Thyroid Ophthalmopathy
Most common cause of unilateral and bilateral proptosis in adults. Approximately 40 percent of patients with Graves disease have or will develop signs of thyroid-related orbitopathy.
Pathophysiology Autoimmune-mediated inflammation of the extraocular muscle and periorbital connective tissue Early inflammatory infiltrate of the extraocular muscles, connective tissues, and lacrimal gland is later replaced by fibrosis. Not clear if this is a cell-mediated or a humoral immune response Inflammation of the orbital soft tissues and extraocular muscles is thought to be regulated by thyroid-stimulating hormone (TSH) receptor protein (CD40), which may be expressed on orbital fibroblasts causing chemotaxis of inflammatory cells in the orbit. Lymphocytic infiltration of the orbital tissue causes a release of cytokines which act primarily on fibroblasts. Fibroblasts secrete hyaluronic acid. Doubling the hyaluronic acid content in orbital tissue causes a 5-fold increase in the tissue osmotic load. The osmotic damage results in muscle edema, leading to proptosis, subsequent fibrosis of muscle fibers, and eventually tissue atrophy.
Clinical
Graves’ disease consists of hyperthyroidism associated with goiter, pretibial dermopathy, and infiltrative ophthalmopathy. natural course of Graves’ ophthalmopathy is usually self-limiting but may not correspond directly with the patient’s thyroid status. most common finding is eyelid retraction, although the spectrum of findings is wide, ranging from subtle lid lag to disabling diplopia, severe exposure keratopathy, and potentially blinding optic neuropathy. Upper lid retraction (Dalrymple sign) due to 1. Proptosis 2. sympathetic drive of the Müller muscle 3. fibrosis of inferior rectus, leading to overaction of superior rectus and levator 4. contralateral ptosis (myasthenia). Lid lag on downgaze (von Graefe sign) Pseudoptosis – due to contralateral lid retraction is present. Ptosis - levator dehiscence or concurrent myasthenia Chemosis periorbital edema Altered ocular motility Strabismus common with extraocular muscle involvement deep glabellar rhytides caused by hypertrophy of brow depressor muscles compensating for lid retraction. Optic neuropathy - nerve constriction due to “cone” of inflamed muscles Compressive optic neuropathy is the most common cause of irreversible visual loss secondary to thyroid-related orbitopathy. Compressive optic neuropathy, which is characterized by painless, gradual loss of visual function, is best assessed by pupillary abnormalities (afferent pupillary defect in the presence of asymmetric disease), diminished color vision, and visual field defects; in some patients, central vision may not be affected.
Investigations Blood o TFTs, Antithyroid peroxidase antibody US o may show thickened muscles CT/MRI: o thickened muscles – usually medial and inferior rectus. o dilated superior ophthalmic vein. Histologic Findings: o Lymphocytic cell infiltration o Enlargement of fibroblasts o Accumulation of mucopolysaccharides o Interstitial edema o Increased collagen production
Treatment Regulation of thyroid function does not abort eye involvement. Usually runs a self-limited but prolonged course over 1 or more years. Patients also should realize that no immediate cure is available. Thyroid ablation with orally ingested radioactive iodine (RAI; I-131) may exacerbate the eye disease compared to antithyroid drugs or surgical ablation.
Symptomatic Treat dry eyes Monitor for exposure Sleep head up to reduce oedema
Medical Oral steroids - reserved for patients with severe inflammation or compressive optic neuropathy. Steroids may decrease the production of mucopolysaccharides by the fibroblasts. Effective in temporary preservation of vision. Pentoxifylline and nicotinamide may be useful. Both agents are believed to inhibit cytokine-induced glycosaminoglycan synthesis by the retroorbital fibroblasts. plasmapheresis and intravenous immunoglobulin Orbital radiation – for moderate-to-severe inflammatory symptoms, diplopia, and visual loss, and in cases in which steroid therapy is contraindicated or ineffective o Low dose - 1500-2000 cGy fractionated over 10 d o believed to damage orbital fibroblasts or perhaps lymphocyte o risks: Cataract, radiation retinopathy, and radiation optic neuropathy
Surgery Surgical intervention is not recommended during the inflammatory stage. Stability of the disease should be documented for at least 6 months before any operative correction is undertaken.
Surgical options
Lid camouflage techniques 1. Lid lengthening surgery (for mild cases) Upper lid retraction lengthening of levator aponeurosis or division of Mullers muscles (mild 2-3mm lid retraction) decreases corneal exposure and can be used to camouflage mild-to- moderate proptosis. Most common complication - high eyelid crease eyelid retraction may develop in the contralateral lid (Herings Law) Lower lid lengthening usually requires a spacer material, need 4x wider than the amount of scleral show. Graft materials include human acellular dermis, tarsus, and conjunctiva from the upper lid, hard palate, and ear cartilage. Recurrence of retraction common, reduced by tarsorraphy and lateral strip
2. Lateral tarsorrhaphy – alternative for lid retraction. Note that horizontal tightening procedures (ie lateral strip) will increase scleral show, better to combine them.
Decompression
Indications 1. a sight-threatening compressive optic neuropathy unresponsive to immunosuppressive therapy 2. proptosis causing severe ocular surface disease 3. cosmetic appearance unlikely to be improved by lid surgery alone Anterior decompressions are effective in reducing proptosis. In compressive optic neuropathy, however, decompression along the posterior medial wall is necessary to address apical optic nerve compression
1. Orbital fat decompresion indicated for predominant enlargement of the orbital fat compartment, rather than the rectus muscles on orbital imaging Unlike cosmetic blepharoplasty, fat is also removed posterior to the equator of the globe Combined transconjuctival and blepharoplasty incisions 2. Expansion osteotomy (originally advocated by Tessier) 3. Orbital decompression- initial treatment of compressive optic neuropath or after failed medical treatment Incisions: a. Transorbital i. subciliary incisions ii. lid crease incisions (blepharoplasty) iii. transconjuctival - provides excellent visualization of the orbital floor and medial wall. Visualization of the most posterior portion of the medial wall, which must be adequately removed for treatment of compressive optic neuropathy, may be suboptimal in this approach iv. transcaruncular v. Lynch incision b. Transcranial coronal incisions. c. transantral – sublabial incision d. endonasal - allows the removal of the orbital floor and medial wall, especially at the orbital apex. Visualization of the medial orbital wall is superior to other approaches, permitting more complete medial posterior orbital wall decompression. Access to the anterior orbital floor is limited. e. Osteotomies o At least 2 orbital walls usually are decompressed o Most commonly the medial wall and floor of the orbit via transantral approach . Sublabial incision . excellent visualization of the floor and inferior portion of the medial wall. . visualization of the orbital apex, posterior ethmoids, and lateral wall of the sphenoid sinus is difficult. o Other options: a. Lateral orbital wall - Lateral wall decompression does not adequately address the medial wall of the orbit, which is required for treatment of compressive optic neuropathy. b. Orbital floor c. Lateral wall + lateral part of floor (Matton) d. Medial and lateral walls (balanced decompression – avoids diplopia) e. Orbital roof - transfrontal decompression has significant risk of cerebrospinal fluid leakage, meningitis, and transmission of cerebral pulsations to the eyes. f. Medial wall + partial floor + partial lateral wall + fat (Roncevic and Jackson) g. 3-wall resection 4. 4-wall resection (combined neurosurgery)
Adjunctive surgeries 1. Strabismus surgery - goal of surgery is to minimize diplopia in primary and reading positions 2. Blepharoplasty Usually last operation required. Conservative skin excisions only. Set fold lower (ie 6-7mm)
Medial wall removal should not extend above the frontoethmoidal suture. This averts bleeding from the ethmoidal arteries and prevents cerebrospinal fluid (CSF) leaks. When the orbital floor is removed, preservation of a strut of bone between the ethmoid and maxillary bones may reduce strabismus from inferomedial shift in the globe position. Lateral wall decompression does little to relieve apical compression but helps to reproduce proptosis.
Complications of orbital decompression include blindness, hemorrhage, diplopia, periorbital numbness, globe malposition, sinusitis, lid malposition.
Transcaruncular approach (PRS Sept 2003)
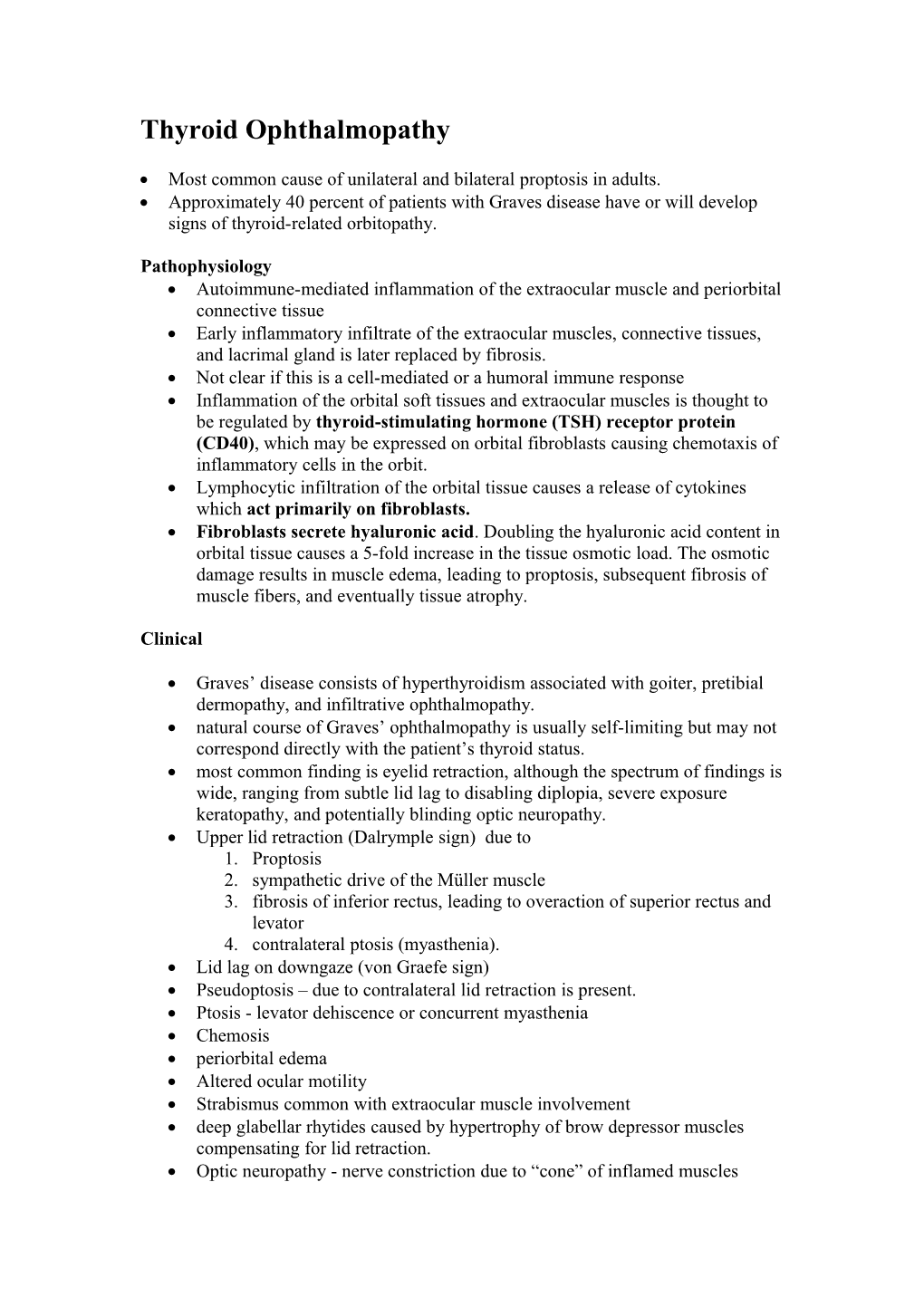
(Above, left) Caruncle and medial conjunctiva exposed. Silk traction sutures are placed through the tarsus of the upper and lower eyelids just lateral to the puncta. The dotted black line indicates incision site. (Above, right) Medial incision made at the junction of the posterior one third and anterior two thirds of caruncle. (Below, left) Blunt dissection with tips of scissors placed firmly against the posterior edge of the posterior lacrimal crest, revealing the plane of dissection. (Below, right) Exposure of the medial wall of the orbit with malleable retractor protecting the globe. Orbital retractor used to retract herniated orbital fat.
Incision at the junction of the posterior one third and anterior two thirds of the caruncle allows passage along a natural plane between the Horner muscle and the medial orbital septum. Horner muscle buffers this safe and bloodless plane from the lacrimal sac.
Because dissection is carried out posterior to the lacrimal system, the canthal tendon attachments are left intact.
The plica semilunaris should not be confused with the caruncle as this will result in too deep a dissection plane with possible damage to the medial rectus muscle and poor visualization secondary to herniation of orbital fat
Under direct visualization, the medial wall of the orbit was infractured with a periosteal elevator and removed with bayonet forceps. Ethmoid air cells were removed in a graded fashion using endoscopic instruments.
Care was taken to limit dissection inferior to the level of the anterior and posterior ethmoidal foramina (frontal-ethmoidal suture) to avoid violating the intracranial space and creating the potential for cerebrospinal fluid leaks.
Photograph of orbit from adult human skull depicting bony landmarks. The dashed line marks the posterior lacrimal crest. The asterisks mark the anterior and posterior ethmoidal foramina. The dotted line below the asterisks shows the frontoethmoidal suture, which serves as landmark for the level of the cribriform plate. The ribbon- shaped area shows the position of the inferomedial orbital strut at the maxilloethmoidal junction. The floor of orbit medial to infraorbital neurovascular junction is retroilluminated, demonstrating the thinnest portion of the floor of the orbit approximately 1.5 cm posterior to the orbital rim.