however done in most PGS standard genetic analyses anyway (Preimplantation Genetic Testing, n.d.).
Current Public Opinion This area of “designing babies” is very controversial today, with there being many arguments for and against the technique. One argument for selecting the sex of a baby is that there might be legitimate medical reasons for wanting a child to be a certain sex. This is because there are many diseases that can only be passed on through either the male line or female line of descendants (Biotechnology latest news: Special focus Designer Babies, n.d.). This is quite a moral argument although PGD can be used instead of selecting the sex before the embryo is even checked for the disease. This however is the most plausible reason in public opinion. Another reason for selecting the sex is if a couple has had all of one sex and desperately wants a child of the opposite sex. This is not really a plausible argument in public opinion as a want is not really a good enough reason for “playing God”. However, there have been cases of this occurring and it is probably because people can relate to the situation. The last reason is to simply choose the sex of your child based on your preference, which is the most controversial of all the reasons in public opinion. Again a want is not really a valid reason for using this technique and this is really getting close to the literal meaning of “designing babies” and could even lead to Eugenics in some peoples’ opinions (Deneen, n.d., Cookson, 2001, Biotechnology latest news: Special focus Designer Babies, n.d.). Also, this could lead to an unbalanced male: female ratio, although there would have to be a lot of people selecting one sex for this to occur significantly (Biotechnology latest news: Special focus Designer Babies, n.d.).
Future Public Opinion In the future the public opinion on this technique of selecting the sex of a baby, will probably get more relaxed for the reason of passing on diseases down a specific sex line, and maybe even for choosing the sex based on only having had children of the other sex before, but public opinion will not really get more relaxed on the last reason for choosing sex. This however will even become a more accepted idea in the distant future but only when the technology and safety of the procedure improve.
Current Laws The law in Western Australia now stands that it is illegal for the sex of a child to be chosen using any of the methods mentioned above, but mainly PGS. The Human Reproductive Technology Amendment Act 2004 and the Acts Amendment (Prohibition of Human Cloning and Other Practices) Act 2004 (Reproductive Technology Council) says that PGD is only legal for diagnosing disorders that are at a high risk of being passed on from parent to child in both IVF and non-IVF couples. It then goes on to say that sex selection is not yet permitted.
Future Laws The future of this law is likely to be the legalisation to select the sex of one’s child for legitimate medical reasons. This will be because of the moral aspect involved and that it is very similar to the two previous “designer baby” techniques. Public opinion on this becoming more relaxed will be the main influencing factor. The selecting of the sex of a baby for selfish reasons whether or not you have had only children of one sex will probably not really become legal for a while except in exclusive cases. However, laws will probably get more relaxed in for these procedures, and these may eventually be legalised in the future.
4. PICKING AN EMBRYO FOR ITS SPECIFIC TRAITS
The fourth technique of “designing babies” is picking an embryo for its specific traits which would require PGS, as traits can only be identified in an embryo by looking at its genes and therefore chromosomes. This technology is not yet a reality as scientists have not identified the genes responsible for specific and desirable traits, however it is predicted that doctors will be able to generate a general genetic profile of a couple’s embryos of which they can then choose (Biotechnology latest news: Special focus Designer Babies, n.d., Preimplantation Genetic Testing, n.d.).
Current Public Opinion This is not accepted by the public as there is always the worry of Eugenics, already practiced in Europe with Stalin in Russia, Hitler in Germany and Mao in China. Also, there are fears of the creation of a super-race which are people that have been chosen for their good traits when they were embryos. This will create segregation in societies with only the rich and elite being able to afford this procedure (Biotechnology latest news: Special focus Designer Babies, n.d., Deneen, n.d.).
Future Public Opinion In the future public opinion will be very similar to this, although there will be some people who feel they need to take natural selection into their own hands and create a perfect race. If any of these kinds of people are in places of power the use of this technology could get really out of hand and much destruction to the social aspect of the human race could come about. Also, some people might make the argument that by using this technique we are eliminating the undesirable and creating more humans who have desirable traits and so eventually the world will become a better place. They could argue that they are “saving” the human race without having to kill anyone. Maybe this could become a widely held belief.
Current Laws There are no laws on this technique as the technology is not yet here, but if there was to be a law on this technique, it would say that it was illegal. This is due to the strong public opinion surrounding such issues at the moment and to do with the general public fear about a re-emergence of eugenics.
Future Laws In the future it would be illegal for the same reasons, unless somebody in power feels that it would be a benefit to the human race without hurting anyone and passed a law to make it legal. They would need laws about financial support for the procedure, otherwise there would only be a few people who would be able to afford it and that segregation would not be good for society. Also, there would need to be an incentive or a law that strongly recommended couples undergo this procedure, which of course would be an issue with religious groups. Maybe the law to allow it would only be able to come about after the fall of fundamentalism.
5. GENETIC MANIPULATION FOR THERAPEUTIC REASONS
Genetic manipulation for therapeutic reasons is the fifth technique of “designing babies” which requires the use of what’s called germ line therapy. Germ line means that it is performed on an egg, sperm or an embryo and the idea is that pieces of diseased or defective DNA are removed and replaced with healthy DNA (Biotechnology latest news: Special focus Designer Babies, n.d.). The embryo is improved, in terms of health, at the genetic level. This however is not yet a reality as this kind of technology is not yet available but there have been recent breakthroughs in this area.
Public Opinion Public opinion on this, in the future as it has not yet been invented, would probably be that it is fairly plausible for similar reasons as screening embryos for high-risk and unknown diseases. Again it is morally sound although genetic manipulation is actually altering the DNA, instead of just choosing out of what is already there, and so this procedure will be more controversial. People also might question whether it is okay to make an embryo even healthier than it possibly ever would be. Also there would be controversy on whether or not cutting out one piece and replacing it will cause other complications down the track (Deneen, n.d., Cookson, 2001).
Legal Status There are no laws on this area as is not a reality yet, but when the technology comes about it will probably be made legal. This will be due to the therapeutic reasons of this technique. Also as the technology improves so will the safety of the procedure and so people will relax their opinions of it and so too will the laws become more relaxed. It will however probably only be legal if there is a council to approve it in each particular case, and there would need to be many regulations.
6. GENETIC MANIPULATION FOR COSMETIC REASONS
Genetic manipulation for cosmetic reasons is also a technique of “designing babies” that is not yet a reality. Germ line therapy would again be used but instead of removing unhealthy DNA and replacing with healthy DNA, sections of DNA or genes that are known to give certain desirable traits would be added. Also sections that give bad traits could be cut out. This technique would mainly alter traits like hair colour, eye colour and height and not traits like intelligence and beauty as they are so influenced by environmental factors such as parenting and nutrition (Biotechnology latest news: Special focus Designer Babies, n.d.).
Public Opinion Public opinion on this technique will most probably be that it is not acceptable. Even now there are fears of this occurring in the human race due to technological advances. There is always the big worry of eugenics appearing again and this technique will gives means to this. Religious groups will be strongly against this technique as it is “playing God” and not for any therapeutic reasons which are even very controversial in religious groups. Also there are fears of a super-race being created in which everyone is beautiful, rich and elite because they are the only ones that can afford the procedure. This will cause great societal segregation (Deneen, n.d., Cookson, 2001, Biotechnology latest news: Special focus Designer Babies, n.d.).
Legal Status The laws on this will most probably come about when the technology appears, but as yet there are not laws on the technique of genetic manipulation for cosmetic reasons. When the technology becomes available it will be illegal due to a very strong public opinion, which is even present about this kind of technique these days. Maybe it would be made legal if it is found that certain diseases are more likely in people with certain physical traits that can be altered by this technique of genetic manipulation. There would however have to be a significant risk of the disease being present and the procedure would be very regulated (Reproductive Technology Council). In tyrannical societies, people with power could utilise this technology to create a race that they want, and to control people, which obviously would be a very dangerous thing for the human race (Deneen, n.d.).
Designing babies is a very controversial area of reproductive technology in this day and age, although most of the public hysteria on this topic is falsely fuelled by the media. Scientifically there are six different techniques that could be classified under the term “designer babies” of which three are already available and three are merely ideas. With the advancements of these technologies future generations are going to be greatly influenced in the ways of their opinions and the laws governing these areas of ART. Generally, public opinions will be that therapeutic techniques are plausible with regulations and cosmetic techniques are not plausible with the laws always reflecting these opinions. OVARIAN TISSUE CRYOPRESERVATION Emily Cook
What is ovarian tissue cryopreservation? Ovarian tissue cryopreservation is a reproductive technology that may have an impact in the future. It is currently being used by some cancer patients to restore fertility after chemotherapy. It is a process whereby women have part of the ovarian cortex removed by laproscopy and the tissue is then cryopreserved. The cortex is used because it contains an abundance of primordial follicles and these immature follicles have been found to withstand cryopreservation at a more successful rate compared to later stages in follicle development (Gosden, Mullan, Picton, Yin, Tan, 2002). Cryopreservation allows for storage of healthy primordial follicles, which if not removed, would mature or be affected by chemotherapy. The ovarian cortex can be grafted back onto the original ovary to another site in the body after thawing (Lobo, 2005). After this in vitro fertilization (IVF) procedures can be used to extract eggs and fertilize with sperm, or if transplanted onto the ovary, natural conception has been known to occur (Meirow, Levron, & Eldar-Geva, 2005).
Case studies Cryopreservation of ovarian tissue has been studied for over forty years but with little success, however in the last few years the technology has developed so that it can be offered as a potential option for preserving fertility in patients undergoing chemotherapy or who have other medical conditions affecting fertility (Ovarian tissue cryopreservation, 2005). Patients with cancer are likely to become infertile due to harsh chemotherapy treatment. As an option to preserve fertility, women can freeze their ovarian tissue, and use it for conception after treatment has finished. (Lobo, 2005). There is an increasing amount of cases being reported where a pregnancy, and a subsequent birth has been achieved. One study reported that a live birth by IVF occurred after a patient with Non Hodgkin’s Lymphoma cryopreserved her ovarian tissue (Meirow, Levron, & Elder-Geva 2005). During the cancer treatment, the patient did not menstruate. A transplantation of thawed ovarian tissue into the left ovary, and some of the right ovary, was performed two years after treatment. Menstruation resumed eight months after transplantation, and a second menstrual period after nine months. The patient decided to undergo IVF and a pregnancy was achieved with normal fetal growth and development, and a healthy appearing female was born at 3000g. This shows that there is potential for this technology to restore fertility in cancer patients where they are likely to be rendered infertile from chemotherapy. This option is of particular interest for children with cancer, as other options available to adults such as oocyte and embryo cryopreservation cannot be offered because children are not mature enough and they are likely to not have a partner (Poirot, Vacher-Lavenu, Helardot, Guibert, Brugieres, & Jouannet, 2002). The laproscopy procedure is invasive, requiring two to four operations (Lobo, 2005). IVF is needed to fertilize the ovum, which is also an invasive and costly procedure. There is also a theoretical risk involved for women who have had cancer in the area of the ovary, where malignant cells may be grafted back into the patient after treatment (Meirow, Levron, Eldar-Geva, 2005). A similar case in which a pregnancy was achieved, involved 24-year-old monozygotic twins (Silber et al, 2005). One twin had been infertile after having only three menstrual periods after the age of fourteen; these then ceased and she had not menstruated for 10 years; she also had atrophic ovaries, no follicles and a small uterus. Her twin was fertile and had given birth to three children. The fertile twin donated her left ovary to her sister. One third was transplanted on each of the recipient twin’s ovaries; the remaining third was cryopreserved for the future. Eighty days after transplantation menses resumed, and 176 days after transplantation, a natural conception, with no medical assistance, was achieved. A healthy appearing female was born at 3600g. With both of the above procedures, and others involving ovarian grafting, there has been speculation about whether the conception was due to the transplanted ovarian tissue, or the original ovary. Meirow, Levron and Eldar-Geva (2005) did not rule this out, but claimed that the chemotherapy caused ovarian failure, and ovarian function resumed after transplantation, so it is likely that the transplanted tissue contained the follicles used in conception.
Opinions of others This technology is only in its developmental stages, and should only be considered experimental, as the success of thawing after cryopreservation is not guaranteed. (Ovarian tissue cryopreservation, 2005). There is not enough knowledge yet on the effectiveness of the procedure. An article by Canadian www.eye.net, “The Baby Factory”(Stone, 2000) expresses concerns of the public, and fellow reproductive biologists on ovarian tissue storage and grafting. One surgeon involved in assisted reproductive technologies claimed that the procedure is invasive, the success rate is not high enough and ovaries do not freeze well, therefore the procedure is impractical. This surgeon was arguing this in the view that the procedure may not be restricted to cancer patients. After news spread that one of the pioneers in the ovarian grafting technology, Roger Gosden, performed a successful ovarian graft, a newspaper reported he could ‘reverse menopause’. Many women expressed interest in ovarian storage for the future. The Eye claims that Gosden and colleagues were contacted “by women in their 30s, 40s, 50s and 60s, with and without ovaries, menstrual cycles or previous children. Nearly all of them wanted to go through birth. None of them wanted to go through menopause if they could help it, and none knew what the ovarian graft procedure was for.” These researchers claimed that the procedure cannot be performed on all age groups, and preferably women under 35, however they have made predictions that this procedure will become more routine and increase in demand as the technology increases. Gosden has been accused of actually developing the technology initially for commercial purposes for women delaying having children, instead of for cancer patients. In this report, the executive director of the Toronto Infertility Network, Diane Allen, expresses her concerns over the procedure. She claims that women are not aware that they have a limited reproductive life, and that counseling is needed to honestly inform women of their limited reproductive years. She thinks the procedure is a way of ‘rearranging life’. This report has viewed ovarian grafting as a commercial venture that could potentially restore fertility in many women and it also may relieve some of the effects of menopause. An option for menopause? In patients like the two cases mentioned previously, they both suffered menopausal symptoms due to the atresia of their ovarian follicles. When an ovarian graft was performed, menstrual cycles resumed, and these two women gave birth, one through IVF and one naturally. Women in the future may be able to cryopreserve some ovarian tissue at an early age, and graft it back before menopause occurs, to prolong the onset of menopause. In this way, gonadal steroids can be secreted and delay menopause. However some research has shown that their may only be nine months to three years of endocrine function after replacement (Lobo, 2005), so really the woman is only obtaining an extra three years maximum of normal endocrine function, and menopause will inevitably occur.
Cryopreserve to delay reproduction The concerns of the public and some reproductive biologists it seems, is that soon this procedure is likely to develop so that it can also be used by women who want to delay reproduction. The trend over the last thirty years has seen an increase in the amount of women giving birth in their thirties, due to lifestyle factors and employment opportunities (Australian Bureau of Statistics 2001). As a woman ages, the amount of primordial follicles in her ovarian cortex depletes, so that by menopause there are little or none. The primary oocytes in the follicles are also more likely to undergo nondisjunction and have chromosomal anomalies due to the increased amount of time they have been suspended in meiosis (Lobo, 2005). With this procedure, women will be able store healthy primordial follicles, delay reproduction and establish a career, then when she is ready she can thaw her ovarian tissue, graft it back onto her ovary or other site in the body, then using IVF, conceive a child. Delaying reproduction may become an easy process; however it may not be so easy due to legislation.
Legislation The Human Reproductive Technology Act (1991) allows eligibility for IVF technologies if the female is medically infertile and if infertility is not due to age; and she has to be in a married, de facto or single sex relationship. This means that when the woman wants to thaw her tissue so that it can be used for conception, she will have to be medically infertile. Women who choose this procedure so that the have less risk of chromosomal defects may not necessarily be infertile. Women cannot delay this procedure after their forties, as there is an decreased success rate for IVF in this age group. So women are really only adding another 5-10 years of successful reproductive life with this technology. IVF does not have to be used, as conceptions have occurred after a graft and without IVF, but there is debate about whether this is a result of old or transplanted ovarian tissue. With either procedure, the technique is invasive. Should a woman go through such an invasive procedure so that she can delay reproduction, without any guarantee a child would be conceived in the future? This is another issue that will not really be resolved unless the technology improves and there is an increased success rate for the thawing process after cryopreservation and also an increased guarantee that a healthy birth can be achieved. There is no legislation as yet in Western Australia on the cryopreservation of ovarian tissue and the subsequent grafting techniques. If there is a progression in technology, and more public knowledge, there may be an increase in demand for the procedure. Legislation may ban this technique in the future or it may allow it. Legislation allows for the cryopreservation of oocytes, so it should not be any different for ovarian tissue. Age restrictions may be made for the procedure, as IVF techniques are less successful in older women.
REFERENCES
Australian Bureau of Statistics. (2005). Australian Social Trends 2001: Family - Family Formation: Older Mothers (Catalogue No. 4102.0). Canberra: ABS. Retrieved April 4 2005, from AusStats.
Biotechnology latest news: Special focus Designer Babies (n.d.). Retrieved August 31,2005, from www.tecsoc.org/biotech/focusbabies.htm.
Cookson, C. (2001). Unease over ‘beauty genes’. Davos 2001 - Day One News and Analysis. Retrieved August 31, 2005, from http://specials.ft.com/davos2001/FT3ED70YEIC.html .
Deneen, S. (n.d.). Designer people: The Human Genetic Blueprint Has Been Drafted, Offering Both Perils and Opportunities for the Environment. The Big Question: Are We Changing the Nature of Nature? emagazine.com. Retrieved August 31, 2005, from http://www.emagazine.com/view/?112.
Gosden, R.G., Mullan, J., Picton, H.M., Yin, H., & Tan, S. (2002). Current perspective on primordial follicle cryopreservation and culture for reproductive medicine. Human Reproduction Update, 8(2), 105-110.
Government Response to the Report from the House of Commons Science and Technology Committee. (n.d.). Human Reproductive Technologies and the Law. HM Government. Retrieved August 6, 2005, from www.dh.gov.uk/assetRoot/04/11/78/74/04117874.pdf.
House of Representatives Standing Committee on Legal and Constitutional Affairs, Research Involving Embryos and Prohibition of Human Cloning Bill 2002, (June 2002). Little, M., 1998, ‘Animal cloning and the possibility of cloning humans – Science, law and ethics’, Judicial Review, 57, 61-64.
Lupton, M., 1997, ‘Human cloning—The law’s response’ (1997), Bond Law Review, 9, 123-131. Lobo, R.A. (2005). Potential options for preservation of fertility in women. the new England Journal of Medicine, 353(1), 64-73.
Meirow, D., Levron, J., & Eldar-Geva, T. (2005). Pregnancy after Transplantation of Cryopreserved Ovarian Tissue in a Patient with Ovarian Failure after Chemotherapy. The New England Journal of Medicine, 353(3), 318-321.
Ovarian tissue cryopreservation. Retrieved September 9, 2005 from http://www.conceptfert.com.au/facts/ovarian_tissue_cryopreservation.h tm Poirot, C., Vacher-Lavenu, M., Helardot, P., Guibert, J., Brugieres, L., & Jouannet, P. (2002). Human ovarian tissue cryopreservation: indications and feasibility. Human Reproduction 17 (6), 1447-1452.
Preimplantation Genetic Testing (n.d.). Retrieved August 6, 2005, from www.conceptfert.com.au.
Reproductive Technology Council (2004). Retrieved August 6, 2005, from www.rtc.org.au/reports/docs/AR2004.pdf.
Reproductive Technology: Legislation around Australia (n.d.). Retrieved August 6, 2005, from www.dh.sa.gov.au/reproductive-technology/other.asp.
Science screens out defective genes. (2000, November 18). BBC News: Health. Retrieved August 31, 2005, from http://news.bbc.co.uk/1/hi/health/1027076.stm.
Screening picks ‘best chance’ embryos. (2000, October 23). BBC News: Health. Retrieved August 31, 2005, from http://news.bbc.co.uk/1/hi/health/980277.stm.
Silber, S.J., Lenahan, K.M., Levine, D.J., Pineda, J.A., Gorman, K.S., Friez, M.J., Crawford, E.C., & Gosden, R.G. (2005). Ovarian Transplantation between Monozygotic Twins Discordant for Premature Ovarian Failure. The New England Journal of Medicine, 353(1), 58-63.
Stone, K. (2000). The baby factory: A tale of hype, hope and high-tech fertility. Retrieved September 7, 2005, from http://www.eye.net/eye/issue/print.asp? issue_02.17.00/news/baby.html