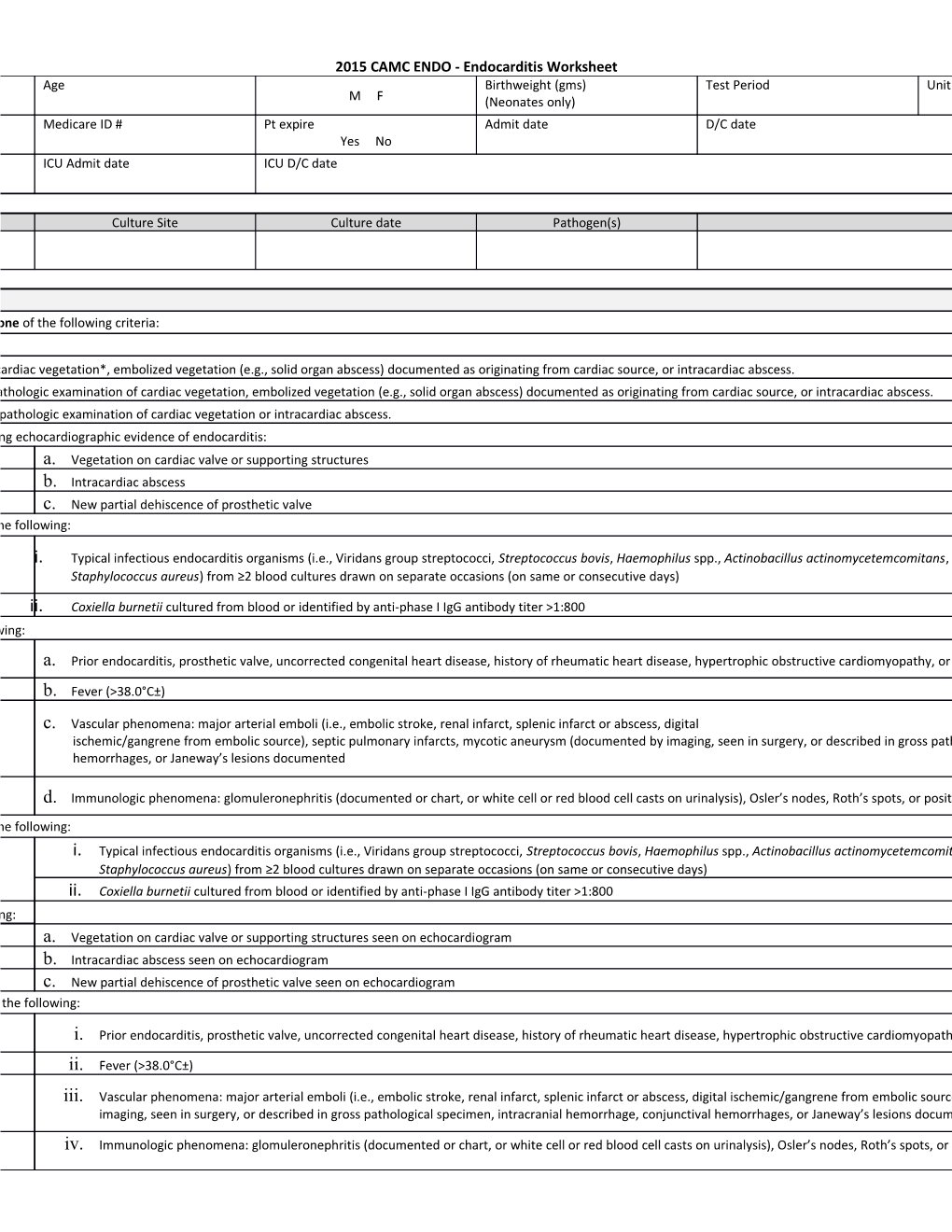
2015 CAMC ENDO - Endocarditis Worksheet Age Birthweight (gms) Test Period Unit M F (Neonates only) Medicare ID # Pt expire Admit date D/C date Yes No ICU Admit date ICU D/C date
Culture Site Culture date Pathogen(s)
at least one of the following criteria:
Organisms cultured from cardiac vegetation*, embolized vegetation (e.g., solid organ abscess) documented as originating from cardiac source, or intracardiac abscess. Organisms seen on histopathologic examination of cardiac vegetation, embolized vegetation (e.g., solid organ abscess) documented as originating from cardiac source, or intracardiac abscess. Endocarditis seen on histopathologic examination of cardiac vegetation or intracardiac abscess. of the following echocardiographic evidence of endocarditis: a. Vegetation on cardiac valve or supporting structures b. Intracardiac abscess c. New partial dehiscence of prosthetic valve of the following:
i. Typical infectious endocarditis organisms (i.e., Viridans group streptococci, Streptococcus bovis, Haemophilus spp., Actinobacillus actinomycetemcomitans, Cardiobacterium hominis Staphylococcus aureus) from ≥2 blood cultures drawn on separate occasions (on same or consecutive days)
ii. Coxiella burnetii cultured from blood or identified by anti-phase I IgG antibody titer >1:800 of the following:
a. Prior endocarditis, prosthetic valve, uncorrected congenital heart disease, history of rheumatic heart disease, hypertrophic obstructive cardiomyopathy, or known IV drug use
b. Fever (>38.0°C±)
c. Vascular phenomena: major arterial emboli (i.e., embolic stroke, renal infarct, splenic infarct or abscess, digital ischemic/gangrene from embolic source), septic pulmonary infarcts, mycotic aneurysm (documented by imaging, seen in surgery, or described in gross pathological specimen, intracranial hemorrhage, conjunctival hemorrhages, or Janeway’s lesions documented
d. Immunologic phenomena: glomuleronephritis (documented or chart, or white cell or red blood cell casts on urinalysis), Osler’s nodes, Roth’s spots, or positive rheumatoid factor. of the following: i. Typical infectious endocarditis organisms (i.e., Viridans group streptococci, Streptococcus bovis, Haemophilus spp., Actinobacillus actinomycetemcomitans Staphylococcus aureus) from ≥2 blood cultures drawn on separate occasions (on same or consecutive days) ii. Coxiella burnetii cultured from blood or identified by anti-phase I IgG antibody titer >1:800 of the following: a. Vegetation on cardiac valve or supporting structures seen on echocardiogram b. Intracardiac abscess seen on echocardiogram c. New partial dehiscence of prosthetic valve seen on echocardiogram of the following:
i. Prior endocarditis, prosthetic valve, uncorrected congenital heart disease, history of rheumatic heart disease, hypertrophic obstructive cardiomyopathy, or known IV drug use
ii. Fever (>38.0°C±)
iii. Vascular phenomena: major arterial emboli (i.e., embolic stroke, renal infarct, splenic infarct or abscess, digital ischemic/gangrene from embolic source), septic pulmonary infarcts, mycotic aneurysm (documented by imaging, seen in surgery, or described in gross pathological specimen, intracranial hemorrhage, conjunctival hemorrhages, or Janeway’s lesions documented
iv. Immunologic phenomena: glomuleronephritis (documented or chart, or white cell or red blood cell casts on urinalysis), Osler’s nodes, Roth’s spots, or positive rheumatoid factor. 2015 CAMC ENDO - Endocarditis Worksheet v. Identification of an organism from the blood by at least one of the following methods: Recognized pathogen cultured from one or more blood cultures, Same common commensal organism cultured from ≥2 blood cultures drawn on separate occasions (on same or consecutive days), or Organism identified by non-culture diagnostic test from blood (e.g., serology, PCR) All of the following criteria:
a. Prior endocarditis, prosthetic valve, uncorrected congenital heart disease, history of rheumatic heart disease, hypertrophic obstructive cardiomyopathy, or known IV drug use
b. Fever (>38.0°C±) c. Vascular phenomena: major arterial emboli (i.e., embolic stroke, renal infarct, splenic infarct or abscess, digital ischemic/gangrene from embolic source), septic pulmonary infarcts, mycotic aneurysm (documented by imaging, seen in surgery, or described in gross pathological specimen, intracranial hemorrhage, conjunctival hemorrhages, or Janeway’s lesions documented
d. Immunologic phenomena: glomuleronephritis (documented or chart, or white cell or red blood cell casts on urinalysis), Osler’s nodes, Roth’s spots, or positive rheumatoid factor.
e. Identification of an organism from the blood by at least one of the following methods: recognized pathogen cultured from one or more blood cultures, same common commensal organism cultured from ≥2 blood cultures drawn on separate occasions (on same or consecutive days), or organism identified by non-culture diagnostic test from blood (e.g., serology, PCR)
Cardiac vegetation” includes vegetation on a pacemaker/ defibrillator lead. 2015 CAMC ENDO - Endocarditis Worksheet Table of Events I n f e c t i D o at H n e os W U D of pit i RI n at E al n T i e v Da d t e y o n w t
P e r i o d 2015 CAMC ENDO - Endocarditis Worksheet
Infection Window Period (first + diagnostic test, 3 days before & 3 days after) Repeat Infection Timeframe-RIT (14 day timeframe where date of event = day 1) Date of Event (date the first element occurs for the first time within the infection window period) Secondary BSI Attribution Period (Infection Window Period + RIT)