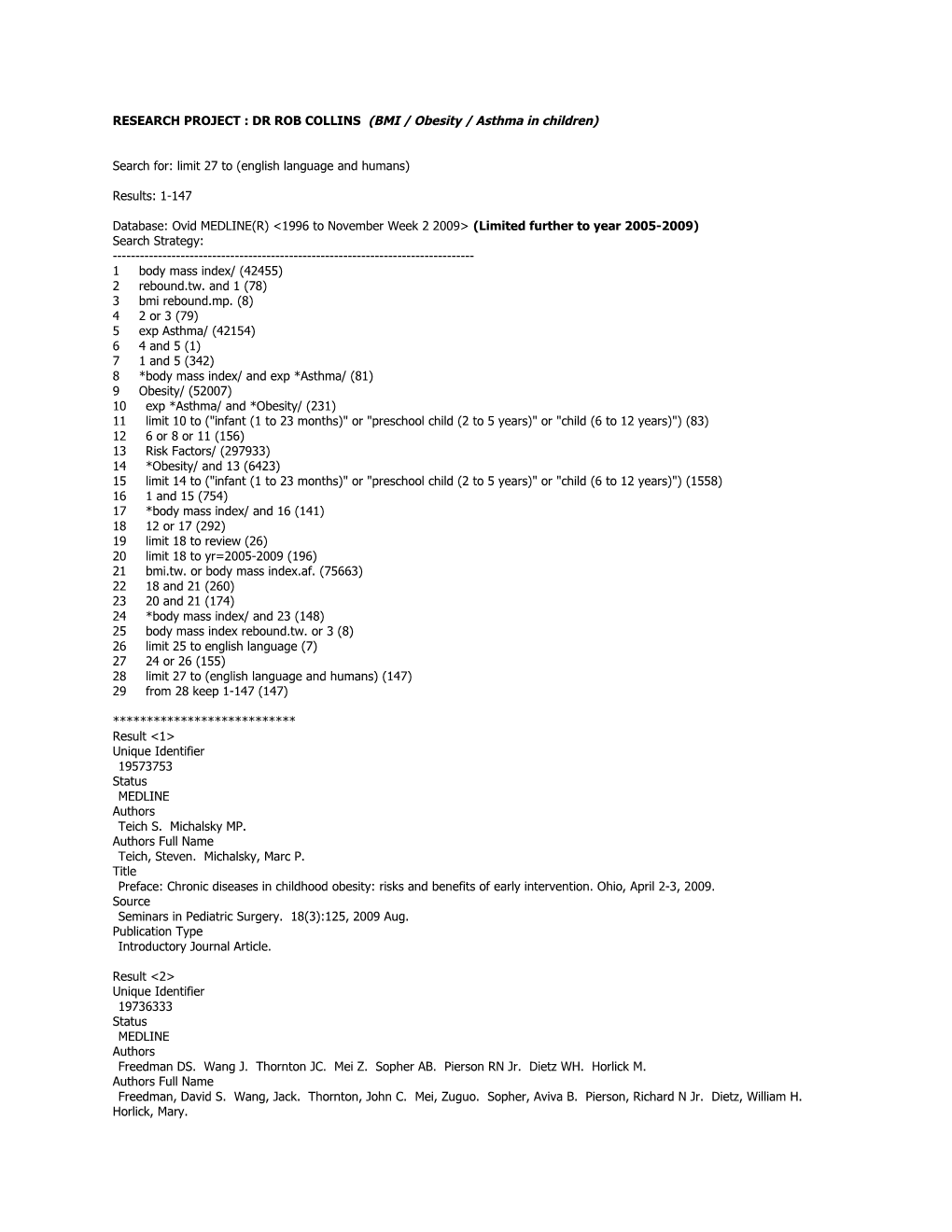
RESEARCH PROJECT : DR ROB COLLINS (BMI / Obesity / Asthma in children)
Search for: limit 27 to (english language and humans)
Results: 1-147
Database: Ovid MEDLINE(R) <1996 to November Week 2 2009> (Limited further to year 2005-2009) Search Strategy: ------1 body mass index/ (42455) 2 rebound.tw. and 1 (78) 3 bmi rebound.mp. (8) 4 2 or 3 (79) 5 exp Asthma/ (42154) 6 4 and 5 (1) 7 1 and 5 (342) 8 *body mass index/ and exp *Asthma/ (81) 9 Obesity/ (52007) 10 exp *Asthma/ and *Obesity/ (231) 11 limit 10 to ("infant (1 to 23 months)" or "preschool child (2 to 5 years)" or "child (6 to 12 years)") (83) 12 6 or 8 or 11 (156) 13 Risk Factors/ (297933) 14 *Obesity/ and 13 (6423) 15 limit 14 to ("infant (1 to 23 months)" or "preschool child (2 to 5 years)" or "child (6 to 12 years)") (1558) 16 1 and 15 (754) 17 *body mass index/ and 16 (141) 18 12 or 17 (292) 19 limit 18 to review (26) 20 limit 18 to yr=2005-2009 (196) 21 bmi.tw. or body mass index.af. (75663) 22 18 and 21 (260) 23 20 and 21 (174) 24 *body mass index/ and 23 (148) 25 body mass index rebound.tw. or 3 (8) 26 limit 25 to english language (7) 27 24 or 26 (155) 28 limit 27 to (english language and humans) (147) 29 from 28 keep 1-147 (147)
*************************** Result <1> Unique Identifier 19573753 Status MEDLINE Authors Teich S. Michalsky MP. Authors Full Name Teich, Steven. Michalsky, Marc P. Title Preface: Chronic diseases in childhood obesity: risks and benefits of early intervention. Ohio, April 2-3, 2009. Source Seminars in Pediatric Surgery. 18(3):125, 2009 Aug. Publication Type Introductory Journal Article.
Result <2> Unique Identifier 19736333 Status MEDLINE Authors Freedman DS. Wang J. Thornton JC. Mei Z. Sopher AB. Pierson RN Jr. Dietz WH. Horlick M. Authors Full Name Freedman, David S. Wang, Jack. Thornton, John C. Mei, Zuguo. Sopher, Aviva B. Pierson, Richard N Jr. Dietz, William H. Horlick, Mary. Institution Division of Nutrition and Physical Activity, Centers for Disease Control and Prevention, 4770 Buford Highway, Atlanta, GA 30341- 3717, USA. [email protected] Title Classification of body fatness by body mass index-for-age categories among children. Source Archives of Pediatrics & Adolescent Medicine. 163(9):805-11, 2009 Sep. Abstract OBJECTIVE: To examine the ability of various body mass index (BMI)-for-age categories, including the Centers for Disease Control and Prevention's 85th to 94th percentiles, to correctly classify the body fatness of children and adolescents. DESIGN: Cross- sectional. SETTING: The New York Obesity Research Center at St Luke's-Roosevelt Hospital from 1995 to 2000. PARTICIPANTS: Healthy 5- to 18-year-old children and adolescents (N = 1196) were recruited in the New York City area through newspaper notices, announcements at schools and activity centers, and word of mouth. MAIN OUTCOME MEASURES: Percent body fat as determined by dual-energy x-ray absorptiometry. Body fatness cutoffs were chosen so that the number of children in each category (normal, moderate, and elevated fatness) would equal the number of children in the corresponding BMI-for-age category (<85th percentile, 85th-94th percentile, and > or =95th percentile, respectively). RESULTS: About 77% of the children who had! a BMI for age at or above the 95th percentile had an elevated body fatness, but levels of body fatness among children who had a BMI for age between the 85th and 94th percentiles (n = 200) were more variable; about one-half of these children had a moderate level of body fatness, but 30% had a normal body fatness and 20% had an elevated body fatness. The prevalence of normal levels of body fatness among these 200 children was highest among black children (50%) and among those within the 85th to 89th percentiles of BMI for age (40%). CONCLUSION: Body mass index is an appropriate screening test to identify children who should have further evaluation and follow-up, but it is not diagnostic of level of adiposity. Publication Type Journal Article. Research Support, N.I.H., Extramural.
Result <3> Unique Identifier 19640961 Status MEDLINE Authors Corvalan C. Uauy R. Stein AD. Kain J. Martorell R. Authors Full Name Corvalan, Camila. Uauy, Ricardo. Stein, Aryeh D. Kain, Juliana. Martorell, Reynaldo. Institution Emory University, Atlanta, GA, USA. [email protected] Title Effect of growth on cardiometabolic status at 4 y of age. Source American Journal of Clinical Nutrition. 90(3):547-55, 2009 Sep. Abstract BACKGROUND: Cardiovascular disease (CVD) risks are increasingly being diagnosed in children and track into adulthood. Growth is associated with CVD risk in adulthood; however, its contribution to CVD risks in children facing the obesity epidemic is unclear. OBJECTIVE: The objective was to assess relations between growth from age 0 to 4 y and CVD status at 4 y in 323 Chilean children with normal birth weight. DESIGN: From health records we obtained weight and height every 6 mo from age 0 to 3 y and calculated body mass index (BMI; weight/height(2)). At age 4 y, we measured height, waist circumference, insulin, glucose, and plasma lipids; infant feeding information was provided by the mothers. Outcomes were metabolic score (waist-to-height ratio + glucose + insulin + triglycerides - HDL-cholesterol z scores/5), total cholesterol (TC):HDL cholesterol, and homeostasis model of assessment of insulin resistance. RESULTS: At 4 y, the prevalence of obesity was 13%. Changes in BMI,! particularly from 6 to 24 mo, predicted a higher metabolic score (standardized regression coefficient = 0.29; 95% CI: 0.16, 0.42) but were unrelated to homeostasis model of assessment of insulin resistance and TC:HDL cholesterol. Height changes were not associated with CVD risks at the age of 4 y. Mode of infant feeding was unrelated to CVD status at 4 y; however, in children who were exclusively breastfed at 4 mo, an increase in BMI from 0 to 6 mo was positively associated with TC:HDL cholesterol at 4 y (standardized regression coefficient = 0.24; 95% CI: -0.02, 0.50), whereas in children who were partially or nonbreastfed at 4 mo, it was negatively associated with TC:HDL cholesterol at 4 y (standardized regression coefficient = -0.30; 95% CI: -0.52, -0.08). CONCLUSION: In children with normal birth weight and a high prevalence of obesity at 4 y, changes in BMI after 6 mo predicted a higher overall CVD risk at 4 y. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <4> Unique Identifier 19615731 Status MEDLINE Authors Clerisme-Beaty EM. Karam S. Rand C. Patino CM. Bilderback A. Riekert KA. Okelo SO. Diette GB. Authors Full Name Clerisme-Beaty, Emmanuelle M. Karam, Sabine. Rand, Cynthia. Patino, Cecilia M. Bilderback, Andrew. Riekert, Kristin A. Okelo, Sande O. Diette, Gregory B. Institution Department of Medicine, Johns Hopkins University, Baltimore, MD, USA. Title Does higher body mass index contribute to worse asthma control in an urban population?. Source Journal of Allergy & Clinical Immunology. 124(2):207-12, 2009 Aug. Other ID Source: NLM. NIHMS123143 [Available on 08/01/10] Source: NLM. PMC2733240 [Available on 08/01/10] Abstract BACKGROUND: Epidemiologic findings support a positive association between asthma and obesity. OBJECTIVE: Determine whether obesity or increasing level of body mass index (BMI) are associated with worse asthma control in an ethnically diverse urban population. METHODS: Cross-sectional assessment of asthma control was performed in patients with asthma recruited from primary care offices by using 4 different validated asthma control questionnaires: the Asthma Control and Communication Instrument (ACCI), the Asthma Control Test (ACT), the Asthma Control Questionnaire (ACQ), and the Asthma Therapy Assessment Questionnaire (ATAQ). Multiple linear regression analysis was performed to evaluate the association between obesity and increasing BMI level and asthma control. RESULTS: Of 292 subjects with a mean age of 47 years, the majority were women (82%) and African American (67%). There was a high prevalence of obesity with 63%, with only 15% normal weight. The mean score from all 4! questionnaires showed an average suboptimal asthma control (mean score/maximum possible score): ACCI (8.3/19), ACT (15.4/25), ACQ (2.1/6), and ATAQ (1.3/4). Regression analysis showed no association between obesity or increasing BMI level and asthma control using all 4 questionnaires. This finding persisted even after adjusting for FEV(1), smoking status, race, sex, selected comorbid illnesses, and long-term asthma controller use. CONCLUSION: Using 4 validated asthma control questionnaires, we failed to find an association between obesity and asthma control in an urban population with asthma. Weight loss may not be an appropriate strategy to improve asthma control in this population. Publication Type Journal Article. Research Support, N.I.H., Extramural.
Result <5> Unique Identifier 19123432 Status MEDLINE Authors Delgado J. Barranco P. Quirce S. Authors Full Name Delgado, J. Barranco, P. Quirce, S. Institution Allergy Service, University Hospital Virgen Macarena, Sevilla, Spain. [email protected] Title Obesity and asthma. [Review] [51 refs] Source Journal of Investigational Allergology & Clinical Immunology. 18(6):420-5, 2008. Abstract Asthma and obesity have a considerable impact on public health and their prevalence has increased in recent years. Numerous studies have linked these disorders. Most prospective studies show that obesity is a risk factor for asthma and have found a positive correlation between baseline body mass index and the subsequent development of asthma. Furthermore, several studies suggest that whereas weight gain increases the risk of asthma, weight loss improves the course of the illness. Different factors could explain this association. Obesity is capable of reducing pulmonary compliance, lung volumes, and the diameter of peripheral respiratory airways as well as affecting the volume of blood in the lungs and the ventilation-perfusion relationship. Furthermore, the increase in the normal functioning of adipose tissue in obese subjects leads to a systemic proinflammatory state, which produces a rise in the serum concentrations of several cytokines, the soluble fractions of their re! ceptors, and chemokines. Many of these mediators are synthesized and secreted by cells from adipose tissue and receive the generic name of adipokines, including IL-6, IL-10, eotaxin, tumor necrosis factor-alpha, transforming growth factors-beta1, C- reactive protein, leptin, and adiponectin. Finally, specific regions of the human genome related to both asthma and obesity have been identified. Most studies point out that obesity is capable of increasing the prevalence and incidence of asthma, although this effect appears to be modest. The treatment of obese asthmatics must include a weight control program. [References: 51] Publication Type Journal Article. Review.
Result <6> Unique Identifier 19183310 Status MEDLINE Authors Viner RM. Hindmarsh PC. Taylor B. Cole TJ. Authors Full Name Viner, R M. Hindmarsh, P C. Taylor, B. Cole, T J. Institution Children and Young People's Diabetes Service, University College London, London, UK. [email protected] Title Childhood body mass index (BMI), breastfeeding and risk of Type 1 diabetes: findings from a longitudinal national birth cohort. Source Diabetic Medicine. 25(9):1056-61, 2008 Sep. Abstract AIMS: To perform a longitudinal analysis of the association between childhood body mass index (BMI) and later risk of Type 1 diabetes, controlling for socio-economic status, birthweight, height in early and late childhood, breastfeeding history and pubertal status. METHODS: Analysis of the 1970 British Birth Cohort, followed up at age 5, 10 and 30 years (n = 11,261). Data were available on birthweight, breastfeeding; height, weight, pubertal status, socio-economic status at age 10 years; self-report data on history of diabetes (type, age at onset) at age 30 years. Cox proportional hazards models were used to examine relations of childhood growth, socio-economic status and breastfeeding history to the incidence of Type 1 diabetes between 10 and 30 years of age. RESULTS: Sixty-one subjects (0.5%) reported Type 1 diabetes at 30 years of age; 47 (77%) reported onset >or= age 10 years. Higher BMI z-score at 10 years predicted higher risk of subsequent Type 1 diabetes (hazard ra! tio 1.8, 95% confidence interval 1.2 to 2.8, P = 0.01) when adjusted for birthweight, pubertal status, breastfeeding history and socio-economic status. Repeating the model for childhood obesity, the hazard ratio was 3.1 (1.0, 9.3; P = 0.05). Birthweight, breastfeeding, height growth and pubertal timing were not associated with incidence of Type 1 diabetes. CONCLUSIONS: Higher BMI in childhood independently increased the risk of later Type 1 diabetes, supporting suggestions that obesity may provide a link between Type 1 and Type 2 diabetes. This supports observations of a rise in Type 1 diabetes prevalence. Reduction in childhood obesity may reduce the incidence of Type 1 as well as Type 2 diabetes. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <7> Unique Identifier 19558003 Status MEDLINE Authors Dogra S. Baker J. Ardern CI. Authors Full Name Dogra, Shilpa. Baker, Joseph. Ardern, Chris I. Institution Lifespan Health and Performance Laboratory, York University, Toronto, Ontario, Canada. [email protected] Title The role of physical activity and body mass index in the health care use of adults with asthma. Source Annals of Allergy, Asthma, & Immunology. 102(6):462-8, 2009 Jun. Abstract BACKGROUND: Health care use in patients with asthma is affected by many factors, including sex and ethnicity. The role of physical activity (PA) and body mass index (BMI) (calculated as weight in kilograms divided by height in meters squared) in this relationship is unknown. OBJECTIVE: To determine the role of PA and BMI in the health care use of patients with asthma. METHODS: A sample of adults with asthma (n=6,835) and without asthma (n=78,051) from cycle 3.1 of the Canadian Community Health Survey was identified. Health care use was self-reported as overnight hospital stays (yes or no), length of overnight hospital stay (<4 or > or =4 nights), and physician consultations (<3 or > or =3). Self-reported physical activities were used to derive total energy expenditure and to classify participants as active (>3.0 kcal/kg of body weight per day), moderately active (1.5-3.0 kcal/kg of body weight per day), and inactive (<1.5 kcal/kg of body weight per day). The BMI was catego! rized as normal weight (18.5-24.9), overweight (25.0-29.9), and obese (30.0-59.9). RESULTS: Adjusted logistic regression models revealed that patients with asthma were more likely to have an overnight hospital stay (odds ratio [OR], 2.25; 95% confidence interval [CI], 1.95-2.60), 4 or more overnight hospital stays (OR, 1.48; 95% CI, 1.12-1.96), and 3 or more physician consultations (OR, 2.43; 95% CI, 2.18-2.71) compared with patients without asthma (OR, 1.00). Inactive patients with asthma were more likely to have an overnight hospital stay (OR, 1.68; 95% CI, 1.31-2.16) and 3 or more physician consultations (OR, 1.23; 95% CI, 1.04- 1.46) than active patients with asthma (OR, 1.00). Inactive/obese patients with asthma were 2.35 (95% CI, 1.69-3.27) times more likely to have an overnight hospital stay and 2.76 (95% CI, 2.11-3.60) times more likely to have 3 or more physician consultations than active/normal weight patients with asthma (OR, 1.00). CONCLUSIONS: Higher PA levels a! re associated with lower health care use in individuals with and witho ut asthma. In those with asthma, PA was a more important factor in overnight hospital stays than BMI, whereas both BMI and PA were important determinants of physician consultations. Publication Type Journal Article.
Result <8> Unique Identifier 19584884 Status MEDLINE Authors Nonnemaker JM. Morgan-Lopez AA. Pais JM. Finkelstein EA. Authors Full Name Nonnemaker, James M. Morgan-Lopez, Antonio A. Pais, Joanne M. Finkelstein, Eric A. Institution RTI International, Research Triangle Park, North Carolina, USA. [email protected] Title Youth BMI trajectories: evidence from the NLSY97. Source Obesity. 17(6):1274-80, 2009 Jun. Abstract We examined heterogeneity in BMI trajectory classes among youth and variables that may be associated with trajectory class membership. We used data from seven rounds (1997-2003) of the 1997 National Longitudinal Survey of Youth (NLSY97), a nationally representative, longitudinal survey of people born between 1980 and 1984 who were living in the United States in 1997. The analyses were based on an accelerated longitudinal design. General growth mixture modeling implemented in Mplus (version 4.1) was used to identify subtypes of youth BMI growth trajectories over time. Four distinct youth BMI trajectories were identified. Class 1 includes youth at high risk for becoming obese by young adulthood (at age 12 and 23, approximately 67 and 90%, respectively, are classified as obese, and almost 72% will have had a BMI>or=40 at some time during this developmental period). Class 2 includes youth at moderate-to-high risk (at age 12 and 23, approximately 55 and 68%, respectively, are c! lassified as obese). Class 3 includes youth at low-to-moderate risk (i.e., at age 12 and 23, approximately 8 and 27%, respectively, are classified as obese). Class 4 includes youth at low risk (few of these youth are obese at any age during this developmental period). These results highlight the importance of considering heterogeneity in BMI growth among youth and early interventions among those most at risk of the adverse health consequences of excess weight. Publication Type Journal Article. Research Support, U.S. Gov't, P.H.S..
Result <9> Unique Identifier 19197261 Status MEDLINE Authors Lim S. Zoellner JM. Lee JM. Burt BA. Sandretto AM. Sohn W. Ismail AI. Lepkowski JM. Authors Full Name Lim, Sungwoo. Zoellner, Jamie M. Lee, Joyce M. Burt, Brian A. Sandretto, Anita M. Sohn, Woosung. Ismail, Amid I. Lepkowski, James M. Institution Bureau of Epidemiology Services, Division of Epidemiology, New York City Department of Health and Mental Hygiene, New York, New York, USA. [email protected] Title Obesity and sugar-sweetened beverages in African-American preschool children: a longitudinal study. Source Obesity. 17(6):1262-8, 2009 Jun. Abstract A representative sample of 365 low-income African-American preschool children aged 3-5 years was studied to determine the association between sugar-sweetened beverage consumption (soda, fruit drinks, and both combined) and overweight and obesity. Children were examined at a dental clinic in 2002-2003 and again after 2 years. Dietary information was collected using the Block Kids Food Frequency Questionnaire. A BMI score was computed from recorded height and weight. Overweight and obesity were defined by national reference age-sex specific BMI: those with an age-sex specific BMI>or=85th, but <95th percentile as overweight and those with BMI>or=95th age-sex specific percentile as obese. The prevalence of overweight was 12.9% in baseline, and increased to 18.7% after 2 years. The prevalence of obesity increased from 10.3 to 20.4% during the same period. Baseline intake of soda and all sugar-sweetened beverages were positively associated with baseline BMI z-scores. After adjus! ting for covariates, additional intake of fruit drinks and all sugar-sweetened beverages at baseline showed significantly higher odds of incidence of overweight over 2 years. Among a longitudinal cohort of African-American preschool children, high consumption of sugar-sweetened beverages was significantly associated with an increased risk for obesity. Publication Type Journal Article. Research Support, N.I.H., Extramural. Research Support, Non-U.S. Gov't.
Result <10> Unique Identifier 19546463 Status MEDLINE Authors Lyn R. McCarty F. Authors Full Name Lyn, Rodney. McCarty, Frances. Title Interpret results with caution.[comment]. Comments Comment on: CMAJ. 2009 Mar 31;180(7):719-26; PMID: 19332753 Source CMAJ Canadian Medical Association Journal. 180(13):1330; author reply 1330, 2009 Jun 23. Other ID Source: NLM. PMC2696531 Publication Type Comment. Letter.
Result <11> Unique Identifier 18674392 Status MEDLINE Authors Nitzan Kaluski D. Demem Mazengia G. Shimony T. Goldsmith R. Berry EM. Authors Full Name Nitzan Kaluski, Dorit. Demem Mazengia, Getachew. Shimony, Tal. Goldsmith, Rebecca. Berry, Elliot M. Institution Department of Epidemiology and Preventive Medicine, Sackler Faculty of Medicine, Tel-Aviv University, Tel Aviv, Israel. Title Prevalence and determinants of physical activity and lifestyle in relation to obesity among schoolchildren in Israel. Source Public Health Nutrition. 12(6):774-82, 2009 Jun. Abstract OBJECTIVE: To describe the relationships between physical activity, lifestyle determinants and obesity in adolescent Israeli schoolchildren.Design and settingCross-sectional survey. SUBJECTS: The MABAT Youth Survey was a nationally representative, school-based study of youth in grades 7 to 12 (ages 11-19 years). METHODS: Self-administered questionnaires assessed health behaviours and anthropometric indices were measured. Logistic regression analysis was used to examine the associations between obesity, physical activity, socio-economic status and other lifestyle habits. One-way ANOVA was used to determine mean physical activity levels (MET values) by BMI categories. RESULTS: The prevalence of overweight was 13-15 % and of obesity 4-9 % depending on gender and ethnicity, and was higher among the non-Jewish sectors. Thirty-six per cent and 57 % of Jewish girls and boys, and 40 % and 58 % of non-Jewish girls and boys, respectively, were optimally active. Boys from low socio-e! conomic schools and those who slept for less than 6 h at night were less active. Girls from middle school were found to be 53 % more optimally physically active among Jews, and 89 % more among non-Jews, compared with girls from high school (P = 0.001); girls with less educated parents were also less physically active. No clear relationship was found between the level of obesity and physical activity. CONCLUSIONS: Physical inactivity was strongly related to gender, age, social status, sleeping habits, hookah smoking, and parental educational status. Education and intervention programmes should focus on these risk factors. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <12> Unique Identifier 19576566 Status MEDLINE Authors Murphy A. Tantisira KG. Soto-Quiros ME. Avila L. Klanderman BJ. Lake S. Weiss ST. Celedon JC. Authors Full Name Murphy, Amy. Tantisira, Kelan G. Soto-Quiros, Manuel E. Avila, Lydiana. Klanderman, Barbara J. Lake, Stephen. Weiss, Scott T. Celedon, Juan C. Institution Channing Laboratory, Brigham and Women's Hospital, Boston, MA 02115, USA. Title PRKCA: a positional candidate gene for body mass index and asthma. Source American Journal of Human Genetics. 85(1):87-96, 2009 Jul. Abstract Asthma incidence and prevalence are higher in obese individuals. A potential mechanistic basis for this relationship is pleiotropy. We hypothesized that significant linkage and candidate-gene association would be found for body mass index (BMI) in a population ascertained on asthma affection status. Linkage analysis for BMI was performed on 657 subjects in eight Costa Rican families enrolled in a study of asthma. Family-based association studies were conducted for BMI with SNPs within a positional candidate gene, PRKCA. SNPs within PRKCA were also tested for association with asthma. Association studies were conducted in 415 Costa Rican parent-child trios and 493 trios participating in the Childhood Asthma Management Program (CAMP). Although only modest evidence of linkage for BMI was obtained for the whole cohort, significant linkage was noted for BMI in females on chromosome 17q (peak LOD = 3.39). Four SNPs in a candidate gene in this region (PRKCA) had unadjusted associa! tion p values < 0.05 for BMI in both cohorts, with the joint p value for two SNPs remaining significant after adjustment for multiple comparisons (rs228883 and rs1005651, joint p values = 9.5 x 10(-)(5) and 5.6 x 10(-)(5)). Similarly, eight SNPs had unadjusted association p values < 0.05 for asthma in both populations, with one SNP remaining significant after adjustment for multiple comparisons (rs11079657, joint p value = 2.6 x 10(-)(5)). PRKCA is a pleiotropic locus that is associated with both BMI and asthma and that has been identified via linkage analysis of BMI in a population ascertained on asthma. Publication Type Journal Article. Research Support, N.I.H., Extramural.
Result <13> Unique Identifier 19490650 Status MEDLINE Authors Nishimura R. Sano H. Matsudaira T. Morimoto A. Miyashita Y. Shirasawa T. Kokaze A. Tajima N. Authors Full Name Nishimura, Rimei. Sano, Hironari. Matsudaira, Toru. Morimoto, Aya. Miyashita, Yumi. Shirasawa, Takako. Kokaze, Akatsuki. Tajima, Naoko. Institution Division of Diabetes, Metabolism and Endocrinology, Department of Internal Medicine, Jikei University School of Medicine, Tokyo, Japan. [email protected] Title Changes in body mass index, leptin and adiponectin in Japanese children during a three-year follow-up period: a population-based cohort study. Source Cardiovascular Diabetology. 8:30, 2009. Other ID Source: NLM. PMC2701411 Abstract OBJECTIVE: The study examined changes in and relationship between body mass index (BMI), leptin and adiponectin levels over a 3-year period in a pediatric population-based cohort. STUDY DESIGN: A 3-year prospective cohort study of 268 boys and 251 girls aged 9-10 in Ina, Saitama, Japan. RESULTS: Median body mass index (BMI) significantly increased from baseline (age 9-10) to follow up (age 12-13) in boys from 17.1 to 18.3 kg/m2 (P < 0.001) and in girls from 16.5 to 18.5 kg/m2 (P < 0.001), respectively. Adiponectin values significantly decreased from baseline to follow up in boys (13.5 to 8.9 microg/ml, respectively) (P < 0.001) and in girls (12.4 to 9.5 microg/ml, respectively) (P < 0.001). Leptin values at follow up significantly decreased from baseline in boys (4.9 to 2.3 ng/dl, respectively) (P < 0.001) and also in girls (5.3 to 5.1 ng/dl, respectively) (P = 0.049). A relatively strong correlation was seen in BMI (Spearman's correlation coefficient, r = 0.864, P < 0.001! in boys; r = 0.873, P < 0.001 in girls), adiponectin (r = 0.705, P < 0.001 in boys; r = 0.695, P < 0.001 in girls), and leptin (r = 0.449, P < 0.001 in boys; r = 0.610, P < 0.001 in girls) before and after the three-year period. The ratio of follow up to baseline BMI was negatively correlated with that for adiponectin (r = -0.224, P < 0.001 in boys; r = -0.165, P = 0.001 in girls) and positively correlated with that for leptin (r = 0.518, P < 0.001 in boys; r = 0.609, P < 0.001 in girls). CONCLUSION: This study demonstrated that baseline adiponectin, leptin and BMI values measured at ages 9-10 correlated with those measured three years later. However, adiponectin values decreased and leptin values increased in those subjects whose BMI increased during over this period. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <14> Unique Identifier 19501235 Status MEDLINE Authors Sutherland ER. Lehman EB. Teodorescu M. Wechsler ME. National Heart, Lung, and Blood Institute's Asthma Clinical Research Network. Authors Full Name Sutherland, E Rand. Lehman, Erik B. Teodorescu, Mihaela. Wechsler, Michael E. National Heart, Lung, and Blood Institute's Asthma Clinical Research Network. Institution National Jewish Health, Denver, CO 80206, USA. [email protected] Title Body mass index and phenotype in subjects with mild-to-moderate persistent asthma. Source Journal of Allergy & Clinical Immunology. 123(6):1328-34.e1, 2009 Jun. Abstract BACKGROUND: Although obesity has been hypothesized to worsen asthma, data from studies of subjects with well-characterized asthma are lacking. OBJECTIVE: We sought to evaluate the relationship between body mass index (BMI), asthma impairment, and response to therapy. METHODS: BMI (in kilograms per meter squared) and asthma phenotypic and treatment response data were extracted from Asthma Clinical Research Network studies. The cross-sectional relationship between BMI and asthma impairment was analyzed, as was the longitudinal relationship between BMI and response to asthma controller therapies. RESULTS: One thousand two hundred sixty-five subjects with mild-to-moderate persistent asthma were evaluated. Analyses of lean versus overweight/obese asthmatic subjects demonstrated small differences in FEV1 (3.05 vs 2.91 L, P = .001), FEV1/forced vital capacity ratio (mean, 83.5% vs 82.4%; P = .01), rescue albuterol use (1.1 vs 1.2 puffs per day, P = .03), and asthma-related qualit! y of life (5.77 vs 5.59, P = .0004). Overweight/obese asthmatic subjects demonstrated a smaller improvement in exhaled nitric oxide levels with inhaled corticosteroid (ICS) treatment than did lean asthmatic subjects (3.6 vs 6.5 ppb, P = .04). With ICS/long- acting beta-agonist treatment, overweight/obese asthmatic subjects demonstrated smaller improvements in lung function than lean asthmatic subjects, with an 80 mL (P = .04) and 1.7% (P = .02) lesser improvement in FEV1 and FEV1/forced vital capacity ratio, respectively. Significant differences in therapeutic response to leukotriene modifiers between BMI categories were not observed. CONCLUSIONS: Increased BMI is not associated with clinically significant worsening of impairment in subjects with mild-to- moderate persistent asthma. There is a modest association between increased BMI and reduced therapeutic effect of ICS-containing regimens in this patient population. Prospective studies evaluating the effect of being overwei! ght or obese on treatment response in asthma are warranted. Publication Type Journal Article. Research Support, N.I.H., Extramural.
Result <15> Unique Identifier 19462676 Status MEDLINE Authors Scheffler C. Schuler G. Authors Full Name Scheffler, Christiane. Schuler, Grit. Institution Institute of Biochemistry and Biology, Human Biology, Potsdam University, Germany. [email protected] Title Analysis of BMI of preschool children--results of longitudinal studies. Source Anthropologischer Anzeiger. 67(1):53-63, 2009 Mar. Abstract Exceeding weight gain in childhood is a prevailing issue in industrialised countries, such as in Germany. The aim of this study was to detect a critical age for exceeding weight gain. It is assumed that especially in the early years of life, the years of nursery school age, the individual development of weight is fundamental for the prediction of obesity. The data of 638 children (324 boys and 314 girls) and the data of additional 1390 children of a preceding longitudinal study were analysed. The results show that overweight newborns are not at higher risk of becoming overweight children later, in the first place. But the results identify a high risk of becoming overweight for children 4.5-years-old through a BMI rebound. In addition, this comparably earlier BMI rebound is linked with an increasing percentage of body fat. This leads to the assumption, that a comparably early BMI rebound is remarkably atypical for healthy child development. The results are also interrelated! with the test person's sex. Endangered girls are of pyknomorphic body type. In contrast, the boys' results are independent of the body type. Obesity of boys therefore is strongly assumed to be caused by environmental factors. Publication Type Journal Article.
Result <16> Unique Identifier 18798801 Status MEDLINE Authors Van Gysel D. Govaere E. Verhamme K. Doli E. De Baets F. Authors Full Name Van Gysel, D. Govaere, E. Verhamme, K. Doli, E. De Baets, F. Institution Department of Pediatrics, O.L. Vrouw Hospital, Aalst B-9300, Belgium. Title Body mass index in Belgian schoolchildren and its relationship with sensitization and allergic symptoms. Source Pediatric Allergy & Immunology. 20(3):246-53, 2009 May. Abstract Results of studies of the influence of body mass index (BMI) on the allergic status are controversial. As a part of the Aalst Allergy Study, we assessed the prevalence of the different BMI categories (underweight, normal weight, overweight, and obesity) and a possible association between BMI and atopy in 1576 unselected Belgian schoolchildren, aged from 3.4 to 14.8 yr. BMI was used to determine weight status. Skin prick testing with the most common aeroallergens was performed. A parental questionnaire documented data on respiratory and allergic disorders, demographic characteristics and other potential risk factors for sensitization. Among the total children, 4.1% of the children were underweight, 14.5% were overweight, and 7.4% were obese. More girls than boys were overweight (p = 0.015). In the group of children older than 12 yr, we found more overweight (p = 0.03) and obese (p = 0.004) girls, and more obese boys (p = 0.004) than in the younger age groups. In contrast wi! th reports in the literature, an increased prevalence of allergic sensitization in underweight girls only [adjusted odd ratio (OR(adj)) = 2.9, 95% confidence interval (CI): 1.3-6.4] was documented. A strong association between obesity and exercise-induced respiratory symptoms was found in both boys (OR(adj) = 14.5, 95% CI: 2.9-73.3) and girls (OR(adj) = 4.9, 95% CI: 1.3-17.4). No correlations with allergic respiratory symptoms, eczema, or rhinoconjunctivitis could be documented. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <17> Unique Identifier 18979276 Status MEDLINE Authors Grech V. Farrugia Sant'Angelo V. Authors Full Name Grech, Victor. Farrugia Sant'Angelo, Victoria. Institution Paediatric Department, Mater Dei Hospital, Malta. [email protected] Title Body mass index estimation in a school-entry aged cohort in Malta. Source International Journal of Pediatric Obesity. 4(2):126-8, 2009. Abstract This study measured body mass index (BMI) in a national cohort of school-entry children in Malta (04/2007, n=3461). By International Obesity Task Force criteria, over a quarter are overweight/obese. CDC criteria classify one-third as overweight/obese. BMIs were higher in the less affluent south of the island, especially in the Grand Harbour area. Analysis by school showed differences in boys only with lowest BMIs in private schools, followed by subsidized church schools and by free State schools. These differences are attributed to a lower level of education with regard to the consequences of obesity in the less affluent southern part of the island, along with lifestyles adopted in this area. We estimate that obesity will eventually cost Malta 70,000,000 euros/annum and therefore hope that this study will serve as a catalyst for further population-based BMI estimations and for an intensive effort to curtail this chronic disease. Publication Type Journal Article.
Result <18> Unique Identifier 19242839 Status MEDLINE Authors Krukowski RA. West DS. Authors Full Name Krukowski, Rebecca A. West, Delia Smith. Title Response to the article, "The risks of a quick fix: a case against mandatory body mass index reporting laws".[comment]. Comments Comment on: Eat Disord. 2008 Jan-Feb;16(1):2-13; PMID: 18175229 Source Brunner-Mazel Eating Disorders Monograph Series. 17(2):103-6; author reply 107-8, 2009 Mar-Apr. Publication Type Comment. Letter.
Result <19> Unique Identifier 19148130 Status MEDLINE Authors Mamun AA. O'Callaghan MJ. Cramb SM. Najman JM. Williams GM. Bor W. Authors Full Name Mamun, Abdullah A. O'Callaghan, Michael J. Cramb, Susanna M. Najman, Jake M. Williams, Gail M. Bor, William. Institution Longitudinal Studies Unit, School of Population Health, University of Queensland, Queensland, Australia. [email protected] Title Childhood behavioral problems predict young adults' BMI and obesity: evidence from a birth cohort study. Source Obesity. 17(4):761-6, 2009 Apr. Abstract We examined whether behavioral problems in childhood and adolescence are associated with young adults' BMI and obesity, and tested whether childhood behavioral problems have a greater impact on young adults' obesity than adolescent behavioral problems. The data were from the Mater-University of Queensland Study of Pregnancy (MUSP) and Its Outcomes, a population-based birth cohort study commenced in Brisbane, Australia, in 1981. A subsample of 2,278 children for whom we had prospective information on their behavioral problems at ages 5 and 14 and measured BMI, and its categories (normal, overweight, and obese) at age 21 was chosen. Young adults who experienced behavioral problems at ages 5 or 14 had a greater average BMI and were more likely to be obese compared to young adults without behavioral problems at both ages. The childhood onset group was at greater risk of becoming obese by age 21 compared to the adolescent onset group (P = 0.04). These associations remained cons! istent after adjusting for a variety of potential covariates including maternal characteristics (i.e., demographics and life style), child dietary patterns, family meals, television (TV) watching, and participation in sports and exercise at 14 years. Childhood as well as persistent behavioral problems during childhood and adolescence predicts young adults' BMI and obesity. Although further studies are needed to confirm this association, there is a need for close monitoring of children presenting with behavioral problems. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <20> Unique Identifier 19410692 Status MEDLINE Authors Tantisira KG. Authors Full Name Tantisira, Kelan G. Title In asthma, the apple falls faster than the pear.[comment]. Comments Comment on: J Allergy Clin Immunol. 2009 May;123(5):1069-74, 1074.e1-4; PMID: 19321196 Source Journal of Allergy & Clinical Immunology. 123(5):1075-6, 2009 May. Publication Type Comment. Editorial. Research Support, N.I.H., Extramural.
Result <21> Unique Identifier 19321196 Status MEDLINE Authors Marcon A. Corsico A. Cazzoletti L. Bugiani M. Accordini S. Almar E. Cerveri I. Gislason D. Gulsvik A. Janson C. Jarvis D. Martinez-Moratalla J. Pin I. de Marco R. Therapy and Health Economics Group of the European Community Respiratory Health Survey. Authors Full Name Marcon, Alessandro. Corsico, Angelo. Cazzoletti, Lucia. Bugiani, Massimiliano. Accordini, Simone. Almar, Enrique. Cerveri, Isa. Gislason, David. Gulsvik, Amund. Janson, Christer. Jarvis, Deborah. Martinez-Moratalla, Jesus. Pin, Isabelle. de Marco, Roberto. Therapy and Health Economics Group of the European Community Respiratory Health Survey. Institution Department of Medicine and Public Health, Unit of Epidemiology and Medical Statistics, University of Verona, Verona, Italy. [email protected] Title Body mass index, weight gain, and other determinants of lung function decline in adult asthma.[see comment]. Comments Comment in: J Allergy Clin Immunol. 2009 May;123(5):1075-6; PMID: 19410692 Source Journal of Allergy & Clinical Immunology. 123(5):1069-74, 1074.e1-4, 2009 May. Abstract BACKGROUND: Little is known about factors associated with lung function decline in asthma. OBJECTIVE: To identify the determinants of FEV(1) decline in adults with asthma with and without airflow obstruction at baseline. METHODS: An international cohort of 638 subjects with asthma (20-44 years old) was identified in the European Community Respiratory Health Survey (1991- 1993) and followed up from 1998 to 2002. Spirometry was performed on both occasions. FEV(1) decline was related to potential determinants evaluated at baseline and during the follow-up by random intercept linear regression models. The analyses were stratified by the presence of airflow obstruction (FEV(1)/forced vital capacity < 0.70) at baseline. RESULTS: In the group of individuals without airflow obstruction (n = 544), a faster FEV(1) decline was observed for subjects with intermediate body mass index (BMI) than for lean and obese subjects. FEV(1) decline was associated with weight gain independently of ! baseline BMI, and this association was stronger in men (20; 95% CI, 10-30, mL/y/kg gained) than in women (6; 95% CI, 1-11, mL/y). In the group of individuals with airflow obstruction (n = 94), the absence of allergen sensitization and a low BMI at baseline were associated with a faster FEV(1) decline, whereas weight gain was not associated with decline. CONCLUSIONS: The detrimental effect of weight gain on FEV(1) decline is particularly relevant in subjects with asthma who still do not have an established airflow obstruction. Our findings support the importance of weight management in asthma and recommend weight loss in overweight or obese individuals with asthma. Publication Type Journal Article. Multicenter Study. Research Support, Non-U.S. Gov't.
Result <22> Unique Identifier 19130040 Status MEDLINE Authors Lammi N. Moltchanova E. Blomstedt PA. Tuomilehto J. Eriksson JG. Karvonen M. Authors Full Name Lammi, N. Moltchanova, E. Blomstedt, P A. Tuomilehto, J. Eriksson, J G. Karvonen, M. Institution Diabetes Unit, Department of Health Promotion and Chronic Disease Prevention, National Public Health Institute, Mannerheimintie 166, 00300, Helsinki, Finland. [email protected] Title Childhood BMI trajectories and the risk of developing young adult-onset diabetes. Source Diabetologia. 52(3):408-14, 2009 Mar. Abstract AIMS/HYPOTHESIS: The aim of this study was to examine the effects of childhood BMI growth dynamics on the risk of developing young adult-onset type 1 and type 2 diabetes. METHODS: Finnish national healthcare registers were used to identify individuals with diabetes diagnosed between 1992 and 1996 at 15-39 years of age. Non-diabetic control participants were chosen from the National Population Registry. Anthropometric measurements were obtained from the original child welfare clinic records. Only the case-control pairs with sufficient growth data recorded were included in the analyses (218/1,388 for type 1 diabetes [16%] and 64/1,121 for type 2 diabetes [6%]). Two developmental stages in BMI growth (the points of infancy maximum BMI and the BMI rebound) were examined, and conditional logistic regression was applied to the variables of interest. RESULTS: The risk for type 1 diabetes increased 1.19-fold per 1 kg/m(2) rise in the infancy maximum BMI (p = 0.02). In addition, th! ere was a 1.77-fold increase in the risk for type 2 diabetes per 1 kg/m(2) rise in the level of BMI at the BMI rebound (p = 0.04). Higher values of BMI at these points corresponded to a larger BMI gain from birth to that developmental stage. Age at the infancy maximum BMI or age at the BMI rebound did not affect the risk for either type of diabetes. CONCLUSIONS/INTERPRETATION: The BMI gain in infancy among individuals who subsequently developed young adult-onset type 1 diabetes was faster than that of those who remained healthy. The excess BMI gain in individuals who developed young adult-onset type 2 diabetes could already be seen during early childhood. Publication Type Journal Article. Research Support, N.I.H., Extramural. Research Support, Non-U.S. Gov't.
Result <23> Unique Identifier 19373639 Status MEDLINE Authors Lang JE. Feng H. Lima JJ. Authors Full Name Lang, Jason E. Feng, Hua. Lima, John J. Institution Division of Pulmonology, Allergy & Immunology, Nemours Children's Clinic, Jacksonville, FL 32207, USA. [email protected] Title Body mass index-percentile and diagnostic accuracy of childhood asthma. Source Journal of Asthma. 46(3):291-9, 2009 Apr. Abstract OBJECTIVE: To determine whether high BMI-percentile is associated with misdiagnosis of asthma among children referred to an asthma specialist. METHODS: We queried the electronic records of children 8 to 18 years of age seen by a Nemours pediatric pulmonologist. All visits during a 6-year period with the chief complaint of asthma, or an asthma-like symptom such as wheeze, cough, or dyspnea, were included. We collected spirometry, blood counts, and immunoglobulin E (IgE) if available. We determined whether the child had referring physician-diagnosed asthma, specialist-diagnosed asthma, or both. Specialist-diagnosed asthmatics who met additional objective "gold-standard" criterion were labeled strict-criterion asthma. RESULTS: Prevalence of high BMI- percentile was extremely common in all defined asthma groups, even those meeting strict criteria for diagnosis. Referring physician- diagnosed asthmatics did not have higher rates of obesity, and referring physician-diagnosed asthm! atics had objective indicators of asthma that were the same as asthmatics diagnosed by a specialist. There was good diagnostic correlation between referring physicians and asthma specialists that was not affected by BMI. Among specialist-diagnosed asthmatics, increased BMI-percentile associated with significantly reduced forced expiratory volume in 1 second (FEV(1)), forced expiratory flow during the middle half of the forced vital capacity (FEF(25 - 75)), and FEV(1)/forced vital capacity (FVC); and significantly increased total blood leukocytes, neutrophils, and platelets compared to leans. For all 2,258 referrals, the estimated odds ratio of receiving a specialist-diagnosis of asthma increased by 0.4% with each increasing BMI percentile. CONCLUSIONS: Referring physicians do not appear to erroneously diagnose children with asthma due to overweight status. Our data confirm that overweight status is extremely high in children with true asthma and likely increases the risk fo! r true asthma. Although these data cannot discern causality, high BMI- percentile is associated with greater airflow obstruction and elevated markers of systemic inflammation that could contribute to underlying mechanisms of asthma. Publication Type Journal Article.
Result <24> Unique Identifier 19332753 Status MEDLINE Authors Harris KC. Kuramoto LK. Schulzer M. Retallack JE. Authors Full Name Harris, Kevin C. Kuramoto, Lisa K. Schulzer, Michael. Retallack, Jennifer E. Institution Department of Pediatrics, British Columbia Children's Hospital, Vancouver, BC. [email protected] Title Effect of school-based physical activity interventions on body mass index in children: a meta-analysis.[see comment]. [Review] [76 refs] Comments Comment in: CMAJ. 2009 Mar 31;180(7):701-2; PMID: 19332745 Source CMAJ Canadian Medical Association Journal. 180(7):719-26, 2009 Mar 31. Other ID Source: NLM. PMC2659836 Abstract BACKGROUND: The prevalence of childhood obesity is increasing at an alarming rate. Many local governments have enacted policies to increase physical activity in schools as a way to combat childhood obesity. We conducted a systematic review and meta- analysis to determine the effect of school-based physical activity interventions on body mass index (BMI) in children. METHODS: We searched MEDLINE, EMBASE, CINAHL and the Cochrane Central Register of Controlled Trials up to September 2008. We also hand- searched relevant journals and article reference lists. We included randomized controlled trials and controlled clinical trials that had objective data for BMI from before and after the intervention, that involved school-based physical activity interventions and that lasted for a minimum of 6 months. RESULTS: Of 398 potentially relevant articles that we identified, 18 studies involving 18 141 children met the inclusion criteria. The participants were primarily elementary school c! hildren. The study duration ranged from 6 months to 3 years. In 15 of these 18 studies, there was some type of co-intervention. Meta-analysis showed that BMI did not improve with physical activity interventions (weighted mean difference -0.05 kg/m(2), 95% confidence interval -0.19 to 0.10). We found no consistent changes in other measures of body composition. INTERPRETATION: School-based physical activity interventions did not improve BMI, although they had other beneficial health effects. Current population-based policies that mandate increased physical activity in schools are unlikely to have a significant effect on the increasing prevalence of childhood obesity. [References: 76] Publication Type Journal Article. Meta-Analysis. Review.
Result <25> Unique Identifier 19307476 Status MEDLINE Authors Mamun AA. O'Callaghan M. Callaway L. Williams G. Najman J. Lawlor DA. Authors Full Name Mamun, Abdullah A. O'Callaghan, Michael. Callaway, Leonie. Williams, Gail. Najman, Jake. Lawlor, Debbie A. Institution School of Population Health, University of Queensland, Herston Rd, Herston, QLD 4006, Australia. [email protected] Title Associations of gestational weight gain with offspring body mass index and blood pressure at 21 years of age: evidence from a birth cohort study. Source Circulation. 119(13):1720-7, 2009 Apr 7. Abstract BACKGROUND: Maternal weight gain in pregnancy is positively associated with offspring body mass index (BMI) and obesity risk in childhood, but whether this increased risk extends into adulthood or results in increases in other cardiovascular risk factors such as elevated blood pressure (BP) is unclear. METHODS AND RESULTS: We used a population-based birth cohort of 2432 individuals (50% male) born in Brisbane, Australia, between 1981 and 1983 to prospectively examine the association between maternal gestational weight gain (GWG) and offspring BMI and BP at 21 years. On average, each mother gained 14.8 kg (SD, 5.1 kg) during her pregnancy. At 21 years of age, offspring mean BMI, systolic BP, and diastolic BP were 24.2 kg/m(2) (SD, 4.9 kg/m(2)), 116.4 mm Hg (SD, 14.5 mm Hg), and 67.7 mm Hg (SD, 8.5 mm Hg), respectively. Offspring BMI was on average 0.3 kg/m(2) (95% confidence interval, 0.1 to 0.4 kg/m(2)) higher for each 0.1-kg/wk greater GWG after adjustment for potential c! onfounding factors. Systolic BP also was greater (0.2 mm Hg per 0.1 kg; 95% confidence interval, -0.2 to 0.6) in offspring whose mothers had higher GWG. Although this association was not statistically significant, it was consistent in magnitude with the association of maternal GWG with offspring BMI and of offspring BMI with BP. CONCLUSIONS: Our findings show that greater GWG is associated with greater offspring BMI into early adulthood and that this may translate into higher systolic BP in offspring. Further large studies are required to confirm an effect of GWG on a range of offspring cardiovascular risk factors. Publication Type Journal Article. Research Support, N.I.H., Extramural. Research Support, Non-U.S. Gov't.
Result <26> Unique Identifier 18689988 Status MEDLINE Authors Balamuthusamy S. Paramesh A. Zhang R. Florman S. Shenava R. Islam T. Wagner J. Killackey M. Alper B. Simon EE. Slakey D. Authors Full Name Balamuthusamy, Saravanan. Paramesh, Anil. Zhang, Rubin. Florman, Sander. Shenava, Rajesh. Islam, Tareq. Wagner, Janis. Killackey, Mary. Alper, Brent. Simon, Eric E. Slakey, Douglas. Institution Tulane Abdominal Transplant Institute, Tulane University Health Sciences Center, 1430 Tulane Avenue SL-45, New Orleans, LA 70112, USA. [email protected] Title The effects of body mass index on graft survival in adult recipients transplanted with single pediatric kidneys. Source American Journal of Nephrology. 29(2):94-101, 2009. Abstract BACKGROUND: There is insufficient data on the impact of recipient body mass index (BMI) on the long-term graft survival of adult patients transplanted with single pediatric kidneys. METHODS: We performed a retrospective analysis of adult patients transplanted with single pediatric kidneys at our center. The recipients were classified into 2 groups: group 1 (BMI > or =30) and group 2 (BMI <30). Donor/recipient demographics, postoperative outcomes and survival rates were compared between the 2 groups. RESULTS: There was no significant difference in donor/recipient demographics between the 2 groups. In group 1, the death-censored graft survival (DCGS) at 1, 3 and 5 years was 90% at all 3 time points, and in group 2 it was 86, 68 and 60%, respectively (p = 0.05). The mean glomerular filtration rate (with standard deviation in parentheses) at 1, 3 and 5 years was, respectively, 55 (15), 59 (19) and 55 (28) ml/min for group 1, compared to 65 (28), 69 (23) and 67 (20) ml/min in g! roup 2 (p = NS). Multivariate analysis revealed a hazard ratio of 5.12 (95% confidence interval 1.06-24.7; p = 0.04) for graft loss in nonobese patients when compared to obese patients. Obese patients had an increased risk for acute rejections within the first month of transplant (p = 0.02). CONCLUSION: Patients with a BMI > or =30 transplanted with single pediatric kidneys have better DCGS rates when compared to nonobese patients. Copyright (c) 2008 S. Karger AG, Basel. Publication Type Journal Article.
Result <27> Unique Identifier 19254998 Status MEDLINE Authors Freedman DS. Dietz WH. Srinivasan SR. Berenson GS. Authors Full Name Freedman, David S. Dietz, William H. Srinivasan, Sathanur R. Berenson, Gerald S. Institution Centers for Disease Control and Prevention, K-26, 4770 Buford Hwy, Atlanta, GA 30341-3724, USA. [email protected] Title Risk factors and adult body mass index among overweight children: the Bogalusa Heart Study. Source Pediatrics. 123(3):750-7, 2009 Mar. Abstract OBJECTIVE: Compared with thinner children, overweight children (BMI for age between the 85th and 94th Centers for Disease Control and Prevention percentiles) have moderately elevated levels of lipids and blood pressure and are at increased risk for becoming obese adults. We examined the ability of BMI for age, the skinfold sum (subscapular + triceps), and the waist/height ratio to identify which overweight children are at greatest risk. METHODS: Cross-sectional (n = 2501) and longitudinal (n = 2124) analyses were performed among subjects who participated in the Bogalusa Heart Study. RESULTS: Levels of risk factors and adult BMI (median: 32 kg/m(2)) among overweight children were midway between those of thinner children and obese children (BMI for age >/= 95th percentile). Although there was a wide range of skinfold sums among the overweight children, levels of BMI for age and the skinfold sum provided relatively little information on adverse risk-factor levels and adult BM! I. Overweight children with a relatively high (upper tertile) waist/height ratio, however, were approximately 2 to 3 times more likely to have adverse levels of most risk factors than were those with a low waist/height ratio. CONCLUSIONS: Overweight children vary substantially in terms of body fatness and risk-factor levels. Among these overweight children, levels of waist/height ratio are more strongly associated with adverse risk-factor levels than are levels of BMI for age or skinfold thickness. Additional information is needed on the relation of childhood waist/height ratio to adult complications. Publication Type Journal Article. Research Support, N.I.H., Extramural.
Result <28> Unique Identifier 18818065 Status MEDLINE Authors Ciprandi G. Pistorio A. Tosca M. Ferraro MR. Cirillo I. Authors Full Name Ciprandi, Giorgio. Pistorio, Angela. Tosca, Mariangela. Ferraro, Maria Rosaria. Cirillo, Ignazio. Institution Department of Internal Medicine, University of Genoa, Genoa, Italy. [email protected] Title Body mass index, respiratory function and bronchial hyperreactivity in allergic rhinitis and asthma. Source Respiratory Medicine. 103(2):289-95, 2009 Feb. Abstract BACKGROUND: Several studies have outlined a possible relationship between an increased body mass index (BMI) and respiratory allergic diseases, such as asthma and rhinitis. The aim of the study was to analyse the relationship between BMI and allergic diseases, including allergic rhinitis and asthma, and functional parameters, such as nasal airflow, FEV(1), and non-specific BHR to methacholine, in a cohort of navy army subjects. METHODS: The study included 100 patients with moderate-severe persistent allergic rhinitis alone, 100 with intermittent allergic asthma alone, and 100 healthy controls. All subjects were evaluated performing skin prick test, spirometry, and bronchostimulation test with methacholine. Rhinomanometry was performed in patients with rhinitis. RESULTS: BMI values were significantly lower in control subjects with respect to patients with rhinitis (P=0.0002) and with respect to patients with asthma (P<0.0001). BMI was also significantly higher in males with! respect to females (P=0.005). A significant relationship has been observed between some categories of BHR and BMI either in patients with rhinitis (P<0.01) or in patients with asthma (P<0.01), whereas there was no association between BMI and functional parameters. CONCLUSION: This study provides the first evidence of a significant relationship between BMI and allergic rhinitis and between BMI and BHR in both allergic disorders. Publication Type Journal Article.
Result <29> Unique Identifier 19121863 Status MEDLINE Authors Macsali F. Real FG. Omenaas ER. Bjorge L. Janson C. Franklin K. Svanes C. Authors Full Name Macsali, Ferenc. Real, Francisco Gomez. Omenaas, Ernst Reidar. Bjorge, Line. Janson, Christer. Franklin, Karl. Svanes, Cecilie. Institution Department of Gynecology and Obstetrics, Haukeland University Hospital, Bergen, Norway. Title Oral contraception, body mass index, and asthma: a cross-sectional Nordic-Baltic population survey. Source Journal of Allergy & Clinical Immunology. 123(2):391-7, 2009 Feb. Abstract BACKGROUND: Emerging evidence suggests that sex steroid hormones may influence airways obstruction, and that metabolic status may modify potential effects. OBJECTIVE: This study investigated the association between use of oral contraceptive pills (OCPs) and asthma in a Nordic-Baltic population-based study, while taking into account possible interplay with body mass index (BMI). METHODS: Postal questionnaires were sent to subjects in Denmark, Estonia, Iceland, Norway, and Sweden from 1999 to 2001 (response rate in women, 77%). Pregnant women, women using hormone replacement therapy, and women >45 years were excluded. Analyses included 5791 women 25 to 44 years old, of whom 961 (17%) used OCP. Logistic regression analyses included adjustment for smoking, irregular menstruation, BMI, age, type of dwelling, and center. RESULTS: Oral contraceptive pills were associated with increased risk for asthma (odds ratio, 1.42; 95% CI, 1.09-1.86), asthma with hay fever (1.48; 1.08-2.03),! wheeze with shortness of breath (1.27; 1.02-1.60), hay fever (1.25; 1.06-1.48), and >/=3 asthma symptoms (1.29; 1.05-1.58). The findings were consistent between centers. The associations were present only among normal weight women (BMI 20-25 kg/m(2), asthma: 1.45; 1.02-2.05) and overweight women (BMI >25kg/m(2): 1.91; 1.20-3.02), but not among lean women (BMI <20 kg/m(2): 0.41; 0.12-1.40). Interaction between BMI and OCP in association with asthma was significant (P(interaction) < .05). CONCLUSIONS: Women using oral contraceptive pills had more asthma. This was found only in normal weight and overweight women, indicating interplay between sex hormones and metabolic status in effect on the airways. The findings originate from a cross-sectional postal survey and should be interpreted with caution; it is recommended that asthma symptoms are included in clinical trials of oral contraception. Publication Type Journal Article. Multicenter Study. Research Support, Non-U.S. Gov't.
Result <30> Unique Identifier 19191138 Status MEDLINE Authors Szczepankiewicz A. Breborowicz A. Sobkowiak P. Popiel A. Authors Full Name Szczepankiewicz, Aleksandra. Breborowicz, Anna. Sobkowiak, Paulina. Popiel, Anna. Institution Clinics of Pediatric Pulmonology, Allergy and Clinical Immunology, Poznan University of Medical Sciences, Poznan, Poland. [email protected] Title Are genes associated with energy metabolism important in asthma and BMI?. Source Journal of Asthma. 46(1):53-8, 2009 Feb. Abstract OBJECTIVE: Increased serum leptin levels have been observed in asthmatic patients. Leptin, via proliferation and activation of Th2 cells, may induce inflammation in asthma. It has also been demonstrated that leptin mRNA expression and protein levels increase in response to inflammatory stimuli. We hypothesized that polymorphisms in the leptin receptor, leptin and ghrelin genes, may affect their expression and, therefore, be responsible for altered response to increased leptin levels observed in asthma. To our knowledge, there were no studies on a potential role of LEPR, LEP, and GHRL polymorphisms in asthma. SUBJECTS AND METHODS: We analyzed 129 pediatric patients with asthma and 114 healthy children from the control group ranging from 6 to 18 years of age. The diagnosis of allergic asthma was based on clinical symptoms, the lung function test, and the positive skin prick test and/or increased immunoglobulin E (IgE) levels. Polymorphisms were genotyped by the polymerase ch! ain reaction-restriction fragment length polymorphism (PCR-RFLP) method. Statistical analyses were performed with Statistica v.7.1 software (Statistica, StatSoft, Poland; available free at http://www.broad.mit.edu/mpg/haploview/index.php). Linkage disequilibrium analysis was performed with Haploview v.4.0. RESULTS: We observed a statistically significant association of the 3'UTR A/G and the -2549A/G polymorphisms of the leptin gene with asthma. No association with asthma was observed for the K109R and the Q223R polymorphisms of the LEPR gene and the Met72Leu polymorphism of the ghrelin gene. In the analysis of body mass index (BMI) stratified by genotype, we found an association of the -2549A/G LEP, but not of LEPR and GHRL polymorphisms, with higher BMI values in asthmatic patients. We found suggestive evidence for linkage between the two polymorphisms of the LEPR gene (D' = 0.84 CI: 0.71-0.92; r(2) = 0.29) in linkage disequilibrium analysis: The GG haplotype was more freq! uent in the control healthy group (p = 0.057). No linkage disequilibri um was detected between LEP polymorphisms. CONCLUSIONS: Polymorphisms of the leptin gene may be associated with asthma and higher BMI in asthmatic patients. Polymorphisms of the LEPR and GHRL seem unlikely to be associated with asthma or BMI in our sample. The results of haplotype analysis for the LEPR gene may suggest a protective role of the GG haplotype against asthma; however, studies on larger groups are necessary to confirm the observed trend towards association. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <31> Unique Identifier 19191130 Status MEDLINE Authors Tsai HJ. Tsai AC. Authors Full Name Tsai, Hsin-Jen. Tsai, Alan C. Institution Department of Health Management, I-Shou University, Kaohsiung County, Taiwan. [email protected] Title The association of BMI and sedentary time with respiratory symptoms and asthma in 5th grade schoolchildren in Kaohsiung, Taiwan. Source Journal of Asthma. 46(1):9-15, 2009 Feb. Abstract This study aimed to evaluate the association of body fatness and sedentary status with asthma and respiratory symptoms in schoolchildren in Kaohsiung, Taiwan. A questionnaire study elicited episodes of respiratory symptoms and data on lifestyle and anthropometric parameters in 1329 5th grade schoolchildren. Results showed that 12.4% of boys and 9.5% of girls had physician- diagnosed asthma, whereas 15.1% of boys and 12.4% of girls had suspected asthma. Significantly greater proportions of boys had non-exercise-induced respiratory symptoms than girls (p < 0.05). The number of respiratory symptoms was positively correlated with TV-watching time per day and self-reported sedentary time per weekend-day in girls (p < 0.05). Underweight was positively associated with one of the seven respiratory symptoms in girls (p < 0.05). At risk of overweight was positively associated with two of the seven respiratory symptoms in boys and one of the seven respiratory symptoms in girls (all p ! < 0.05). The risk of having physician-diagnosed asthma and suspected asthma increased 93% and 72%, respectively, in schoolchildren at risk of overweight (p < 0.05). Overweight was associated with a 78% increase in physician-diagnosed asthma (adjusted odd ratio (aOR) = 1.78, 95% CI = 1.08-2.91, p < 0.05). Higher sedentary time was significantly associated with more occurrences of one of the seven respiratory symptoms in girls (aOR = 1.05, 95% CI = 1.00-1.11, p < 0.05). Higher body mass index (BMI) was significantly correlated with longer TV-watching time per day in girls and longer self-reported sedentary time per weekday in boys (p < 0.05). In summary, schoolchildren who are at risk of overweight or overweight and/or have more sedentary time have increased risk of respiratory symptoms and asthma. Weight and sedentary statuses of schoolchildren can affect their respiratory health. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <32> Unique Identifier 19104889 Status MEDLINE Authors Schwandt P. Kelishadi R. Haas GM. Authors Full Name Schwandt, Peter. Kelishadi, Roya. Haas, Gerda-Maria. Institution Arteriosklerose-Praventions-Institut, Munich-Nuremberg, Germany. [email protected] Title First reference curves of waist circumference for German children in comparison to international values: the PEP Family Heart Study. Source World Journal of Pediatrics. 4(4):259-66, 2008 Nov. Abstract BACKGROUND: Waist circumference (WC) is a sensitive marker for abdominal obesity in the pediatric age group. However, WC is influenced by age, sex, ethnicity and body mass index (BMI), causing difficulties in the selection of the most appropriate cut-off value. Considering the lack of reference values in Germany, we developed age- and gender-specific WC smoothed reference curves in German children, and compared them with reference curves obtained from different countries. METHODS: A representative sample of 3531 German children (1788 boys, 1743 girls) aged 3-11 years participating in the Prevention Education Program (PEP) Family Heart Study was studied. WC was measured according to the recommendations of the World Health Organization, then age- and sex-specific WC reference curves were constructed and smoothed using the LMS method and SPSS 14.0 for statistical analysis. RESULTS: WC increased with age in both boys and girls. Boys had higher values of WC than girls at every ! age and percentile level. 4.1% of the boys and 2.8% of the girls had WC values >97th percentile as compared to 6.3% of the boys and 4.9% of the girls with >97th percentile of BMI (severe obesity). 3.1% of the boys and 2% of the girls had both risk factors. Because 85.3% of the boys and 87.3% of the girls with WC<90th percentile had normal weight, this cut-off point might be appropriate for defining high WC. CONCLUSIONS: These first WC reference curves of German children can be added to the existing international curves for children; comparison of different populations demonstrated that the German values are in the middle range of the curves obtained in different countries. Our findings about significant differences between the reference curves obtained in various regions emphasize the necessity of developing population-specific percentiles, and to use them in clinical and epidemiological studies among children. Publication Type Comparative Study. Journal Article. Research Support, Non-U.S. Gov't. Result <33> Unique Identifier 18974465 Status MEDLINE Authors Solhpour A. Pourhoseingholi MA. Soltani F. Zarghi A. Habibi M. Ghafarnejad F. Tajik Z. Rostaminejad M. Ramezankhani A. Zali MR. Authors Full Name Solhpour, Ali. Pourhoseingholi, Mohamad Amin. Soltani, Fereshteh. Zarghi, Afsaneh. Habibi, Manijeh. Ghafarnejad, Fatemeh. Tajik, Zohreh. Rostaminejad, Mohammad. Ramezankhani, Ali. Zali, Mohammad Reza. Institution Research Center For Gastroenterology and Liver Diseases, Taleghani Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran. [email protected] Title Gastro-esophageal reflux symptoms and body mass index: no relation among the Iranian population. Source Indian Journal of Gastroenterology. 27(4):153-5, 2008 Jul-Aug. Abstract An association between obesity and symptoms of gastro-esophageal reflux disease (GERD) has been frequently reported in western societies. A recent study indicated a consistent association between abdominal diameter and reflux-type symptoms in the white population, but no consistent association in the black population or Asians. It is unclear whether an association persists after adjusting for known risk factors of GERD among Asian populations. We did a population-based, cross-sectional interview study to estimate the strength of association between body mass and symptoms of reflux. During interviews, participants completed a valid gastro-esophageal reflux questionnaire. Odds ratio (OR) with 95% confidence interval (CI), calculated by logistic regression with multivariate adjustments for covariates, were the measures of association. Symptoms of reflux at least once a week over the past 3 months were reported by 522 (9.1%) of the 5733 interviewees. Among those who were overw! eight or obese (BMI> 25 kg/m2), the OR of having symptoms of reflux was 0.88 (95% CI: 0.66-1.16) compared with those who were not overweight or obese. Thus, among Asians, symptoms of GERD occur independently of body mass index. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <34> Unique Identifier 18980776 Status MEDLINE Authors Coogan PF. Palmer JR. O'Connor GT. Rosenberg L. Authors Full Name Coogan, Patricia F. Palmer, Julie R. O'Connor, George T. Rosenberg, Lynn. Institution Slone Epidemiology Center at Boston University, Boston, MA 02215, USA. [email protected] Title Body mass index and asthma incidence in the Black Women's Health Study.[see comment]. Comments Comment in: J Allergy Clin Immunol. 2009 Jan;123(1):96-7; PMID: 19130929 Source Journal of Allergy & Clinical Immunology. 123(1):89-95, 2009 Jan. Abstract BACKGROUND: Evidence from prospective studies consistently links obesity to asthma onset in white women, although there is controversy as to whether the association is causal. There are few data on this topic in black women, among whom the prevalence of obesity and asthma is high. OBJECTIVE: We prospectively assessed the relation of body mass index (BMI) to asthma incidence in the Black Women's Health Study. METHODS: We followed 46,435 women from 1995 through 2005 with biennial mailed questionnaires. Cox regression models were used to estimate incidence rate ratios and 95% CIs. RESULTS: During 403,394 person- years of follow-up, 1068 participants reported physician-diagnosed asthma and concurrent use of asthma medication. Compared with women with BMIs of 20 to 24, the multivariate incidence rate ratios for higher categories of BMI increased from 1.26 (95% CI, 1.05-1.51) for BMIs of 25 to 29 to 2.85 (95% CI, 2.19-3.72) for BMIs of 40 or greater, with a significant trend. The! association of BMI with asthma risk was consistent across strata of smoking status, age, presence of sleep apnea, parental history of asthma, BMI at age 18 years, and energy expenditure and intake. CONCLUSION: In this large cohort of African American women, there was a positive association between BMI and asthma risk that was similar in magnitude to those observed in longitudinal studies of white women. Publication Type Journal Article. Research Support, N.I.H., Extramural.
Result <35> Unique Identifier 18811794 Status MEDLINE Authors Garcia-Marcos L. Valverde-Molina J. Ortega ML. Sanchez-Solis M. Martinez-Torres AE. Castro-Rodriguez JA. Authors Full Name Garcia-Marcos, Luis. Valverde-Molina, Jose. Ortega, Maria L Castanos. Sanchez-Solis, Manuel. Martinez-Torres, Antonia E. Castro-Rodriguez, Jose A. Institution Department of Pediatrics, Virgen Arrixaca University Children's Hospital, 30120 El Palmar, Murcia, Spain. [email protected] Title Percent body fat, skinfold thickness or body mass index for defining obesity or overweight, as a risk factor for asthma in schoolchildren: which one to use in epidemiological studies?. Source Maternal & Child Nutrition. 4(4):304-10, 2008 Oct. Abstract None of the epidemiological studies indicating that obesity is a risk factor for asthma in schoolchildren have used the percent body fat (PBF) to define obesity. The present study compares the definition of obesity using body mass index (BMI), PBF and the raw sum of the thickness of four skinfolds (SFT) to evaluate this condition as a risk factor for asthma. All classes of children of the target ages of 6-8 years of all schools in four municipalities of Murcia (Spain) were surveyed. Participation rate was 70.2% and the number of children included in the study was 931. Height, weight and SFT (biceps, triceps, subscapular and suprailiac) were measured according to standard procedures. Current active asthma was defined from several questions of the International Study of Asthma and Allergies in Childhood questionnaire. Obesity was defined using two standard cut-off points for BMI and PBF, and the 85th percentile for BMI, PBF and SFT. The highest quartile of each type of measu! rement was also compared with the lowest. A multiple logistic regression analysis was made for the various obesity definitions, adjusting for age, asthma in the mother and father and gender. The adjusted odds ratios of having asthma among obese children were different for boys and girls and varied across the different obesity definitions. For the standard cut-off points of BMI they were 1.19 [95% confidence interval (CI) 0.41-3.43] for girls and 2.00 (95% CI 0.97-4.10) for boys; however, for PBF (boys 25%, girls 30%) the corresponding figures were 1.54 (95% CI 0.63-3.73) and 1.20 (95% CI 0.66-2.21). BMI, PBF and SFT showed more consistency between each other when using the other cut-off points. BMI, PBF (except standard cut-off points) and SFT produce relatively comparable results when analysing the interaction between obesity and asthma. Publication Type Journal Article.
Result <36> Unique Identifier 19000844 Status MEDLINE Authors Bell JF. Wilson JS. Liu GC. Authors Full Name Bell, Janice F. Wilson, Jeffrey S. Liu, Gilbert C. Institution Department of Health Services, School of Public Health and Community Medicine, University of Washington, Seattle, Washington 98195-7230, USA. [email protected] Title Neighborhood greenness and 2-year changes in body mass index of children and youth.[see comment]. Comments Comment in: Am J Prev Med. 2008 Dec;35(6):604-5; PMID: 19000850 Source American Journal of Preventive Medicine. 35(6):547-53, 2008 Dec. Abstract BACKGROUND: Available studies of the built environment and the BMI of children and youth suggest a contemporaneous association with neighborhood greenness in neighborhoods with high population density. The current study tests whether greenness and residential density are independently associated with 2-year changes in the BMI of children and youth. METHODS: The sample included children and youth aged 3-16 years who lived at the same address for 24 consecutive months and received well-child care from a Marion County IN clinic network within the years 1996-2002 (n=3831). Multiple linear regression was used to examine associations among age- and gender-specific BMI z-scores in Year 2, residential density, and a satellite-derived measure of greenness, controlling for baseline BMI z-scores and other covariates. Logistic regression was used to model associations between an indicator of BMI z-score increase from baseline to Time 2 and the above-mentioned predictors. RESULTS: High! er greenness was significantly associated with lower BMI z-scores at Time 2 regardless of residential density characteristics. Higher residential density was not associated with Time 2 BMI z-scores in models regardless of greenness. Higher greenness was also associated with lower odds of children's and youth's increasing their BMI z-scores over 2 years (OR=0.87; 95% CI=0.79, 0.97). CONCLUSIONS: Greenness may present a target for environmental approaches to preventing child obesity. Children and youth living in greener neighborhoods had lower BMI z-scores at Time 2, presumably due to increased physical activity or time spent outdoors. Conceptualizations of walkability from adult studies, based solely on residential density, may not be relevant to children and youth in urban environments. Publication Type Journal Article. Research Support, N.I.H., Extramural. Research Support, U.S. Gov't, P.H.S..
Result <37> Unique Identifier 18677544 Status MEDLINE Authors Amin TT. Al-Sultan AI. Ali A. Authors Full Name Amin, Tarek Tawfik. Al-Sultan, Ali Ibrahim. Ali, Ayub. Institution Family and Community Medicine Dept, College of Medicine, King Faisal University-Al Hassa, Al-Hassa, Saudi Arabia. [email protected] Title Overweight and obesity and their relation to dietary habits and socio-demographic characteristics among male primary school children in Al-Hassa, Kingdom of Saudi Arabia. Source European Journal of Nutrition. 47(6):310-8, 2008 Sep. Abstract BACKGROUND: Several studies were carried out to study the prevalence of overweight and obesity among Saudi children, but those assessed the association between eating habits, socio-demographic differentials and obesity in these children are scarce. OBJECTIVES: To assess the magnitude of obesity and overweight among male primary schoolchildren and to find the possible association between obesity/overweight with dietary habits and socio-demographic differentials among them. STUDY DESIGN AND METHODS: A cross-sectional descriptive study including 1,139 Saudi male enrolled in the fifth and sixth grades in public primary schools in Al Hassa, KSA, through a multistage random sampling technique, submitted to interview using Youth and Adolescent Food Frequency Questionnaire, gathering data regarding dietary intake, some dietary habits, followed by anthropometric measurements with calculation of body mass index, the interpretation of which was based on using Cole's tables for standa! rd definition of overweight and obesity. Socio-demographics data were collected through parental questionnaire form. Data analysis was carried out using SPSS 12 (SPSS Inc. Chicago, IL, USA), univariate as well as multivariate analyses were conducted. RESULTS: The age ranged from 10 to 14 years. The prevalence of overweight among the included subjects was 14.2% while obesity was 9.7%, more in urban, older age students, mothers of obese and overweight were less educated, more working. Missing and or infrequent intake of breakfast at home, frequent consumption of fast foods, low servings of fruits, vegetables, milk and dairy product per day, with frequent consumption of sweets/candy and carbonated drinks were all predictors of obesity and overweight among the included male schoolchildren. CONCLUSION: The prevalence of childhood obesity is escalating and approaching figures reported in the developed countries. Less healthy dietary habits and poor food choices may be responsible! for this high prevalence. Publication Type Journal Article.
Result <38> Unique Identifier 18587680 Status MEDLINE Authors Zhang CX. Tse LA. Deng XQ. Jiang ZQ. Authors Full Name Zhang, Cai-Xia. Tse, Lap-Ah. Deng, Xue-Qing. Jiang, Zhuo-Qin. Institution Dept of Biostatistics and Epidemiology, School of Public Health, Sun Yat-sen University, Guangzhou, PR China. Title Cardiovascular risk factors in overweight and obese Chinese children: a comparison of weight-for-height index and BMI as the screening criterion. Source European Journal of Nutrition. 47(5):244-50, 2008 Aug. Abstract BACKGROUND: Childhood obesity is a widespread and growing problem in the world. Body mass index (BMI) and weight-for-height criterion have been used to determine childhood obesity. No data was available to evaluate cardiovascular risk factors in overweight and obese Chinese children screened by weight-for-height index and Chinese newly developed BMI criterion. AIM OF THE STUDY: To evaluate cardiovascular risk factors in overweight and obese Chinese children by using Chinese BMI and weight-for-height index as screening criterion. METHODS: A total of 215 children aged 7.5-13 years were recruited from 3 primary schools in Guangzhou, PR China. Measurements included body weight, height, waist and hip circumference, fasting serum glucose, insulin, total triglyceride (TG), total cholesterol (TC), high density lipoprotein cholesterol (HDL-C), low density lipoprotein cholesterol (LDL-C), apolipoprotein A (apo A), apolipoprotein B (apo B). Chinese BMI and weight-for- height criterio! n were used to classify overweight and obesity. RESULTS: According to Chinese BMI criterion, 65 from 108 obese children originally identified by weight-for-height were reclassified as obese and other 41 children were classified as overweight. Compared with non- obese children, obese children screened by Chinese BMI and weight-for-height index had increased levels of TG, LDL-C, apo B, insulin; decreased levels of HDL-C, apo A; and significantly higher prevalence of hypertriglyceridemia and high LDL-C. Children identified as overweight by Chinese BMI criterion had also shown high TG, LDL-C, apo B, insulin levels, low HDL-C, apo A levels, and significantly higher prevalence of hypertriglyceridemia than the normal weight children. CONCLUSIONS: Our study reveals that overweight and/or obesity screened by both Chinese new BMI and weight-for-height criterion are associated with increased levels of cardiovascular risk factors (e.g., elevated serum TG, LDL, apo B, and reduced HDL-C, ! apo A levels). Using Chinese BMI criterion may underestimate the preva lence of childhood obesity but it could be adopted as a unique tool for screening children's overweight in population-based screening programs. Publication Type Journal Article.
Result <39> Unique Identifier 18766115 Status MEDLINE Authors Jacobi C. Schmitz G. Agras WS. Authors Full Name Jacobi, Corinna. Schmitz, Gabriele. Agras, William Stewart. Institution University of Dresden, Clinical Psychology and Psychotherapy, Dresden, Germany. [email protected] Title Interactions between disturbed eating and weight in children and their mothers. Source Journal of Developmental & Behavioral Pediatrics. 29(5):360-6, 2008 Oct. Abstract OBJECTIVE: This study assessed the interaction between disturbed eating behavior and body mass index (BMI) in children aged 8 to 12 and maternal eating problems and BMI. METHOD: In a cohort study, four hundred twenty-six 8- to 12-year-old children and their primary caretakers (91% mothers) were assessed in a small city. Disturbed eating behavior in children was measured by the "IEG-IEG-Child-Questionnaire," a validated German self-report instrument for children. Disturbed eating behavior in mothers was assessed by TFEQ-subscale disinhibition. RESULTS: Children's BMI was a significant covariate of disturbed eating. Older girls with higher BMI endorsed more problems with eating and weight, and more body dissatisfaction than boys and younger children. Daughters of overweight mothers restrained their own eating behavior more than daughters of normal weight mothers and sons regardless of mothers' weight. Older daughters of overweight mothers were more dissatisfied with their ow! n bodies than younger daughters and children of normal weight mothers. Children of mothers with elevated disinhibition showed more body dissatisfaction than children of mothers with lower disinhibition. CONCLUSIONS: The results illustrate the complex and differential relationships between age, gender, BMI, and maternal variables and eating disturbances in children. Preventive interventions for the reduction of disturbed eating in children should be targeted at overweight mothers and mothers with disinhibited eating. Publication Type Journal Article.
Result <40> Unique Identifier 18719630 Status MEDLINE Authors Stovitz SD. Pereira MA. Vazquez G. Lytle LA. Himes JH. Authors Full Name Stovitz, Steven D. Pereira, Mark A. Vazquez, Gabriela. Lytle, Leslie A. Himes, John H. Institution Department of Family Medicine and Community Health, University of Minnesota, Minneapolis, Minnesota, USA. [email protected] Title The interaction of childhood height and childhood BMI in the prediction of young adult BMI. Source Obesity. 16(10):2336-41, 2008 Oct. Abstract The purpose of this study was to examine the interaction of childhood height and childhood BMI in the prediction of young adult BMI. The 2,802 subjects in this study were from the Child and Adolescent Trial for Cardiovascular Health (CATCH). The subjects' heights and weights were measured in 3rd grade (mean age 8.7 years) and again in 12th grade (mean age 18.3 years). The associations and interactions between height (cm) and BMI (kg/m(2)) were assessed using mixed linear regression models with adult BMI as the dependent variable. We found a significant interaction between childhood height and childhood BMI in the prediction of adult BMI (P < 0.0001). Stratification by Centers for Disease Control and Prevention (CDC) reference quintiles revealed that a positive association between childhood height and adult BMI existed only for those subjects in the top quintile of childhood BMI, within whom predicted adult BMI ranged from 27.5 (95% confidence interval = 26.4-28.6) for thos! e in the shortest height quintile to 30.2 (95% confidence interval = 29.7-30.6) for those in the highest height quintile. Among children with high BMI levels, those who were taller, as compared to those who were shorter, had significantly higher young adult BMI levels. This pattern seems primarily due to the positive association of childhood height and childhood BMI. Clinicians should recognize the risk of excess body weight in young adulthood for all children who have a high BMI, and pay special attention to those who are tall, because their childhood height will not protect them from subsequent weight gain and elevated BMI. Publication Type Journal Article. Multicenter Study. Randomized Controlled Trial. Research Support, N.I.H., Extramural. Research Support, Non- U.S. Gov't.
Result <41> Unique Identifier 18778466 Status MEDLINE Authors Beyerlein A. Fahrmeir L. Mansmann U. Toschke AM. Authors Full Name Beyerlein, Andreas. Fahrmeir, Ludwig. Mansmann, Ulrich. Toschke, Andre M. Institution Ludwig-Maximilians University of Munich, Division of Pediatric Epidemiology, Institute of Social Pediatrics and Adolescent Medicine, Munich, Germany. [email protected] Title Alternative regression models to assess increase in childhood BMI. Source BMC Medical Research Methodology. 8:59, 2008. Other ID Source: NLM. PMC2543035 Abstract BACKGROUND: Body mass index (BMI) data usually have skewed distributions, for which common statistical modeling approaches such as simple linear or logistic regression have limitations. METHODS: Different regression approaches to predict childhood BMI by goodness-of-fit measures and means of interpretation were compared including generalized linear models (GLMs), quantile regression and Generalized Additive Models for Location, Scale and Shape (GAMLSS). We analyzed data of 4967 children participating in the school entry health examination in Bavaria, Germany, from 2001 to 2002. TV watching, meal frequency, breastfeeding, smoking in pregnancy, maternal obesity, parental social class and weight gain in the first 2 years of life were considered as risk factors for obesity. RESULTS: GAMLSS showed a much better fit regarding the estimation of risk factors effects on transformed and untransformed BMI data than common GLMs with respect to the generalized Akaike information criter! ion. In comparison with GAMLSS, quantile regression allowed for additional interpretation of prespecified distribution quantiles, such as quantiles referring to overweight or obesity. The variables TV watching, maternal BMI and weight gain in the first 2 years were directly, and meal frequency was inversely significantly associated with body composition in any model type examined. In contrast, smoking in pregnancy was not directly, and breastfeeding and parental social class were not inversely significantly associated with body composition in GLM models, but in GAMLSS and partly in quantile regression models. Risk factor specific BMI percentile curves could be estimated from GAMLSS and quantile regression models. CONCLUSION: GAMLSS and quantile regression seem to be more appropriate than common GLMs for risk factor modeling of BMI data. Publication Type Comparative Study. Journal Article. Research Support, Non-U.S. Gov't.
Result <42> Unique Identifier 18635892 Status MEDLINE Authors Sutherland ER. Goleva E. Strand M. Beuther DA. Leung DY. Authors Full Name Sutherland, E Rand. Goleva, Elena. Strand, Matthew. Beuther, David A. Leung, Donald Y M. Institution Department of Medicine, National Jewish Medical and Research Center, 1400 Jackson Street, J-220 Denver, CO 80206, USA. [email protected] Title Body mass and glucocorticoid response in asthma. Source American Journal of Respiratory & Critical Care Medicine. 178(7):682-7, 2008 Oct 1. Other ID Source: NLM. PMC2556450 [Available on 10/01/09] Abstract RATIONALE: Obesity may alter glucocorticoid response in asthma. OBJECTIVES: To evaluate the relationship between body mass index (BMI, kg/m(2)) and glucocorticoid response in subjects with and without asthma. METHODS: Nonsmoking adult subjects underwent characterization of lung function, BMI, and spirometric response to prednisone. Dexamethasone (DEX, 10(-6) M)- induced mitogen-activated protein kinase phosphatase-1 (MKP-1) and baseline tumor necrosis factor (TNF)-alpha expression were evaluated by polymerase chain reaction in peripheral blood mononuclear cells (PBMCs) and bronchoalveolar lavage cells. The relationship between BMI and expression of MKP-1 and TNF-alpha was analyzed. MEASUREMENTS AND MAIN RESULTS: A total of 45 nonsmoking adults, 33 with asthma (mean [SD] FEV(1)% of 70.7 [9.8]%) and 12 without asthma were enrolled. DEX-induced PBMC MKP-1 expression was reduced in overweight/obese versus lean patients with asthma, with mean (+/- SEM) fold-induction of 3.11 (+/! -0.46) versus 5.27 (+/-0.66), respectively (P = 0.01). In patients with asthma, regression analysis revealed a -0.16 (+/-0.08)-fold decrease in DEX-induced MKP-1 per unit BMI increase (P = 0.04). PBMC TNF-alpha expression increased as BMI increased in subjects with asthma, with a 0.27 unit increase in log (TNF-alpha [ng/ml]) per unit BMI increase (P = 0.01). The ratio of PBMC log (TNF-alpha):DEX-induced MKP-1 also increased as BMI increased in patients with asthma (+0.09 +/- 0.02; P = 0.004). In bronchoalveolar lavage cells, DEX-induced MKP-1 expression was also reduced in overweight/obese versus lean patients with asthma (1.36 +/- 0.09-fold vs. 1.76 +/- 0.15-fold induction; P = 0.05). Similar findings were not observed in control subjects without asthma. CONCLUSIONS: Elevated BMI is associated with blunted in vitro response to dexamethasone in overweight and obese patients with asthma. Publication Type In Vitro. Journal Article. Research Support, N.I.H., Extramural.
Result <43> Unique Identifier 18788265 Status MEDLINE Authors Siminialayi IM. Emem-Chioma PC. Dapper DV. Authors Full Name Siminialayi, I M. Emem-Chioma, P C. Dapper, D V. Institution Department of Pharmacology, Faculty of Basic Medical Sciences, College of Health Sciences, University of Port Harcourt, Port Harcourt. [email protected] Title The prevalence of obesity as indicated by BMI and waist circumference among Nigerian adults attending family medicine clinics as outpatients in Rivers State. Source Nigerian Journal of Medicine: Journal of the National Association of Resident Doctors of Nigeria. 17(3):340-5, 2008 Jul-Aug. Abstract BACKGROUND: The prevalence of overweight and obesity in most developed countries and in urban areas of many less developed countries has been increasing markedly over the past twenty years. This study's aims were to determine the prevalence of obesity using BMI and waist circumference among Nigerian adults attending Family Medicine Clinics as outpatients and to assess the relative associations with CVD risk factors. METHODS: Subjects, who all volunteered for this study reported at the study centres after an overnight fast, to be weighed (in kg), for their heights (in metres), blood pressure and waist circumference (in cm) measured, and their venous blood samples taken for lipid studies and fasting blood glucose estimation. Results were analysed using SPSS for windows software (version 11) and Epi Info (version 6. 04d). RESULTS: The prevalence of obesity as determined by large waist circumference was 31.7% at the Okrika (rural) centre and 16.9% at the Port Harcourt centre. ! It was 16.3% at the Okrika centre and 14% at the Port Harcourt centre, as determined by BMI > or = 30 kgm(-2). Obesity as determined by BMI > or = 30 kgm(-2) is more prevalent among young adults (< 40 years) in Port Harcourt than at Okrika. Obesity by both definitions is more prevalent among females than among males (p < 0.01) and more among subjects older than 40 years. Both indices of obesity appear to be significantly associated with CVD risk factors. CONCLUSION: Obesity in our environment is strongly associated with a family history of obesity and a sedentary lifestyle. It is therefore not surprisingly more prevalent among females and older members of society. Healthier eating and social habits, and increased physical activity need to be strongly encouraged. Publication Type Journal Article.
Result <44> Unique Identifier 18654874 Status MEDLINE Authors Iughetti L. De Simone M. Verrotti A. Iezzi ML. Predieri B. Bruzzi P. Bernasconi S. Balli F. Bedogni G. Authors Full Name Iughetti, Lorenzo. De Simone, Michele. Verrotti, Alberto. Iezzi, Maria Laura. Predieri, Barbara. Bruzzi, Patrizia. Bernasconi, Sergio. Balli, Fiorella. Bedogni, Giorgio. Institution Department of Pediatrics, University of Modena and Reggio Emilia, Via del Pozzo 71, Modena 41100, Italy. [email protected] Title Thirty-year persistence of obesity after presentation to a pediatric obesity clinic. Source Annals of Human Biology. 35(4):439-48, 2008 Jul-Aug. Abstract BACKGROUND: Few large, long-term studies are available on the relationship between childhood and adult obesity. AIM: The present study examined the 30-year association between childhood and adult obesity in a large sample of girls with essential and uncomplicated obesity. SUBJECTS AND METHODS: 318 girls who had visited our Pediatric Obesity Clinic between January 1972 and December 1974 were re-contacted between January 2002 and December 2005. All had undergone an assessment of weight, height and pubertal status at the baseline visit. Anthropometry was performed again on those who agreed to take part in the follow-up visit. The women's general practitioners were also asked to compile a health questionnaire. Hypertension, hypercholesterolemia, hypertriglyceridemia and diabetes were defined according to current guidelines. Rates are expressed as number of cases per 1000 person-years (PY). Multivariable Poisson regression was used to identify predictors of persistent obesity. ! RESULTS: 224 (70%) of the 318 girls took part to the 30-year follow-up study. They had the same baseline anthropometry of those not available at follow-up. Sixteen per cent of them were still obese at the 30-year follow-up, giving a persistence rate of obesity of 5.2 x 1000 PY. Tanner stages > or = 1 [rate = ratios (RR) from 4.73 to 7.74 for different stages, p < or = 0.021] and Z-score of BMI (RR = 2.72 for one SDS, p = 0.019) were independent predictors of obesity persistence. Having a university degree vs. an elementary degree was instead protective (RR = 0.32, p = 0.009). The most prevalent complication was hypertriglyceridemia (8.8 x 1000 PY), followed by hypercholesterolemia (rate = 8.4 x 1000 PY), hypertension (rate = 5.2 x 1000 PY) and diabetes mellitus (rate = 1.0 x 1000 PY). CONCLUSION: The study reinforces the notion that obesity should be prevented at an early age and shows that adolescents with severe obesity and low educational degree are at greater risk of be! coming obese adults. Publication Type Journal Article.
Result <45> Unique Identifier 18612899 Status MEDLINE Authors Sithole F. Douwes J. Burstyn I. Veugelers P. Authors Full Name Sithole, Fortune. Douwes, Jeroen. Burstyn, Igor. Veugelers, Paul. Institution School of Public Health, University of Alberta, Edmonton, Alberta, Canada. Title Body mass index and childhood asthma: a linear association?. Source Journal of Asthma. 45(6):473-7, 2008 Aug. Abstract Our objective was to characterize the association between body mass index (BMI) and childhood asthma while adjusting for individual and neighborhood socioeconomic factors. Data were obtained from 3,804 students 10 to 11 years of age in Nova Scotia, Canada. Asthma was defined as parent-reported doctor-diagnosed asthma or bronchitis. Smoothed curves suggested a linear association between BMI and asthma with a 6 % increase in prevalence per unit increase of BMI. This association was independent of allergies, sex, and socioeconomic factors. Girls from socioeconomically disadvantaged neighborhoods were less likely to be asthmatic as were boys from well-educated and wealthy families. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <46> Unique Identifier 18612501 Status MEDLINE Authors Lambert M. Delvin EE. Levy E. O'Loughlin J. Paradis G. Barnett T. McGrath JJ. Authors Full Name Lambert, Marie. Delvin, Edgard E. Levy, Emile. O'Loughlin, Jennifer. Paradis, Gilles. Barnett, Tracie. McGrath, Jennifer J. Institution Department of Pediatrics, Universite de Montreal, CHU Sainte-Justine, Montreal, Canada. [email protected] Title Prevalence of cardiometabolic risk factors by weight status in a population-based sample of Quebec children and adolescents. Source Canadian Journal of Cardiology. 24(7):575-83, 2008 Jul. Abstract BACKGROUND: There are few data on the prevalence of cardiometabolic risk factors in population-based samples of overweight and obese youth. OBJECTIVES: To compare the prevalence of individual and multiple cardiometabolic risk factors across body mass index (BMI) categories in a population-based sample of youth. METHODS: In 1999, a school-based survey of a provincially representative sample of youth nine, 13 and 16 years of age was conducted in Quebec (1778 boys, 1835 girls). Overweight was defined as BMI in the 85th percentile or higher and lower than the 95th percentile of the Centers for Disease Control and Prevention 2000 growth charts, and obesity was defined as BMI in the 95th percentile or higher. Levels of total cholesterol, low-density lipoprotein cholesterol, apolipoprotein B, high-density lipoprotein cholesterol, triglycerides, insulin, glucose, C-reactive protein and systolic blood pressure were categorized as desirable, borderline or unfavourable. RESULTS: The ! proportions of overweight and obese participants were 14% and 10% in boys, and 14% and 7% in girls, respectively. With the exception of total cholesterol and low-density lipoprotein cholesterol in girls, and glucose in both sexes, the prevalence of all investigated risk factors (borderline or unfavourable) was significantly higher among overweight and obese participants. Almost one-third of obese participants had unfavourable levels of at least two of seven risk factors (apolipoprotein B, high-density lipoprotein cholesterol, triglycerides, insulin, glucose, C-reactive protein and systolic blood pressure) compared with 3% of normal weight participants (adjusted OR 15 and 18 in boys and girls, respectively). Thirty-four per cent of obese youth did not have unfavourable levels of any risk factor. CONCLUSION: There is marked heterogeneity in the association between excess weight and cardiometabolic risk factors. Nonetheless, the present study highlights a high prevalence of mu! ltiple risk factors in a population-based sample of overweight and obe se youth. Publication Type Comparative Study. Journal Article.
Result <47> Unique Identifier 18451781 Status MEDLINE Authors Skelton JA. DeMattia LG. Flores G. Authors Full Name Skelton, Joseph A. DeMattia, Laure G. Flores, Glenn. Institution Division of Pediatric Gastroenterology and Nutrition, Department of Pediatrics, Medical College of Wisconsin, Milwaukee, Wisconsin, USA. [email protected] Title A pediatric weight management program for high-risk populations: a preliminary analysis. Source Obesity. 16(7):1698-701, 2008 Jul. Abstract OBJECTIVE: To determine whether a multidisciplinary pediatric weight management program effectively improves BMI, BMI z- score, and cardiovascular risk factors (CVRFs) in high-risk populations. METHODS AND PROCEDURES: A retrospective chart review was performed on children seen in the NEW Kids Program at the Children's Hospital of Wisconsin, a family-based clinic that treats pediatric obesity using medical management, nutrition education, behavioral intervention, and physical activity. Inclusion criteria were program participation for >or=9 months and >4 visits. Analyses were performed to identify factors associated with pre- to postintervention changes in BMI, BMI z-score, and CVRF laboratory values. RESULTS: A total of 66 patients met inclusion criteria; the mean age was 11 years (s.d.+/-3.4), 56% were racial/ethnic minorities, 45% were Medicaid recipients, 48% resided in impoverished communities, and 38% had a BMI >or=40 kg/m(2). Of the 66 patients, 91% had more than one ! weight-related comorbidity, 88% had CVRFs, and the preintervention mean BMI was 37 kg/m(2). After the intervention, there was an overall increase in absolute BMI, but a small, yet significant decrease in BMI z-score (mean -0.03+/-0.16; P<0.05). There were significant pregroup to postgroup improvements in total cholesterol, low-density lipoprotein, and triglycerides levels (P<0.05). Insurance coverage, race/ethnicity, gender, age, and initial BMI were not significantly associated with changes in BMI or BMI z- score. DISCUSSION: A multidisciplinary pediatric weight management program can improve the weight status of high-risk populations, including minorities, Medicaid recipients, patients with multiple comorbidities and CVRFs, and the severely obese. Publication Type Journal Article.
Result <48> Unique Identifier 18451769 Status MEDLINE Authors I'Allemand D. Wiegand S. Reinehr T. Muller J. Wabitsch M. Widhalm K. Holl R. APV-Study Group. Authors Full Name I'Allemand, Dagmar. Wiegand, Susanna. Reinehr, Thomas. Muller, Jorg. Wabitsch, Martin. Widhalm, Kurt. Holl, Reinhard. APV-Study Group. Institution Children's Hospital of Eastern Switzerland, St Gallen, Switzerland. [email protected] Title Cardiovascular risk in 26,008 European overweight children as established by a multicenter database. Source Obesity. 16(7):1672-9, 2008 Jul. Abstract OBJECTIVE: Although the obesity epidemic is progressing in European children too, there is no consensus on the population- specific prevalence of comorbidities or efficient diagnostic strategies. Therefore, weight-related risk factors, their interrelationship, and association with biological parameters were assessed in a large group of overweight (OW) children, documented by an electronic database. METHODS AND PROCEDURES: Data of 26,008 children (age 12.6+/-2.9 years, 56% females) presented for OW (BMI >90th percentile) or obesity (>97th percentile) in 98 specialized centers were evaluated using a simple software (Adipositas Patienten Verlaufsbeobachtung (APV)) for standardized longitudinal documentation. After local anonymization, data were transmitted for central analysis including multiple logistic regression. RESULTS: A total of 5.9% of the children were normal weight, 41% obese (OB), and 37% extremely OB (>99.5th percentile, XXL; 41% of the girls). In 50%, at least one! risk factor and in 11% a cluster of two were found, comprising increased blood pressure (BP): 35.4%, dyslipidemia: 32% (total cholesterol: 14.1%, low-density lipoprotein (LDL)-cholesterol: 15.8%, high-density lipoprotein (HDL)-cholesterol: 11.1%, triglycerides: 14.3%), impaired glucose tolerance (IGtT): 6.5% and suspicion of diabetes: 0.7%. The degree of OW was inversely associated with HDL-cholesterol and directly with clustered risk factors, impaired glucose metabolism, increased BP and triglycerides (odds ratios (ORs) XXL vs. normal=6.15, >10, 4.3, 3.0 and 2.5, respectively), but not with LDL-cholesterol. DISCUSSION: In a very large cohort of young Europeans risk factors for cardiovascular (CV) diseases are frequently found, related to the degree of OW and tend to cluster, thus a comprehensive screening is justified in all OW or OB children. Electronic patient documentation is feasible in a large obesity care network. Publication Type Journal Article. Multicenter Study. Research Support, Non-U.S. Gov't.
Result <49> Unique Identifier 18421272 Status MEDLINE Authors Lumeng JC. Cardinal TM. Sitto JR. Kannan S. Authors Full Name Lumeng, Julie C. Cardinal, Tiffany M. Sitto, Jacinta R. Kannan, Srimathi. Institution Center for Human Growth and Development, University of Michigan, Ann Arbor, Michigan, USA. [email protected] Title Ability to taste 6-n-propylthiouracil and BMI in low-income preschool-aged children. Source Obesity. 16(7):1522-8, 2008 Jul. Abstract BACKGROUND: Sensitivity to the bitter compound 6-n-propylthiouracil (PROP) is genetically mediated. Sensitivity to PROP has been associated with weight status in both adults and children. OBJECTIVE: To determine whether there is an association between PROP sensitivity and BMI in low-income children of diverse race/ethnicity, among whom there is a high prevalence of obesity. METHODS AND PROCEDURES: Eighty-one preschool-aged children attending Head Start tasted a solution of 560 micromol/l PROP and reported whether it tasted "like water" or "like something else". Mothers reported child's race, age, maternal education, maternal weight and height, child's reluctance to sample new foods via the Food Neophobia Scale (FNS), and child's dietary intake using a food frequency questionnaire. Child weight and height were measured. BMI was calculated and for children, expressed in z-scores. Regression analyses were used to evaluate the relationship between child's PROP taster status an! d BMI z-score, testing covariates child's age, gender, race, maternal education and BMI, and child's FNS score. Children's dietary intake was compared by PROP taster status. RESULTS: PROP tasters, compared with nontasters, had significantly higher BMI z- scores (0.99 (s.d. 1.24) vs. 0.03 (1.12), P=0.004) and had a significantly higher prevalence of overweight (31.8% vs. 5.6%, P=0.025), but demonstrated no differences in reported dietary intake. The most parsimonious model predicting the child's BMI z- score included only maternal BMI and the child's PROP taster status (R(2)=22.3%). DISCUSSION: A genetically mediated ability to taste bitter may contribute to obesity risk in low-income, preschool-aged children. Publication Type Comparative Study. Journal Article.
Result <50> Unique Identifier 18421262 Status MEDLINE Authors Haworth CM. Plomin R. Carnell S. Wardle J. Authors Full Name Haworth, Claire M A. Plomin, Robert. Carnell, Susan. Wardle, Jane. Institution Social, Genetic and Developmental Psychiatry Centre, Institute of Psychiatry, King's College London, London, UK. [email protected] Title Childhood obesity: genetic and environmental overlap with normal-range BMI. Source Obesity. 16(7):1585-90, 2008 Jul. Abstract OBJECTIVE: To understand the overlap between the etiology of obesity and normal variation in BMI in children. METHODS AND PROCEDURES: Height and weight data were available from a large UK representative sample of twins: 2,342 same-sex pairs at 7 years and 3,526 same-sex pairs at 10 years. The twin method and model-fitting techniques were used to estimate genetic and environmental contributions to BMI. DeFries-Fulker (DF) extremes analysis was used to investigate genetic and environmental influences on the mean difference between obese and normal-weight children. Obesity was classified using the International Obesity Task Force (IOTF) criteria. RESULTS: At both ages, BMI and obesity were highly heritable (0.60-0.74) and only modestly influenced by shared environmental factors (0.12-0.22). Extremes analyses indicated that genetic and environmental influences on obesity are quantitatively and qualitatively similar to those operating across the range of BMI. DISCUSSION: Obesit! y is the extreme of the same genetic and environmental factors responsible for variation throughout the distribution of BMI. This finding implies that genes that influence obesity will also be associated with BMI in the normal range, and similar environmental influences will affect BMI in the clinical and normal range. Knowing that obesity is influenced by the same genetic and environmental factors that affect weight at all levels has implications for investigating the mechanisms for weight gain and developing interventions for weight control. Publication Type Journal Article. Multicenter Study. Research Support, Non-U.S. Gov't. Twin Study.
Result <51> Unique Identifier 18375449 Status MEDLINE Authors Benzinou M. Chevre JC. Ward KJ. Lecoeur C. Dina C. Lobbens S. Durand E. Delplanque J. Horber FF. Heude B. Balkau B. Borch-Johnsen K. Jorgensen T. Hansen T. Pedersen O. Meyre D. Froguel P. Authors Full Name Benzinou, Michael. Chevre, Jean-Claude. Ward, Kirsten J. Lecoeur, Cecile. Dina, Christian. Lobbens, Stephane. Durand, Emmanuelle. Delplanque, Jerome. Horber, Fritz F. Heude, Barbara. Balkau, Beverley. Borch-Johnsen, Knut. Jorgensen, Torben. Hansen, Torben. Pedersen, Oluf. Meyre, David. Froguel, Philippe. Institution CNRS 8090-Institute of Biology, Pasteur Institute, Lille, France. Title Endocannabinoid receptor 1 gene variations increase risk for obesity and modulate body mass index in European populations. Source Human Molecular Genetics. 17(13):1916-21, 2008 Jul 1. Abstract The therapeutic effects of cannabinoid receptor blockade on obesity-associated phenotypes underline the importance of the endocannabinoid pathway on the energy balance. Using a staged-approach, we examined the contribution of the endocannabinoid receptor 1 gene (CNR1) on obesity and body mass index (BMI) in the European population. With the input of CNR1 exons and 3' and 5' regions sequencing and HapMap database, we selected and genotyped 26 tagging single-nucleotide polymorphisms (SNPs) in 1932 obese cases and 1173 non-obese controls of French European origin. Variants that showed significant associations (P < 0.05) with obesity after correction for multiple testing were further tested in two additional European cohorts including 2645 individuals. For the identification of the potential causal variant(s), we further genotyped SNPs in high linkage disequilibrium (LD) with the obesity-associated variants. Of the 25 successfully genotyped CNR1 SNPs, 12 showed nominal evidenc! e of association with childhood obesity, class I and II and/or class III adult obesity (1.16 < OR < 1.40, 0.00003 < P < 0.04). Intronic SNPs rs806381 and rs2023239, which resisted correction for multiple testing were further associated with higher BMI in both Swiss obese subjects and Danish individuals. The genotyping of all know variants in partial LD (r(2) > 0.5) with these two SNPs in the initial case-control study, identified two better associated SNPs (rs6454674 and rs10485170). Our study of 5750 subjects shows that CNR1 variations increase the risk for obesity and modulate BMI in our European population. As CB1 is a drug target for obesity, a pharmacogenetic analysis of the endocannabinoid blockade obesity treatment may be of interest to identify best responders. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <52> Unique Identifier 18517076 Status MEDLINE Authors Henkin S. Brugge D. Bermudez OI. Gao X. Authors Full Name Henkin, Stanislav. Brugge, Doug. Bermudez, Odilla I. Gao, Xiang. Institution Department of Public Health and Family Medicine, Tufts University School of Medicine, Boston, Massachusetts 21111, USA. Title A case-control study of body mass index and asthma in Asian children. Source Annals of Allergy, Asthma, & Immunology. 100(5):447-51, 2008 May. Abstract BACKGROUND: The prevalence of obesity and asthma in the United States has increased in past decades. Numerous studies have focused on the relationship between the 2 factors. However, to our knowledge, this association in Asian Americans has not been extensively studied. OBJECTIVE: To assess the association between body mass index (BMI) and asthma in an Asian American pediatric population. METHODS: We conducted a case-control medical record review study of 94 pediatric patients with and without asthma at Tufts-New England Medical Center, Boston, Massachusetts. The BMI of asthmatic children before and after their asthma diagnosis was compared with the BMI of children without asthma. RESULTS: Multiple analyses showed no significant (P > .05) association between various measures of BMI and asthma in this population. After adjustment for atopic dermatitis, allergic rhinitis, and other allergies, the odds ratio in our longitudinal analysis using BMI greater than the 85th percent! ile for asthmatic children vs nonasthmatic children was 0.92 (95% confidence interval, 0.40-2.20). CONCLUSIONS: Either overweight and obesity do not lead to asthma in Asian immigrant children, consistent with our results, or something about our method limited our ability to observe the association. In either case, more research in the population is needed. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <53> Unique Identifier 18517029 Status MEDLINE Authors Horne J. Authors Full Name Horne, James. Title Too weighty a link between short sleep and obesity?[see comment][comment]. Comments Comment in: Sleep. 2008 Sep 1;31(9):1203; PMID: 18788643, Comment on: Sleep. 2005 Oct 1;28(10):1289-96; PMID: 16295214, Comment on: Sleep. 2007 Dec 1;30(12):1667-73; PMID: 18246976 Source Sleep. 31(5):595-6, 2008 May 1. Other ID Source: NLM. PMC2398750 Publication Type Comment. Letter.
Result <54> Unique Identifier 18517028 Status MEDLINE Authors Young T. Authors Full Name Young, Terry. Institution Department of Population Health Sciences, University of Wisconsin, Madison, WI, USA. [email protected] Title Increasing sleep duration for a healthier (and less obese?) population tomorrow.[see comment][comment]. Comments Comment in: Sleep. 2008 Sep 1;31(9):1203; PMID: 18788643, Comment on: Sleep. 2008 May 1;31(5):619-26; PMID: 18517032 Source Sleep. 31(5):593-4, 2008 May 1. Other ID Source: NLM. PMC2398749 Publication Type Comment. Journal Article.
Result <55> Unique Identifier 18460103 Status MEDLINE Authors Rockett H. Authors Full Name Rockett, Helaine. Institution Channing Laboratory, Brigham and Women's Hospital & Harvard Medical School, Boston, Massachusetts, USA. [email protected] Title Commentary on lack of association between television viewing, soft drinks, physical activity and body mass index in children. Source Acta Paediatrica. 97(6):699-700, 2008 Jun. Publication Type Journal Article.
Result <56> Unique Identifier 18402677 Status MEDLINE Authors Toschke AM. von Kries R. Beyerlein A. Ruckinger S. Authors Full Name Toschke, Andre M. von Kries, Rudiger. Beyerlein, Andreas. Ruckinger, Simon. Institution King's College London, Division of Health and Social Care Research, Department of Public Health Sciences, 7th Floor Capital House, 42 Weston St, London, SE1 3QD, UK. [email protected] Title Risk factors for childhood obesity: shift of the entire BMI distribution vs. shift of the upper tail only in a cross sectional study. Source BMC Public Health. 8:115, 2008. Other ID Source: NLM. PMC2322977 Abstract BACKGROUND: Previous studies reported an increase of upper body mass index (BMI) quantiles for formula fed infants compared to breastfed infants, while corresponding mean differences were low. The aim of this study was to assess the impact of known risk factors for childhood obesity on the BMI distribution. METHODS: Data on 4,884 children were obtained at obligatory school entry health examinations in Bavaria (Germany). Exposure variables were formula feeding, maternal smoking in pregnancy, excessive TV- watching, low meal frequency, poor parental education, maternal overweight and high infant weight gain. Cumulative BMI distributions and Tukey mean-difference plots were used to assess possible shifts of BMI distributions by exposure. RESULTS: Maternal overweight and high infant weight gain shifted the entire BMI-distribution with an accentuation on upper quantiles to higher BMI values. In contrast, parental education, formula feeding, high TV consumption, low meal frequenc! y and maternal smoking in pregnancy resulted in a shift of upper quantiles only. CONCLUSION: The single shifts among upper parts of the BMI distribution might be due to effect modification of the corresponding exposures by another environmental exposure or genetic predisposition. Affected individuals might represent a susceptible subpopulation of the exposed. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <57> Unique Identifier 18385507 Status MEDLINE Authors Kumar HK. Modi KD. Patnaik SK. Authors Full Name Kumar, Hari K V S. Modi, Kirti D. Patnaik, Saroj K. Title Adolescent overweight and coronary heart disease.[comment]. Comments Comment on: N Engl J Med. 2007 Dec 6;357(23):2371-9; PMID: 18057339 Source New England Journal of Medicine. 358(14):1521; author reply 1522, 2008 Apr 3. Publication Type Comment. Letter.
Result <58> Unique Identifier 18316661 Status MEDLINE Authors Epstein LH. Roemmich JN. Robinson JL. Paluch RA. Winiewicz DD. Fuerch JH. Robinson TN. Authors Full Name Epstein, Leonard H. Roemmich, James N. Robinson, Jodie L. Paluch, Rocco A. Winiewicz, Dana D. Fuerch, Janene H. Robinson, Thomas N. Institution Behavioral Medicine Laboratory, Department of Pediatrics, School of Medicine and Biomedical Sciences, State University of New York at Buffalo, Farber Hall, 3435 Main St, Room G56, Bldg 26, Buffalo, NY 14214-3000, USA. [email protected] Title A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children.[see comment]. Comments Comment in: Arch Pediatr Adolesc Med. 2008 Mar;162(3):283-4; PMID: 18316669, Comment in: Arch Pediatr Adolesc Med. 2008 Sep;162(9):899; author reply 899-900; PMID: 18762613 Source Archives of Pediatrics & Adolescent Medicine. 162(3):239-45, 2008 Mar. Other ID Source: NLM. NIHMS43558 Source: NLM. PMC2291289 Abstract OBJECTIVE: To assess the effects of reducing television viewing and computer use on children's body mass index (BMI) as a risk factor for the development of overweight in young children. DESIGN: Randomized controlled clinical trial. SETTING: University children's hospital. PARTICIPANTS: Seventy children aged 4 to 7 years whose BMI was at or above the 75th BMI percentile for age and sex. INTERVENTIONS: Children were randomized to an intervention to reduce their television viewing and computer use by 50% vs a monitoring control group that did not reduce television viewing or computer use. MAIN OUTCOME MEASURES: Age- and sex-standardized BMI (zBMI), television viewing, energy intake, and physical activity were monitored every 6 months during 2 years. RESULTS: Children randomized to the intervention group showed greater reductions in targeted sedentary behavior (P < . 001), zBMI (P < .05), and energy intake (P < .05) compared with the monitoring control group. Socioeconomic sta! tus moderated zBMI change (P = .01), with the experimental intervention working better among families of low socioeconomic status. Changes in targeted sedentary behavior mediated changes in zBMI (P < .05). The change in television viewing was related to the change in energy intake (P < .001) but not to the change in physical activity (P =.37). CONCLUSIONS: Reducing television viewing and computer use may have an important role in preventing obesity and in lowering BMI in young children, and these changes may be related more to changes in energy intake than to changes in physical activity. Publication Type Clinical Trial. Journal Article. Randomized Controlled Trial. Research Support, N.I.H., Extramural. Research Support, Non-U.S. Gov't.
Result <59> Unique Identifier 18174542 Status MEDLINE Authors Amin R. Anthony L. Somers V. Fenchel M. McConnell K. Jefferies J. Willging P. Kalra M. Daniels S. Authors Full Name Amin, Raouf. Anthony, Leonard. Somers, Virend. Fenchel, Matthew. McConnell, Keith. Jefferies, Jenny. Willging, Paul. Kalra, Maninder. Daniels, Stephen. Institution Cincinnati Children's Hospital Medical Center, Cincinnati, Ohio, USA. [email protected] Title Growth velocity predicts recurrence of sleep-disordered breathing 1 year after adenotonsillectomy.[see comment]. Comments Comment in: Am J Respir Crit Care Med. 2008 Jun 15;177(12):1399; PMID: 18522955, Comment in: Am J Respir Crit Care Med. 2008 Oct 15;178(8):882; PMID: 18832557 Source American Journal of Respiratory & Critical Care Medicine. 177(6):654-9, 2008 Mar 15. Other ID Source: NLM. PMC2267339 [Available on 03/15/09] Abstract RATIONALE: Adenotonsillectomy, the first line of treatment of sleep-disordered breathing (SDB), is the most commonly performed pediatric surgery. Predictors of the recurrence of SDB after adenotonsillectomy and its impact on cardiovascular risk factors have not been identified. OBJECTIVES: Demonstrate that gain velocity in body mass index (BMI) defined as unit increase in BMI/year confers an independent risk for the recurrence of SDB 1 year after adenotonsillectomy. METHODS: Children with SDB and hypertrophy of the tonsils and a comparison group of healthy children were followed prospectively for 1 year. MEASUREMENTS AND MAIN RESULTS: Serial polysomnographies, BMI, and blood pressure were obtained before adenotonsillectomy and 6 weeks, 6 months, and 1 year postoperatively. Gain velocity in BMI, BMI and being African American (odds ratios, 4-6/unit change/yr; 1.4/unit and 15, respectively) provided equal amounts of predictive power to the risk of recurrence of SDB. In the g! roup that experienced recurrence, systolic blood pressure at 1 year was higher than at baseline and higher than in children who did not experience recurrence. CONCLUSIONS: Three clinical parameters confer independent increased risk for high recurrence of SDB after adenotonsillectomy: gain velocity in BMI, obesity, and being African American. A long-term follow-up of children with SDB and monitoring of gain velocity in BMI are essential to identifying children at risk for recurrence of SDB and in turn at risk for hypertension. Publication Type Journal Article. Research Support, N.I.H., Extramural.
Result <60> Unique Identifier 18310186 Status MEDLINE Authors Eijkemans M. Mommers M. de Vries SI. van Buuren S. Stafleu A. Bakker I. Thijs C. Authors Full Name Eijkemans, Marianne. Mommers, Monique. de Vries, Sanne I. van Buuren, Stef. Stafleu, Annette. Bakker, Ingrid. Thijs, Carel. Institution Department of Epidemiology, Nutrition, and Toxicology Research, Institute Maastricht (Nutrim) and School of Public Health and Primary Care (Caphri), Maastricht University, Maastricht, The Netherlands. Title Asthmatic symptoms, physical activity, and overweight in young children: a cohort study. Source Pediatrics. 121(3):e666-72, 2008 Mar. Abstract OBJECTIVE: Prevalence of asthma and overweight has increased simultaneously during the past decades. Several studies have reported an association between these two health problems, but it is unclear whether this relation is causal. We hypothesize that children with asthmatic symptoms are less physically active, which may contribute to the development of overweight. PATIENTS AND METHODS: The study included children from the KOALA Birth Cohort Study who were invited at 4 to 5 years of age to wear an Actigraph accelerometer for 5 days (n = 305; 152 boys). Information on wheezing was gathered by repeated questionnaires completed by parents at child ages 7 months and 1, 2, and 4 to 5 years. Questionnaires on physical activity were completed at child age 4 to 5 years, and height, weight, and abdominal circumference were measured. Accelerometer data were expressed as mean counts per minute, minutes per day performing vigorous activity, and moderate-to-vigorous physical activity d! uring > or = 1 minute. RESULTS: Children who had wheezed in the last 12 months showed very similar activity levels compared with children who had never wheezed. By contrast, boys who had wheezed at least once but not in the last 12 months were more physically active than boys who had never wheezed (geometric mean: 694 vs 625 cpm; adjusted geometric mean ratio: 1.11). This was not found for girls. Similar results were found in parent-reported physical activity data. No association was found between wheezing at any age and overweight at the age of 4 to 5 years. CONCLUSIONS: These results do not support our hypothesis and previous studies that showed that wheezing children are less physically active. Our data provide no evidence that asthmatic symptoms induce a lower physical activity level and more overweight. Additional research could concentrate on the effect of physical activity and overweight on the development of asthmatic symptoms. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <61> Unique Identifier 18239560 Status MEDLINE Authors Pinhas-Hamiel O. Frumin K. Gabis L. Mazor-Aronovich K. Modan-Moses D. Reichman B. Lerner-Geva L. Authors Full Name Pinhas-Hamiel, Orit. Frumin, Katia. Gabis, Lidia. Mazor-Aronovich, Kineret. Modan-Moses, Dalit. Reichman, Brian. Lerner-Geva, Liat. Institution Pediatric Endocrinology and Diabetes Unit, Edmond and Lily Safra Children's Hospital, Sheba Medical Center, Tel Hashomer, Ramat-Gan, Israel. [email protected] Title Headaches in overweight children and adolescents referred to a tertiary-care center in Israel. Source Obesity. 16(3):659-63, 2008 Mar. Abstract OBJECTIVE: To assess the association between obesity and primary headaches in children and adolescents. METHODS AND PROCEDURES: In a prospective study, the short-questionnaire version based on existing International Headache Society diagnostic criteria was administered. Two hundred and seventy-three children and adolescents (61% females) aged 9-17 years were assessed. One hundred and sixteen (42.5%) subjects were of normal weight, 45 (16.5%) were at risk for overweight (BMI >85th and <95th percentile for age and gender) and 112 (41%) were overweight (BMI >/=95th percentile). The outcome measures were prevalence of headaches, type of headaches, association between headaches and elevated blood pressure in overweight subjects. RESULTS: Headache was reported in 39 (14.3%) subjects, with a similar rate in females (14.5%) and males (14%). Among 39 subjects with headaches, 20 (17.9%) were overweight, 7 (15.6%) were at risk for overweight and 12 (10.3%) were normal-weight children! . Among females, 7.7% of normal-weight group suffered from headaches, compared with 14.8% of the at risk for overweight group and 20.3% of the overweight group (P for trend 0.04). Among males, the occurrence of headaches was similar in all three weight groups (P = 0.96). The occurrence of headaches increased from 10.6% among children aged 9-11 years to 21.8% in the 15- 18 years age group (P < 0.05). In multivariate analysis, a significant independent risk for headaches was present in overweight females (odds ratio (OR) = 3.93, 95% confidence interval (CI) 1.28-12.1) and in adolescents aged 15-18 years (OR = 2.62, 95% CI 1.07-6.45).Elevated blood pressure was not independently associated with headaches. Of the 15 children with migraine, 12 were either at risk for overweight or overweight. DISCUSSION: Overweight females had an almost fourfold excess risk of headaches when compared with normal-weight girls. Publication Type Journal Article.
Result <62> Unique Identifier 18277189 Status MEDLINE Authors Rebelo D. Teixeira J. Marques-Vidal P. Oliveira JM. Authors Full Name Rebelo, Duarte. Teixeira, Joana. Marques-Vidal, Pedro. Oliveira, Joao Miguel. Institution Nutrition and Metabolism Unit, Instituto de Medicina Molecular, Bugnon, Lausanne, Switzerland. Title Obesity markers and blood pressure in a sample of Portuguese children and adolescents. Source European Journal of Cardiovascular Prevention & Rehabilitation. 15(1):73-7, 2008 Feb. Abstract BACKGROUND: Little information exists regarding the effect of several obesity markers on blood pressure (BP) levels in youth. DESIGN: Transverse study including 2494 boys and 2589 girls. METHODS: Height, weight and waist were measured according to the international criteria and body fat (BF) by bioimpedance. BP was measured by an automated device. Hypertension was defined using sex-specific, age-specific and height-specific observation-points. RESULTS: Body mass index (BMI) and waist were positively related with systolic blood pressure (SBP) and diastolic blood pressure (DBP) and heart rate in both sexes, whereas the relationships with BF were less consistent. Stepwise linear regression analysis showed that BMI was positively related with SBP and DBP in both sexes, whereas BF was negatively related with SBP in both sexes and with heart rate in boys only; finally, waist was positively related with SBP in boys and heart rate in girls. Age and heart rate-adjusted values of SB! P and DBP increased with BMI: for SBP, 117+/-1, 123+/-1 and 124+/-1 mmHg in normal, overweight and obese boys, respectively; corresponding values for girls were 111+/-1, 114+/-1 and 116+/-2 mmHg (mean+/-SE, P<0.001). Overweight and obese boys had an odds ratio for being hypertensive of 2.26 (95% confidence interval: 1.79-2.86) and 3.36 (2.32-4.87), respectively; corresponding values for girls were 1.58 (confidence interval 1.25-1.99) and 2.31 (1.53-3.50). CONCLUSION: BMI, not BF or waist, is consistently and independently related to BP levels in children; overweight and obesity considerably increase the risk of hypertension. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <63> Unique Identifier 18223627 Status MEDLINE Authors Vortmann M. Eisner MD. Authors Full Name Vortmann, Michael. Eisner, Mark D. Institution Division of Occupational and Environmental Medicine and Division of Pulmonary and Critical Care Medicine, Department of Medicine, University of California, San Francisco, California, USA. Title BMI and health status among adults with asthma. Source Obesity. 16(1):146-52, 2008 Jan. Abstract BACKGROUND: A convincing body of literature links obesity with a higher risk for developing adult-onset asthma. The impact of obesity on asthma severity among adults with pre-existing asthma, however, is less clear. METHODS AND PROCEDURES: In a prospective cohort study of 843 adults with severe asthma, we studied the impact of BMI on asthma health status. RESULTS: The prevalence of obesity and overweight were 44% (95% confidence interval (CI) 41-47%) and 28% (95% CI 25-32%). The obese BMI group was associated with a higher risk for daily or near daily asthma symptoms than was the normal BMI group (odds ratio (OR) 1.81; 95% CI 1.10-2.96). Compared to the normal BMI group, generic physical health status was worse in the overweight (mean score decrement -2.42 points; 95% CI -4.39 to -0.45) and the obese groups (-6.31 points; 95% CI -8.14 to -4.49). Asthma- specific quality of life was worse in the underweight (mean score increment 8.66 points; 95% CI 2.53-14.8) and obese group! s (4.51 points; 95% CI 2.21-6.81), compared to those with normal BMI. Obese persons also had a higher number of restricted activity days that past month (5.05 days; 95% CI 2.90-7.19 days). DISCUSSION: It appears that obesity has a substantive negative effect on health status among adults with asthma. Further work is needed to clarify the precise mechanisms. Clinicians should counsel dietary modification and weight loss for their overweight and obese patients with asthma. Publication Type Journal Article. Research Support, N.I.H., Extramural. Research Support, U.S. Gov't, Non-P.H.S..
Result <64> Unique Identifier 17579635 Status MEDLINE Authors Harding S. Maynard MJ. Cruickshank K. Teyhan A. Authors Full Name Harding, S. Maynard, M J. Cruickshank, K. Teyhan, A. Institution MRC Social and Public Health Sciences Unit, Glasgow, UK. [email protected] Title Overweight, obesity and high blood pressure in an ethnically diverse sample of adolescents in Britain: the Medical Research Council DASH study. Source International Journal of Obesity. 32(1):82-90, 2008 Jan. Abstract OBJECTIVES: To examine the impact of overweight on mean, high normal and high blood pressure in early adolescence, and how this relates to ethnicity and socio-economic status. DESIGN: Cross-sectional study with anthropometric and blood pressure measurements. SETTING: A total of 51 secondary schools in London. SAMPLE: A total of 6407 subjects, 11-13 years of age, including 1204 White UK, 698 Other Whites, 911 Black Caribbeans, 1065 black Africans, 477 Indians and 611 Pakistanis/Bangladeshis. MAIN OUTCOME MEASURES: Mean, high normal (gender, age and height-percentile-specific 90-94th percentile) and high (>/=95th percentile) blood pressure. RESULTS: Based on the International Obesity Task Force age-specific thresholds, 19% of boys and 23% of girls were overweight, and 8% of each were obese. Overweight and obesity were associated with large increases in the prevalence of high normal and high blood pressures compared with those not overweight. The increases in the prevalence o! f high systolic pressure associated with overweight were as follows: boys, odds ratio 2.50 (95% confidence intervals 1.73-3.60) and girls 3.39 (2.36-4.85). Corresponding figures for obesity were: boys 4.31 (2.82-6.61) and girls 5.68 (3.61-8.95). Compared with their White British peers, obesity was associated with larger effects on blood pressure measures only among Indians, despite more overweight and obesity among black Caribbean girls and overweight among Black African girls. The effect of socio-economic status was inconsistent. CONCLUSIONS: The tendency to high blood pressure among adult Black African origin populations was not evident at these ages. These results suggest that the rise in obesity in adolescence portends a rise in early onset of cardiovascular disease across ethnic groups, with Indians appearing to be more vulnerable. Publication Type Journal Article.
Result <65> Unique Identifier 18175229 Status MEDLINE Authors Cogan JC. Smith JP. Maine MD. Authors Full Name Cogan, Jeanine C. Smith, Joslyn P. Maine, Margo D. Institution Eating Disorders Coalition for Research, Policy & Action, USA. [email protected] Title The risks of a quick fix: a case against mandatory body mass index reporting laws. Source Brunner-Mazel Eating Disorders Monograph Series. 16(1):2-13, 2008 Jan-Feb. Abstract As the United States addresses obesity, a number of state legislatures are considering laws that require schools to track and report students' body mass index (BMI), a measurement of body weight (weight/height2). This article describes the state level activity on mandatory BMI reporting, offers numerous arguments against this practice, and suggests an alternative approach to promoting health in youth. Mandatory BMI reporting laws place a new and inappropriate responsibility on the schools. Proponents of such laws imply that BMI reporting will have positive outcomes, yet there is virtually no independent research to support this assumption. The authors argue that these laws could do significant harm, including an increased risk for children to develop eating disorder symptoms. Publication Type Journal Article.
Result <66> Unique Identifier 18156567 Status MEDLINE Authors Taylor B. Mannino D. Brown C. Crocker D. Twum-Baah N. Holguin F. Authors Full Name Taylor, B. Mannino, D. Brown, C. Crocker, D. Twum-Baah, N. Holguin, F. Institution Emory University, Atlanta, Georgia, USA. Title Body mass index and asthma severity in the National Asthma Survey.[see comment]. Comments Comment in: Thorax. 2008 Jul;63(7):659; PMID: 18587041 Source Thorax. 63(1):14-20, 2008 Jan. Abstract BACKGROUND: The association between obesity and asthma severity remains controversial and limited to small studies. METHODS: We determined the association of body mass index (BMI) and asthma severity in the National Asthma Survey. We included adults (age > or = 18 years) who self-reported symptoms of asthma in the past 5 years. A total of 3095 patients were divided into the following BMI categories: 1080 (35%) non-overweight (BMI < 25), 993 (32%) overweight (BMI > or = 25 and < 30) and 1022 (33%) obese (BMI > or = 30). Asthma severity measures included respiratory symptoms, healthcare utilisation, medication use, missed work days and the Global Initiative for Asthma (GINA) severity classification. Models were adjusted for: gender, race, age, education, income, employment status, smoking status, family history of asthma, state of residence and residence in a metropolitan statistical area. RESULTS: Compared with non-overweight subjects, obese subjects with asthma were more l! ikely to report continuous symptoms (OR 1.66, 95% CI 1.09 to 2.54), miss more work days (OR 1.35, 95% CI 1.01 to 1.81), use short acting beta agonists (OR 1.36, 95% CI 1.06 to 1.75), use inhaled corticosteroids (OR 1.34, 95% CI 1.01 to 1.79) and use any controller medication according to GINA guidelines (OR 1.37, 95% CI 1.01 to 1.85). Also, obese respondents were less likely to be in asthma remission (OR 0.56, 95% CI 0.38 to 0.82) and were more likely to have severe persistent asthma (GINA IV) (OR 1.42, 95% CI 1.05 to 1.90). CONCLUSIONS: In a large, diverse sample of adults with asthma, obesity was associated with measures of asthma severity after adjusting for potential confounders. Publication Type Journal Article. Multicenter Study. Research Support, N.I.H., Extramural. Research Support, Non-U.S. Gov't. Research Support, U.S. Gov't, P.H.S..
Result <67> Unique Identifier 17573441 Status MEDLINE Authors Misso NL. Petrovic N. Grove C. Celenza A. Brooks-Wildhaber J. Thompson PJ. Authors Full Name Misso, N L A. Petrovic, N. Grove, C. Celenza, A. Brooks-Wildhaber, J. Thompson, P J. Institution Lung Institute of Western Australia (Inc.), Centre for Asthma, Allergy and Respiratory Research, The University of Western Australia, Perth, Australia. [email protected] Title Plasma phospholipase A2 activity in patients with asthma: association with body mass index and cholesterol concentration. Source Thorax. 63(1):21-6, 2008 Jan. Abstract BACKGROUND: Secretory phospholipases A2 (sPLA2) have functions relevant to asthmatic inflammation, including eicosanoid synthesis and effects on dendritic cells and T cells. The aim of this study was to measure sPLA2 activity in patients with stable and acute asthma and to assess potential associations with body mass index (BMI), and plasma cholesterol and vitamin C concentrations. METHODS: Plasma sPLA2 activity and concentrations of cholesterol and vitamin C were measured in 23 control subjects and 61 subjects with stable asthma (42 mild to moderate, 19 severe). In addition, sPLA2 activity was measured in 36 patients experiencing acute asthma and in 22 of these patients after recovery from the acute attack. RESULTS: sPLA2 activity was not significantly greater in severe (499.9 U; 95% confidence interval (CI) 439.4 to 560.4) compared with mild to moderate asthmatic subjects (464.8; 95% CI 425.3 to 504.3) or control subjects (445.7; 95% CI 392.1 to 499.4), although it was h! igher in patients with acute asthma (581.6; 95% CI 541.2 to 622.0; p<0.001). Male gender, high plasma cholesterol, increased BMI and atopy were associated with increased sPLA2 activity, while plasma vitamin C was inversely correlated with sPLA2 activity in patients with stable asthma and in control subjects. There were significant interactions between gender and plasma cholesterol and between gender and vitamin C in relation to sPLA2 activity. CONCLUSIONS: Plasma sPLA2 may provide a biological link between asthma, inflammation, increased BMI, lipid metabolism and antioxidants. Interactions among these factors may be pertinent to the pathophysiology and increasing prevalence of both asthma and obesity. Publication Type Journal Article.
Result <68> Unique Identifier 17931348 Status MEDLINE Authors Albertini A. Tripodi A. Fabbri A. Mattioli M. Cavrini G. Cecchetti R. Dalle Donne E. Cortesi C. De Giorgi S. Contarini V. Andreotti L. Veronesi B. Stefanelli I. Di Martino E. Authors Full Name Albertini, A. Tripodi, A. Fabbri, A. Mattioli, M. Cavrini, G. Cecchetti, R. Dalle Donne, E. Cortesi, C. De Giorgi, S. Contarini, V. Andreotti, L. Veronesi, B. Stefanelli, I. Di Martino, E. Institution Nutrition and Food Health Services, Nutritional team, Region of Emilia-Romagna, Modena, Italy. Title Prevalence of obesity in 6- and 9-year-old children living in Central-North Italy. Analysis of determinants and indicators of risk of overweight. Source Obesity Reviews. 9(1):4-10, 2008 Jan. Abstract The objective of our article is to survey the prevalence of overweight and obesity among 6- and 9-year-old children in Emilia- Romagna, a region of Central-North Italy, and to study the eating habits and behaviours of these children and their families. During 2003 and 2005, we analysed a stratified sample of the general population of children attending pre-school (2681 children aged 6 years) and primary school (2955 children aged 9 years). Their height and weight were measured by healthcare workers. In the 6- year-old children, information concerning their eating habits was collected by means of a questionnaire completed by their parents. The prevalence of overweight was 16.5% in 6-year-old children and 20.6% in 9-year-old children. The increase of overweight from 6- to 9-year-old children was observed in males (13.5% in 6-year-old/21.3% in 9-year-old boys), but not in females. The prevalence of obesity was 8.9% in children aged 6 years and 9.0% in those aged 9 years, and it! was higher in comparison with Italian surveys carried out in 1993 and in 2001: 7.5% in 6-year-old and 7.8% in 9-year-old children in 1993, and 6.6% in 6-year-old and 7.2% in 9-year-old children in 2001. In pre-school children, overweight and obesity were closely influenced by the education level, occupation and nutritional status of the parents. Publication Type Journal Article.
Result <69> Unique Identifier 18053018 Status MEDLINE Authors Jacobson JS. Mellins RB. Garfinkel R. Rundle AG. Perzanowski MS. Chew GL. Andrews HF. Goldstein IF. Authors Full Name Jacobson, J S. Mellins, R B. Garfinkel, R. Rundle, A G. Perzanowski, M S. Chew, G L. Andrews, H F. Goldstein, I F. Institution Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, NY 10032, USA. Title Asthma, body mass, gender, and Hispanic national origin among 517 preschool children in New York City. Source Allergy. 63(1):87-94, 2008 Jan. Abstract BACKGROUND: Striking differences in asthma prevalence have been reported among Hispanic adults and children living in different cities of the USA. Prevalence is highest among those of Puerto Rican and lowest among those of Mexican origin. We hypothesized that body size would mediate this association. METHODS: Parents of children in New York City Head Start programs completed a questionnaire including demographic factors, health history, a detailed history of respiratory conditions, lifestyle, and home environment. Children's height and weight were measured in home visits. Logistic regression was used to model the association of asthma with body mass index percentile (<85th percentile, gender/age specific vs>or=85th percentile, gender/age specific), national origin, and other factors. RESULTS: Of 517 children at mean age of 4.0 +/- 0.6 years, 34% met the study criteria for asthma, and 43% were above the 85th percentile. Asthma was strongly associated with non-Mexican nation! al origin, male gender, allergy symptoms, and maternal asthma, and marginally with body size. The odds of asthma among boys of non-Mexican origin was 5.9 times that among boys of Mexican origin [95% confidence interval (CI): 2.9-12.2]; the comparable odds ratio (OR) among girls was 1.8 (95% CI: 0.9-3.6). Body mass was associated with asthma among girls [OR = 2.0 (95% CI: 1.1- 3.7)], but not boys [OR = 1.4 (95% CI: 0.8-2.6)]. CONCLUSIONS: The association of asthma with both body mass and national origin was gender-specific among the children in our study. Ours is one of the first studies to report on pediatric asthma in different Hispanic populations in the same city, by gender. Publication Type Journal Article. Research Support, N.I.H., Extramural.
Result <70> Unique Identifier 18097866 Status MEDLINE Authors Davis A. Lipsett M. Milet M. Etherton M. Kreutzer R. Authors Full Name Davis, Adam. Lipsett, Michael. Milet, Meredith. Etherton, Melody. Kreutzer, Richard. Institution American Lung Association of California, Emeryville, CA 94608, USA. [email protected] Title An association between asthma and BMI in adolescents: results from the California Healthy Kids Survey. Source Journal of Asthma. 44(10):873-9, 2007 Dec. Abstract We examined the relationship between asthma prevalence and BMI in a cross-sectional survey of 471,969 adolescents. The size of the survey allowed us to investigate this relationship with much greater resolution than previously possible. Both lifetime and current asthma prevalence increased monotonically with increasing BMI, starting with individuals as low as the 45th to 55th percentiles of BMI. The pattern was similar between males and females and among six racial/ethnic groups. The results suggest that weight reduction even among persons not classified as overweight or obese may be an important component of asthma management. Publication Type Journal Article. Research Support, U.S. Gov't, P.H.S..
Result <71> Unique Identifier 17928281 Status MEDLINE Authors Chrzanowska M. Koziel S. Ulijaszek SJ. Authors Full Name Chrzanowska, Maria. Koziel, Slawomir. Ulijaszek, Stanlej J. Institution Department of Anthropology, Academy of Physical Education, Av. Jana Pawla II 78, 31-571 Krakow, Poland. wachrzan@cyf- kr.edu.pl Title Changes in BMI and the prevalence of overweight and obesity in children and adolescents in Cracow, Poland, 1971-2000. Source Economics & Human Biology. 5(3):370-8, 2007 Dec. Abstract The aim of this study is to examine changes in prevalence of overweight and obesity, using International Obesity Task Force criteria, in three cohorts of children and youth living in Cracow, Poland, in 1971, 1983 and 2000. Rates of overweight and obesity doubled among boys and girls, from 7.5% and 6.5% in 1971, to 15.2% and 11.8% in the year 2000. The greatest increases in prevalence occurred in the youngest age groups (7-12 years for boys and 7-10 years for girls), increases being less extensive among adolescents, and lowest of all in the oldest age groups (16-18 years in boys and 14-18 years in girls). The absence of a positive secular trend in BMI among adolescent females relative to males may be due to sociocultural pressures associated with transition to a free market economy in Poland. The extent to which girls attempt to achieve the ideal body, as portrayed by media and society more generally, increases across adolescence. Publication Type Journal Article.
Result <72> Unique Identifier 17890469 Status MEDLINE Authors Rodrigo GJ. Plaza V. Authors Full Name Rodrigo, Gustavo J. Plaza, Vicente. Institution Departamento de Emergencia, Hospital Central de las FF.AA, Av. 8 de Octubre 3020, Montevideo 11600, Uruguay. [email protected] Title Body mass index and response to emergency department treatment in adults with severe asthma exacerbations: a prospective cohort study. Source Chest. 132(5):1513-9, 2007 Nov. Abstract BACKGROUND: In acute asthma (AA), overweight/obesity (body mass index [BMI]>or=25 kg/m2) have been related to poorer outcomes and higher risk of complications. METHODS: We designed a prospective cohort study to determine if overweight/obese adults with severe episodes of AA require longer duration of emergency department (ED) treatment and have higher hospitalization rates compared with underweight/normal asthmatics (BMI<25 kg/m2). All patients received inhaled albuterol (maximum 6 h). Patients were discharged or admitted according to standard accepted criteria. The weight and height of each patient were measured during the ED stay. RESULTS: Four hundred twenty-six patients (mean, 33.4+/-11.5 years [+/-SD]; 63% women) with severe exacerbations (FEV1, 28.2+/-11.9% of predicted) were enrolled. One hundred sixty-three patients (38.3%) were classified as overweight/obese. Patients with BMI>or=25 kg/m2 showed significant increases in length of ED stay (2.3 h vs 1.9 h, p=0.01) a! nd rate of hospitalization (13.7% vs 6.8%, p=0.02), despite adjustments for other confounding variables. They also presented a higher rate of use of inhaled steroids and theophylline within the past 7 days. At the end of treatment, overweight/obese patients displayed more wheezing. Multivariate analysis demonstrated that BMI>or=25 kg/m2 resulted unrelated to final change in peak expiratory flow from baseline. By contrast, BMI>or=25 kg/m2 was related with duration of ED treatment (p=0.002). CONCLUSIONS: Overweight/obese patients were admitted to the hospital more frequently than underweight/normal patients. This may reflect a difference in the perception of dyspnea, or it may reflect an underlying difference in asthma severity between the two groups. Publication Type Journal Article.
Result <73> Unique Identifier 17923271 Status MEDLINE Authors Liu JM. Ye R. Li S. Ren A. Li Z. Liu Y. Li Z. Authors Full Name Liu, Jian-Meng. Ye, Rongwei. Li, Song. Ren, Aiguo. Li, Zhiwen. Liu, Yinghui. Li, Zhu. Institution Institute of Reproductive and Child Health and National Center for Maternal and Infant Health, Peking University Health Science Center, Beijing, People's Republic of China. [email protected] Title Prevalence of overweight/obesity in Chinese children. Source Archives of Medical Research. 38(8):882-6, 2007 Nov. Abstract BACKGROUND: The purpose of this paper was to report the prevalence of overweight/obesity by area, age, and gender in the year 2000 and to explore at what age adiposity rebound as measured by BMI occurs for Chinese children. METHODS: A cross-sectional study was carried out among 262,738 children aged 3.5-6.4 years in 26 counties/cities in China. Weight and height were measured from March 2000 through July 2000 by local trained health workers. International age- and gender-specific BMI cut-off points were used to obtain comparable prevalence rates of overweight/obesity. Multiple logistic regression was used to estimate odds ratios (OR) of being overweight/obesity for different comparisons. RESULTS: There were 19,390 overweight (16,738) or obese (2,652) children, resulting in an overall prevalence rate of 7.4% (95% CI: 7.3-7.5%). Girls were more likely to be overweight or obese than boys (OR = 1.14, 95% CI: 1.11-1.17). Compared with children living in the southern urban area,! multivariate ORs for those living in northern rural and southern rural areas were 2.58 and 1.15, respectively. Compared with children aged 6.0-6.4 years old, multivariate ORs for children aged 3.5, 4.0, 4.5, 5.0 and 5.5 years were 1.96, 1.88, 1.56, 1.53, and 1.11, respectively (p<0.001). CONCLUSIONS: Childhood overweight/obesity in Chinese children in 2000 is similar to the conditions of Great Britain or the U.S. in the 1980s or earlier. Age at adiposity rebound as measured by BMI for Chinese children is >6.5 years old. Publication Type Comparative Study. Journal Article. Research Support, Non-U.S. Gov't.
Result <74> Unique Identifier 17903329 Status MEDLINE Authors Aranceta J. Perez-Rodrigo C. Serra-Majem L. Bellido D. de la Torre ML. Formiguera X. Moreno B. Authors Full Name Aranceta, Javier. Perez-Rodrigo, Carmen. Serra-Majem, Lluis. Bellido, Diego. de la Torre, Martin Lopez. Formiguera, Xavier. Moreno, Basilio. Institution Commmunity Nutrition Unit, Bilbao Department of Public Health, University of Navarra, Pamplona, Spain. [email protected] Title Prevention of overweight and obesity: a Spanish approach. [Review] [49 refs] Source Public Health Nutrition. 10(10A):1187-93, 2007 Oct. Abstract BACKGROUND: Obesity is considered a major public health issue in most developed countries nowadays. This paper provides an overview of current population data available in Spain and the approach to develop preventive strategies in the country. METHODS: Review of population data available is based on individually measured weight and height as well as determinants. On this basis, the approach used in the country to develop preventive strategies is discussed. RESULTS: According to the DORICA study, the prevalence of obesity (BMI >or=30 kg m-2) is 15.5% in Spanish adults aged 25-60 years (13.2% in men and 17.5% in women). Obesity rates are higher among women aged 45 years and older, low social class, living in semi-urban places. Population estimates for the prevalence of obesity in Spanish children and young people based on the enKid study are 13.9% for the whole group. In this study, overweight and obesity is related to absence of breastfeeding, low consumption of fruit and v! egetables, high consumption of cakes, buns, softdrinks and butchery products, low physical activity levels and a positive association with time spent watching TV. In 2005, the Spanish Ministry of Health jointly with the Spanish Agency for Food Safety and Nutrition launched the multifaceted NAOS strategy for nutrition, physical activity and the prevention of obesity. The important role of the family and the school setting as well as the responsibility of the Health Administration and Pediatric Care in the prevention of obesity is highlighted in the document. The need for environmental actions is recognised. The PERSEO programme, a multicomponent school-based intervention project is part of the strategy currently in place.Conclusion: Obesity is a public health issue in Spain. A national multifaceted strategy was launched to counteract the problem. Environmental and policy actions are a priority. Young children and their families are among the main target groups. [References: ! 49] Publication Type Journal Article. Review.
Result <75> Unique Identifier 17904934 Status MEDLINE Authors Novotny R. Coleman P. Tenorio L. Davison N. Camacho T. Ramirez V. Vijayadeva V. Untalan P. Tudela MD. Authors Full Name Novotny, Rachel. Coleman, Patricia. Tenorio, Lynn. Davison, Nicola. Camacho, Tayna. Ramirez, Vickie. Vijayadeva, Vinutha. Untalan, Pedro. Tudela, Margaret Diaz. Institution Department of Human Nutrition, Food and Animal Sciences, University of Hawaii at Manoa, Honolulu 96822, USA. [email protected] Title Breastfeeding is associated with lower body mass index among children of the Commonwealth of the Northern Mariana Islands. [see comment]. Comments Comment in: J Am Diet Assoc. 2007 Oct;107(10):1701; PMID: 17904923 Source Journal of the American Dietetic Association. 107(10):1743-6, 2007 Oct. Abstract OBJECTIVE: To describe the prevalence of breastfeeding and overweight in the Commonwealth of the Northern Mariana Islands (CNMI), and the relationship between the two. DESIGN AND METHODS: A random cluster survey of 420 children (aged 6 months to 10 years), was conducted in the CNMI in June and July of 2005. Children were measured for weight and height and caregivers were asked about past feeding habits by trained investigators. RESULTS: Seventy-three percent of children were ever breastfed; 53% were still breastfed at 6 months, and 22% at 1 year of age. Five percent of children were found to be underweight (<5th percentile), while 15% were at risk for overweight (85th to <95th percentile) and 19% were overweight (>95th percentile), according to the Centers for Disease Control and Prevention body mass index for age reference data. Children who had been breastfed had a substantially lower body mass index than children who had not breastfed, after adjusting for age, sex, birt! hweight, and years of mother's education. DISCUSSION: These findings will be used to guide program development in the CNMI. Publication Type Journal Article. Research Support, U.S. Gov't, Non-P.H.S..
Result <76> Unique Identifier 17855436 Status MEDLINE Authors Blair NJ. Thompson JM. Black PN. Becroft DM. Clark PM. Han DY. Robinson E. Waldie KE. Wild CJ. Mitchell EA. Authors Full Name Blair, Nikki J. Thompson, John M D. Black, Peter N. Becroft, David M O. Clark, Phillipa M. Han, Dug Yeo. Robinson, Elizabeth. Waldie, Karen E. Wild, Chris J. Mitchell, Edwin A. Institution Department of Paediatrics, University of Auckland, Auckland, New Zealand. Title Risk factors for obesity in 7-year-old European children: the Auckland Birthweight Collaborative Study. Source Archives of Disease in Childhood. 92(10):866-71, 2007 Oct. Abstract OBJECTIVE: To identify risk factors associated with obesity in primary school children, with a particular focus on those which can be modified. To identify critical periods and growth patterns in the development of childhood obesity. METHODS: 871 New Zealand European children were enrolled in a longitudinal study at birth and data were collected at birth, 1, 3.5 and 7 years of age. Data collected at 7 years included weight, height, bioelectrical impedance analysis (BIA), television viewing time and a 24 h body movement record (actigraphy). The outcome measure was percentage body fat (PBF), which was calculated at 3.5 and 7 years using BIA. Univariate and multiple regression analyses were carried out using PBF as a continuous variable. RESULTS: Multivariable analysis found maternal overweight/obesity, maternal age, female gender, sedentary activity time and hours of television viewing to be independently associated with PBF at 7 years. Growth variables (birth weight, rapid ! weight gain in infancy, early (1-3.5 years) and middle childhood (3.5-7 years)) were also independently associated with adiposity at 7 years. There was a strong correlation between PBF at 3.5 years and PBF at 7 years. CONCLUSIONS: Many primary school aged children start on the trajectory of obesity in the preschool years, which suggests interventions need to start early. Maternal overweight/obesity, television watching, sedentary activity time and rapid weight gain in infancy, early and middle childhood are risk factors for childhood obesity, and are all potentially modifiable. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <77> Unique Identifier 17704040 Status MEDLINE Authors Ho CS. Tsai AC. Authors Full Name Ho, Ching-Sung. Tsai, Alan C. Institution Department of Healthcare Administration, Asia University, 500 Liufeng Rd., Wufeng, Taichung, Taiwan. [email protected] Title Prevalence of overweight and obesity and its associated factors in aboriginal Taiwanese: findings from the 2001 National Health Interview Survey in Taiwan. Source Asia Pacific Journal of Clinical Nutrition. 16(3):572-9, 2007. Abstract The study was undertaken to assess the prevalence of obesity in Taiwanese aborigines and to identify the associated factors. Data for this study were from the "2001 National Health Interview Survey (NHIS)" that conducted in-home, face-to-face, interviews on 6,592 households (26,658 persons) of a national probability sample in Taiwan. Aborigine-dense mountainous areas are over- sampled. BMI values were used to indicate obesity status. Logistic regression analyses were used to determine the significance of the association of the variables with the obesity status. Results showed that approximately 10.5% of aboriginal men and 14.5% of women compared to 4.1% and 3.5% of their non-aboriginal counterparts were obese (BMI > 30). An additional 45.1% of aboriginal men and 33.3% of women compared to 27.6% and 17.7% of their non-aboriginal counterparts were overweight (BMI 25-30). Regression analyses revealed few associations with increased risk of obesity in the aborigines. However, t! he aborigines and non-aborigines were distinctly different from each other in socio-economic status, lifestyle, environmental factors and attitude toward obesity. Results indicate that obesity is more prevalent among the aborigines but the causal reasons are not apparent. The public health authorities should develop more culturally appropriate community-based intervention strategies to promote the health of the aborigines. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <78> Unique Identifier 17668643 Status MEDLINE Authors Bhowmick SK. Dasari G. Levens KL. Rettig KR. Authors Full Name Bhowmick, Samar K. Dasari, Gayathri. Levens, Kara L. Rettig, Kenneth R. Institution Division of Endocrine and Metabolic Disease, University of South Alabama College of Medicine, 2451 Fillingim St., Suite 212, Mobile, AL 36617-2293, USA. [email protected] Title The prevalence of elevated serum thyroid-stimulating hormone in childhood/adolescent obesity and of autoimmune thyroid diseases in a subgroup. Source Journal of the National Medical Association. 99(7):773-6, 2007 Jul. Abstract OBJECTIVES: 1) To ascertain the frequency of elevated thyroid-stimulating hormone (TSH) level in obese children and adolescents and 2) to determine the prevalence of positive thyroid antibodies in the subgroup of obese children with elevated serum TSH concentration. METHODS: Retrospective chart review and prospective observation of 308 children, ages 6-17 years, with nonorganic, nonsyndromic obesity with BMI > 97th percentile. The control population consisted of 286 nonobese, otherwise-healthy children of the same age range. Thyroid function tests (free T4 or T4 with TSH) were obtained on all patients in both groups. Thyroid antibodies (thyroid peroxidase and thyroglobulin) were determined among those with elevated TSH levels. RESULTS: Elevated TSH levels of > 4 uIU/ml (reference interval 0.4-4) were noted in 36 patients within the obese group (11.7%) but only two in the control group (< 0.7%). Five out of the 36 in the obese subgroup with elevated TSH levels had positive ! thyroid antibodies (14%). All five subjects in the obese subgroup with positive thyroid antibodies had TSH levels >7.4 uIU/ml, with an average of 9.8 uIU/ml. Thirty-one children in the obese subgroup with negative thyroid antibodies had TSH levels < 6.7 uIU/ml (average 5.33 uIU/ml). CONCLUSION: A higher prevalence of TSH elevation was observed in the obese group (11.7%) than in the control group (0.7%). Positive thyroid peroxidase and thyroglobulin antibodies were observed in higher frequency in the obese subgroup with an elevated TSH level. The obese subgroup with positive thyroid antibodies also had higher TSH levels. Therefore, some instances of high TSH, especially those associated with antibodies, are likely due, at least in part, to thyroid disease, and others (possibly a majority) may be due to obesity, not its cause. It remains to be seen whether any children with mild TSH elevation benefit from thyroid hormone treatment. Publication Type Journal Article.
Result <79> Unique Identifier 17650825 Status MEDLINE Authors Vargas PA. Perry TT. Robles E. Jo CH. Simpson PM. Magee JM. Feild CR. Hakkak R. Carroll PA. Jones SM. Authors Full Name Vargas, Perla A. Perry, Tamara T. Robles, Elias. Jo, Chan-Hee. Simpson, Pippa M. Magee, James M. Feild, Charles R. Hakkak, Reza. Carroll, Polly A. Jones, Stacie M. Institution Department of Pediatrics, University of Arkansas for Medical Sciences and Arkansas Children's Hospital, Little Rock 72202-3591, USA. [email protected] Title Relationship of body mass index with asthma indicators in head start children. Source Annals of Allergy, Asthma, & Immunology. 99(1):22-8, 2007 Jul. Abstract OBJECTIVE: To examine the relationship of body mass index (BMI) and asthma indicators on children with asthma in a Head Start (HS) program. METHODS: In this cross-sectional study (November 18, 2000, to December 12, 2003) of children aged 3 to 5 years with asthma, we compared the BMI data of HS asthmatic patients (n = 213) with the data of peer control subjects from a sample (n = 816) of the National Health and Nutrition Examination Survey aged 3 to 5 years and with children in prekindergarten in Arkansas public schools (n = 1,024). Parental reports of asthma symptoms, health care use, medication use, school days missed, and quality of life were used as indicators of asthma morbidity. Categorical analysis and chi2 tests were performed to examine the relationship between BMI and asthma morbidity. RESULTS: The prevalence of overweight (> or =95th percentile) was significantly higher in HS children with asthma compared with the National Health and Nutrition Examination Survey ! children (P < .001) and Arkansas prekindergarten children (P = .05). Compared with HS asthmatic children with a BMI less than the 85th percentile, HS asthmatic patients with a BMI of the 85th percentile or greater reported significantly more school days missed (P = .02), lifetime hospitalizations (P = .04), emergency department visits (P = .02), and activity limitations (P = .03) and fewer oral corticosteroid bursts (P = .04). There was also a trend for more daytime symptoms (P = .05) and lower quality of life (P = .06). No differences were observed in rescue (P = .28) or controller (P = .47) medications, environmental tobacco smoke exposure (P = .47), positive allergy test results (P = .85), and nighttime symptoms (P > .99). CONCLUSIONS: Having an increased BMI was associated with more asthma morbidity in this group of HS asthmatic patients. Despite the lack of a clear explanation for the link between asthma and BMI, our data suggest that an increased BMI significantly aff! ects the well-being of young asthmatic patients and should be further addressed. Publication Type Journal Article. Research Support, Non-U.S. Gov't. Research Support, U.S. Gov't, P.H.S..
Result <80> Unique Identifier 17006770 Status MEDLINE Authors Huang JS. Lee TA. Lu MC. Authors Full Name Huang, Jennifer S. Lee, Tiffany A. Lu, Michael C. Institution Department of Obstetrics and Gynecology, David Geffen School of Medicine at UCLA, Los Angeles, CA, USA. Title Prenatal programming of childhood overweight and obesity. Source Maternal & Child Health Journal. 11(5):461-73, 2007 Sep. Abstract OBJECTIVE: To review the scientific evidence for prenatal programming of childhood overweight and obesity, and discuss its implications for MCH research, practice, and policy. METHODS: A systematic review of observational studies examining the relationship between prenatal exposures and childhood overweight and obesity was conducted using MOOSE guidelines. The review included literature posted on PubMed and MDConsult and published between January 1975 and December 2005. Prenatal exposures to maternal diabetes, malnutrition, and cigarette smoking were examined, and primary study outcome was childhood overweight or obesity as measured by body mass index (BMI) for children ages 5 to 21. RESULTS: Four of six included studies of prenatal exposure to maternal diabetes found higher prevalence of childhood overweight or obesity among offspring of diabetic mothers, with the highest quality study reporting an odds ratio of adolescent overweight of 1.4 (95% CI 1.0-1.9). The Dutch fam! ine study found that exposure to maternal malnutrition in early, but not late, gestation was associated with increased odds of childhood obesity (OR 1.9, 95% CI 1.5-2.4). All eight included studies of prenatal exposure to maternal smoking showed significantly increased odds of childhood overweight and obesity, with most odds ratios clustering around 1.5 to 2.0. The biological mechanisms mediating these relationships are unknown but may be partially related to programming of insulin, leptin, and glucocorticoid resistance in utero. CONCLUSION: Our review supports prenatal programming of childhood overweight and obesity. MCH research, practice, and policy need to consider the prenatal period a window of opportunity for obesity prevention. Publication Type Journal Article. Research Support, N.I.H., Extramural. Research Support, Non-U.S. Gov't.
Result <81> Unique Identifier 17623411 Status MEDLINE Authors Downey DB. Boughton HR. Authors Full Name Downey, Douglas B. Boughton, Heather R. Institution Department of Sociology, Ohio State University, Ohio, USA. Title Childhood body mass index gain during the summer versus during the school year. Source New Directions for Youth Development. (114):33-43, 2007. Abstract The nationwide increase in obesity affects all population sectors, but the impact on children is of special concern because overweight children are prone to becoming overweight adults. Contrary to the opinion of experts, research suggests that schools may be more part of the solution than the problem. Recent seasonal comparison research (comparing children's outcomes during the summer and during school year) reports that children gain body mass index (BMI) nearly twice as fast during the summer as during the school year. Whereas most children experience healthier BMI gain during the school year than the summer, this is especially the case for black and Hispanic children and for children already overweight. Publication Type Journal Article.
Result <82> Unique Identifier 17613637 Status MEDLINE Authors Tsai HJ. Tsai AC. Nriagu J. Ghosh D. Gong M. Sandretto A. Authors Full Name Tsai, Hsin-Jen. Tsai, Alan C. Nriagu, Jerome. Ghosh, Debashis. Gong, Molly. Sandretto, Anita. Institution Department of Environmental Health Sciences, School of Public Health, University of Michigan, Ann Arbor, Michigan, USA. [email protected] Title Associations of BMI, TV-watching time, and physical activity on respiratory symptoms and asthma in 5th grade schoolchildren in Taipei, Taiwan. Source Journal of Asthma. 44(5):397-401, 2007 Jun. Abstract The study evaluated the associations of body fatness, TV-watching time, and physical activity with the occurrences of asthma and respiratory symptoms in schoolchildren in Taipei, Taiwan. A questionnaire survey was conducted to elicit episodes of respiratory symptoms and data on lifestyle and anthropometric factors in 2290 5th-grade schoolchildren. Results show that overweight was positively associated with 5 of the 7 respiratory symptoms. The risk of having respiratory symptoms increased 47%-94% in overweight schoolchildren. Watching TV > or = 3 hrs/day was associated with more occurrences of respiratory symptoms (aOR = 1.42-1.90). Physical activity > or =3 times/week was associated with fewer occurrences of respiratory symptoms (aOR = 0.66- 0.73). Overweight was positively associated with an increased risk of suspected asthma in boys (aOR = 1.56, 95% CI = 1.07-2.29), but not in girls. In summary, overweight and greater TV-watching time increase the risk of respiratory symp! toms, while habitual physical activity decreases the risk of respiratory symptoms. Weight status, sedentary life, and frequency of physical exercise are the factors that can impact on the respiratory health of schoolchildren. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <83> Unique Identifier 17310222 Status MEDLINE Authors Stratton G. Canoy D. Boddy LM. Taylor SR. Hackett AF. Buchan IE. Authors Full Name Stratton, G. Canoy, D. Boddy, L M. Taylor, S R. Hackett, A F. Buchan, I E. Institution Research into Activity and Children's Health Group, Research Institute for Sports and Exercise Sciences, Liverpool John Moores University, Liverpool, UK. [email protected] Title Cardiorespiratory fitness and body mass index of 9-11-year-old English children: a serial cross-sectional study from 1998 to 2004. Source International Journal of Obesity. 31(7):1172-8, 2007 Jul. Abstract OBJECTIVE: To examine the changes over time in cardiorespiratory fitness and body mass index (BMI) of children. DESIGN: Serial cross-sectional, population-based study. SETTING: Primary schools in Liverpool, UK. PARTICIPANTS: A total of 15,621 children (50% boys), representing 74% of eligible 9-11-year olds in the annual school cohorts between 1998/9 and 2003/4, who took part in a 20m multi-stage shuttle run test (20mMST). MAIN OUTCOME MEASURES: Weight, height, BMI (kg/m(2)) and obesity using the International Obesity Taskforce definition. RESULTS: Median (95% confidence interval) 20mMST score (number of runs) fell in boys from 48.9 (47.9-49.9) in 1998/9 to 38.1 (36.8-39.4) in 2003/4, and in girls from 35.8 (35.0-36.6) to 28.1 (27.2-29.1) over the same period. Fitness scores fell across all strata of BMI (P<0.001). Moreover, BMI increased over the same 6-year period even among children in fittest third of 20mMST. CONCLUSION: In a series of uniform cross-sectional assessment! s of school-aged children, BMI increased whereas cardiorespiratory fitness levels decreased within a 6-year period. Even among lean children, fitness scores decreased. Public health measures to reduce obesity, such as increasing physical activity, may help raise fitness levels among all children - not just the overweight or obese. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <84> Unique Identifier 17589633 Status MEDLINE Authors Rosa ML. Mesquita ET. da Rocha ER. Fonseca Vde M. Authors Full Name Rosa, Maria Luiza Garcia. Mesquita, Evandro Tinoco. da Rocha, Emanuel Ribeiro Romeiro. Fonseca, Vania de Matos. Institution Universidade Federal Fluminense, Instituto de Saude da Comunidade and Department of Internal Medicine, Niteroi, RJ, Brazil. Title Body mass index and waist circumference as markers of arterial hypertension in adolescents. Source Arquivos Brasileiros de Cardiologia. 88(5):573-8, 2007 May. Abstract OBJECTIVE: To evaluate the sensitivity and specificity of anthropometric measurements of body fat in a sample of Brazilian adolescents for the prediction of hypertension. METHODS: The arterial blood pressure was measured on two visits in a sample of 456 students aged 12 to 17 years, from public and private schools of the Fonseca neighborhood, in Niteroi, between 2003 and 2004. A subject was defined as hypertensive if he/she had systolic and diastolic pressures above the 95th percentile for sex, age and height. A questionnaire was applied and Body Mass Index (BMI) and waist circumference (WC) measurements were made. RESULTS: A statistically significant correlation was observed between hypertension and the cutoff points considered unfavorable, both for BMI and WC. The greatest association was with the cutoff point proposed for the Brazilian population. As to the BMI sensitivity used for American Black or White populations or for the Brazilian population, we found 52.4% to 57! .1% and 52.4%, respectively. And BMI specificity was 69.3%, 70.0% and 80.88%, respectively. The sensitivity found in our sample, relative to the cutoff points for WC proposed for all American ethnic groups, was also low (45.0%) and specificity was a little higher (77.6% and 74.5%, respectively). CONCLUSION: Existing American WC measurements showed low sensitivity and specificity for hypertension in our population. As to BMI, the available cutoff points also showed a low level of sensitivity. There is a need to establish body fat cutoff points that can provide a better prediction of cardiovascular risk. Publication Type Journal Article.
Result <85> Unique Identifier 17581198 Status MEDLINE Authors Todd DC. Armstrong S. D'Silva L. Allen CJ. Hargreave FE. Parameswaran K. Authors Full Name Todd, D C. Armstrong, S. D'Silva, L. Allen, C J. Hargreave, F E. Parameswaran, K. Institution Department of Medicine, Firestone Institute for Respiratory Health, St. Joseph's Healthcare, McMaster University, Hamilton, ON, Canada. Title Effect of obesity on airway inflammation: a cross-sectional analysis of body mass index and sputum cell counts. Source Clinical & Experimental Allergy. 37(7):1049-54, 2007 Jul. Abstract BACKGROUND: Several observational studies have demonstrated an association between obesity and asthma. Studies evaluating exhaled nitric oxide levels and obesity have revealed that a higher body mass index (BMI) is associated with elevated exhaled nitric oxide levels. Airway inflammation using sputum cell counts has not been assessed in obese patients with airway diseases. OBJECTIVE: The primary aim of this study was to determine whether obesity (based on BMI) is associated with eosinophilic or neutrophilic bronchitis. METHODS: The results from a database of induced sputum cell counts were compared with BMI and analysed using correlation statistics, regression and parametric and non-parametric analysis. RESULTS: Seven-hundred and twenty- seven adult participants with an equal number of sputum samples were included in the analysis. BMI varied from 14.5 to 55 kg/m(2). Sputum total cell count (mean+/-SD: 12.9 x 10(6) cell/g+/-21.5), eosinophil percent (median; min to max: 0.3%! ; 0-89.0), and neutrophil percent (mean+/-SD: 63.5+/-26.6%) were within normal limits. Participants with asthma had a higher percentage of sputum eosinophils than those without asthma (P=0.01). However, there was no difference in the total or differential cell counts among the obese and non-obese participants, when the data were analysed according to BMI category, gender, dose of inhaled corticosteroid, and presence or absence of asthma. CONCLUSION: In this large sample of adult asthmatic and non- asthmatic participants, there was no association between BMI and airway inflammation measured by sputum cell counts. Other mechanisms to explain the relationship between obesity and asthma will need to be explored if this association is to be better understood. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <86> Unique Identifier 17161525 Status MEDLINE Authors El-Assmy AM. Shokeir AA. El-Nahas AR. Shoma AM. Eraky I. El-Kenawy MR. El-Kappany HA. Authors Full Name El-Assmy, Ahmed M. Shokeir, Ahmed A. El-Nahas, Ahmed R. Shoma, Ahmed M. Eraky, Ibrahim. El-Kenawy, Mahmoud R. El- Kappany, Hamdy A. Institution Urology & Nephrology Center, Mansoura University, Mansoura, Egypt. Title Outcome of percutaneous nephrolithotomy: effect of body mass index.[see comment]. Comments Comment in: Eur Urol. 2007 Jul;52(1):204-5; PMID: 17616085 Source European Urology. 52(1):199-204, 2007 Jul. Abstract OBJECTIVE: The surgical management of renal and upper ureteral calculi presents unique challenges in obese patients. We reviewed our recent experience with percutaneous nephrolithotomy (PNL) in obese patients to determine the safety and outcome of this procedure in such group of patients. PATIENTS AND METHODS: The surgical records of 1121 patients treated with PNL between 2000 and 2004 were reviewed. Patients were stratified into four groups according to the World Health Organization classification of body mass index (BMI): <25 (average), 25-29.9 (overweight), 30-39.9 (obese), and >40 kg/m(2) (morbidly obese). The outcomes of PNL in these four groups were compared. RESULTS: A total of 1287 procedures were performed on 1155 renal units (1.1 procedures per renal unit). The overall stone-free rate was 85.1% and the mean hospital stay was 3.3+/-2.6 d. Major complications were seen in 72 patients (6.4%). No statistically significant differences were found in decrease in haemogl! obin concentration, hospital stay, and complication rate among the four study groups. The need for auxiliary procedures and stone- free rates were comparable. CONCLUSIONS: PNL in obese and morbidly obese patients yields a stone-free rate that is comparable to that achieved in nonobese patients. The complication rate and length of hospital stay are also similar. Publication Type Journal Article.
Result <87> Unique Identifier 17474948 Status MEDLINE Authors Nafiu OO. Reynolds PI. Bamgbade OA. Tremper KK. Welch K. Kasa-Vubu JZ. Authors Full Name Nafiu, Olubukola O. Reynolds, Paul I. Bamgbade, Olumuyiwa A. Tremper, Kevin K. Welch, Kathy. Kasa-Vubu, Josephine Z. Institution Department of Anesthesiology, University of Michigan Medical School, Ann Arbor, MI 48109, USA. [email protected] Title Childhood body mass index and perioperative complications.[see comment]. Comments Comment in: Paediatr Anaesth. 2007 Oct;17(10):1011-2; author reply 1012-3; PMID: 17767647 Source Paediatric Anaesthesia. 17(5):426-30, 2007 May. Abstract BACKGROUND: Our aim was to describe the incidence of quality assurance events between overweight/obese and normal weight children. METHODS: This is a retrospective review of the quality assurance database of the Mott Children's Hospital, University of Michigan for the period January 2000 to December 2004. Using directly measured height and weight, we computed the body mass index (BMI) in 6094 children. Overweight and obesity were defined using age and gender-specific cut off according to the National Center for Health Statistics (NCHS)/Centers for Disease Control and Prevention (CDC) (2000) growth charts. Frequency of quality assurance events were compared between normal weight, overweight, and obese children. RESULTS: There were 3359 males (55.1%) and 2735 females (44.9%). The mean age for the entire population was 11.9 +/- 5.2 while the mean BMI was 21.6 +/- 6.7 kg x m(-2). The overall prevalence of overweight and obesity was 31.6%. Obesity was more prevalent in boys tha! n girls (P = 0.016). Preoperative diagnoses of hypertension, type II diabetes, and bronchial asthma were more common in overweight and obese than normal weight children (P = 0.0001 for hypertension, P = 0.001 for diabetes and P = 0.014 for bronchial asthma). Difficult airway, upper airway obstruction in the postanesthesia care unit (PACU) and PACU stay longer than 3 h and need for two or more antiemetics were more common in overweight and obese than normal weight children (P = 0.001). There was no significant difference in the incidence of unplanned hospital admission following an outpatient surgical procedure between normal weight and overweight/obese children. DISCUSSION: Studies on perioperative aspects of childhood overweight and obesity are rare. Our report shows a high prevalence of overweight and obesity in this cohort of pediatric surgical patients. Certain perioperative morbidities are more common in overweight and obese than in normal weight children. There is a n! eed for prospective studies of the impact of childhood overweight and obesity on anesthesia and surgical outcome. Publication Type Journal Article.
Result <88> Unique Identifier 17437645 Status MEDLINE Authors Komakula S. Khatri S. Mermis J. Savill S. Haque S. Rojas M. Brown L. Teague GW. Holguin F. Authors Full Name Komakula, Sushma. Khatri, Sumita. Mermis, Joel. Savill, Samira. Haque, Shireen. Rojas, Mauricio. Brown, LouAnn. Teague, Gerald W. Holguin, Fernando. Institution Department of Medicine, Emory University, Atlanta, USA. [email protected] Title Body mass index is associated with reduced exhaled nitric oxide and higher exhaled 8-isoprostanes in asthmatics. Source Respiratory Research. 8:32, 2007. Other ID Source: NLM. PMC1855924 Abstract BACKGROUND: Recently, it has been shown that increasing body mass index (BMI) in asthma is associated with reduced exhaled NO. Our objective in this study was to determine if the BMI-related changes in exhaled NO differ across asthmatics and controls, and to determine if these changes are related to increased airway oxidative stress and systemic levels of leptin and adiponectin. METHODS: Observational study of the association of BMI, leptin, and adiponectin with exhaled nitric oxide (NO) and exhaled 8- isoprostanes in 67 non-smoking patients with moderate to severe persistent asthma during baseline conditions and 47 controls. Measurements included plasma levels of leptin, adiponectin, exhaled breath condensates for 8-isoprostanes, exhaled NO, pulmonary function tests, and questionnaires regarding asthma severity and control. RESULTS: In asthmatics, BMI and the ratio of leptin to adiponectin were respectively associated with reduced levels of exhaled NO (beta = -0.04 [95% C.! I. -0.07, -0.1], p < 0.003) and (beta = -0.0018 [95% C.I. -0.003, -0.00034], p = 0.01) after adjusting for confounders. Also, BMI was associated with increased levels of exhaled 8-isoprostanes (beta = 0.30 [95% C.I. 0.003, 0.6], p = 0.03) after adjusting for confounders. In contrast, we did not observe these associations in the control group of healthy non-asthmatics with a similar weight distribution. CONCLUSION: In adults with stable moderate to severe persistent asthma, but not in controls, BMI and the plasma ratio of leptin/adiponectin is associated with reduced exhaled NO. Also, BMI is associated with increased exhaled 8-isoprostanes. These results suggest that BMI in asthmatics may increase airway oxidative stress and could explain the BMI-related reductions in exhaled NO. Publication Type Journal Article.
Result <89> Unique Identifier 17171692 Status MEDLINE Authors Ross JA. Authors Full Name Ross, Julie A. Institution Department of Pediatrics, Division of Epidemiology and Clinical Research, University of Minnesota, Minneapolis, Minnesota 55455, USA. [email protected] Title Genetic susceptibility and body mass in childhood cancer survivors. [Review] [52 refs] Source Pediatric Blood & Cancer. 48(7):731-5, 2007 Jun 15. Abstract Childhood cancer survivors are at increased risk of many long-term treatment-related sequel such as second cancers, cardiovascular disease, and pulmonary complications. Certain treatments seem to influence the risk of becoming overweight, obese, or underweight, and abnormal body mass index (BMI) is associated with increased morbidity and mortality. Because BMI is modifiable, it is important to identify treatment and patient-related factors contributing to altered BMI. New research areas include exploring how genetic susceptibility through population polymorphism may contribute to BMI. Illuminating potential gene- environment interactions that influence obesity and underweight might be more readily accomplished in a study of high-risk individuals (i.e., childhood cancer survivors) with well-characterized exposures. The new Childhood Cancer Research Network in the Children's Oncology Group, when fully implemented, should make it less difficult in the future to recruit the lar! ge numbers of patients needed for such studies. (c) 2006 Wiley-Liss, Inc. [References: 52] Publication Type Journal Article. Research Support, N.I.H., Extramural. Research Support, Non-U.S. Gov't. Review.
Result <90> Unique Identifier 17384659 Status MEDLINE Authors Mamun AA. Lawlor DA. Alati R. O'Callaghan MJ. Williams GM. Najman JM. Authors Full Name Mamun, A A. Lawlor, D A. Alati, R. O'Callaghan, M J. Williams, G M. Najman, J M. Institution Longitudinal Studies Unit, School of Population Health, University of Queensland, Brisbane, Australia. [email protected] Title Increasing body mass index from age 5 to 14 years predicts asthma among adolescents: evidence from a birth cohort study. Source International Journal of Obesity. 31(4):578-83, 2007 Apr. Abstract BACKGROUND: Obesity and asthma are common disorders, and the prevalence of both has increased in recent decades. It has been suggested that increases in the prevalence of obesity might in part explain the increase in asthma prevalence. This study aims to examine the prospective association between change in body mass index (BMI) z-score between ages 5 and 14 years and asthma symptoms at 14 years. METHODS: Data was taken from the Mater University Study of Pregnancy and its outcomes (MUSP), a birth cohort of 7223 mothers and children started in Brisbane (Australia) in 1981. BMI was measured at age 5 and 14 years. Asthma was assessed from maternal reports of symptoms at age 5 and 14 years. In this study analyses were conducted on 2911 participants who had information on BMI and asthma at both ages. RESULTS: BMI z-score at age 14 and the change in BMI z-score from age 5 to 14-years were positively associated with asthma symptoms at age 14 years, whereas BMI z-score at age 5 wa! s not associated with asthma at age 14. Adjustment for a range of early-life exposures did not substantially alter these findings. The association between change in BMI z-score with asthma symptoms at 14 years appeared stronger for male subjects compared with female subjects but there was no statistical evidence for a sex difference (P=0.36). CONCLUSIONS: Increase in BMI z-score between age 5 and 14 years is associated with increased risk of asthma symptoms in adolescence. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <91> Unique Identifier 17043845 Status MEDLINE Authors Bidad K. Anari S. Aghamohammadi A. Pourpak Z. Moayeri H. Authors Full Name Bidad, Katayoon. Anari, Shahab. Aghamohammadi, Asghar. Pourpak, Zahra. Moayeri, Heshmat. Institution Immunology, Asthma and Allergy Research Institute, Tehran University of Medical Sciences, No 62, Dr Gharib st, Keshavarz Blvd., Tehran, 14194, Iran. [email protected] Title Prevalence of asthma related to BMI in adolescents in Tehran, Iran, 2004-2005. Source European Journal of Pediatrics. 166(5):453-4, 2007 May. Abstract Both asthma and obesity have become more common in affluent societies during the recent decades, and several studies have shown a correlation between the presence of asthma and obesity. Publication Type Journal Article.
Result <92> Unique Identifier 17105842 Status MEDLINE Authors Bell LM. Byrne S. Thompson A. Ratnam N. Blair E. Bulsara M. Jones TW. Davis EA. Authors Full Name Bell, Lana M. Byrne, Sue. Thompson, Alisha. Ratnam, Nirubasini. Blair, Eve. Bulsara, Max. Jones, Timothy W. Davis, Elizabeth A. Institution Telethon Institute for Child Health Research, Center for Child Health Research, University of Western Australia, Australia. Title Increasing body mass index z-score is continuously associated with complications of overweight in children, even in the healthy weight range. Source Journal of Clinical Endocrinology & Metabolism. 92(2):517-22, 2007 Feb. Abstract CONTEXT: Overweight/obesity in children is increasing. Incidence data for medical complications use arbitrary cutoff values for categories of overweight and obesity. Continuous relationships are seldom reported. OBJECTIVES: The objective of this study is to report relationships of child body mass index (BMI) z-score as a continuous variable with the medical complications of overweight. DESIGN: This study is a part of the larger, prospective cohort Growth and Development Study. SETTING: Children were recruited from the community through randomly selected primary schools. Overweight children seeking treatment were recruited through tertiary centers. PARTICIPANTS: Children aged 6-13 yr were community-recruited normal weight (n = 73), community-recruited overweight (n = 53), and overweight treatment-seeking (n = 51). Medical history, family history, and symptoms of complications of overweight were collected by interview, and physical examination was performed. Investigations i! ncluded oral glucose tolerance tests, fasting lipids, and liver function tests. MAIN OUTCOME MEASURE: Adjusted regression was used to model each complication of obesity with age- and sex-specific child BMI z-scores entered as a continuous dependent variable. RESULTS: Adjusted logistic regression showed the proportion of children with musculoskeletal pain, obstructive sleep apnea symptoms, headaches, depression, anxiety, bullying, and acanthosis nigricans increased with child BMI z-score. Adjusted linear regression showed BMI z-score was significantly related to systolic and diastolic blood pressure, insulin during oral glucose tolerance test, total cholesterol, high-density lipoprotein, triglycerides, and alanine aminotransferase. CONCLUSION: Child's BMI z- score is independently related to complications of overweight and obesity in a linear or curvilinear fashion. Children's risks of most complications increase across the entire range of BMI values and are not defined by th! resholds. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <93> Unique Identifier 17194858 Status MEDLINE Authors Milne E. Simpson JA. Johnston R. Giles-Corti B. English DR. Authors Full Name Milne, Elizabeth. Simpson, Julie A. Johnston, Robyn. Giles-Corti, Billie. English, Dallas R. Institution Telethon Institute for Child Health Research, Centre for Child Health Research, University of Western Australia, West Perth. [email protected] Title Time spent outdoors at midday and children's body mass index. Source American Journal of Public Health. 97(2):306-10, 2007 Feb. Other ID Source: NLM. PMC1781390 [Available on 02/01/09] Abstract OBJECTIVES: We investigated whether the Kidskin sun protection intervention increased children's body mass index by reducing the time spent outdoors at midday. METHODS: The Kidskin sun protection intervention involved 1614 Australian school children assigned to 1 of 3 groups: a control group, a moderate-intervention group, or a high-intervention group. Schools in the control group received the standard health curriculum and schools in the intervention groups received a multicomponent intervention. Outcomes included time spent outdoors and nevus development (a marker of melanoma risk). Height and weight were measured at 3 time points. Body mass index was transformed into age- and gender-specific z scores; z scores at each age were modeled simultaneously. Time spent outdoors at ages 10 and 12 years was analyzed using a linear mixed effects modeling. RESULTS: The proportion of children who were overweight or obese increased with age. The moderate-intervention and control grou! ps had a minimal increase in z score over time, and the z score for the high-intervention group decreased over time. There were no differences among groups with respect to total time outdoors at any age. CONCLUSIONS: It is possible to reduce the time children spend outdoors when ultraviolet radiation is high without producing an unfavorable effect on the children's body mass index. Publication Type Controlled Clinical Trial. Journal Article. Research Support, Non-U.S. Gov't.
Result <94> Unique Identifier 17228049 Status MEDLINE Authors Cheung N. Saw SM. Islam FM. Rogers SL. Shankar A. de Haseth K. Mitchell P. Wong TY. Authors Full Name Cheung, Ning. Saw, Seang Mei. Islam, F M Amirul. Rogers, Sophie L. Shankar, Anoop. de Haseth, Kristin. Mitchell, Paul. Wong, Tien Yin. Institution Centre for Eye Research Australia, University of Melbourne, 32 Gisborne Street, Victoria 3002, Australia. Title BMI and retinal vascular caliber in children. Source Obesity. 15(1):209-15, 2007 Jan. Abstract OBJECTIVE: In adult populations, changes in retinal vascular caliber have been linked with obesity and metabolic syndrome. We examined the association of BMI and weight with retinal vascular caliber in children. RESEARCH METHODS AND PROCEDURES: This was a school-based, cross-sectional study of 768 children, 7 to 9 years old, randomly sampled from the Singapore Cohort Study of the Risk Factors for Myopia. Participants had digital retinal photographs. Retinal vascular caliber was measured using a computer- based program and combined to provide average calibers of arterioles and venules in that eye. Weight and height were measured using standardized protocol. These data were used to calculate BMI. RESULTS: In this population, the mean retinal arteriolar and venular calibers were 156.40 microm [95% confidence interval (CI), 155.44 to 157.36] and 225.43 microm (95% CI, 224.10 to 226.74) respectively. After controlling for age, gender, race, parental monthly income, axial length,! birth weight, and birth length, each 3.1 kg/m2 (standard deviation) increase in BMI was associated with a 2.55-microm (95% CI, 1.21 to 3.89; p < 0.001) larger retinal venular caliber. In multivariable analysis, greater weight was also significantly associated with larger retinal venular caliber. BMI and weight were not associated with retinal arteriolar caliber. Height was not significantly associated with retinal arteriolar or venular caliber. DISCUSSION: Greater BMI and weight are associated with larger retinal venular caliber in healthy children. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <95> Unique Identifier 17160975 Status MEDLINE Authors Benefice E. Lopez R. Monroy SL. Rodriguez S. Authors Full Name Benefice, Eric. Lopez, Ronald. Monroy, Selma Luna. Rodriguez, Sonia. Institution Research Unit R024, Epidemiology and Prevention, Institut de Recherche pour le Developpement, Representacion IRD en Bolivia, La Paz, Bolivia. [email protected] Title Fatness and overweight in women and children from riverine Amerindian communities of the Beni River (Bolivian Amazon). Source American Journal of Human Biology. 19(1):61-73, 2007 Jan-Feb. Abstract Obesity is a worldwide public health problem impacting not only industrialized nations but also developing countries. The main objective of this paper was to analyze risk factors for overweight among Amerindian children and their mothers. Data were collected in 15 Amerindian riverside communities from the Beni River (Bolivia). The total sample was of 195 mothers and 452 children, 0-15 years of age. Information about family activity and dietary patterns was collected, and a clinical examination was performed. Stool samples were collected in children for parasitological screening. Anthropometric measurements, including weight, height, arm circumference, and four skinfolds, were taken. A bioelectrical impedance analysis was performed in mothers. In total, 12.2% (95% confidence interval (CI(95%)) 9.1-15.9%) of the children were considered overweight; less than 1% were overtly obese International Obesity Task Force (IOTF) criteria. Among their mothers, 35.3% (CI(95%), 28.7-42.5! %) were overweight (BMI (weight/height (2)) >25 kg/m(2)), and 5% (CI(95%), 2.5-5.1%) were obese (BMI >30 kg/m(2)). BMI was moderately related to anthropometric indices of body composition in children, but was highly correlated with fatness in mothers. The risk of overweight was not associated with environmental factors in children. In mothers, there was a significant relationship between BMI, health status, and dietary diversity score. There was a moderate association in boys between fatness and the BMI of their mothers (R(2) = 0.12, P < 0.001), but not in girls. These findings suggest a trend toward accumulation of fat related to possible changes at the economic and agricultural levels, even in remote rural areas. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <96> Unique Identifier 17679804 Status MEDLINE Authors Murdock DK. Olson KJ. Juza RM. Hendricks BL. Authors Full Name Murdock, David K. Olson, Karen J. Juza, Ryan M. Hendricks, Bryan L. Institution Cardiovascular Associates of Northern Wisconsin, SC, Wausau, WI, USA. Title Effect of body mass index on insulin resistance and lipids in prepubertal and postpubertal children: SCHOOL observations. Source Journal of the CardioMetabolic Syndrome. 1(4):242-7, 2006. Abstract As part of the School Children Have Early Onset of Leading Risk Factors for Cardiovascular Disease and Diabetes Mellitus (SCHOOL) project, this study examines the effect of elevated body mass index on metabolic parameters and its relationship to insulin resistance in prepubertal and postpubertal students from the Wausau School District in central Wisconsin. Two hundred forty-seven nondiabetic students were randomly selected (125 prepubertal [2nd graders] and 122 postpubertal [11th graders]). Waist/hip ratio and body mass index corrected for age and sex were calculated. Fasting insulin, glucose, and nuclear magnetic resonance lipid profiles were measured. Relative insulin resistance was defined as quantitative insulin sensitivity check index > 1 SD below the mean of normal-weight children. Twenty-eight percent of 2nd graders and 33% of 11th graders were overweight. Relative insulin resistance was present in 47% of overweight 2nd graders and 51 % of overweight 11th graders a! nd was associated with higher triglycerides, lower high-density lipoprotein, smaller low-density lipoprotein particles and, in 11th graders, higher waist/hip ratio. Relative insulin resistance prevalence is high among overweight children and adolescents. Biomarkers of increased risk of adverse cardiovascular outcomes are already present in overweight school children. Publication Type Comparative Study. Journal Article. Research Support, Non-U.S. Gov't. Research Support, U.S. Gov't, P.H.S..
Result <97> Unique Identifier 17249484 Status MEDLINE Authors da Silva AC. Rosa AA. Authors Full Name da Silva, Ana Carolina Pio. Rosa, Alberto A. Institution Medical School of the Federal University of Rio Grande do Sul, Brazil. Title Blood pressure and obesity of children and adolescents association with body mass index and waist circumference. Source Archivos Latinoamericanos de Nutricion. 56(3):244-50, 2006 Sep. Abstract The objective of this work was to evaluate the association between the average levels of blood pressure of 706 children in Porto Alegre with their nutritional state--body mass index (BMI), body fat percentage, waist circumference--and with their social-economic state. A prevalence of 12.3% (n=87) of high blood pressure was found. According to the BMI, 11% of the sample was obese. 47.7% belonged to the social class with an income less than two monthly minimum salaries. All of the correlations of the SBP (systolic blood pressure) and DBP (diastolic blood pressure) with variables in the nutritional state showed to be significant (p < 0.001). What ended up having a stronger association was the BMI and waist circumference with SBP (R = 0.27). This study made it possible to notice that the anthropometric indicator that best is related to the existence of high BP is the BMI along with the waist circumference. This seems to be an easy method that is noninvasive and of low cost to ! detect the risk of high BP in children and adolescents. Publication Type Journal Article.
Result <98> Unique Identifier 17176785 Status MEDLINE Authors Kalpaklioglu AF. Kara T. Kurtipek E. Saygun M. Authors Full Name Kalpaklioglu, A Fusun. Kara, Turkan. Kurtipek, Ercan. Saygun, Meral. Institution Department of Allergy, Kirikkale University Faculty of Medicine, Kirikkale, Turkey. [email protected] Title Effect of body mass index on quality of life in allergic/asthmatic patients. Source Allergy & Asthma Proceedings. 27(6):499-503, 2006 Nov-Dec. Abstract Evaluation of quality of life (QoL) is of particular interest in patients suffering from chronic diseases. Although studies have shown an association between QoL and obesity and allergy/asthma, the effect of obesity on QoL is not well known. The aim of this study was to assess the impact of body mass index (BMI) as a contributory factor on QoL in patients with a diagnostic label of allergy/asthma. We surveyed 100 patients (69 F/31 M) (age 34.15+/-13.32 years), and 65 healthy controls (42 F/23 M) (age 35.45 +/-8.96 years). QoL was determined by SF-36. BMI > or = 25 kg/m(2) was accepted as overweight/obesity. Forty-five percent of the patients had BMI > or = 25 kg/m(2) with no difference between the genders. They were significantly older and more likely to have less education level than those with BMI < 25 kg/m(2). Quality-of-life scores among patients with allergy/asthma were lower than those in the control group, irrespective of BMI. However, increased BMI was found to be ! related with improved quality of life among controls. Pearson's analysis showed that BMI was inversely correlated with physical functioning among patients (r = -0.229, p = 0.034), but in the control group it was positively correlated with QoL. All the domains of SF-36, except role-physical ones, among female subjects were significantly impaired more than those of male patients. It has been shown that the major determinants of impaired QoL are female sex, older age, and less educational status in patients with allergic/asthmatic symptoms. The impact of BMI on QoL could be undermined, because it seems to play a minor role. Publication Type Journal Article.
Result <99> Unique Identifier 17142530 Status MEDLINE Authors Glazebrook C. McPherson AC. Macdonald IA. Swift JA. Ramsay C. Newbould R. Smyth A. Authors Full Name Glazebrook, Cristine. McPherson, Amy C. Macdonald, Ian A. Swift, Judy A. Ramsay, Christopher. Newbould, Rachel. Smyth, Alan. Institution School of Community Health Sciences, University of Nottingham, Nottingham, United Kingdom. [email protected] Title Asthma as a barrier to children's physical activity: implications for body mass index and mental health.[see comment]. Comments Comment in: Pediatrics. 2007 Jun;119(6):1247-8; author reply 1248-9; PMID: 17545400 Source Pediatrics. 118(6):2443-9, 2006 Dec. Abstract OBJECTIVES: The purpose of this work was to identify barriers to physical activity in children with asthma and to compare their customary activity levels, BMI and emotional well-being with that of children with other medical conditions. It was hypothesized that children with asthma would have higher BMI and lower levels of customary activity. PATIENTS AND METHODS: We studied children aged 7 to 14 years attending hospital outpatient clinics for either asthma (asthma group: n = 56) or for otorhinolaryngology or dermatological conditions (nonasthma group: n = 61). In this cross-sectional survey, children's weight and height were recorded and their BMI classified according to International Obesity Task Force classification of obesity. Child mental health was assessed by the parent-rated Strengths and Difficulties Questionnaire. The child-rated Physical Activity Questionnaire assessed total sedentary and physical activities during the previous 24 hours. RESULTS: The asthma grou! p had a higher mean BMI (20.78 vs 18.82) and higher rates of obesity (21.4% vs 6.6%). Children with asthma reported fewer physical activities than the nonasthma group (median 4 per day vs 6 per day) but comparable levels of sedentary activities. Asthma was the strongest predictor of lower activity scores, followed by younger age. The asthma group had higher levels of emotional difficulties and, within this group, more active children had better mental health. More parents in the asthma group identified the child's health as a barrier to exercise (60.7% vs 11%). The same was true of children (66.1% vs 11.5%). CONCLUSIONS: We found that children attending a hospital clinic for asthma were more likely to be obese and were significantly less active than a comparison group with other medical conditions. Asthma was identified as a barrier to exercise by parents and children. Strategies to promote exercise within pediatric asthma care are needed to protect both mental and physical! health. Publication Type Comparative Study. Journal Article. Research Support, Non-U.S. Gov't.
Result <100> Unique Identifier 17111885 Status MEDLINE Authors He Q. Authors Full Name He, Qing. Title BMI monitoring in the management of obesity in toddlers.[comment]. Comments Comment on: Am Fam Physician. 2006 Nov 1;74(9):1527-32; PMID: 17111891 Source American Family Physician. 74(9):1483-4, 2006 Nov 1. Publication Type Comment. Editorial.
Result <101> Unique Identifier 17094261 Status MEDLINE Authors Chen L. Velasco Mondragon HE. Lazcano-Ponce E. Collins A. Shugart YY. Authors Full Name Chen, Lina. Velasco Mondragon, H Eduardo. Lazcano-Ponce, Eduardo. Collins, Andrew. Shugart, Yin Yao. Institution Department of Social Medicine, University of Bristol, Bristol, UK. Title Effect of the peroxisome proliferators-activated receptor (PPAR) gamma 3 gene on BMI in 1,210 school students from Morelos, Mexico. Source Pacific Symposium on Biocomputing. :467-77, 2006. Abstract Little research has been undertaken on risk factors for obesity in young people in Latin America, including Mexico, despite the fact that obesity constitutes the number one public health problem in Mexico. Our objective was to investigate the effect of the Peroxisome proliferators-activated receptor (PPAR)_3 gene on BMI measured among adolescents collected from a cohort study originally designed for epidemiological studies. METHODS: Blood samples and anthropometric measurements were collected from 1,210 out of 13,294 public school students of both sexes, aged 11-24 years in Morelos, Mexico. In this study, we genotyped 7 selected SNPs of the PPAR_ transcript variant 3 (including Pro12Ala) in a group of unrelated 717 males and 493 females (age range 11-24), including 3 SNPs located in the 5' untranslated region. These 7 SNPs were selected by the tagging algorithm implemented in the program haploview to scan the whole gene. We tested each of the 7 SNPs individually for associ! ation with the body mass index (BMI), and two SNPs (rs2938392 and rs1175542) revealed significant associations with BMI (p- value=0.008 and 0.029, respectively). The SNP rs2938392 is roughly 41.5 Kb from rs1801282 (Pro12Ala in PPAR_2). Furthermore, we examined the association between haplotypes built from 7 SNPs and BMI using a score statistic implemented in the program haplo.stats. While the permutation based global p-value was 0.544, one individual haplotype with a frequency of 0.279 gave a p- value of 0.089 (permutation based). However, when the analyses were conducted in males only, the permutation based global p- value was 0.055 and one individual haplotype with a frequency of 0.28 gave a significant p-value of 0.013. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <102> Unique Identifier 16895959 Status MEDLINE Authors Pena AS. Wiltshire E. MacKenzie K. Gent R. Piotto L. Hirte C. Couper J. Authors Full Name Pena, Alexia Sophie. Wiltshire, Esko. MacKenzie, Karen. Gent, Roger. Piotto, Lino. Hirte, Craig. Couper, Jennifer. Institution Department of Endocrinology, University of Adelaide, Women's and Children's Hospital, North Adelaide, SA 5006, Australia. [email protected] Title Vascular endothelial and smooth muscle function relates to body mass index and glucose in obese and nonobese children. Source Journal of Clinical Endocrinology & Metabolism. 91(11):4467-71, 2006 Nov. Abstract CONTEXT: Endothelial and smooth muscle dysfunction are critical precursors of atherosclerosis. These can be detected in children at risk of cardiovascular disease. OBJECTIVE: The objective of this study is to evaluate endothelial and smooth muscle function and their determinants using flow-mediated dilatation (FMD) and glyceryl trinitrate-mediated dilatation (GTN) in obese, nonobese, and type 1 diabetes mellitus (T1DM) children. DESIGN: This is a cross-sectional study. SUBJECTS: The study subjects were 270 children [140 males, mean age 13.7 (2.8) yr] including 58 obese, 53 nonobese, and 159 T1DM children. MEASUREMENTS: Vascular function (FMD and GTN), body mass index (BMI) z-score, blood pressure, glucose, glycosylated hemoglobin, lipids, folate, homocysteine, and high sensitive C-reactive protein were measured. RESULTS: FMD and GTN were significantly lower in obese and T1DM compared with nonobese subjects (P < 0.001, P < 0.001). FMD and GTN were similarly reduced in obese! and T1DM subjects (P = 0.22, P = 0.28). In all nondiabetic subjects (n = 111), both FMD and GTN were significantly and independently related to BMI z-score (r = -0.28, P = 0.003, beta = -0.36, P < 0.001) and weight z-score (beta = -0.31, P = 0.002; r = -0.52, P < 0.001). FMD related independently to total cholesterol (beta = -0.22, P = 0.02). GTN related independently to vessel diameter (beta = -0.49, P < 0.001). GTN related to glucose within the normal range (r = -0.34, P = 0.001). CONCLUSIONS: Children with obesity and T1DM have a similar degree of vascular dysfunction. BMI and weight adjusted for age and sex relate to endothelial and smooth muscle function in nonobese and obese children. Glucose relates to smooth muscle function in nonobese nondiabetic children. This suggests a continuum effect of BMI and glucose within the normal range on vascular function in childhood. Publication Type Comparative Study. Journal Article. Research Support, Non-U.S. Gov't.
Result <103> Unique Identifier 17068825 Status MEDLINE Authors Hong SJ. Lee MS. Lee SY. Ahn KM. Oh JW. Kim KE. Lee JS. Lee HB. for the Korean ISAAC Study Group, Korean Academy of Pediatric Allergy and Respiratory Disease, Seoul, Korea. Authors Full Name Hong, Soo-Jong. Lee, Moo-Song. Lee, Soo-Young. Ahn, Kang-Mo. Oh, Jae-Won. Kim, Kyu-Earn. Lee, Joon-Sung. Lee, Ha-Baik. for the Korean ISAAC Study Group, Korean Academy of Pediatric Allergy and Respiratory Disease, Seoul, Korea. Institution Department of Pediatrics, Ulsan University College of Medicine, Seoul, Korea. Title High body mass index and dietary pattern are associated with childhood asthma. Source Pediatric Pulmonology. 41(12):1118-24, 2006 Dec. Abstract The increasing prevalence of asthma has coincided with an increase of body mass index (BMI) in both children and adults. We investigated the relationship between BMI and the symptom prevalence of asthma and the possible influences of dietary pattern. This was a community-based, cross-sectional study of 24,260 school children aged 6-12 years. Prevalences of asthma and potential confounding factors were assessed using a Korean version of the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire which was completed by parents. We analyzed the relationship between BMI and symptoms of asthma and the possible influences of dietary pattern. A significant positive association between high BMI and previous 12-month prevalence of wheeze remained in boys (adjusted odds ratio, 1.610; 95% confidence interval, 1.274-2.033) but not in girls. In addition, there were significant associations between high BMI and lifetime prevalence of wheeze, previous 12-month whee! ze, exercise-induced wheeze, diagnosis, and treatment of asthma. There were significant associations between high BMI and previous 12-month wheeze regardless of breast-milk feeding or whole-milk feeding. Frequent intake of fresh seafood, fresh fruits, and vegetables was associated with reduced prevalence of current asthma symptoms and was also associated with decreased BMI. These results indicate that BMI may be an independent risk factor for the development of asthma symptoms in boys. Intake of fresh seafood, fresh fruit, and vegetables, which may be associated with decreased BMI, may contribute to protect against the development of asthma symptoms in Korean elementary schoolchildren. Publication Type Journal Article.
Result <104> Unique Identifier 17026635 Status MEDLINE Authors Navuluri S. Authors Full Name Navuluri, Sriram. Title Is overweight based on BMI a good predictor of risk for hypertension among adolescents?. Source Journal of School Health. 76(9):441, 2006 Nov. Publication Type Letter.
Result <105> Unique Identifier 16964359 Status MEDLINE Authors Ziegler A. Barth N. Coners H. Mayer H. Hebebrand J. Authors Full Name Ziegler, A. Barth, N. Coners, H. Mayer, H. Hebebrand, J. Institution Institut fur Medizinische Biometrie und Statistik, Universitat zu Lubeck, 23538 Lubeck, Germany. [email protected] Title Practical considerations on the use of extreme sib-pairs for obesity. Source Methods of Information in Medicine. 45(4):419-23, 2006. Abstract OBJECTIVES: The extreme sib-pair approach has been shown to be a powerful strategy to identify susceptibility loci linked to quantitative traits. The body mass index is the usually assessed trait in genetic studies on human obesity. Environmental factors clearly play an important role for this trait. We hypothesized that the low weight of most sibs who were seemingly discordant to the obese index proband was influenced by other environmental and/or genetic factors like restrained eating or psychiatric disorders. METHODS: A screening questionnaire was sent to parents of all consecutively admitted patients three weeks prior to referral of index probands for inpatient treatment of obesity. The first 320 families were further investigated. Twenty-seven seemingly extremely discordant sib-pairs (ED) were identified and examined in detail. RESULTS: The low weight of most sibs who were seemingly discordant to the obese index proband was influenced by factors like restrained eating! or psychiatric disorders. Only 20% of the interviewed ED could be considered as genuine ED. CONCLUSION: We conclude that extensive medical evaluation is necessary if the aim is to guarantee genuine ED in family studies for human obesity. Non-paternity deserves specific attention in ED studies. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <106> Unique Identifier 16929003 Status MEDLINE Authors Kostikas K. Papaioannou AI. Gourgoulianis KI. Authors Full Name Kostikas, Konstantinos. Papaioannou, Andriana I. Gourgoulianis, Konstantinos I. Title BMI and gastroesophageal reflux in women.[comment]. Comments Comment on: N Engl J Med. 2006 Jun 1;354(22):2340-8; PMID: 16738270 Source New England Journal of Medicine. 355(8):848; author reply 849-50, 2006 Aug 24. Publication Type Comment. Letter.
Result <107> Unique Identifier 16503404 Status MEDLINE Authors Kilpelainen M. Terho EO. Helenius H. Koskenvuo M. Authors Full Name Kilpelainen, Maritta. Terho, Erkki O. Helenius, Hans. Koskenvuo, Markku. Institution Department of Pulmonary Diseases and Clinical Allergology, Turku University Hospital, Kiinamyllynkatu 4-8, FIN-20520 Turku, Finland. [email protected] Title Body mass index and physical activity in relation to asthma and atopic diseases in young adults. Source Respiratory Medicine. 100(9):1518-25, 2006 Sep. Abstract BACKGROUND: Obesity has been shown to increase the risk of asthma and wheezing. Conditioning exercise might decrease the asthma risk, and that could partly explain the association. The relation between obesity and allergic diseases is quite conflicting. METHODS: The association between body mass index (BMI) and physician-diagnosed asthma, allergic rhinitis or conjunctivitis, atopic dermatitis, and self-reported wheezing was investigated in a questionnaire study among 10,667 Finnish first-year university students aged 18-25 years. Logistic regression was used to evaluate possible confounding by parental education, passive smoking at age 0-2, childhood residential environment, current and past smoking and leisure time physical activity index. RESULTS: In men, there was a greater risk of asthma, but not wheezing with increasing BMI. Compared to those with BMI below 20, OR for male asthma was 1.98 (95% CI 1.11-3.52) in BMI category 20.0-22.4, 1.90 (95% CI 1.05-3.41) in BMI 22.! 5-24.9, and 3.5 (95% CI 1.63-7.64) in BMI > or = 27.5. Among women, the risks of asthma and wheezing were about two-fold among the overweight-obese subjects. Moderate leisure time physical activity was associated with lower risk of asthma in men (OR 0.62, 95% CI 0.62 (0.42-0.92), but not among women. The risk of allergic rhinoconjunctivitis and atopic dermatitis increased quite linearly with BMI among women but not men. CONCLUSIONS: Low leisure time physical activity seems not to explain the greater risk of asthma among obese men and women. The quite linear association between BMI and both allergic rhinoconjunctivitis and wheezing among women suggests the independent effect of body fat on atopic diseases. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <108> Unique Identifier 16776880 Status MEDLINE Authors Cho J. Juon HS. Authors Full Name Cho, Juhee. Juon, Hee-Soon. Institution Johns Hopkins Bloomberg School of Public Health, Department of Health, Behavior, and Society, 624 N Broadway, Room 727, Baltimore, MD 21205-1996, USA. [email protected] Title Assessing overweight and obesity risk among Korean Americans in California using World Health Organization body mass index criteria for Asians. Source Preventing Chronic Disease. 3(3):A79, 2006 Jul. Other ID Source: NLM. PMC1636717 Abstract INTRODUCTION: Although it is known that at comparable body mass index (BMI) levels Asian Americans have a higher prevalence of high blood pressure, heart disease, and type 2 diabetes than whites, little is known about the social, behavioral, and cultural factors associated with obesity risk in this population. METHODS: A cross-sectional analysis of the 2003 California Health Interview Survey was performed to estimate overweight and obesity prevalence among Korean Americans using BMI criteria suggested by the World Health Organization for Asian populations worldwide. In addition, associations between demographics, social, behavioral, and cultural factors and the risk of being overweight and obese were examined. RESULTS: Of 492 Korean American respondents, 38% were overweight and 8% were obese according to World Health Organization body mass index criteria for Asians. In a multivariate analysis, sex, marital status, poverty, and length of residence in the United States were ! associated with BMI. Men were more likely to be overweight or obese than women, and length of residence in the United States was strongly associated with higher body mass index. CONCLUSION: Like other ethnic groups, Korean Americans have a sociodemographic profile that is identified with an increased risk of becoming obese. Considering these factors in developing early diet and physical activity interventions could be an important opportunity to prevent weight gain and diminish disease caused by obesity. This study also suggests how meaningful BMI criteria tailored for Asian Americans could be used to more accurately measure risk of obesity within a heterogeneous population such as the U.S. population. Publication Type Journal Article.
Result <109> Unique Identifier 16773410 Status MEDLINE Authors Foster BJ. Shults J. Zemel BS. Leonard MB. Authors Full Name Foster, Bethany J. Shults, Justine. Zemel, Babette S. Leonard, Mary B. Institution Department of Pediatrics, Division of Nephrology, Montreal Children's Hospital, McGill University School of Medicine, Montreal, Quebec, Canada. [email protected] Title Risk factors for glucocorticoid-induced obesity in children with steroid-sensitive nephrotic syndrome.[see comment]. Comments Comment in: Pediatr Nephrol. 2007 Mar;22(3):471; author reply 472-3; PMID: 17151875 Source Pediatric Nephrology. 21(7):973-80, 2006 Jul. Abstract The objective of this work was to determine the prevalence of obesity, defined as BMI >95th percentile, in children treated with glucocorticoids for steroid-sensitive nephrotic syndrome (SSNS), and to identify risk factors for the development for glucocorticoid- induced obesity. The experimental design involved a cross-sectional study of 96 individuals (4 to 21 yrs) treated with glucocorticoids for SSNS and 186 healthy reference subjects. Logistic regression was used to generate odds ratios for obesity. Glucocorticoid exposure was classified as recent in the 54 subjects treated with glucocorticoids in the prior six months, and remote in the remaining 42 subjects. Recent exposure was associated with significantly increased odds of obesity [odds ratio (95% CI): 26.14 (7.54, 90.66)] in non-blacks only. Each one-unit increase in maternal BMI was associated with a 35% increase in the odds of obesity in recent SSNS subjects (p=0.003). The effect of maternal BMI on the odds of obe! sity was significantly greater in recent SSNS subjects than in reference subjects (test for interaction p=0.038). The odds of obesity were also significantly increased [odds ratio 5.22 (1.77, 15.41), p=0.003] in all subjects with remote glucocorticoid exposure (black and non-black). These results indicate that non-black race and increased maternal BMI are risk factors for glucocorticoid-induced obesity in subjects with recent exposure. Publication Type Journal Article.
Result <110> Unique Identifier 16739045 Status MEDLINE Authors Kwon HL. Ortiz B. Swaner R. Shoemaker K. Jean-Louis B. Northridge ME. Vaughan RD. Marx T. Goodman A. Borrell LN. Nicholas SW. Harlem Children's Zone Asthma Initiative. Authors Full Name Kwon, Helen L. Ortiz, Benjamin. Swaner, Rachel. Shoemaker, Katherine. Jean-Louis, Betina. Northridge, Mary E. Vaughan, Roger D. Marx, Terry. Goodman, Andrew. Borrell, Luisa N. Nicholas, Stephen W. Harlem Children's Zone Asthma Initiative. Institution Department of Epidemiology, Mailman School of Public Health, Columbia University, 722 W. 168th Street, 7th Floor, New York, NY, 10032, USA. [email protected] Title Childhood asthma and extreme values of body mass index: the Harlem Children's Zone Asthma Initiative. Source Journal of Urban Health. 83(3):421-33, 2006 May. Other ID Source: NLM. PMC2527185 Abstract To examine the association between body mass index (BMI) percentile and asthma in children 2-11 years of age, we performed a cross-sectional analysis of 853 Black and Hispanic children from a community-based sample of 2- to 11-year olds with measured heights and weights screened for asthma by the Harlem Children's Zone Asthma Initiative. Current asthma was defined as parent/guardian-reported diagnosis of asthma and asthma-related symptoms or emergency care in the previous 12 months. Among girls, asthma prevalence increased approximately linearly with increasing body mass index (BMI) percentile, from a low of 12.0% among underweight girls (BMI 95! th percentile). After adjusting for age, race/ethnicity, and household smoking, among girls, having asthma was associated with being at risk for overweight (odds ratio [OR], 2.6; 95% confidence interval [CI], 1.4-5.0) and being overweight (OR, 2.1; 95% CI, 1.2-3.8) compared to normal weight; among boys, having asthma was associated both with overweight (OR, 2.4; 95% CI, 1.4-4.3) and with underweight (OR, 2.9; 95% CI, 1.1-7.7). Large, prospective studies that include very young children are needed to further explore the observed association between underweight and asthma among boys. Early interventions that concomitantly address asthma and weight gain are needed among pre-school and school-aged children. Publication Type Journal Article. Research Support, N.I.H., Extramural. Research Support, Non-U.S. Gov't. Research Support, U.S. Gov't, P.H.S..
Result <111> Unique Identifier 16679218 Status MEDLINE Authors Thorsdottir I. Gunnarsdottir I. Palsson GI. Johannsson E. Authors Full Name Thorsdottir, Inga. Gunnarsdottir, Ingibjorg. Palsson, Gestur I. Johannsson, Erlingur. Institution Unit for Nutrition Research, Landspitali-University Hospital and Department of Food Science, University of Iceland, 101 Reykjavik, Iceland. Title Anthropometric predictors of serum fasting insulin in 9- and 15-year-old children and adolescents. Source Nutrition Metabolism & Cardiovascular Diseases. 16(4):263-71, 2006 May. Abstract BACKGROUND AND AIM: As the prevalence of overweight and obesity increases, the risk of insulin resistance rises. The aim was to study the association between anthropometric measurements and fasting insulin concentration in a population-based sample of 9- and 15-year-old children and adolescents. METHODS AND RESULTS: Subjects were randomly selected 9- and 15-year-old pupils (n=262) in a cross-sectional, population-based study. Weight and height, waist, hip and mid-arm-circumference and subcutaneous skinfolds were measured using standard procedures. Fasting insulin was measured. In general the mean anthropometric measurements increased across insulin quartiles. Higher fasting insulin concentration was seen in overweight children and adolescents than in those of normal weight (8.3+/-4.4 vs. 4.9+/-3.6 mmol/L and 11.0+/-4.4 vs. 9.0+/-4.2 mmol/L in 9- and 15 year-olds, respectively). The odds ratio for having insulin in the highest quartile (age and gender-specific) was, when co! mpared with the lowest quartile, 7.2 (95% CI 3.0-17.2) for body mass index and 6.9 (2.8-16.7) for waist circumference. Other measurements of body fatness were less predictive. About 14-20% of children defined as being of normal weight had high fasting insulin values, i.e., were in the highest quartile of fasting insulin. CONCLUSIONS: Body fatness is positively related to fasting insulin concentration in 9- and 15-year-old children. A large number of normal-weight individuals with high fasting insulin concentration was observed, and these children could be at increased risk of weight gain, compared with normal-weight individuals with normal fasting insulin concentration. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <112> Unique Identifier 16675350 Status MEDLINE Authors Alexis NE. Peden DB. Authors Full Name Alexis, Neil E. Peden, David B. Title Inflammatory response of the airway to inhaled endotoxin correlates with body mass index in atopic patients with asthma but not in normal volunteers. Source Journal of Allergy & Clinical Immunology. 117(5):1185-6, 2006 May. Publication Type Comparative Study. Letter. Research Support, N.I.H., Extramural. Research Support, Non-U.S. Gov't. Research Support, U.S. Gov't, Non-P.H.S..
Result <113> Unique Identifier 16673811 Status MEDLINE Authors Ma GS. Li YP. Hu XQ. Cui ZH. Yang XG. Chen CM. Authors Full Name Ma, Guan-Sheng. Li, Yan-Ping. Hu, Xiao-Qi. Cui, Zhao-Hui. Yang, Xiao-Guang. Chen, Chun-Ming. Institution National Institute for Nutrition and Food Safety, Chinese Center for Disease Control and Prevention, 29 Nan wei Road, Beijing 100050, China. [email protected] Title Report on childhood obesity in China (2). Verification of BMI classification reference for overweight and obesity in Chinese children and adolescents. Source Biomedical & Environmental Sciences. 19(1):1-7, 2006 Feb. Abstract OBJECTIVE: To verify Working Group for Obesity in China (WGOC) recommended body mass index (BMI) classification reference for overweight and obesity in Chinese children and adolescents using the data of 2002 China Nationwide Nutrition and Health Survey. METHODS: Pediatric metabolic syndrome (MetS) and abnormality of each risk factor for MetS were defined using the criteria for US adolescents. Definition of hyper-TC, LDL, and dyslipidemia in adults was applied as well. The average level and abnormality rate of the metabolic indicators were described by BMI percentiles and compared with general linear model analysis. Receiver operating characteristic analysis was used to summarize the potential of BMI to discriminate between the presence and absence of the abnormality of these indicators. RESULTS: There was neither significantly increasing nor significantly decreasing trend of biochemical parameter levels in low BMI percentile range (<65th). Slight increasing trend from the ! 75th and a significant increase were found when BMI > or =85th percentile. In general, the prevalence of the examined risk factors varied slightly when BMI percentile<75th, and substantial increases were consistently seen when BMI percentile > or =75th. As an indicator of hyper-TG, hypertension and MetS, the sensitivity and specificity were equal at the point of BMI<75th percentile, and the Youden's index of risk factors also reached peak point before 75th percentile except for MetS. When the BMI percentile was used as the screening indicator of MetS, Youden's index reached peak point at 85th percentile, just the point in the ROC graph that was nearest to the upper left corner. CONCLUSION: The BMI classification reference for overweight and obesity recommended by WGOC is rational to predict and prevent health risks in Chinese children and adolescents. Lower screening cut-off points, such as 83th percentile or 80th percentile, should not be excluded when they are considered ! as overweight criteria in future intervention or prevention studies. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <114> Unique Identifier 16600926 Status MEDLINE Authors Lawlor DA. Martin RM. Gunnell D. Galobardes B. Ebrahim S. Sandhu J. Ben-Shlomo Y. McCarron P. Davey Smith G. Authors Full Name Lawlor, Debbie A. Martin, Richard M. Gunnell, David. Galobardes, Bruna. Ebrahim, Shah. Sandhu, Jat. Ben-Shlomo, Yoav. McCarron, Peter. Davey Smith, George. Institution Department of Social Medicine, University of Bristol, Canynge Hall, Whiteladies Road, Bristol BS8 2PR, United Kingdom. [email protected] Title Association of body mass index measured in childhood, adolescence, and young adulthood with risk of ischemic heart disease and stroke: findings from 3 historical cohort studies. Source American Journal of Clinical Nutrition. 83(4):767-73, 2006 Apr. Abstract BACKGROUND: It is unclear whether early life body mass index (BMI; in kg/m(2)) is associated with adult cardiovascular disease. OBJECTIVE: The objective was to assess the association of early life BMI with the risk of ischemic heart disease (IHD) and stroke. DESIGN: The association between early life BMI and risk of adult mortality from IHD and stroke was assessed in 3 historical cohort studies in which height and weight had been assessed by using standard procedures. Participants were traced and linked to national mortality data. Participants in the 3 cohorts were born between 1922 and 1937, 1927 and 1956, and 1928 and 1950 and were aged 2-15, 9-18, and 16-22 y, respectively, at the time of assessment of their height and weight. RESULTS: Participants in all 3 cohorts had mean BMIs similar to those reported for contemporary children and young adults, but fewer of the cohort participants were overweight or obese. BMI was not associated with future risk of IHD or stroke in a! ny cohort. The pooled (all 3 cohorts) adjusted hazard ratio per SD of early life BMI was 1.09 (95% CI: 1.01, 1.19) for IHD and 0.94 (95% CI: 0.82, 1.08) for stroke. The pooled hazard ratio of IHD when participants who were overweight or obese for their age were compared with all other participants was 1.34 (95% CI: 0.95, 1.91), and no association was found between overweight or obesity and stroke risk. The effects of BMI did not vary by cohort or by age. CONCLUSION: These results do not provide strong evidence that being overweight or obese in childhood is associated with future cardiovascular disease risk. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <115> Unique Identifier 16477656 Status MEDLINE Authors Mansell AL. Walders N. Wamboldt MZ. Carter R. Steele DW. Devin JA. Monica TH. Miller AL. Wamboldt FS. Authors Full Name Mansell, Anthony L. Walders, Natalie. Wamboldt, Marianne Z. Carter, Rick. Steele, Dale W. Devin, Jerilyn A. Monica, Taylor H. Miller, Alison L. Wamboldt, Frederick S. Institution Department of Pediatrics, Rhode Island Hospital, Brown University, Providence, 02903, USA. [email protected] Title Effect of body mass index on response to methacholine bronchial provocation in healthy and asthmatic adolescents. Source Pediatric Pulmonology. 41(5):434-40, 2006 May. Abstract A linkage between airway hyperreactivity and obesity could partly explain the prevalence of obesity in asthmatics. To test for such a linkage, we analyzed body mass index (BMI), pulmonary function, methacholine bronchial provocation, and asthma severity scores in 216 adolescents (aged 12-18 years), of whom 82 were healthy and 134 were asthmatic. Methacholine provocations in a subgroup of 36 subjects (healthy and asthmatic) enabled us to examine the effects of BMI on dynamic hyperinflation and ventilatory indices during induced bronchospasm. Age- and gender-specific BMI was higher in asthmatics (74 +/- 24%) compared to healthy subjects (61 +/- 28%, P < 0.002). General linear model analysis, in which baseline spirometric results were adjusted for gender, age, race, and height, showed opposing effects of BMI on expiratory flow in controls and asthmatics (P < 0.05), i.e., forced expired volume in 1 sec increased with BMI in controls (P < 0.02), but forced expiratory flow (FEF)! (25-75%) decreased with BMI in asthmatics (P < 0.05). However, linear regression analysis showed no effect of BMI on the provocation dose for methacholine (PD(20)) in either controls or asthmatics, and there was no effect of BMI on asthma severity scores. Overweight (BMI >85th percentile) and nonoverweight subjects had similar degrees of dynamic hyperinflation during positive provocations, but overweight subjects had greater decreases in mean inspiratory flow (mean, 28% vs. 9%, P < 0.05). We conclude that our measurements support a relationship between overweight and baseline flow limitation, rather than a relationship between overweight and airways hyperreactivity, in the linkage between overweight and asthma during adolescence. Publication Type Comparative Study. Journal Article. Research Support, N.I.H., Extramural.
Result <116> Unique Identifier 16570091 Status MEDLINE Authors Dubois L. Girard M. Authors Full Name Dubois, L. Girard, M. Institution Canada Research Chair in Nutrition and Population Health, Department of Epidemiology and Community Medicine, University of Ottawa, Ottawa, Ontario, Canada K1N 6N5. [email protected] Title Early determinants of overweight at 4.5 years in a population-based longitudinal study. Source International Journal of Obesity. 30(4):610-7, 2006 Apr. Abstract OBJECTIVES: The roots of the obesity epidemic need to be traced back as early in life as possible in order to develop effective means for preventing obesity and its health consequences in the future. The aim of this paper is to examine a broad range of factors that may simultaneously contribute to childhood overweight in a population-based cohort of children followed from birth to 4.5 years, to determine which factors exert the most influence in early life. DESIGN: The analyses were performed using data from the Quebec Longitudinal Study of Child Development 1998-2002 (QLSCD). SUBJECTS: The study follows a representative sample (n=2103) of children born in 1998 in the Canadian province of Quebec. MEASURE: Measured height and weight were available for 1550 children aged 4.5 years. At 4.5 years, BMI was analyzed using the US CDC sex- and age-specific growth charts. In order to study children at their highest weights at various ages, odds ratios were presented for high birth ! weight, weight-for-stature at or above the 95th percentile at 5 months, and BMI at or above the 95th percentile at 4.5 years. Monthly weight gain between birth and five months has been analyzed. Children were also evaluated by the Z-score obtained from the standardized weight divided by height. Factors potentially related to children's weight include sex, gestational age and birth rank, breastfeeding, mothers' smoking status during pregnancy, family type at child's birth, and family income before pregnancy and when the children were 5 months and 4.5 years old. Other parental factors such as height and overweight/obesity (based on BMI) and other maternal factors (age, education, immigrant status) were also part of the analysis. RESULTS: Being in the highest quintiles of weight gain between birth and 5 months, as well as maternal smoking during pregnancy, almost double the odds of being overweight at 4.5 years. Parental overweight or obesity also increased the odds of being o! verweight at this age, as well as being raised in middle-income or in poor families. A greater proportion of children born to nonsmoking mothers with higher weights (more than 4000 g) were overweight at 4.5 years, the percentage being greatest for those in the highest weight-gain categories from birth to 5 months. The pattern was different for children born to smoking mothers. The greatest proportion of 4.5-year-old overweight children was seen for children born in the normal weight-range category (3000-4000 g) who were in the highest quintiles of weight gain from birth to 5 months, and for children with high birth weights (more than 4000 g) who were in the lowest quintiles of birth-to-5-months weight gain. Children who were overweight at 4.5 years and who had been born to smoking mothers started life with a birth weight around that for the population means, but they gained more weight in the first 5 months of life than did the children of nonsmoking mothers. CONCLUSION: This study indicates that behavioral and social factors exert critical in! fluences on the onset of childhood overweight in preschool years. From a population-health perspective, interventions aimed at preventing childhood obesity would do well to target smoking pregnant women, as well as nonsmoking pregnant women at risk for giving birth to high-birth-weight children, paying particular attention to rapid weight gain in the first months of life. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <117> Unique Identifier 16314873 Status MEDLINE Authors Voss LD. Metcalf BS. Jeffery AN. Wilkin TJ. Authors Full Name Voss, L D. Metcalf, B S. Jeffery, A N. Wilkin, T J. Institution Department of Endocrinology and Metabolism, Peninsula Medical School, Plymouth, UK. [email protected] Title IOTF thresholds for overweight and obesity and their relation to metabolic risk in children (EarlyBird 20). Source International Journal of Obesity. 30(4):606-9, 2006 Apr. Abstract The International Obesity TaskForce has published paediatric cutoffs from the age of 2 years for overweight and obesity, based on adult thresholds. We question their rationale. The adult cutoffs were based on known health risk; the children's were not. Data from the EarlyBird Study show that BMI category for overweight and obesity in young children are poor markers of insulin resistance and, by implication, of metabolic risk and diabetes. Moreover, BMI is known to track poorly from early childhood to adulthood. We know even less about the tracking of insulin resistance and other indices of metabolic risk from the earliest years. Until we understand more about which children acquire such risk factors, any such thresholds for overweight and obesity should be used with caution in the very young, as they may unnecessarily stigmatise the heavier child. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <118> Unique Identifier 16507848 Status MEDLINE Authors Peters-Golden M. Swern A. Bird SS. Hustad CM. Grant E. Edelman JM. Authors Full Name Peters-Golden, M. Swern, A. Bird, S S. Hustad, C M. Grant, E. Edelman, J M. Institution Division of Pulmonary and Critical Care Medicine, University of Michigan, 6301 MSRB III, 1150 W. Medical Center Drive, Ann Arbor, MI 48109-0642, USA. [email protected] Title Influence of body mass index on the response to asthma controller agents. Source European Respiratory Journal. 27(3):495-503, 2006 Mar. Abstract The incidence of asthma has been positively associated with obesity. Asthma comprises diverse "phenotypes" reflecting heterogeneity in a number of characteristics, including response to therapy. The present authors examined whether body mass index (BMI) influenced the response to placebo, as well as to two asthma controller medications. A post hoc analysis was performed, pooling data from four double-blind, placebo-controlled studies randomising 3,073 moderate asthmatic adults to montelukast (n=1,439), beclomethasone (n=894) or placebo (n=740). The primary end point was asthma control days; other end points were forced expiratory volume in one second, beta-agonist use and nocturnal awakening. Analyses were conducted using BMI classification into normal (<25.0 kg.m-2; 52% of patients), overweight (25-29.9 kg.m-2; 32%) and obese (>or=30.0 kg.m-2; 16%) categories, as well as BMI as a continuous variable. The treatment groups were balanced for BMI, demographic characteristics ! and parameters of asthma control. The placebo response for all end points was generally lower with increasing BMI. Similarly, the response to the inhaled corticosteroid decreased, whereas the response to the leukotriene antagonist remained stable. In conclusion, post hoc data from the present study suggested that body mass index may influence the natural history of asthma control (as reflected by response to placebo) and may differentially influence response to the two active agents, warranting explicit testing in future prospective studies. Publication Type Journal Article. Randomized Controlled Trial. Research Support, Non-U.S. Gov't.
Result <119> Unique Identifier 16159709 Status MEDLINE Authors Lavoie KL. Bacon SL. Labrecque M. Cartier A. Ditto B. Authors Full Name Lavoie, Kim L. Bacon, Simon L. Labrecque, Manon. Cartier, Andre. Ditto, Blaine. Institution Research Center, Department of Chest Medicine, J-3190, Hopital du Sacre-Coeur de Montreal, 5400 Gouin West, Montreal, Quebec, Canada H4J 1C5. [email protected] Title Higher BMI is associated with worse asthma control and quality of life but not asthma severity. Source Respiratory Medicine. 100(4):648-57, 2006 Apr. Abstract Asthma and obesity tend to co-occur, but relatively few studies have linked obesity, measured using body mass index (BMI), to clinically relevant measures of asthma morbidity. This study assessed BMI in a Canadian sample of asthma outpatients, and evaluated associations between BMI and levels of asthma severity, asthma control, and asthma-related quality of life. A total of 382 adult asthma patients underwent demographic and medical history interviews on the day of their clinic visit. Patients' self-reported height and weight were used to calculate BMI (kg/m(2)). Asthma severity was classified according the GINA (2002) guidelines. Patients completed the Asthma Control (ACQ) and Asthma Quality of Life (AQLQ) Questionnaires and underwent standard pulmonary testing (spirometry). A total of 139 (36%) patients had a normal BMI; 149 (39%) patients were overweight; and 94 (25%) patients were obese. There was no relationship between BMI and asthma severity when controlling for age! and sex. Patients with higher BMI scores had higher ACQ and lower AQLQ scores, independent of age, sex and asthma severity. Results identify higher BMI and obesity as potential behavioral factors related to worse asthma control and quality of life, but not asthma severity, and suggest important avenues for asthma management and control initiatives. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <120> Unique Identifier 16374023 Status MEDLINE Authors Garcia-Marcos L. Valverde-Molina J. Sanchez-Solis M. Soriano-Perez MJ. Baeza-Alcaraz A. Martinez-Torres A. Perez-Fernandez V. Guillen-Perez JJ. Authors Full Name Garcia-Marcos, L. Valverde-Molina, J. Sanchez-Solis, M. Soriano-Perez, M J. Baeza-Alcaraz, A. Martinez-Torres, A. Perez- Fernandez, V. Guillen-Perez, J J. Institution Institute of Respiratory Health, University of Murcia, Pabellon Docente HUVA, Campus Ciencias de la SaludES-30120 El Palmar, Spain. [email protected] Title Validity of parent-reported height and weight for defining obesity among asthmatic and nonasthmatic schoolchildren. Source International Archives of Allergy & Immunology. 139(2):139-45, 2006. Abstract BACKGROUND: The relationship between parent-reported and measured height and weight is not well established in schoolchildren. This relationship has never been studied in asthmatic children. The objective of this study is to test the validity of the parent-reported weight and height for defining obesity by BMI and to know whether the perception of this height and weight changes when the child suffers from asthma. METHODS: All classes of children of the target ages of 6-8 years (n = 1,672, participation rate 70.2%) of all schools in four municipalities of Murcia (Spain) were included. Parents were asked about their children's weight and height using a questionnaire which included the International Study of Asthma and Allergies in Childhood (ISAAC) core questions on asthma. Parents were not aware that their children were going to be weighed and measured within 1 week's time. Measurements were performed using a rigid stadiometer to the nearest 0.1 cm and a scale to the neares! t 0.1 kg. RESULTS: The bias (reported minus real) was, respectively, for nonasthmatics and asthmatics: weight +0.42 kg (95% CI +0.24; +0.59 kg) versus +0.97 kg (+0.50; +1.44 kg), height +2.37 cm (+2.06; +2.68 cm) versus +2.87 cm (+1.87; +3.87 cm); BMI -0.39 kg/m(2) (-0.52; -0.23 kg/m(2)) versus -0.23 kg/m(2) (-0.58; +0.13 kg/m(2)). Diagnostic accuracy of obesity calculated from reported measurements was, respectively, for nonasthmatics and asthmatics: sensitivity 78.0 versus 77.8%, specificity 96.2 versus 94.5%, positive predictive value 77.2 versus 73.7% and negative predictive value 96.4 versus 91.7%. CONCLUSIONS: Reported weights and heights had large biases, comparable between parents of both asthmatic and those of nonasthmatic children. However, this information could be reasonably valid for classifying children as obese or nonobese in large epidemiological studies. Publication Type Comparative Study. Journal Article. Research Support, Non-U.S. Gov't. Validation Studies.
Result <121> Unique Identifier 16244093 Status MEDLINE Authors Gomez Real F. Svanes C. Bjornsson EH. Franklin KA. Gislason D. Gislason T. Gulsvik A. Janson C. Jogi R. Kiserud T. Norback D. Nystrom L. Toren K. Wentzel-Larsen T. Omenaas E. Authors Full Name Gomez Real, F. Svanes, C. Bjornsson, E H. Franklin, K A. Gislason, D. Gislason, T. Gulsvik, A. Janson, C. Jogi, R. Kiserud, T. Norback, D. Nystrom, L. Toren, K. Wentzel-Larsen, T. Omenaas, E. Institution Department of Gynecology and Obstetrics, Haukeland University Hospital, 5021 Bergen, Norway. [email protected] Title Hormone replacement therapy, body mass index and asthma in perimenopausal women: a cross sectional survey.[erratum appears in Thorax. 2006 Mar;61(3):274 Note: Franklin, K [corrected to Franklin, KA]]. Source Thorax. 61(1):34-40, 2006 Jan. Abstract BACKGROUND: Hormone replacement therapy (HRT) and obesity both appear to increase the risk of asthma. A study was undertaken to investigate the association of HRT with asthma and hay fever in a population of perimenopausal women, focusing on a possible interaction with body mass index (BMI). METHODS: A postal questionnaire was sent to population based samples in Denmark, Estonia, Iceland, Norway, and Sweden in 1999-2001, and 8588 women aged 25-54 years responded (77%). Pregnant women, women using oral contraceptives, and women <46 years were excluded. Analyses included 2206 women aged 46-54 years of which 884 were menopausal and 540 used HRT. Stratified analyses by BMI in tertiles were performed. RESULTS: HRT was associated with an increased risk for asthma (OR 1.57 (95% CI 1.07 to 2.30)), wheeze (OR 1.60 (95% CI 1.22 to 2.10)), and hay fever (OR 1.48 (95% CI 1.15 to 1.90)). The associations with asthma and wheeze were significantly stronger among women with BMI in the low! er tertile (asthma OR 2.41 (95% CI 1.21 to 4.77); wheeze OR 2.04 (95% CI 1.23 to 3.36)) than in heavier women (asthma: p(interaction) = 0.030; wheeze: p(interaction) = 0.042). Increasing BMI was associated with more asthma (OR 1.08 (95% CI 1.05 to 1.12) per kg/m2). This effect was only found in women not taking HRT (OR 1.10 (95% CI 1.05 to 1.14) per kg/m2); no such association was detected in HRT users (OR 1.00 (95% CI 0.92 to 1.08) per kg/m2) (p(interaction) = 0.046). Menopause was not significantly associated with asthma, wheeze, or hay fever. CONCLUSIONS: In perimenopausal women there is an interaction between HRT and BMI in the effects on asthma. Lean women who were HRT users had as high a risk for asthma as overweight women not taking HRT. It is suggested that HRT and overweight increase the risk of asthma through partly common pathways. Publication Type Journal Article. Multicenter Study. Research Support, Non-U.S. Gov't.
Result <122> Unique Identifier 16039767 Status MEDLINE Authors Cohen DA. Finch BK. Bower A. Sastry N. Authors Full Name Cohen, Deborah A. Finch, Brian K. Bower, Aimee. Sastry, Narayan. Institution RAND Corporation, 1776 Main Street, Santa Monica, CA 90407, USA. [email protected] Title Collective efficacy and obesity: the potential influence of social factors on health. Source Social Science & Medicine. 62(3):769-78, 2006 Feb. Abstract Social determinants have been identified as a fundamental cause of health and disease in most industrialized countries. However, much less is known about which characteristics of communities may lead to disparities in health outcomes. Collective efficacy--the willingness of community members to look out for each other and intervene when trouble arises--is a social factor shown to be associated with outcomes related to obesity, including premature mortality and cardiovascular disease. The objective of this study is to determine whether neighborhood collective efficacy is associated with individual measures of body mass index (BMI) in adolescents. We use a multi-level, cross-sectional survey in Los Angeles County, involving 807 adolescents in 684 households in 65 neighborhoods in addition to a sample of 3000 adult respondents. The main outcomes measures are BMI, at risk of overweight, and overweight status. Using a two-level model, we find significant relationships between c! ollective efficacy and all three outcomes, net of levels of neighborhood disadvantage. The associations between BMI and collective efficacy could potentially be explained by several factors, including a metabolic pathway, neighborhood differences in the physical and social environments, or a combination of these two. If group-level collective efficacy is indeed important in the regulation of individual-level net energy balance, it suggests that future interventions to control weight by addressing the social environment at the community level may be promising. Publication Type Journal Article. Research Support, U.S. Gov't, P.H.S..
Result <123> Unique Identifier 16332664 Status MEDLINE Authors Owen CG. Martin RM. Whincup PH. Davey-Smith G. Gillman MW. Cook DG. Authors Full Name Owen, Christopher G. Martin, Richard M. Whincup, Peter H. Davey-Smith, George. Gillman, Matthew W. Cook, Derek G. Institution Division of Community Health Sciences, St George's, University of London, London, United Kingdom. [email protected] Title The effect of breastfeeding on mean body mass index throughout life: a quantitative review of published and unpublished observational evidence. [Review] [69 refs] Source American Journal of Clinical Nutrition. 82(6):1298-307, 2005 Dec. Abstract BACKGROUND: Evidence from observational studies has suggested that breastfeeding may reduce the prevalence of obesity in later life. OBJECTIVE: The objective was to examine whether initial breastfeeding is related to lower mean body mass index (BMI; in kg/m(2)) throughout life. DESIGN: The study was a systematic review of published studies investigating the association between infant feeding and a measure of obesity or adiposity in later life, which was supplemented with data from unpublished sources. Analyses were based on the mean differences in BMI between those subjects who were initially breastfed and those who were formula-fed (expressed as breastfed minus bottle-fed), which were pooled by using fixed-effects models throughout. RESULTS: From 70 eligible studies, 36 mean differences in BMI (from 355 301 subjects) between those breastfed and those formula-fed (reported as exclusive feeding in 20 studies) were obtained. Breastfeeding was associated with a slightly lower! mean BMI than was formula feeding (-0.04; 95% CI: -0.05, -0.02). The mean difference in BMIs appeared larger in 15 small studies of <1000 subjects (-0.19; 95% CI: -0.31, -0.08) and smaller in larger studies of >or=1000 subjects (-0.03; 95% CI: -0.05, -0.02). An Egger test was statistically significant (P = 0.002). Adjustment for socioeconomic status, maternal smoking in pregnancy, and maternal BMI in 11 studies abolished the effect (-0.10; 95% CI: -0.14, -0.06 before adjustment; -0.01; 95% CI: -0.05, 0.03 after adjustment). CONCLUSIONS: Mean BMI is lower among breastfed subjects. However, the difference is small and is likely to be strongly influenced by publication bias and confounding factors. Promotion of breastfeeding, although important for other reasons, is not likely to reduce mean BMI. [References: 69] Publication Type Journal Article. Meta-Analysis. Research Support, Non-U.S. Gov't. Review.
Result <124> Unique Identifier 16303694 Status MEDLINE Authors Eriksson M. Rasmussen F. Nordqvist T. Authors Full Name Eriksson, Marit. Rasmussen, Finn. Nordqvist, Tobias. Institution Division of Epidemiology, Stockholm Centre for Public Health, Sweden. Title Changes in shape and location of BMI distributions of Swedish children. Source Acta Paediatrica. 94(11):1558-65, 2005 Nov. Abstract AIMS: One aim was to disentangle how the shape and location of the BMI distribution changed among Swedish children over a 12 y period. Another aim was to identify the age during childhood when changes occurred or became manifest. METHODS: Two population-based cohorts-2,591 children from Stockholm born 1985-1987 and 3,650 from Gothenburg born 1973-1975-were compared with respect to BMI distributions from 2 to 15 y of age. RESULTS: Differences between the BMI distributions of the two cohorts were present from 5-6 y of age. From age 7, the children born in 1985-1987 and belonging to the upper parts of the BMI distribution, e.g. those above the 90th or 95th BMI percentiles, had much higher BMI mean values compared to their counterparts born 12 y earlier. Comparisons with respect to the 5th, 10th, 25th, 50th, 75th, 90th and 95th BMI percentiles showed that changes appeared above the 25th percentile and became increasingly pronounced in the upper parts of the BMI distributions.C! ONCLUSION: School-aged children in the rightmost parts of the BMI distributions may be more susceptible to "obesogenic" environmental exposures than those in the middle or leftmost parts. The results support the suggestion that the period of BMI rebound is critical for the development of obesity. Publication Type Comparative Study. Journal Article.
Result <125> Unique Identifier 16044176 Status MEDLINE Authors Steinberger J. Jacobs DR. Raatz S. Moran A. Hong CP. Sinaiko AR. Authors Full Name Steinberger, J. Jacobs, D R. Raatz, S. Moran, A. Hong, C-P. Sinaiko, A R. Institution Department of Pediatrics, University of Minnesota Medical School, Minneapolis, MN 55455, USA. [email protected] Title Comparison of body fatness measurements by BMI and skinfolds vs dual energy X-ray absorptiometry and their relation to cardiovascular risk factors in adolescents.[erratum appears in Int J Obes (Lond). 2006 Jul;30(7):1170]. Source International Journal of Obesity. 29(11):1346-52, 2005 Nov. Abstract OBJECTIVE: To compare estimates of adiposity by dual emission X-ray absorptiometry (DXA), skinfolds and body mass index (BMI); and to evaluate the relation of these measures to cardiovascular risk in adolescents. DESIGN: In a cohort of adolescents participating in a longitudinal study of insulin resistance, Slaughter formulas were used to estimate adiposity from skinfolds and DXA was used to estimate adiposity as % body fat (%BF) and fat mass (FBM). BMI, blood pressure, lipids and insulin resistance were measured. SUBJECTS: Male and female, 11-17 y old (n=130). MEASUREMENTS: To compare DXA with two office-based methods of assessing fatness and cardiovascular risk. RESULTS: Slaughter estimates were highly correlated with DXA (%BF r=0.92, P=0.0001; FBM r=0.96, P=0.0001). Correlations were similar in heavy and thin children. BMI was also highly correlated with DXA (%BF r=0.85, P=0.0001; FBM r=0.95, P=0.0001), and these relations were stronger in heavy than thin children. BMI ! and the Slaughter formulas were similar to DXA in their relations to cardiovascular risk factors. CONCLUSIONS: Adiposity by BMI and Slaughter formulas are highly correlated with DXA and similarly related to cardiovascular risk factors. BMI is easy to obtain and is an acceptable method for initial office estimation of body fatness. BMI and skinfolds compare well with DXA in predicting adverse cardiovascular risk profile. Publication Type Comparative Study. Journal Article. Research Support, N.I.H., Extramural.
Result <126> Unique Identifier 16236985 Status MEDLINE Authors Chen Y. Rennie D. Cormier Y. Dosman J. Authors Full Name Chen, Yue. Rennie, Donna. Cormier, Yvon. Dosman, James. Institution Department of Epidemiology and Community Medicine, Faculty of Medicine, University of Ottawa, 451 Smyth Rd, Ottawa, ON, Canada K1H 8M5. [email protected] Title Sex specificity of asthma associated with objectively measured body mass index and waist circumference: the Humboldt study. Source Chest. 128(4):3048-54, 2005 Oct. Abstract STUDY OBJECTIVE: To investigate the possibility of sex specificity for the association of obesity and asthma using objective measures of body mass index (BMI) and waist circumference (WC). DESIGN: Cross-sectional study of adults (n = 2,057) living in Humboldt, SK, Canada in 2003. SETTING: A rural community. MEASUREMENTS: Ever-asthma was defined as lifetime physician- diagnosed asthma, and recent asthma was defined as asthma diagnosed by a physician during the past 12 months. BMI and WC were objectively measured. RESULTS: Among the participants, 5.6% of men and 10.0% of women reported having ever-asthma, and 2.7% and 6.0% had recent asthma, respectively. Higher levels of both BMI and WC were significantly associated with asthma in women but not in men. The adjusted odds ratios for women with a BMI of at least 30.0 kg/m2 relative to women with a BMI of < 25.0 kg/m2 were 2.06 (95% confidence interval [CI], 1.42 to 4.05) for ever-asthma and 3.47 (95% CI, 1.64 to 7.32) for recen! t asthma. CONCLUSIONS: Our study demonstrated that the increased risk of asthma associated with obesity was only significant in women but not in men even when BMI was objectively measured, and this association was robust to the anthropometric measures. Publication Type Comparative Study. Journal Article. Research Support, Non-U.S. Gov't.
Result <127> Unique Identifier 16227047 Status MEDLINE Authors Jani M. Ogston S. Mukhopadhyay S. Authors Full Name Jani, Meghna. Ogston, Simon. Mukhopadhyay, Somnath. Institution Division of Maternal and Child Health Sciences, University of Dundee Medical School, Ninewells Hospital and Medical School, Dundee, Scotland, UK. Title Annual increase in body mass index in children with asthma on higher doses of inhaled steroids. Source Journal of Pediatrics. 147(4):549-51, 2005 Oct. Abstract There is a greater annual increase in body mass index in children with asthma receiving inhaled steroids at a dose > or =400 microg/day (0.5 kg/m2/year; n=100) compared with those receiving < or =200 microg/day (0.1 kg/m2/year; n=98) (P=.0003). This is consistent with an annual increase in body fat in children with asthma receiving > or =400 microg/day of inhaled steroids. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <128> Unique Identifier 16220765 Status MEDLINE Authors Wright JD. Powell MA. Mutch DG. Rader JS. Gibb RK. Gao F. Herzog TJ. Authors Full Name Wright, Jason D. Powell, Matthew A. Mutch, David G. Rader, Janet S. Gibb, Randall K. Gao, Feng. Herzog, Thomas J. Institution Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Washington University School of Medicine, St Louis, MO 63110, USA. [email protected] Title Relationship of ovarian neoplasms and body mass index. Source Journal of Reproductive Medicine. 50(8):595-602, 2005 Aug. Abstract OBJECTIVE: To describe the distribution of benign and malignant ovarian neoplasms among overweight and obese women. STUDY DESIGN: A review of patients who presented with a preoperative diagnosis of a pelvic mass between 1996 and 2001 was performed; 1,096 patients were identified. Patients were stratified by body mass index into 3 groups: normal weight, overweight and obese. The pathologic findings in the 3 groups were compared. RESULTS: Complete follow-up was available on 668 patients. Overall, 248 patients were obese, 176 were overweight, and 244 had a normal body mass index. A significant difference existed in the pathologic findings in the 3 groups (p = 0.049). Women with normal body mass indices were more likely to have malignant ovarian tumors (35.2%) than were the overweight (23.9%) and obese (25.8%) women. Conversely, borderline ovarian tumors were less frequent in women with body mass indices of <25 (5.7%) than in the overweight (13.1%) and obese (10.9%) patients. ! Benign ovarian neoplasms occurred in 20-25% of the women. CONCLUSION: Significant differences exist in the distribution of ovarian neoplasms among women with different body mass indices. Obese women are more likely to have ovarian tumors of low malignant potential, while women with normal body mass indices more commonly have invasive ovarian tumors. Body mass index may be an important factor in preoperative counseling and risk assessment. Publication Type Comparative Study. Journal Article.
Result <129> Unique Identifier 16210050 Status MEDLINE Authors Calvert J. Burney P. Authors Full Name Calvert, James. Burney, Peter. Institution Department of Public Health Sciences, King's College School of Medicine, London, United Kingdom. [email protected] Title Effect of body mass on exercise-induced bronchospasm and atopy in African children. Source Journal of Allergy & Clinical Immunology. 116(4):773-9, 2005 Oct. Abstract BACKGROUND: Sensitization to allergen is common in rural populations in less affluent countries, but atopic disease is less frequent than in richer countries. Variables explaining this dichotomy may provide insight into underlying mechanisms of atopic diseases like asthma. OBJECTIVE: To test whether risk of exercise-induced bronchospasm (EIB) in urbanized African populations is increased in association with greater skin sensitivity or increased body mass. METHODS: A total of 3322 children were enrolled in a prevalence survey of EIB in urban and rural South Africa. Children responding positively to an exercise challenge and a random sample of children responding negatively were recruited into a case-control study (393 controls, 380 cases). Subjects were investigated by using allergen skin prick testing, anthropometry, and assay of IgE. Stools were analyzed for parasite infestation. RESULTS: The prevalence of EIB was higher in urban (14.9%) than rural (8.9%) areas (P < .0001! ). The difference in risk of EIB between urban and rural subjects was associated with atopy (odds ratio [OR] for upper tertile of skin wheal diameter, 2.65; 95% CI, 1.43-4.89; P < .0001), increasing weight (OR for upper tertile of body mass index [BMI], 2.17; 95% CI, 1.45-3.26; P = .001), and affluence. Increasing BMI was also associated with a greater strength of association between specific IgE and the corresponding skin test (Dermatophagoides pteronyssinus, OR for a positive skin test result in presence of specific IgE: heavier subjects, OR, 34.6; 95% CI, 0.9-109.3; P < .0001; lighter subjects, OR, 8.05; 95% CI, 2.74-23.6; P < .001). CONCLUSION: Increases in BMI of rural children in subsistence economies may lead to an increased prevalence of atopic disease. This observation merits further investigation in prospective studies. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <130> Unique Identifier 16190953 Status MEDLINE Authors Okada T. Kuromori Y. Miyashita M. Yoshino Y. Iwata F. Hara M. Harada K. Authors Full Name Okada, Tomoo. Kuromori, Yuki. Miyashita, Michio. Yoshino, Yayoi. Iwata, Fujihiko. Hara, Mitsuhiko. Harada, Kensuke. Institution Department of Pediatrics, Nihon University School of Medicine, Tokyo, Japan. [email protected] Title Assessment of individual changes in body fatness in boys during early pubertal period. Source Pediatrics International. 47(5):495-7, 2005 Oct. Abstract BACKGROUND: In order to know whether the changes in indexes of overweight, body mass index (BMI; kg/m2) and percentage of overweight (POW) (%), really represent the tendency toward obesity, we examined longitudinal individual changes in these indexes, and the change in body composition in boys during early pubertal period. METHODS: The subjects were 50 school boys who lived in Shizuoka, Japan. Standing height and weight were measured, and BMI and POW were obtained. Body fat percentage (BF%), fat mass (FM) and lean body mass (LBM) were estimated by bioelectrical impedance method. The influence of predictive variables (LBM, FM) on the changes in BMI and POW was investigated by multiple regression analysis. We examined the 3-year changes in BMI, POW and predictive variables in each individual, from 9 to 12 years of age. RESULTS: The mean change of BMI was 1.7 +/- 0.3 (mean +/- SEM) kg/m2 and that of POW was 2.2 +/- 1.9%. The influence of predictive variables on the changes in! BMI and POW was determined. The variance of the change in POW could be explained by that in FM (r(2) = 0.737, P < 0.0001), while the change in BMI was influenced by both LBM and FM (r2 = 0.891, P < 0.0001). CONCLUSIONS: Based on the definition of obesity, POW is the better index of body fatness to assess its individual change for boys during early pubertal period, because the index independent from the change in LBM is supposed to be the appropriate index for obesity in practical use. Publication Type Journal Article.
Result <131> Unique Identifier 16083224 Status MEDLINE Authors Jirapinyo P. Densupsoontorn N. Kongtragoolpitak S. Wong-Arn R. Thamonsiri N. Authors Full Name Jirapinyo, Pipop. Densupsoontorn, Narumoon. Kongtragoolpitak, Supinya. Wong-Arn, Renu. Thamonsiri, Nuchnoi. Institution Department of Pediatrics, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok 10700, Thailand. [email protected] Title Increasing risks of becoming obese after 6 years in primary school: comparing the relative risks among some schools in Bangkok, Saraburi and Sakolnakorn. Source Journal of the Medical Association of Thailand. 88(6):829-32, 2005 Jun. Abstract The authors carried out a retrospectively study of bodyweights of primary-school children from Grade I to Grade VI in 4 schools from Bangkok, one school from Saraburi and data of school children from a district in Sakolnakorn with a six year follow-up period. In the cohort there were 437 children from Bangkok, 225 children from Saraburi and 633 children from Sakolnakorn. Initial data show that prevalence of obesity at grade I in schools from Bangkok, Saraburi and Sakolnakorn were 16%, 23% and 4%, respectively. However, when these children were in grade VI, the prevalence of obesity increased to 31%, 30% and 9%, respectively. Relative risks of becoming obese at grade VI in children who were overweight and obese at grade I are 3 and 5 fold in Bangkok, 2 and 3 fold in Saraburi, 6 and 12 fold in Sakolnakorn, respectively. The present study shows that prevalence of obesity increased at quite dramatic rates during the primary school period in these study groups. Publication Type Journal Article.
Result <132> Unique Identifier 16048595 Status MEDLINE Authors Vester U. Schaefer A. Kranz B. Wingen AM. Nadalin S. Paul A. Malago M. Broelsch CE. Hoyer PF. Authors Full Name Vester, Udo. Schaefer, Antonia. Kranz, Birgitta. Wingen, Anne-Margret. Nadalin, Silvio. Paul, Andreas. Malago, Massimo. Broelsch, Christoph E. Hoyer, Peter F. Institution Clinic of Pediatric Nephrology, University of Duisburg-Essen, Essen, Germany. [email protected] Title Development of growth and body mass index after pediatric renal transplantation. Source Pediatric Transplantation. 9(4):445-9, 2005 Aug. Abstract Suboptimal final height and marked weight gain after renal transplantation (RTx) are common and may result in obesity. Steroid free immunosuppression has been advocated to improve growth and limit weight gain. We evaluated retrospectively the evolution of growth and body mass index (BMI) after renal transplantation to study risk factors for weight gain under steroid based treatment. Sixty-four pediatric patients (age 9.9 +/- 5.0 yr) were included in the study. To allow comparison between different age groups, standard deviation scores (SDS) for height and BMI for height age were calculated at time of transplantation and 3, 6, 9, 12, 24, 36, 48 and 60 months later. Induction immunosuppression consisted of basiliximab, cyclosporine and prednisone. Growth retardation at time of RTx was obvious with a SDS for height of -2.20 +/- 1.34. Height during the first year improved to an SDS of -2.0 +/- 1.27 (p < 0.01) but did further not increase in year 2 and 3. More than 40% of all p! atients remained 2 SDS below normal mean. SDS BMI for height age at transplantation was -0.19 +/- 0.98 and increased significantly during the first 3 months after transplantation to +0.64 +/- 1.07 (p < 0.01). Thereafter, BMI remained stable but did not decline to pretransplant values. A SDS BMI for height age of more than 2 SDS was observed in 2, 6, 9 and 11% of children at RTx and 1, 2 and 3 yr later respectively. BMI gain over 3 yr was significantly enhanced in children whose parents (especially the mother) were overweight. No influence of gender, BMI at RTx, dialysis modality prior to RTx or rejection episodes could be detected. We conclude that after RTx children exhibit some improvement in growth but height remains suboptimal. The BMI does increase significantly during the first months after RTx and does not return to baseline values under steroid-based immunosuppression. Obesity (>2 SDS above normal) does not occur more often than in the normal population. The most pr! edictive parameter of inappropriate weight gain during 3 yr is the BMI of the mother. We would speculate that steroids may play a major role in weight gain in the early phase after RTx. However, genetic or environmental factors predict the long-term weight development. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <133> Unique Identifier 15983329 Status MEDLINE Authors Schaefer-Graf UM. Pawliczak J. Passow D. Hartmann R. Rossi R. Buhrer C. Harder T. Plagemann A. Vetter K. Kordonouri O. Authors Full Name Schaefer-Graf, Ute M. Pawliczak, Julia. Passow, Doerte. Hartmann, Reinhard. Rossi, Rainer. Buhrer, Christoph. Harder, Thomas. Plagemann, Andreas. Vetter, Klaus. Kordonouri, Olga. Institution Department of Obstetrics, Vivantes Medical Center Berlin-Neukolln, Rudower Strasse 48, D-12351 Berlin, Germany. ute.schaefer- [email protected] Title Birth weight and parental BMI predict overweight in children from mothers with gestational diabetes. Source Diabetes Care. 28(7):1745-50, 2005 Jul. Abstract OBJECTIVE: To investigate the growth of children from pregnancies with gestational diabetes mellitus (GDM) and its association with antenatal maternal, fetal, and recent anthropometric parameters of mother and father. RESEARCH DESIGN AND METHODS: In 324 pregnancies of Caucasian women with GDM, BMI before pregnancy, maternal glycemic values, and measurements of the fetal abdominal circumference were recorded. The weight and height of infants were measured at birth and at follow-up at 5.4 years (range 2.5-8.5). In addition, somatic data from routine examinations at 6, 12, and 24 months and the BMI of parents at follow-up were obtained. BMI standard deviation scores (SDSs) were calculated based on age-correspondent data. RESULTS: At all time points, BMI was significantly above average (+0.82 SDS at birth; +0.56 at 6, +0.35 at 12, and +0.32 at 24 months; and +0.66 at follow-up; P < 0.001). BMI at birth was related to BMI at follow-up (r = 0.27, P < 0.001). The rate of overweig! ht at follow-up was 37% in children with birth BMI > or =90th percentile and 25% in those with normal BMI at birth (P < 0.05). Abdominal circumference of third trimester and postprandial glucose values were related to BMI at follow-up (r = 0.22 and r = 0.18, P < 0.01). Recent maternal, paternal, and birth BMI were independent predictors of BMI at follow-up (r = 0.42, P < 0.001). Sixty- nine percent of children of parents with BMI > or =30 kg/m(2) were overweight at follow-up compared with 20% of those with parental BMI <30 kg/m(2) (P < 0.001). CONCLUSIONS: Children of mothers with GDM have a high rate of overweight that is associated both with intrauterine growth and parental obesity. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <134> Unique Identifier 15962875 Status MEDLINE Authors Vignolo M. Silvestri M. Parodi A. Pistorio A. Battistini E. Rossi GA. Aicardi G. Authors Full Name Vignolo, Marina. Silvestri, Michela. Parodi, Arianna. Pistorio, Angela. Battistini, Elena. Rossi, Giovanni A. Aicardi, Giorgio. Institution Pediatric Clinic, University of Genoa, Genoa, Italy. Title Relationship between body mass index and asthma characteristics in a group of Italian children and adolescents. Source Journal of Asthma. 42(3):185-9, 2005 Apr. Abstract The prevalence of asthma and obesity, two often associated conditions, is influenced not only by age and gender but also by lifestyle factors. This study aimed to determine whether, in a Mediterranean northern Italian region, Liguria, an increased prevalence of obesity could be detected in asthmatic children and adolescents and to evaluate the possible relationship between body mass index (BMI) and the characteristics and/or severity of asthma. BMI was determined in 554 asthmatic subjects (2.2-16.1 years) and 625 age-matched controls; BMI was expressed as a continuous variable in standard deviation score (SDS) units, determined as difference between the individual observed value and the reference mean for age and sex, divided by the corresponding standard deviation (BMI-SDS). Overweight/obesity was set at BMI-SDS of 2 or more. BMI-SDS was significantly higher in controls than in asthmatics (p = 0.04); however, the proportion of overweight/obesity subjects (BMI-SDS > or = 2! ) was similar in controls and in asthmatic patients (p = 0.08). Evaluation of the asthmatic group revealed that BMI-SDS was independent of gender (p = 0.57), atopic sensitization (p = 0.69), and comorbidity with other allergic symptoms (p = 0.60). By contrast, BMI-SDS was lower in preschool-age children than in school-age children and adolescents (p < 0.0001), in subjects with a high rate of acute respiratory tract infections (p = 0.04), and in those not treated with inhaled corticosteroids (IGCs) (p = 0.02). Although an increase in the prevalence of overweight/obesity was not detected in asthmatic children and adolescents, the results reported here suggest a preventive surveillance of calorie intake and a promotion of physical activity in children requiring long-term treatment with inhaled glucocorticosteroids. Publication Type Journal Article.
Result <135> Unique Identifier 15930225 Status MEDLINE Authors Janssen I. Katzmarzyk PT. Srinivasan SR. Chen W. Malina RM. Bouchard C. Berenson GS. Authors Full Name Janssen, Ian. Katzmarzyk, Peter T. Srinivasan, Sathanur R. Chen, Wei. Malina, Robert M. Bouchard, Claude. Berenson, Gerald S. Institution Department of Community Health and Epidemiology, School of Physical and Health Education, Queen's University, Kingston, ON, K7L 3N6, Canada. [email protected] Title Combined influence of body mass index and waist circumference on coronary artery disease risk factors among children and adolescents. Source Pediatrics. 115(6):1623-30, 2005 Jun. Abstract OBJECTIVES: In adult populations, it is recognized widely that waist circumference (WC) predicts health risk beyond that predicted by BMI alone; current recommendations for adults are that a combination of BMI and WC be used to classify obesity-related health risk. For children and adolescents, however, little is known about the combined influence of BMI and WC on health outcomes. The objectives of this study were to determine whether BMI and WC predict coronary artery disease (CAD) risk factors independently for children and adolescents and to assess the clinical utility of using WC in combination with BMI to identify CAD risk. METHODS: Subjects included 2597 black and white, 5- to 18-year-old, male and female youths. Outcome measures included 7 CAD risk factors. In the first analysis step, BMI and WC were used as continuous variables to predict CAD risk factors. In the second analysis step, participants were placed into normal-weight, overweight, and obese BMI categories! and, within each BMI category, CAD risk factors were compared for groups with low and high WC values. RESULTS: When BMI and WC were included in the same regression model to predict CAD risk factors, the added variance above that predicted by BMI or WC alone was minimal, which indicated that BMI and WC did not have independent effects on the risk factors. For example, for systolic blood pressure, BMI alone explained 7.3% of the variance, WC alone explained 7.7% of the variance, and the combination of BMI and WC explained 8.1% of the variance. When BMI and WC values were categorized with a threshold approach, WC provided information on CAD risk beyond that provided by BMI alone, particularly when the categories were used to predict elevated CAD risk factor levels. For instance, in the overweight BMI category, the high-WC group was approximately 2 times more likely to have high triglyceride levels, high insulin levels, and the metabolic syndrome, compared with the low-WC grou! p. CONCLUSION: These findings provide some evidence that a combination of BMI and WC should be used in clinical settings to evaluate the presence of elevated health risk among children and adolescents. Publication Type Journal Article. Research Support, N.I.H., Extramural. Research Support, Non-U.S. Gov't. Research Support, U.S. Gov't, P.H.S..
Result <136> Unique Identifier 15870687 Status MEDLINE Authors Hasan RA. Nolan BM. Authors Full Name Hasan, Rashed A. Nolan, Brian M. Title Obesity and asthma.[comment]. Comments Comment on: J Pediatr. 2004 Feb;144(2):162-8; PMID: 14760253 Source Journal of Pediatrics. 146(5):714; author reply 714-5, 2005 May. Publication Type Comment. Letter.
Result <137> Unique Identifier 15754333 Status MEDLINE Authors Baillargeon J. Langevin AM. Lewis M. Grady JJ. Thomas PJ. Mullins J. Estrada J. Pitney A. Sacks N. Pollock BH. Authors Full Name Baillargeon, Jacques. Langevin, Anne-Marie. Lewis, Margaret. Grady, James J. Thomas, Paul J. Mullins, Judith. Estrada, Jaime. Pitney, Aaron. Sacks, Nancy. Pollock, Brad H. Institution Center for Epidemiology and Biostatistics, University of Texas Health Science Center, San Antonio, Texas 78229-3900, USA. [email protected] Title Therapy-related changes in body size in Hispanic children with acute lymphoblastic leukemia. Source Cancer. 103(8):1725-9, 2005 Apr 15. Abstract BACKGROUND: The objective of this study was to examine changes over time in body mass index (BMI) from diagnosis through chemotherapy for pediatric patients with B-precursor acute lymphoblastic leukemia (ALL). METHODS: The study cohort consisted of 141 white Hispanic pediatric patients who were diagnosed with ALL and were treated at 2 South Texas pediatric oncology centers between 1993 and 2002. Changes in age-standardized and gender-standardized BMI scores were assessed. RESULTS: The study cohort exhibited a steady increase in age-adjusted and gender-adjusted BMI scores for the first 12 months of therapy, a modest increase in BMI scores during the 18-23 month and 24-29 month periods, followed by a slight decrease in BMI scores at 30 months (end of therapy). A repeated-measures analysis indicated significant effects for time (P = 0.019) and time by baseline BMI category interaction (P = 0.0001) but no significant interaction effect between time and gender (P = 0.65). CONCL! USIONS: Although it is known that leukemia therapy is associated with prevalent obesity in survivorship, its pattern of development during therapy has not been elucidated. In the current cohort of Hispanic children with ALL, BMI scores were elevated at diagnosis (mean +/- standard deviation standardized BMI Z score, 0.33 +/- 1.4), then increased, and remained elevated for the entire duration of chemotherapy. Patients who were classified as normal weight exhibited an increase in BMI over time; patients who were classified as overweight at diagnosis exhibited BMI patterns that were relatively stable; and patients who were classified as obese exhibited a very slight decline over time. These findings suggest that the risk for chemotherapy-related weight gain applies predominantly to children who begin ALL therapy within a normal weight range. (c) 2005 American Cancer Society. Publication Type Journal Article. Research Support, U.S. Gov't, P.H.S..
Result <138> Unique Identifier 15800295 Status MEDLINE Authors Li C. Kaur H. Choi WS. Huang TT. Lee RE. Ahluwalia JS. Authors Full Name Li, Chaoyang. Kaur, Harsohena. Choi, Won S. Huang, Terry T-K. Lee, Rebecca E. Ahluwalia, Jasjit S. Institution Department of Preventive Medicine and Public Health, Kansas Cancer Institute, University of Kansas School of Medicine, Kansas City, KS, USA. [email protected] Title Additive interactions of maternal prepregnancy BMI and breast-feeding on childhood overweight. Source Obesity Research. 13(2):362-71, 2005 Feb. Abstract OBJECTIVE: To examine the interactions of maternal prepregnancy BMI and breast-feeding on the risk of overweight among children 2 to 14 years of age. RESEARCH METHODS AND PROCEDURES: The 1996 National Longitudinal Survey of Youth, Child and Young Adult data in the United States were analyzed (n = 2636). The weighted sample represented 51.3% boys, 78.0% whites, 15.0% blacks, and 7.0% Hispanics. Childhood overweight was defined as BMI >/=95th percentile for age and sex. Maternal prepregnancy obesity was determined as BMI >/=30 kg/m(2). The duration of breast-feeding was measured as the weeks of age from birth when breast-feeding ended. RESULTS: After adjusting for potential confounders, children whose mothers were obese before pregnancy were at a greater risk of becoming overweight [adjusted odds ratio (OR), 4.1; 95% confidence interval (CI), 2.6, 6.4] than children whose mothers had normal BMI (<25 kg/m(2); p < 0.001 for linear trend). Breast-feeding for >/=4 months was ass! ociated with a lower risk of childhood overweight (OR, 0.6; 95% CI, 0.4, 1.0; p = 0.06 for linear trend). The additive interaction between maternal prepregnancy obesity and lack of breast-feeding was detected (p < 0.05), such that children whose mothers were obese and who were never breast-fed had the greatest risk of becoming overweight (OR, 6.1; 95% CI, 2.9, 13.1). DISCUSSION: The combination of maternal prepregnancy obesity and lack of breast-feeding may be associated with a greater risk of childhood overweight. Special attention may be needed for children with obese mothers and lack of breast-feeding in developing childhood obesity intervention programs. Publication Type Journal Article. Research Support, N.I.H., Extramural. Research Support, Non-U.S. Gov't. Research Support, U.S. Gov't, P.H.S..
Result <139> Unique Identifier 15777435 Status MEDLINE Authors Kristensen J. Vestergaard M. Wisborg K. Kesmodel U. Secher NJ. Authors Full Name Kristensen, Janni. Vestergaard, Mogens. Wisborg, Kirsten. Kesmodel, Ulrik. Secher, Niels Jorgen. Institution Perinatal Epidemiological Research Unit, Department of Obstetrics and Gynaecology, Aarhus University Hospital, 8200 Aarhus N, Denmark. Title Pre-pregnancy weight and the risk of stillbirth and neonatal death. Source BJOG: An International Journal of Obstetrics & Gynaecology. 112(4):403-8, 2005 Apr. Abstract OBJECTIVE: To evaluate the association between maternal pre-pregnancy body mass index (BMI) and the risk of stillbirth and neonatal death and to study the causes of death among the children. DESIGN: Cohort study of pregnant women receiving routine antenatal care in Aarhus, Denmark. SETTING: Aarhus University Hospital, Denmark, 1989-1996. POPULATION: A total of 24,505 singleton pregnancies (112 stillbirths, 75 neonatal deaths) were included in the analyses. METHODS: Information on maternal pre- pregnancy weight, height, lifestyle factors and obstetric risk factors were obtained from self-administered questionnaires and hospital files. We classified the population according to pre-pregnancy BMI as underweight (BMI <18.5 kg/m(2)), normal weight (BMI 18.5-24.9 kg/m(2)), overweight (BMI 25-29.9 kg/m(2)) and obese (BMI 30.0 kg/m(2) or more). MAIN OUTCOME MEASURES: Stillbirth and neonatal death and causes of death. RESULTS: Maternal obesity was associated with a more than doubled ! risk of stillbirth (odds ratio = 2.8, 95% confidence interval [CI]: 1.5-5.3) and neonatal death (odds ratio = 2.6, 95% CI: 1.2-5.8) compared with women of normal weight. No statistically significantly increased risk of stillbirth or neonatal death was found among underweight or overweight women. Adjustment for maternal cigarette smoking, alcohol and caffeine intake, maternal age, height, parity, gender of the child, years of schooling, working status and cohabitation with partner did not change the conclusions, nor did exclusion of women with hypertensive disorders or diabetes mellitus. No single cause of death explained the higher mortality in children of obese women, but more stillbirths were caused by unexplained intrauterine death and fetoplacental dysfunction among obese women compared with normal weight women. CONCLUSION: Maternal obesity more than doubled the risk of stillbirth and neonatal death in our study. The present and other studies linking maternal obesity to! an increased risk of severe adverse pregnancy outcomes emphasise the need for public interventions to prevent obesity in young women. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <140> Unique Identifier 15761174 Status MEDLINE Authors Adams AK. Quinn RA. Prince RJ. Authors Full Name Adams, Alexandra K. Quinn, Rachel A. Prince, Ronald J. Institution Department of Family Medicine, University of Wisconsin Madison, 777 South Mills Street, Madison, WI 53715, USA. [email protected] Title Low recognition of childhood overweight and disease risk among Native-American caregivers. Source Obesity Research. 13(1):146-52, 2005 Jan. Abstract OBJECTIVES: Pediatric obesity is a significant and increasing problem in Native-American communities. The aim of this study was to determine whether parents and other caregivers from three Wisconsin tribes recognized overweight children. We also assessed caregiver attributes associated with levels of concern for risk of future overweight and chronic disease. RESEARCH METHODS AND PROCEDURES: Data were obtained from child health screenings and caregiver surveys. Participants included 366 kindergarten- through-second grade child-caregiver dyads. Children's BMI percentiles were calculated and compared with caregiver responses. We assessed the relationships between predictors of caregiver concern for health risk factors and recognition of overweight. RESULTS: Twenty-six percent of children were overweight (>or=95th percentile), and 19% were at risk for being overweight (>or=85th to <95th percentile) using Centers for Disease Control standards. Caregivers recognized only 15.1% of! overweight children. Factors predictive of child overweight recognition included a child BMI >99th percentile and grandmother as caregiver. Overall, caregivers were more concerned about diabetes and cardiovascular disease than obesity. Parents with diabetes and heart disease were more concerned than others about risk for these diseases; however, only diabetic parents made a connection between child weight status and future risk of obesity-related disease. Child sex, child age, and parental education level were not significant predictors for caregiver recognition of an overweight child. DISCUSSION: Most caregivers did not recognize overweight children or associate excess weight with increased risk of disease. When designing community interventions, it is crucial to incorporate caregivers' attitudes and beliefs regarding childhood overweight and risk of future disease. Publication Type Journal Article. Research Support, N.I.H., Extramural. Research Support, Non-U.S. Gov't. Research Support, U.S. Gov't, P.H.S..
Result <141> Unique Identifier 15557135 Status MEDLINE Authors Hancox RJ. Milne BJ. Poulton R. Taylor DR. Greene JM. McLachlan CR. Cowan JO. Flannery EM. Herbison GP. Sears MR. Authors Full Name Hancox, Robert J. Milne, Barry J. Poulton, Richie. Taylor, D Robin. Greene, Justina M. McLachlan, Christene R. Cowan, Jan O. Flannery, Erin M. Herbison, G Peter. Sears, Malcolm R. Institution Dunedin Multidisciplinary Health and Development Research Unit, Department of Preventive and Social Medicine, Dunedin School of Medicine, University of Otago, PO Box 913, Dunedin, New Zealand. [email protected] Title Sex differences in the relation between body mass index and asthma and atopy in a birth cohort. Source American Journal of Respiratory & Critical Care Medicine. 171(5):440-5, 2005 Mar 1. Abstract RATIONALE: Several studies have identified an association between asthma and obesity in women. It remains unclear if this association is due to genuine asthma or to symptoms caused by overweight, at what age the association develops, and whether it is confined to females. OBJECTIVE: To explore the relations between body mass index, asthma, and atopy in a birth cohort of approximately 1,000 individuals. METHODS: Information on asthma and measurements of lung function, airway responsiveness, and atopy were obtained on multiple occasions between ages 9 and 26. Associations between these outcomes and body mass index were analyzed using generalized mixed linear regression models. Further analyses adjusted for potential covariates including breastfeeding, birth order, parental asthma, and personal and family smoking history. MAIN RESULTS: Body mass index was positively associated with asthma, wheeze, asthma treatment, atopy, immunoglobulin E, and inversely with the FEV(1)/FVC ra! tio in females. There was no significant association with airway responsiveness to methacholine or salbutamol. There was little evidence of an association between body mass index and asthma or atopy in males. Analyses adjusting for potential covariates showed similar findings. Asthma was not associated with a raised body mass index in childhood and childhood asthma did not lead to being overweight as an adult. CONCLUSIONS: A raised body mass index is associated with asthma and atopy in women but not men. Population attributable fraction calculations estimate that 28% (95% confidence interval 7-45) of asthma developing in women after age 9 is due to overweight. Publication Type Journal Article. Research Support, Non-U.S. Gov't. Research Support, U.S. Gov't, P.H.S..
Result <142> Unique Identifier 15557134 Status MEDLINE Authors Varraso R. Siroux V. Maccario J. Pin I. Kauffmann F. Epidemiological Study on the Genetics and Environment of Asthma. Authors Full Name Varraso, Raphaelle. Siroux, Valerie. Maccario, Jean. Pin, Isabelle. Kauffmann, Francine. Epidemiological Study on the Genetics and Environment of Asthma. Institution INSERM U472, Epidemiology and Biostatistics, 16 avenue Paul Vaillant Couturier, 94807 Villejuif cedex, France. [email protected] Title Asthma severity is associated with body mass index and early menarche in women. Source American Journal of Respiratory & Critical Care Medicine. 171(4):334-9, 2005 Feb 15. Abstract Asthma severity in relation to body mass index (BMI) has rarely been studied. The relation between BMI and asthma severity was studied by sex in 366 adults with asthma from the Epidemiological Study on the Genetics and Environment of Asthma, a case- control and family study on asthma. Factors related to asthma severity and BMI such as smoking, FEV(1), bronchial hyperresponsiveness, and dyspnea were taken into account. The influence of early menarche was studied to assess the potential role of hormonal factors. Clinical asthma severity in the last 12 months was assessed by a score (0-7) based on the frequency of asthma attacks, persisting symptoms between attacks, and hospitalization. Asthma severity, which was unrelated to sex, increased with BMI in women (p = 0.0001) but not in men (p = 0.3). In women, the association remained after adjustment for age, FEV(1), smoking habits, and BMI-adjusted dyspnea and taking into account familial dependence (p = 0.0001). The association! between BMI and severity was stronger in women with early menarche than in women without early menarche (p interaction = 0.02). Findings support the hypothesis of hormonal factors involved in the severity of asthma. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <143> Unique Identifier 15314630 Status MEDLINE Authors Burke V. Beilin LJ. Simmer K. Oddy WH. Blake KV. Doherty D. Kendall GE. Newnham JP. Landau LI. Stanley FJ. Authors Full Name Burke, V. Beilin, L J. Simmer, K. Oddy, W H. Blake, K V. Doherty, D. Kendall, G E. Newnham, J P. Landau, L I. Stanley, F J. Institution School of Medicine and Pharmacology, The University of Western Australia, Royal Perth Hospital and Western Australian Institute for Medical Research, Perth, Australia. [email protected] Title Predictors of body mass index and associations with cardiovascular risk factors in Australian children: a prospective cohort study. Source International Journal of Obesity. 29(1):15-23, 2005 Jan. Abstract OBJECTIVE: To examine predictors of body mass index (BMI) at the age of 8 y in a prospective study of Australian children. DESIGN: Longitudinal survey of a cohort of Australian children followed from the 16th week of gestation to 8 y. SUBJECTS: In total, 741 boys and 689 girls who attended the survey as 8 y olds. MEASUREMENTS: Weight and height, blood pressure measured by automated oscillometry, fasting blood lipids and glucose. Questionnaire assessment of activity and diet. RESULTS: Proportions of overweight including obesity in boys and girls were, respectively, 22 and 25% at 1 y, 14 and 14% at 3 y, 13 and 18% at 5 y and 15 and 20% at 8 y. At the age of 1, 3, 6 and 8 y, children with overweight including obesity showed significantly more adverse cardiovascular risk factors. Blood pressure (BP) was significantly higher by 2/3 mmHg (systolic/diastolic) at 1 y, 3/2 mmHg at 3 y, 4/2 mmHg at 5 y and 6/2 mmHg at 8 y; HDL was significantly lower (P=0.002) by 8% and triglyceride! s were significantly higher by 27% (P<0.001). In multivariate regression, BMI at the age of 8 y was significantly predicted positively by birth weight, mother's BMI and hours spent in watching television at the time of the survey of 6 y olds. Mothers being ex-smokers or non smokers and children being 'slightly active' and 'active' negatively predicted BMI in 8 y olds. In a subset of 298 children with information about fathers, paternal BMI was an additional independent predictor. Maternal or paternal overweight including obesity each independently increased risk of overweight including obesity at the age of 8 y three-fold. A food factor with consumption of cereals and breads as the major components derived from a Food Frequency Questionnaire in a subset of 340 children was also an independent negative predictor of BMI in multivariate models. CONCLUSION: The increasing rate of overweight including obesity, particularly in girls, is associated with an increase in cardiovascul! ar risk factors very early in life. Improvement of health-related beha viours within the family and a focus on promotion of activity in children should be priorities in achieving weight control. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <144> Unique Identifier 15841767 Status MEDLINE Authors Scaglioni S. Verduci E. Fiori L. Lammardo AM. Rossi S. Radaelli G. Riva E. Giovannini M. Authors Full Name Scaglioni, S. Verduci, E. Fiori, L. Lammardo, A M. Rossi, S. Radaelli, G. Riva, E. Giovannini, M. Institution Department of Paediatrics, San Paolo Hospital, University of Milan, Milan, Italy. [email protected] Title Body mass index rebound and overweight at 8 years of age in hyperphenylalaninaemic children. Source Acta Paediatrica. 93(12):1596-600, 2004 Dec. Abstract AIM: To evaluate whether the age at body mass index (BMI) rebound may be associated with overweight at age 8 y in hyperphenylalaninaemic (HPA) children. METHODS: A longitudinal observational study including 97 HPA children born 1984-1993 and detected by the National Neonatal Screening programme. Children were followed up at the same institution and evaluated for dietary intakes and anthropometrical parameters from diagnosis up to the age of 8 y. Outcome measure was overweight at age 8 y, defined according to the International Obesity Task Force. The age at BMI rebound, BMI before and at rebound were considered as potential determinants. Familial overweight, breastfeeding and macronutrients intake at age 1 y were considered as confounders. RESULTS: Mean (95% confidence interval [CI]) age at BMI rebound was 5.0 (4.7-5.3) y. At the age of 8 y, 24.7% (95% CI 16.3- 33.1%) of children was overweight. Children overweight at the age of 8 y exhibited earlier BMI rebound than non-ove! rweight children (mean difference [95% CI] -2.1 [-2.8 to - 1.4] y) and higher BMI from the age of 1 y (mean difference [95% CI] 1.2 [0.9-2.5] kg/ m2) onward. Overweight was more likely in children with, rather than without, parental overweight (41.0% vs 19.8%). After adjustment for confounders, logistic analysis showed that earlier BMI rebound (odds ratio [OR] 2.4, 95% CI 1.2-4.8) and BMI at age I y (OR 2.3, 95%CI 1.1-4.98) were independently associated with overweight at the age of 8 y. CONCLUSION: Within the population of this study, overweight at age 8 y was positively associated with early BMI rebound and BMI at age 1 y. Publication Type Journal Article.
Result <145> Unique Identifier 11886935 Status MEDLINE Authors He Q. Karlberg J. Authors Full Name He, Qing. Karlberg, Johan. Institution Department of Pediatrics, The University of Hong Kong, Hong Kong SAR, P.R. China. Title Probability of adult overweight and risk change during the BMI rebound period. Source Obesity Research. 10(3):135-40, 2002 Mar. Abstract OBJECTIVE: To develop a probability chart of adult overweight based on childhood body mass index (BMI) values and to evaluate the BMI change during the BMI rebound period during childhood, in different populations, with the use of risk function curves. RESEARCH METHODS AND PROCEDURES: A longitudinal growth study of 3650 full-term healthy Swedish children followed from birth to 18 years of age. Weight and height values of our subjects were obtained. RESULTS: A probability chart for reaching a BMI > 23 kg/m(2) at 18 years of age was constructed for boys and girls. For example, a BMI of 18 kg/m(2) at 4 years of age is associated with 0.70 probability of attaining a BMI > 23 kg/m(2) at 18 years of age in boys; a BMI of 16 kg/m(2) at 4 years of age leads to 0.40 probability of having a BMI > 23 kg/m(2) at 18 years of age in girls. Children with an obvious BMI rebound before 8 years of age have a high risk of being overweight at 18 years of age. There is a clear trend of BMI inc! rease from the 1970s to the 1990s in U.S. children from a parallel dataset, and Hispanic children are at the highest risk of adult overweight. DISCUSSION: The probability chart for adult overweight developed here provides a functional method of defining childhood obesity that is based on the risk of long-term ill health rather than on a certain statistical cut-off point. It will help pediatricians or healthcare workers identify those children who are at a high risk of becoming overweight in adulthood, which will allow clinical intervention at younger ages. Publication Type Journal Article. Research Support, Non-U.S. Gov't.
Result <146> Unique Identifier 11319660 Status MEDLINE Authors Freedman DS. Kettel Khan L. Serdula MK. Srinivasan SR. Berenson GS. Authors Full Name Freedman, D S. Kettel Khan, L. Serdula, M K. Srinivasan, S R. Berenson, G S. Institution Division of Nutrition and Physical Activity, Centers for Disease Control and Prevention, Atlanta, Georgia, USA. [email protected] Title BMI rebound, childhood height and obesity among adults: the Bogalusa Heart Study. Source International Journal of Obesity & Related Metabolic Disorders: Journal of the International Association for the Study of Obesity. 25(4):543-9, 2001 Apr. Abstract OBJECTIVE: The beginning of the post-infancy rise in the body mass index (BMI, kg/m2) has been termed the adiposity rebound, and several studies have found that an early rebound increases the risk for overweight in adulthood. We examined whether this relation is independent of childhood BMI levels. DESIGN: A longitudinal study of 105 subjects who examined at ages 5, 6, 7, 8 and 19-23 y. RESULTS: Subjects with an age at the BMI rebound (age(min)) of < or =5 y were, on average, 4-5 kg/m2 heavier in early adulthood than were subjects whose age(min) was > or =7 y. Age(min), however, was also correlated with childhood BMI levels (r approximately -0.5), and we found that age(min) provided no additional information on adult overweight if the BMI level at age 7 y (or 8 y) was known. In contrast, childhood height, which was also correlated with age(min) (r=-0.47), was independently related to adult BMI. Among relatively heavy (BMI=16.0 kg/m2) 5-y-olds, a child with a height of 120 ! cm was estimated to be 1.2 kg/m2 heavier in adulthood than would a 104 cm tall child. CONCLUSIONS: Although an early BMI rebound was related to higher levels of relative weight in adulthood, this association was not independent of childhood BMI levels. The relation of childhood height to adult BMI needs to confirmed in other cohorts, but it is possible that childhood height may help identify children who are likely to become overweight adults. Publication Type Journal Article. Research Support, Non-U.S. Gov't. Research Support, U.S. Gov't, P.H.S..
Result <147> Unique Identifier 11126216 Status MEDLINE Authors Guo SS. Huang C. Maynard LM. Demerath E. Towne B. Chumlea WC. Siervogel RM. Authors Full Name Guo, S S. Huang, C. Maynard, L M. Demerath, E. Towne, B. Chumlea, W C. Siervogel, R M. Institution Department of Community Health, Wright State University School of Medicine, Dayton, OH 45435, USA. [email protected] Title Body mass index during childhood, adolescence and young adulthood in relation to adult overweight and adiposity: the Fels Longitudinal Study. Source International Journal of Obesity & Related Metabolic Disorders: Journal of the International Association for the Study of Obesity. 24(12):1628-35, 2000 Dec. Abstract BACKGROUND: Childhood overweight develops during 'critical periods', but the relationship of body mass index (BMI) patterns during 'critical periods' from childhood into adulthood with subsequent overweight and adiposity has not been previously investigated. BMI patterns during early childhood, pubescence and post-pubescence and their independent effects on overweight and body fatness at 35-45 y of age were examined along with birth weight and the effects of adult lifestyle factors. METHODS: BMI parameters describing the timing, velocity minimum (min) and maximum (max) values from 2 to 25 y of age were related to adulthood BMI values and total and percentage body fat (TBF, %BF) at 35-45 y. These data were from 180 males and 158 females in the Fels Longitudinal Study. RESULTS: There was no sex difference in the timing of BMI rebound, but the age of BMI maximum velocity and maximum BMI were both earlier in girls. Children with an earlier BMI rebound had larger BMI values at ! rebound and at maximum velocity. Children who reached maximum BMI at later age had larger maximum BMI values. Maximum BMI was a strong predictor for adult BMI and in females, a strong predictor of adulthood TBF and %BF. Maximum BMI was closely related to maximum BMI velocity in females and in males, BMI at maximum velocity is a strong predictor of TBF and %BF. CONCLUSIONS: Changes in childhood BMI were related to adult overweight and adiposity more so in females than males. BMI rebound is a significant important period related to overweight at 35-45 y in females but not in males. However BMI patterns during and post-adolescence were more important than the BMI rebound for adulthood TBF and %BF status. There is marked tracking in BMI from approximately 20 y into 35-45 y. The pattern of BMI changes from 2 to 25 y had stronger effects on subsequent adult overweight than birth weight and adult lifestyle variables. Publication Type Journal Article.