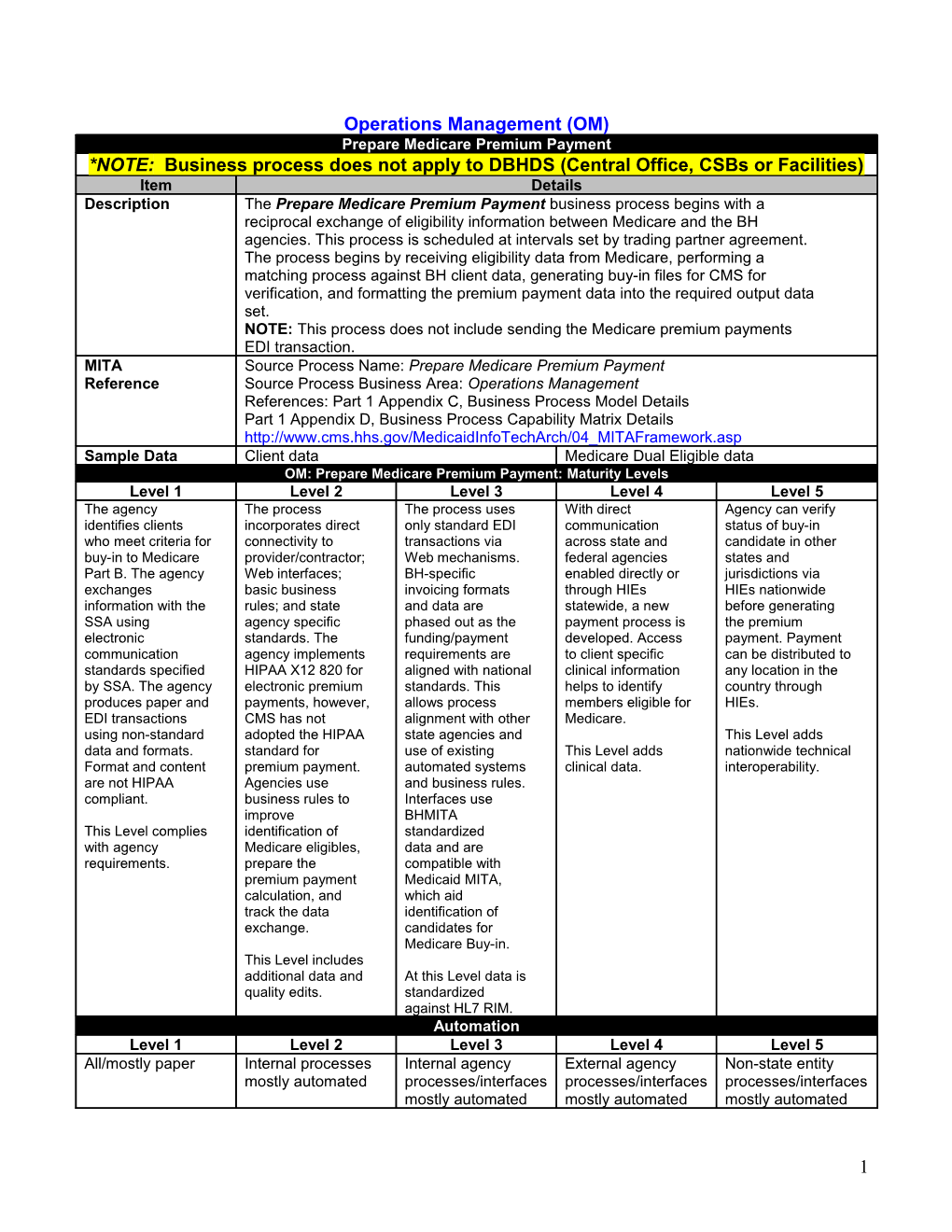
Operations Management (OM) Prepare Medicare Premium Payment *NOTE: Business process does not apply to DBHDS (Central Office, CSBs or Facilities) Item Details Description The Prepare Medicare Premium Payment business process begins with a reciprocal exchange of eligibility information between Medicare and the BH agencies. This process is scheduled at intervals set by trading partner agreement. The process begins by receiving eligibility data from Medicare, performing a matching process against BH client data, generating buy-in files for CMS for verification, and formatting the premium payment data into the required output data set. NOTE: This process does not include sending the Medicare premium payments EDI transaction. MITA Source Process Name: Prepare Medicare Premium Payment Reference Source Process Business Area: Operations Management References: Part 1 Appendix C, Business Process Model Details Part 1 Appendix D, Business Process Capability Matrix Details http://www.cms.hhs.gov/MedicaidInfoTechArch/04_MITAFramework.asp Sample Data Client data Medicare Dual Eligible data OM: Prepare Medicare Premium Payment: Maturity Levels Level 1 Level 2 Level 3 Level 4 Level 5 The agency The process The process uses With direct Agency can verify identifies clients incorporates direct only standard EDI communication status of buy-in who meet criteria for connectivity to transactions via across state and candidate in other buy-in to Medicare provider/contractor; Web mechanisms. federal agencies states and Part B. The agency Web interfaces; BH-specific enabled directly or jurisdictions via exchanges basic business invoicing formats through HIEs HIEs nationwide information with the rules; and state and data are statewide, a new before generating SSA using agency specific phased out as the payment process is the premium electronic standards. The funding/payment developed. Access payment. Payment communication agency implements requirements are to client specific can be distributed to standards specified HIPAA X12 820 for aligned with national clinical information any location in the by SSA. The agency electronic premium standards. This helps to identify country through produces paper and payments, however, allows process members eligible for HIEs. EDI transactions CMS has not alignment with other Medicare. using non-standard adopted the HIPAA state agencies and This Level adds data and formats. standard for use of existing This Level adds nationwide technical Format and content premium payment. automated systems clinical data. interoperability. are not HIPAA Agencies use and business rules. compliant. business rules to Interfaces use improve BHMITA This Level complies identification of standardized with agency Medicare eligibles, data and are requirements. prepare the compatible with premium payment Medicaid MITA, calculation, and which aid track the data identification of exchange. candidates for Medicare Buy-in. This Level includes additional data and At this Level data is quality edits. standardized against HL7 RIM. Automation Level 1 Level 2 Level 3 Level 4 Level 5 All/mostly paper Internal processes Internal agency External agency Non-state entity mostly automated processes/interfaces processes/interfaces processes/interfaces mostly automated mostly automated mostly automated
1 VA As Is: VA To Be: Standards Level 1 Level 2 Level 3 Level 4 Level 5 Use few or no Internal processes Internal agency External agency Non-state entity national standards use national processes/interfaces processes/interfaces processes/interfaces standards mostly use national mostly use national mostly use national standards standards standards VA As Is: VA To Be: Cross Coordination Level 1 Level 2 Level 3 Level 4 Level 5 Little/no Internal agency Internal agency External agency Non-state entity coordination across operational program processes program and program and processes or with processes coordinated operational operational other programs coordinated processes processes coordinated coordinated VA As Is: VA To Be: Client Data Level 1 Level 2 Level 3 Level 4 Level 5 Little/no access to Internal processes Internal agency External agency Non-state entity client specific data have access to processes have processes have processes have client access to client access to client access to client specific data specific data specific data specific data VA As Is: VA To Be: Interoperability Level 1 Level 2 Level 3 Level 4 Level 5 None Limited Interoperability with Interoperability with Interoperability with interoperability internal agency external agency non-state entity internally or limited systems other than systems other than systems to claims processing claims processing claims processing systems VA As Is: VA To Be:
2