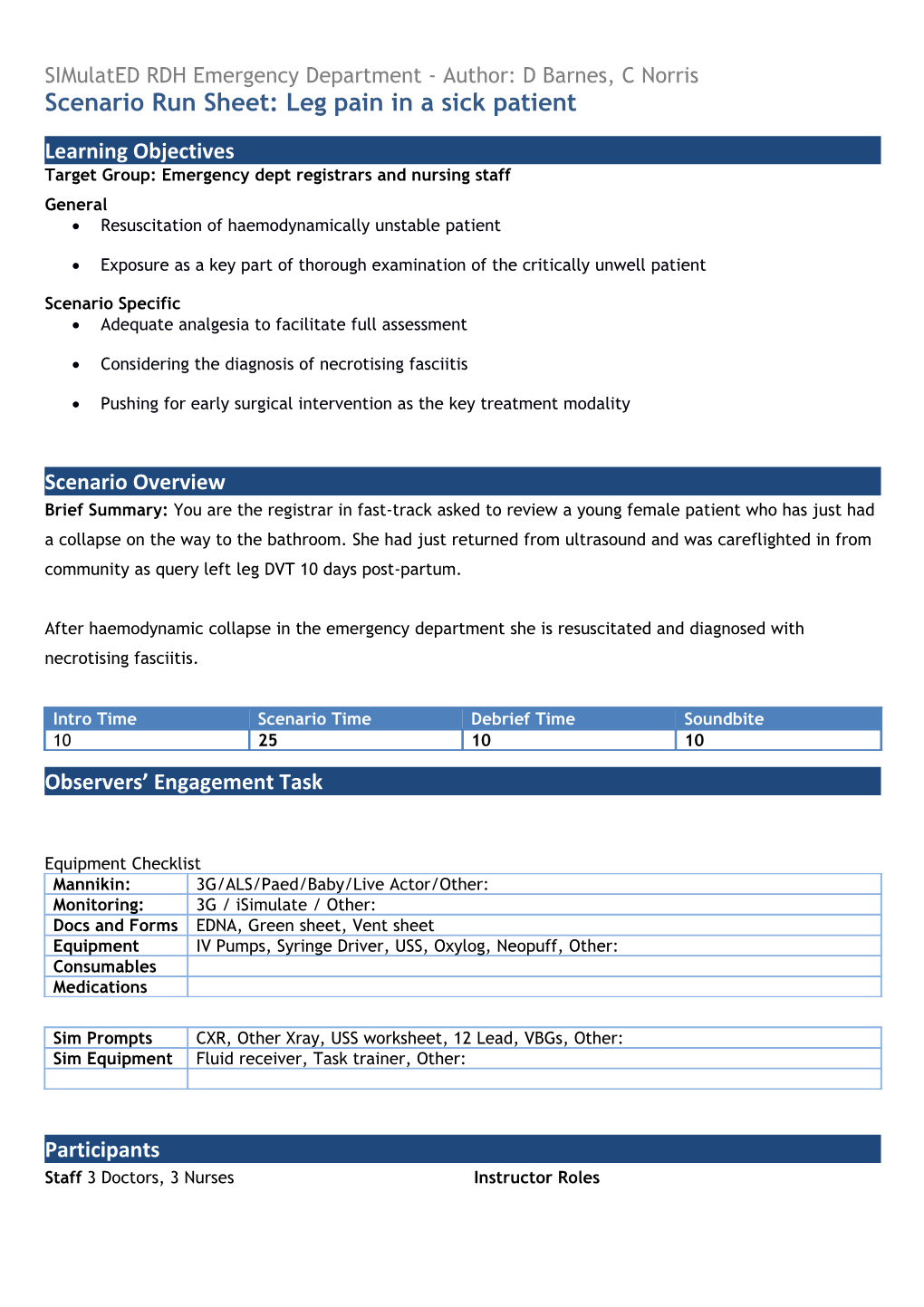
SIMulatED RDH Emergency Department - Author: D Barnes, C Norris Scenario Run Sheet: Leg pain in a sick patient
Learning Objectives Target Group: Emergency dept registrars and nursing staff General Resuscitation of haemodynamically unstable patient
Exposure as a key part of thorough examination of the critically unwell patient
Scenario Specific Adequate analgesia to facilitate full assessment
Considering the diagnosis of necrotising fasciitis
Pushing for early surgical intervention as the key treatment modality
Scenario Overview Brief Summary: You are the registrar in fast-track asked to review a young female patient who has just had a collapse on the way to the bathroom. She had just returned from ultrasound and was careflighted in from community as query left leg DVT 10 days post-partum.
After haemodynamic collapse in the emergency department she is resuscitated and diagnosed with necrotising fasciitis.
Intro Time Scenario Time Debrief Time Soundbite 10 25 10 10 Observers’ Engagement Task
Equipment Checklist Mannikin: 3G/ALS/Paed/Baby/Live Actor/Other: Monitoring: 3G / iSimulate / Other: Docs and Forms EDNA, Green sheet, Vent sheet Equipment IV Pumps, Syringe Driver, USS, Oxylog, Neopuff, Other: Consumables Medications
Sim Prompts CXR, Other Xray, USS worksheet, 12 Lead, VBGs, Other: Sim Equipment Fluid receiver, Task trainer, Other:
Participants Staff 3 Doctors, 3 Nurses Instructor Roles Additional Information/Medical History Demographics 21 year old woman HPC “Sorry to cause a fuss, just the pain in my leg really got to me when I stood up, could I have something for the pain?”
Had a presyncopal event at home 2 days ago in the shower and banged her knee (no LOC, no head injury or actual collapse, no other red flags)
Early hours of the morning yesterday her knee pain was getting worse and she was seen at her community health clinic (CHC)
Delivered at her district hospital 10 days ago, uncomplicated vaginal delivery (no PROM / no fever / no Abx / GBS neg) with a first degree tear, discharged next day with simple analgesia
Denies fevers, no change to lochia or PV discharge, no abdominal pain, no dysuria / haematuria
No dyspnoea, no palpitations, no chest pain, no cough / haemoptysis
Swollen tender calf with a positive Homen’s sign (increased pain on ankle dorsiflexion), external exam of genitalia wound appeared healed, sutures removed, given a stat dose of clexane and transferred to Darwin for further investigation
If asked – observations at the CHC tachycardia 110 and tachypnoea 30 that settled with analgesia with normal saturations and afebrile
PMH Previously well, 1 week post partum, NKDA, Nil reg meds – has been taking Panadol and neurofen for perineal discomfort Exam Flushed uncomfortable 21 year old female dressed in t-shirt and light trackpants, no IV access drip removed on arrival as tissued and uncomfortable
A - patent own
B – chest is clear, obs below
C – obs below, warm peripherally with strong pulses
D – alert and oriented though in pain
E – soft abdo, left leg swollen, erythematous exquisitely tender skin over calf, no visible knee wounds or abrasions, pain on ranging the knee joint but no clinical effusion, tender beyond erythema distally
Only if adequately exposed – region of indurated tender skin extending down from proximal medial thigh with blisters at junction with perineum; perineal wound slightly swollen and also tender but no frank pus or dehiscence
Investigations Worksheet from the Ultrasound shows all the deep veins to the iliacs to be patent
CXR clear, ECG sinus tachycardia
Bloods taken at CHC were sent to the lab on arrival they show 1. Hb 110, platelets 90
2. White cells of 5 neutrophils of 4 and lymphocytes of 0.4
3. Na 137, K 4.2, Cl 104, Ur 9, Cr 110
4. Bili 26, AST 200, ALP 100, GGT 120, Alb 30
5. CRP 360
VBG machine is initially calibrating when back it shows
6. pH 7.1
7. CO2 30
8. HCO3 10, BE 10
9. Na 134, K 5.0, Ca 1.1
10. Cr 200
11. lactate 8 Proposed Scenario Progression
1. Flushed uncomfortable 21 year old female dressed in t-shirt and light trackpants, 30deg head up in a bed in fast track. Receives opiate for leg pain states she feels unwell, becomes drowsy diaphoretic and vomits
2. Septic shower after morphine, hypotensive, drowsy, diaphoretic and vomits, moved to resus, rest of team arrives, unresponsive to 2L fluid, combative and difficult to assess due to pain
3. Consideration of differential diagnosis – with increasing information diagnostic progression towards necrotising fasciitis and involvement of surgeons
4. If scenario progressing rapidly/senior team then surgeon obstructive and states “its vagina cellulitis and needs to go to O&G”. Requires graded assertiveness and ultimately for ED doctor to call surgical consultant or ED Consultant.
Scenario Preparation/Baseline Parameters Stage 1 Progression Stage 2 Progression Stage 3 RR 25 40 Trigger Trigger SpO2 98% 94% HR/Rhythm 110 IV 130 Start BP 110/60 Morphine, 90/50 vasopressors T 36.8 37.4 Other BSL 9 vomit
Debriefing/Guided Reflection Overview Opening Gambit Anticipated themes: What was going on in this scenario
Exploration with key players No fever – why wasn’t this PE
Engaging the general group How can you tell the difference between obstructive Could this lady have had a PE too? shock from PE and septic shock at the bedside (clinical exam/Echo features of both) Sharing facilitator’s thoughts Around diagnostic biases and early closure – “this thing fits so I’m not investigating any other avenues”
Any other questions or issues to discuss? Bedside scalpel test – dishwater exudate
Summary Needs surg – near 100% mortality with NF without it
The Soundbite Neck fash – Not just a trendy abbreviation for scarves, pashminas and neck warmers
Necrotising fasciitis – a rapidly progressive infection of the deep fascial planes that divide tissue compartments (typically muscle with the fat and skin above them) with a mortality as high as 50%
2 main subtypes (but some separate into 4)
1. Many bugs – at least one anaerobe with aerobes
2. One bug – Group A strep (that is Strep Pyogenes)
Rates have been described as low as 0.4 cases per 100,000 people / year
There are ~150,000 people in the NT
latest data - 95 cases at RDH either local or transferred from 2005-2013 (which is 7 per 100,000 per year, and does not include people that never made it to transfer or hospital)
Risk Factors Have a high index of suspicion – as in this case Group A strep NF can kill young healthy people with no comorbidities.
Comorbid disease
12. Diabetes 40-60% prevalence
13. Organ failure - Cirrhosis, Heart failure, Renal failure
14. Underlying malignancy
15. Hypertension, peripheral vascular disease
Immunosuppression – drugs, old age, pregnancy
Lifestyle factors – obesity, IVDU, Alcohol abuse
NSAID use – debate about whether there is a causative role of the anti-inflammatory effect of NSAIDs in changing disease versus pain relief simply delaying diagnosis
Raw seafood (for vibrio / aeromonas infections in a Southeast Asian study)
Clinical presentation
Diagnosis Notoriously challenging – in one review article covering 9 trials with ~1500 patients 75% of patients were misdiagnosed initially
LRINEC is a scoring system that uses Lab values to examine risk of NF o Depending on where the score was used it was variably good or crap
o The surgical department here has done a retrospective case control validation here reporting sensitivity of 76% and specificity of 93%
o The key take home is that there are cases of NF with LRINEC score of 0
Laboratory features
o White cells either high, or low
o Thrombocytopaenia
o Impaired renal function (Cr >200)
o Impaired coagulation
o Impaired liver enzymes
o Elevated CRP
o Elevated CK (low >6-700)
Note that in a case series of 14 patients with GAS NF from Darwin there were some atypical features noted
16. Erythema was less common but pain and swelling were still present
17. No patients had elevated white cells, but all had lymphopaenia
18. CRP was >100 in all that had it measured (up to 500)
19. 80% had renal impairment, and all had hypoalbuminaemia
Treatment Never let the sun set on pus; Heal with steel; Never let the skin stand between you and the diagnosis
Antibiotics – depends on the bug but for GAS beta-lactam plus clindamycin
Consider: hyperbaric oxygen and IVIG General Feedback Prompts/Examples:
Opening Gambit: What did you feel were your specific challenges there?
Let’s talk.
Can you describe to me what was happening to the patient during that scenario?
Can you describe to me what was going on?
What was important to you in choosing to manage that situation?
Can you tell me what your plan was and to what extent that went according to plan?
That seemed to me to go smoothly, what was your impression?
That looked pretty tough. Shall we see if we can work out together what was going on there so that you can find a way to avoid that situation in the future?
Exploration with key players Questions to deepen thinking
Questions to widen conversation
Introduce new concepts; challenge perceptions; listen and build
So what you’re saying is…
Can you expand on…
Can you explain what you meant by…
When you said…
I noticed that you…
Engaging the general group Let’s check with the rest of the group how they reacted to you saying that.
Did you [scenario participants/observers] feel the same?
What did you [scenario participants/observers] want from [scenario participant] at that point?
What ideas or suggestions has anyone else got for how to deal with that situation?
Sharing facilitator’s thoughts Use advocacy with inquiry to share your observations and explore their perception
What does the protocol say on…..
What do you think was happening ….?
How do you think … would respond to…. ? What about next time…..?
Do you think there’s anything to be gained from…?
Any other questions or issues to discuss?
Summary