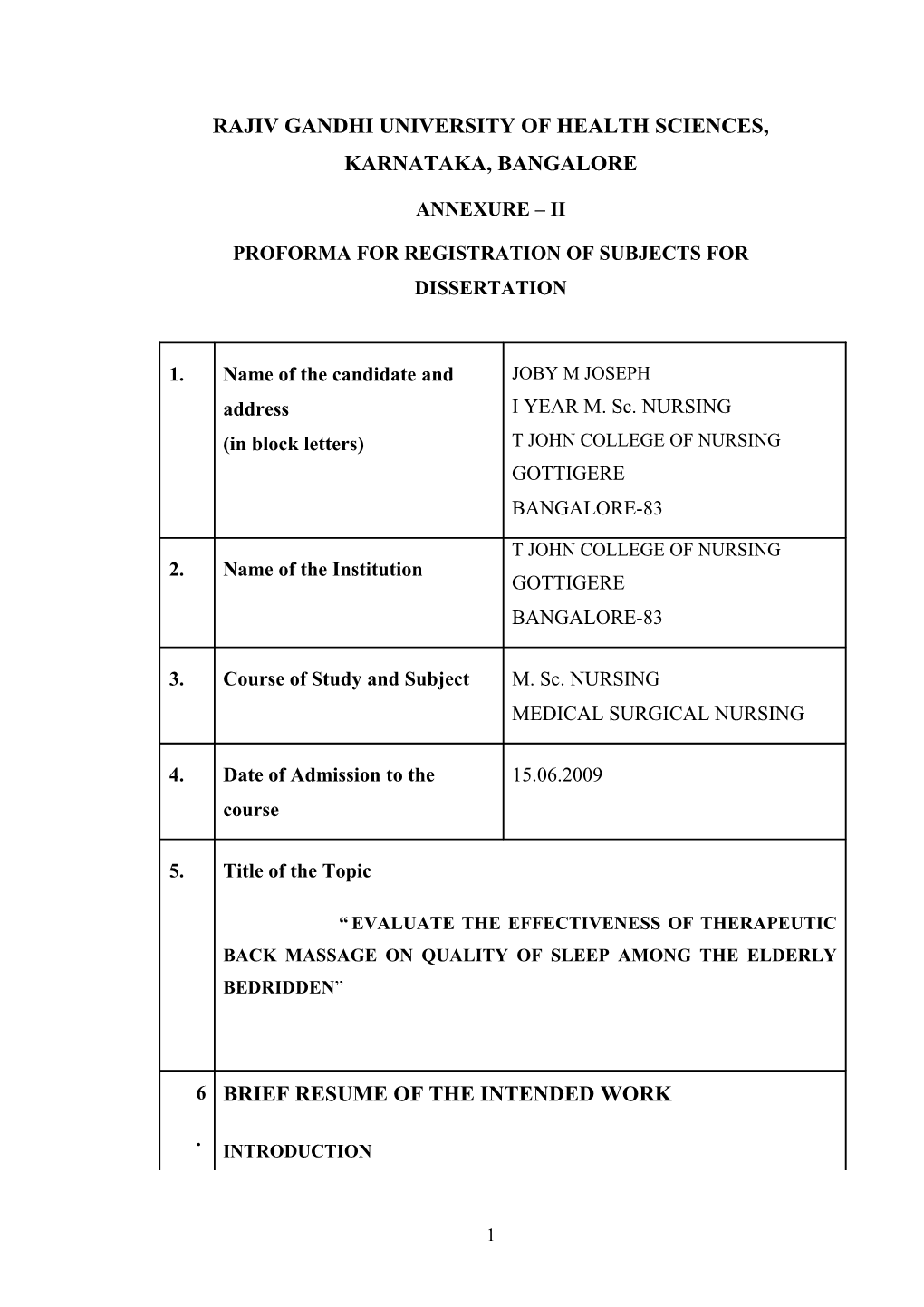
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, KARNATAKA, BANGALORE
ANNEXURE – II
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
1. Name of the candidate and JOBY M JOSEPH address I YEAR M. Sc. NURSING (in block letters) T JOHN COLLEGE OF NURSING GOTTIGERE BANGALORE-83
T JOHN COLLEGE OF NURSING 2. Name of the Institution GOTTIGERE BANGALORE-83
3. Course of Study and Subject M. Sc. NURSING MEDICAL SURGICAL NURSING
4. Date of Admission to the 15.06.2009 course
5. Title of the Topic
“ EVALUATE THE EFFECTIVENESS OF THERAPEUTIC BACK MASSAGE ON QUALITY OF SLEEP AMONG THE ELDERLY BEDRIDDEN”
6 BRIEF RESUME OF THE INTENDED WORK
. INTRODUCTION
1 Medical surgical nursing is the backbone of modern nursing and the practice foundation of virtually all health care institutions1. The geriatric health nursing one of the sub branches of medical surgical nursing which requires more attention and need for the care of old age people. The old age associated with many problems due to aging process. One of the common complaints among the elderly is sleep disturbances mainly those who are in the bed for long time and immobile.2
Sleep disturbances in the old age is insomnia, sleep apnoea, restless legs syndrome, parasomnias, and/or sleep-related eating disorders. Many medical disorders can produce insomnia including asthma, COPD, bronchitis, GERD, dementia, Parkinson’s disease, rheumatoid arthritis, fibromylagia, and hyperthyroidism. Often patients may have poor sleep habits/hygiene which leads to sleep fragmentation. Insomnia most common complaint in sleep disturbances.
The decreased or lack of sleep is known as insomnia.2
Compared to people with normal sleep, patients with insomnia are more likely to experience anxiety and depression and suffer other serious consequences, such as work- and driving-related accidents and an overall increase in mortality rate.3
Acute insomnia is transient short term or adjustment insomnia. The duration of acute insomnia is one night to a few weeks and may be related to environmental or occupational stress or illness. The acute insomnia typically resolves with adaptation or removal of the stressor. Acute insomnia can lead to chronic insomnia if left untreated.
Chronic insomnia is generally defined as difficulty initiating or maintaining nocturnal sleep or difficulty achieving restorative sleep for longer
2 than one month, associated with significant distress and without obvious relationship with other disorders or substance abuse.4
Chronic insomnia can either be primary or co-morbid and waxes and wanes over time. Primary insomnia is the term applied when no co-existing disorder can be identified In addition, primary insomnia often results in other health-related sequelae and patients may present to their primary care physician with major complaints other than insomnia, such as daytime sleepiness, fatigue, mood changes or other symptoms which have a negative impact on daytime functioning. The primary insomnia common among old age people5
Co-morbid insomnia may be obscured by an underlying condition, such as chronic pain, sleep disorders, medications, substance abuse, or a host of other medical and psychiatric conditions 6
Consequently, a diagnosis of insomnia may not be obvious and the
National Centre on Sleep Disorders Research at the National Institutes of Health recently recommended that secondary insomnia be termed ‘co-morbid insomnia’ rather than a symptom of other disorders, emphasizing that large numbers of individuals with chronic illness suffer from fragmented sleep .6
The management of insomnia included the pharmacological and non pharmacological management of insomnia. One of the non pharmacological management of insomnia is therapeutic back massage. Massage therapy means therapists can massage the back by press, rub, and otherwise manipulate the muscles and other soft tissues of the body. They most often use their hands and fingers. Therapeutic back massage induce circulation, relieves pain ,produce relaxation, sense of well being ,maintain hygiene and promote sleep.7
6..1 NEED FOR THE STUDY
3 In the year 2002, all over the world 605 million old person and 400 million living in the low income countries. By 2025, the numbers of elderly expected are 1.2 billion world wide and 840 million in the low income countries.
In 2001 the elderly (people above the age of 60 years) comprise 7.5 percent of total Indian population, and making health care available and accessible to them is one of the health priorities of the country.8
India now has the second largest aged population in the world. The small- family norm means that fewer working, younger individuals are called upon to care for an increasing number of economically unproductive, elderly persons.7
According to the findings of the 60th NSSO Round, the proportion of aged persons who cannot move and are confined to their bed or home ranges from 77 per 1000 in urban areas to 84 per 1000 in rural areas Morbidity9
The epidemiological data on health problems in elderly reported that in
2007 as follows: Poor Vision (45.4%), Hypertension ( 38.2%), Arthritis ( 36.1%),
Bowel complaints ( 31.6%), Depression ( 23.6%), Difficulty in Hearing ( 20.5%),
Weight Loss (19.6%), Anaemia (16.8%), Urinary complaints (13.4%), Diabetes
(13.3%), Fall ( 8.7%), IHD ( 7.7%), Asthma ( 6.6%), COPD ( 4.8%), and
Tuberculosis (3.1%) were the common health problems highlighted by the study.
These all health problems mostly causes sleep disturbances especially bedridden due to any significant problems create sleep disturbances.8
A study was conducted in a skilled-care geriatric hospital regarding sleep disturbances and mortality risk among 272 patients who were aged, in the presence or absence of sleep disturbances were examined by hourly observations of patients over 2 weeks at baseline, and they were prospectively followed up for
2 years to assess mortality. Results show that mortality after 2 years was
4 significantly higher in the night time insomnia, daytime sleepiness, and sleep- onset delay groups. Further, adjusted for age, gender and activities of daily living status, the presence of night time insomnia and sleep-onset delay remained associated with a higher risk of mortality. The study concluded that sleep disturbance may be one of the symptoms indicating poor health or functional deficits, and be an independent risk factor for survival of elderly.10
A study was conducted to assess the adverse effects, sedative-hypnotic drugs (SHDs) are widely used in institutional settings serving the elderly. Using a
2 (Intervention, Control) x 3 (Baseline, Intervention, Withdrawal) mixed design with random assignment to the intervention (n = 15) or control (n = 13) group, the authors sought to determine if a non pharmacological sleep intervention (massage at bedtime) could reduce "as-needed" SHD (PRN-SHD) usage. Each phase of this pilot lasted 7 days and PRN-SHD usage was monitored via chart review. Results, indicating a 13% greater reduction in requests for PRN-SHD for the intervention group when it received massage, approached statistical significance for the quadratic planned comparisons (p = .17) despite limited power (.28) for the observed effect size of .07. While preliminary, results suggest that massage at bedtime may reduce PRN-SHD usage with older adults. Randomized controlled studies with larger samples are needed.11
The number of elderly in the population will be more than double in the next 40 year12. Lindeman(1975) developed an initial list of research priorities for clinical practice that included nursing interventions focused on care of the elderly ,pain management and patient education.13
From the above review and researcher own observation in professionally
5 found that the therapeutic back massage is very effective in promoting the sleep.
Very few studies supporting the therapeutic back massage. The investigator plan to conduct the study to evaluate the effectiveness of therapeutic back massage on quality of sleep among elderly bedridden. 6.2 REVIEW OF LITERATURE
The review of literature discussed under following headings
Studies related to the quality of sleep
A study was conducted on 24 healthy subjects, who wore an actigraph for seven nights while adhering to a regular sleep-wake schedule followed by a 90-minute, polysomnographically-recorded nap. The influence of two-night and seven-night averages of total sleep time immediately prior to the nap on nap architecture was examined. According to the results, less prior nightly total sleep time increased the percentage of REM sleep during the nap. Average total sleep time did not affect any other architecture variable of the nap. Bed and wake time appear to influence REM sleep percentage only in the short-term. “The findings of our study indicate that minute differences in 'normal' sleep duration influence the percentage of REM sleep obtained in a subsequent afternoon nap," said Kanady. "Specifically, 10 minutes less sleep per night led to a 1.3 percent increase in nap REM percentage. These results may have important implications for studies examining sleep-dependent memory consolidation, particularly.14
Studies related to the sleep disturbances in elderly
A study was conducted about the Treatment of elderly primary insomnia
Participants were 149 elderly patients with DSM-IV primary insomnia including evidence of daytime sleepiness (53 males, 96 females; mean age 71.3yrs, range
65-86yrs). A randomized, multi centre, double-blind, placebo-controlled, parallel-
6 group design was used to assess the hypnotic efficacy of EVT 201 1.5 and 2.5mg during seven consecutive nights. Results shows that the compared to placebo,
EVT 201 1.5 and 2.5mg increased TST (30.9, 56.4min, respectively; p=0.0001, p<0.0001); reduced wake after sleep onset (WASO; -15.2, -36.1min, respectively; p=0.014, p<0.0001); reduced latency to persistent sleep (LPS; -15.9, -19.9min, respectively; p=0.009, p=0.001). The 2.5mg dose also reduced WASO in hours 5-
8 (-16.3min, p=0.001). The study concluded that EVT 201 improved PSG measures of sleep onset and sleeps maintenance and significantly reduced daytime physiological sleep tendency. These findings suggest that treatment of primary insomnia in older patients has the potential to improve daytime sleepiness as well as sleep.15
A study was conducted on evaluate the efficacy and tolerability of
Gaboxadol in the treatment of adult and elderly patients with primary insomnia.
Randomized, double-blind, placebo-controlled, multi centre, 30-night, polysomnography studies in sleep laboratory. Among primary insomnia, 18-64 y
(adult study), or > or =65 y (elderly study) patients Primary endpoints were wake after sleep onset (WASO) and latency to persistent sleep (LPS). Slow wave sleep
(SWS) was a secondary endpoint. Analyses were based on the change from baseline for the average of nights 1/2, and nights 29/30, and compared Gaboxadol versus placebo. The study concluded that the maximum studied doses of
Gaboxadol (GBX15 in adult patients and GBX10 in elderly patients) were effective at enhancing objective polysomnography measures of sleep maintenance and SWS, and also some subjective sleep measures, over 30 nights but had little or no effects on sleep onset. The clinical relevance of the enhancement of SWS by
7 Gaboxadol is unclear.16
A Cross-sectional study was conducted on the prevalence, characteristics, and risk factors of sleep and daytime sleepiness problems in this specific population among eight hundred and seventy six patients with CP treated with long-term Opioids. Results shows that Insomnia-type sleep problems and combined sleep and sleepiness problems were reported by 87 percent and 49 percent of the sample, respectively. The study concluded that sleep and daytime sleepiness problems are common among Opioid-treated primary care patients with CP and seem to be related mainly to depression and pain severity. Physicians caring for Opioid-treated patients with CP may want to assess them for sleep disorders as a part of routine CP care.17
A Randomized, double blind, controlled clinical trial was conducted to evaluate 6 months' Eszopiclone treatment upon patient-reported sleep, fatigue and sleepiness, insomnia severity, quality of life, and work limitations. 54 research sites in the U.S. among830 primary insomnia patients who reported mean nightly total sleep time (TST) < or = 6.5 hours/night and/or mean nightly sleep latency
(SL) >30 min. Intervention given as Eszopiclone 3 mg or matching placebo.
Results shows that patient-reported sleep and daytime function were improved more with Eszopiclone than with placebo at all months (P <0.001). Eszopiclone reduced Insomnia Severity Index scores to below clinically meaningful levels for
50% of patients (vs. 19% with placebo; P <0.05) at Month 6. SF-36 domains of
Physical Functioning, Vitality, and Social Functioning were improved with
Eszopiclone vs. placebo for the Month 1-6 average (P < 0.05). Similarly, improvements were observed for all domains of the Work Limitations
8 Questionnaire with Eszopiclone vs. placebo for the Month 1-6 average (P
<0.05The study concluded that this is the first placebo-controlled investigation to demonstrate that long-term nightly pharmacologic treatment of primary insomnia with any hypnotic enhanced quality of life, reduced work limitations, and reduced global insomnia severity, in addition to improving patient-reported sleep variables.18
Studies related to therapeutic back massage and quality of sleep among elderly
A study was conducted on examining the effects of massage therapy for senior citizens and they found that at least 50 percent of the elderly who were tested showed a reduction in their rates of breathing, an increase in their range of motion, an improvement of their postures, development of more body awareness, their skin took on healthier colors and their muscle tones and promotion of sleep were enhanced. The same study also showed that 100 percent of the senior citizen who were tested showed a dramatic improvement in their moods and their attitudes toward life in general.19
A study was conducted on back massage and similar technique to promote sleep in elderly people It states that insomnia is a frequent problem among elderly people. As aconsequence, sedative hypnotic drugs are prescribed very often that can lead to problamaticeffects.as an alternative to sedative hypnotic drugs nurses use relaxing interventions to promote sleep. One of these techniques, the back massage, is very popular because of the expected relaxing effect of touch. gains this back ground ,this review includes 16 surveys of the international nursing literature and the German literature, that analyze the most
9 common intervention in Germany “Atemstimulierende Einreibung”,similar to effleurage. These studies are presented and evaluated. The results indicated that these interventions promote relaxation and sleep and that they are perceived as very pleasant by the elderly.20
A study was conducted on application of The Shuler Nurse
Practitioner Practice Model with elderly patients through use of a gerontological wholistic assessment and the utilization of the model in developing a treatment plan and evaluating patient outcomes. Selected literature from nursing and medicine, including natural, alternative, and complementary (NAC) therapies, as well as the authors' personal experiences. The literature concluded that providing health care services to the elderly involves recognition of not only physical ailments, but also an awareness of how functional status, psychological condition, social support, environmental conditions and cultural, as well as spiritual beliefs, shape the total health care needs of this vulnerable group. Nurse practitioners who work with the aged could benefit from a theoretically based, wholistic assessment guide. Treatment plans that include NAC therapies and healing strategies should be considered. Outcome evaluations should reflect adherence to the elders' preferences regarding quality and end-of-life issues.21
A study was conducted on examine the feasibility of implementing specific nursing interventions to promote sleep in hospitalized older adults. The experimental group received a sleep protocol intervention while the control group received usual night time care. While no differences were noted in sleep quality and duration between groups, the experimental group experienced better sleep quality (P = .001), ability to remain asleep (P = .018) and used fewer sleep
10 medications than the control group (P = .044). In addition, those taking sleep medications experienced more awakenings and fewer sleep hours. Experimental group patients identified preferences such as personal hygiene, awareness of normal bedtime, receiving a back rub, straightening bed linens, and receiving a bedtime snack. This pilot provides initial support for the feasibility and utility of implementing a sleep protocol in an acute care setting.22
The daily stress and strain of life takes a huge toll on our bodies. Result- aching backs, stiff neck and painful shoulders. Getting a massage done is one of the best ways of relaxing and rejuvenating your self. Back massage is a great way of getting rid of back aches as massage helps in relaxation and increased circulation. The best way is to get a back massage done. Get it done from a professional. Here are some helpful tips. While getting a back massage, you need to lie down flat on your belly on a comfortable surface like a floor mat or firm bed. Usually oils are used for back massage to decrease friction on the skin.
However, according to experts, less quantity of oil application leads to greater friction and pressure. The back massage begins at the spine, starts at the lower back area and slowly moves towards the shoulders. Massage also helps in treatment of insomnia along with aiding in providing relief from chronic pain.23
6.3 STATEMENT OF THE PROBLEM
“ A QUASI EXPERIMENTAL STUDY TO EVALUATE THE
EFFECTIVENESS OF THERAPEUTIC BACK MASSAGE ON QUALITY
OF SLEEP AMONG THE ELDERLY BEDRIDDEN IN SELECTED
HOSPITALS OF BANGALORE”
11 6.4 OBJECTIVES OF THE STUDY
1. Assess the pre test level of sleep in both experimental and control
group.
2. Administer therapeutic back massage in experimental group.
3. Evaluate the effectiveness of therapeutic back massage by
comparing the pre test and post test level of sleep in both
experimental and control group.
4. Associate the post test level of sleep with selected socio
demographic variable. 6.5 OPERATIONAL DEFINITION
1. EVALUTE: Measure the level of sleep before and after the therapeutic back massage
2. EFFECTIVENESS: Outcome of the intervention measured in terms of increased in numerical scores.
3. THERAPEUTIC BACK MASSAGE: The one of the type of therapy in this therapist using the fingers to rub and massage the back with four steps such as circular massage ,effleurage, pettisarge and kneading.
4. QUALITY OF SLEEP – A periodic state of rest accompanied by varying degree of unconsciousness and relative inactivity which measured through the scale prepared by the researcher.
5. ELDERLY BEDRIDDEN
Those who are falls on the age group of 60 years and above and unable to move from the bed due to their health condition. 6.6 ASSUMPTIONS
12 1 Therapeutic back massage promote sense of well being of the bedridden
patient
2. Therapeutic back massage reduce the pain and discomfort of the
bedridden patients
3. Elderly bedridden may have sleep disturbances and decreased sleep 6.7 DELIMITATIONS
1. The sample size is limited to 60 elderly bedridden Patients
2. Prescribed data collection period is only 4 to 6 wks
6.8 HYPOTHESIS
H1: There is a significant increase in the level of sleep after the
administration of therapeutic back massage than before in the
experimental group
7. MATERIALS AND METHODS
7.1 SOURCE OF DATA
. Elderly those who are living in the selected areas of Bangalore
13 7.1.1 RESEARCH DESIGN
The research design adopted for the study was quasi experimental
(two group pre test and post test) with manipulation no randomization and control group.
Experiment
al group O1 X O2 Control
group O1 …….. O2
O1-Pretest level of sleep
O2-Posttest level of sleep
X- Intervention- therapeutic back massage 7.1.2 SETTING
The study will be conducted in selected hospitals of Bangalore.
7.1.3 POPULATION
Elderly people those who are admitted in the selected hospitals of Bangalore
CONCEPTUAL FRAMEWORK:
The conceptual frame work of the study based on the Roy’s adaptation
Model
7.2 METHOD OF DATA COLLECTION
7.2.1 SAMPLING PROCEDURE
Non Probability – convenient sampling
7.2.2 SAMPLE SIZE
Sample comprises of 60 elderly bedridden Patients. Thirty in experimental
14 group and thirty in control group
7.2.3 INCLUSION CRITERIA FOR SAMPLING
1. Samples are elderly people admitted in selected Hospitals of
Bangalore.
2. Those who can able to understand the Kannada.and English.
3. Those who are willing to participate in the study.
4. Both male and female elderly person those who are in an age of
above 60.
5. Elderly bed ridden patients those who admitted in selected hospital of
Bangalore.
7.2.4 EXCLUSION CRITERIA FOR SAMPLING.
1. Those who are absent during the period of study.
2. Those who are in critical condition.
3. Those who are using any sleep inducing medicines.
4. Those who are in unconscious state.
7.2.5 INSTRUMENTS INTENDED TO BE USED
This instrument has two parts. Part A consist of
sociodemographic variables of sample, Part B consist of sleep self
instructed rating scale which is prepared by the researcher indented to be
used in the study.
7.2.6 DATA COLLECTION METHOD
Sleep Self instructed rating scale will be used to collect the data.
7.2.7 PLAN FOR DATA ANALYSIS
15 The data analysis planned for the descriptive statistics and inferential
statistics. The descriptive statistics plan to use in data analysis are the
percentage, mean and standard deviation and inferential statistics are paired
‘t’ test and chi square test ETHICAL CONSIDERATION
7.3 Does the study require any intervention to be provided to the elderly? Yes.
7.4 Has ethical clearances being obtained from institution?
Yes.
7.5Have you concerned for the hospital authority?
Yes.
16 LIST OF REFERENCES
1. URL:http://www.evolve.elsiever.com/monahan/medsurg.
2. Mitler MM, Dement WC, Dinges DF. Sleep medicine, public policy, and public health. In: Kryger MH, Roth T, Dement WC, editors. Principles and practices of sleep medicine. 3rd ed. Philadelphia: WB Saunders; P: 2000. pp.
580–8.
3. Kripke DF, Garfinkel L, Wingard DL, et al. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59: 131–6. [PubMed]
4. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. APA: Washington, DC; 1994.
5. National Institutes of Health. State-of-the-Science Conference Statement.
Bethesda, MD: Aug 18, 2005.
6. American Academy of Sleep Medicine. Diagnostic and coding manual.
2nd Ed. Rochester, MN: 2005. International classification of sleep disorder.
7. Bob stockfield. Massage therapy: An Introduction
.nccam..nih.gov/news/2009
8 Srivastava RK. Multicentric study to establish epidemiological data on
health problems in elderly: a Govt. of India and WHO collaboration
programme. Ministry of Health & Family Welfare, Government of
India 2007.
17 9 Health Care and Condition of the Aged. National Sample Survey 60th
Round (January to June 2004). Government of India, March 2006. p. 54-
65
10 K. Manabe, T. Matsui, M. Yamaya, T. et al Sleep Patterns and
Mortality among Elderly Patients in a Geriatric Hospital. Gerontology
2000; 46:318-322. Sato-Nakagawa, N. Okamura, H. Arai, H. Sasaki
11 Rhonda Nelson and Catherine Coyle* Using Massage to Reduce Use o
Sedative-Hypnotic Drugs With Older Adults: A Brief Report From a Pilot
study. Journal of Applied Gerontology 2009; 28: 768.
12 Basavanthappa.B.T. Nursing research.second edition .jaypee
publications. New delhi.2007
13 Nancy Burns, Susan.K.G.Understanding nursing research-building an
evidence based practice. Fourth edition.elsiever publications.2007.
14 Jennifer Kanady .Decreased Total Sleep Time Associated with
Increased REM Sleep during Subsequent Naps American Academy of
Sleep Medicine (2008, June 10). Science Daily. Retrieved December 12,
2009, from http://www.sciencedaily.com
/releases/2008/06/080610071936.htm
15 Walsh JK, Salkeld L, and Knowles LJ, et al .Treatment of elderly
primary insomnia patients with EVT 201 improves sleep initiation, sleep
maintenance, and daytime sleepiness. Sleep Med. 2009 Nov 27. [ Epub
18 ahead of print]
16 Lankford DA, Corser BC, Zheng YP et al. Effect of Gaboxadol on
sleep in adult and elderly patients with primary insomnia: results from two
randomized, placebo-controlled, 30-night polysomnography studies.
Sleep. 2008 Oct 1; 31(10):1359-70.
17 Zgierska A, Brown RT, Zuelsdorff M.Sleep and daytime sleepiness
problems among patients with chronic non cancerous pain receiving long-
term opioid therapy: a cross-sectional study. J Opioid Manag. 2007 Nov-
Dec;3 (6):317-27.
18 Walsh JK, Krystal AD, Amato D A .et al Nightly treatment of primary
insomnia with Eszopiclone for six months: effect on sleep, quality of life,
and work limitations. Sleep. 2007 Aug 1;30(8):959-68
19 Schiff A. Literature review of Back massage and similar techniques to
promote sleep in elderly people.Pflege.2006; 19(3):163-173.
20 Massage Therapy For Senior Citizens© Copyright 2009 updated
MassageTherapyStartup.com
21 Pamela A. Shuler Roxana Huebscher and Judith Hallock Providing
Wholistic Health Care for the Elderly: Utilization of the Shuler Nurse
Practitioner Practice Model. Journal of the American Academy of Nurse
Practitioners. Volume 13 Issue 7, Pages 297 - 303 Published Online:
24 May 2005
19 22 R. Lareau, L. Benson, K. Watcharotone, G. Manguba .Examining the
Feasibility of Implementing Specific Nursing Interventions to Promote
Sleep in Hospitalized Elderly Patients. Geriatric Nursing, Volume 29,
Issue 3, Pages 197-206: 2005 www.elsiever.com
23 Benefits and techniques of back massagewww.ayushveda.com/.../back-
massage-benefits-and-techniques27: Jan 2009.
20 21 8. Signature of the candidate
9. Remarks of the guide
10. Name and designation of (in block letters)
10.1 Guide
10.2 Signature
10.3 Co-guide (if any) .
10.4 Signature
11 11.1 Head of the department
11.2 Signature
12. 12.1 Remarks of the Chairman and Principal
12.2 Signature
22