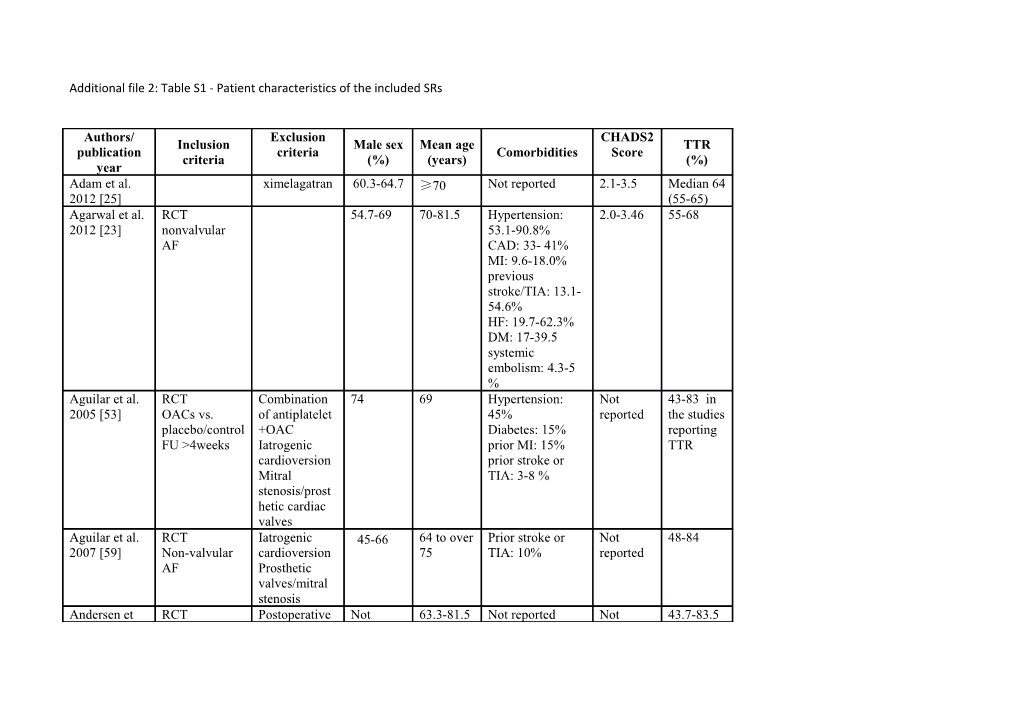
Additional file 2: Table S1 - Patient characteristics of the included SRs
Authors/ Exclusion CHADS2 Inclusion Male sex Mean age TTR publication criteria Comorbidities Score criteria (%) (years) (%) year Adam et al. ximelagatran 60.3-64.7 ≥70 Not reported 2.1-3.5 Median 64 2012 [25] (55-65) Agarwal et al. RCT 54.7-69 70-81.5 Hypertension: 2.0-3.46 55-68 2012 [23] nonvalvular 53.1-90.8% AF CAD: 33- 41% MI: 9.6-18.0% previous stroke/TIA: 13.1- 54.6% HF: 19.7-62.3% DM: 17-39.5 systemic embolism: 4.3-5 % Aguilar et al. RCT Combination 74 69 Hypertension: Not 43-83 in 2005 [53] OACs vs. of antiplatelet 45% reported the studies placebo/control +OAC Diabetes: 15% reporting FU >4weeks Iatrogenic prior MI: 15% TTR cardioversion prior stroke or Mitral TIA: 3-8 % stenosis/prost hetic cardiac valves Aguilar et al. RCT Iatrogenic 45-66 64 to over Prior stroke or Not 48-84 2007 [59] Non-valvular cardioversion 75 TIA: 10% reported AF Prosthetic valves/mitral stenosis Andersen et RCT Postoperative Not 63.3-81.5 Not reported Not 43.7-83.5 al. 2008 [55] AF or flutter AF reported reported FU ≥3 months Valvular disease Assiri et al. RCT 58.7 71 Not reported 1.8-3.47 42-83 2013 [50] Double blind English VKA: INR 2-3 Baker et al. RCT not 69-73 Hypertension: 70- 2.1-3.48 55-64 2012 [33] Nonvalvular reported 90.8%, AF CHF: 31-62.6%, Apixaban, DM: 21.4-40.4%, dabigatran, prior TIA or rivaroxaban vs. stroke: 17.5- warfarin or 54.9% each other outcome: stroke/SE major bleeding Briceno et al. RCT 60.3-80.6 70-74 Not reported 2.1-3.5 55.-70 2015 Nonvalvular AF NOACs or Watchman device vs. warfarin Cameron et al. RCT (phase Trials Not 62-83 Prior stroke 3%- 1.9-3.5 44-83 2014 [49] III) including reported 55% Nonvalvular patients with AF contraindicati on to VKA: INR 2-3 anticoagulatio English n
Capodanno et RCT (hase III) 63 71 Prior stroke/ 2.5 58-66 al. 2013 [27] Non-valvular SE/TIA: 31% (2.1-3.5) AF Prior MI: 16% NOACs vs. Hypertension: warfarin 85% Both efficacy and safety outcomes reported RCT study 69.6-73 Not reported Not 60-65 AF drug: 59- reported Chatterje et al. NOACs 83.7 2013 [42] control drug: 58- 81.1 RCT Postoperative 41-100 65-75 Not reported Not Not ≥18 years atrial reported reported Coleman et al. fibrillation or 2012 [45] AF Report data on flutter MGIB Cooper et al. FU >12 month 32-100 64-80.2 Prior stroke: 0- Not Not 2006 [58] 100% reported reported RCT 60.3-70 70-73 Previous Not Not N >3000 stroke/TIA: reported reported intention-to- 19.8-24 % treat analysis Hypertension: 72-90,3% Dogliotti et al. 2013 [28] Diabetes: 23.1-40,4%
LVD or heart failure: 31.8-62.6% Dogliotti et al. RCT (phase II FU <1 year 50-100 64-83 Hypertension: 2-3.47 or Not 2014 [46] or III) Subgroup 31.5-90.5% not reported VKA, ASA, analysis Diabetes: 4-40% reported clopidogrel or Posthoc prior MI: 9-19% for single NOACs analysis or not reported; studies Non-valvular Low-dose prior TIA or AF warfarin stroke: 5-55% or Intention-to- Registry data not reported treat analysis Harenberg et RCT 60.30- 70-73 Not reported ≥3: 55-66 al. 2012 [61] Control: VKA 64.75 30.22- adjusted (INR 86.95 2-3) Hart et al. RCT Mitral 71 69 Hypertension: 45 Not Not 1999 [4] FU >3 months stenosis/prost % reported reported hetic cardiac prior stroke or valves TIA: 20% RCT Mitral 75 71 Not reported Not Not Hart et al. Nonvalvular stenosis/prost reported reported 2007 [57] AF hetic cardiac FU ≥12 weeks valves RCT 59-82 65-73 Not reported 1.8-3.5 45.1-66 NOAC Holster et al. bleeding as 2013 outcome indication for anticoagulation RCT ximelagatran 57-82.9 70-73 previous 2.1-3.5 44-68 NOAC vs. darexaban stroke/TIA:18- warfarin 63.9% AF Heart failure: 32- Jia et al. 2014 63% Diabetes: 23- 62.8% Hypertension: 79- 94% Lega et al. RCT Not 70-73 Not reported Not 55-64 2014 nonvalvular reported reported AF results reported according to age, CHADS2 score, heart failure, diabetes GFR prioir exposure to VKA, prior stroke or TIA RCT Approx. 70-73 Not reported 2.1-3.5 58-68.4 Patients with 66 AF NOAC vs. warfarin FU >1 year One of the Liew et al. following 2014 [29] outcomes: intracranial bleeding, bleeding-,all- cause or vascular mortality Lin et al. 2015 RCT (II or III) warfarin at NRSs 71.5 Hypertension 17- 2.3 Not observational non-standard 56%, 94%, chronic reported studies doses RCTs heart failure 1- AF triple therapy 62% 70%, diabetes warfarin, ASA with warfarin, mellitus 3-45%, or NOACs ASA, prior TIA/ stroke clopidogrel 3-55% Lip et al. 2006 RCT Not 64-80 Not reported Not Not [54] Non-valvular reported reported reported AF
Miller et al. RCT ximelagatran 60.3-65 70-73 Prior stroke/TIA: 2.1-3.5 55-64 2012 [30] Oral 19.2-62.6% anticoagulants Heart failure: AF 31.8-62.6% FU > 1 year Diabetes mellitus: 23.4-40.4% Hypertension: 78.9-90.8% RCT (phase Phase II trials 60.3-80.6 70-73 CHF: 32.0-62.5% 2.1-3.5 55-68 III) Observational Hypertension: NOACs vs. studies 72.2-93.5% warfarin Interventions Diabetes: Providência et Non-valvular (e.g. catheter 23.3-39.9% al. 2014 [31] AF ablation) as Prior stroke/TIA: comparison 18.3-63.6% Prior MI: 7.7- 17.3% RCT 57-65 70-73 previous 2.1-3.5 58-68 AF stroke/TIA: 18- NOACs vs. 55% Rong et al. warfarin Heart failure: 32- 2015 63% Diabetes: 23-40% Hypertension: 79- 94% RCT Phase I trials 60-70 67.6-74.9 Not reported Not 65 Patients with reported AF treated for the prevention of stroke VKA, aspirin, Roskell et al. clopidogrel, 2010 [47] indobufen, idraparinux, triflusal, ximelagatran, and dabigatran
Ruff et al. 60-65 70-73 Previous 2.1-3.5 65 2014 [44] RCT (phase stroke/TIA: 29% (58-68) III) (20-55%) Patients with Heart failure: AF 46% (35-63%) Diabetes: 31% NOACs vs. (23-40%) warfarin Hypertension: 88% (79-94%) Prior myocardial infarction: 15% (11-18%) RCT 61-64 70.1-71 Prior stroke/TIA: Not 57.1-65 NOACs vs. 100% reported conventional Diabetes: 21.4- therapy 26% Sardar et al. patients with Hypertension: 77- 2013 [43] and without 85% prior stroke/TIA FU >1years Sardar et al. RCT in AF 53,9 - Not reported Not Not 2014 [26] NOACs (vs. trials 58- 71,6 reported reported conventional 65 subgroup therapy) for ≥75 elderly participants Schneeweiss RCT (phase 60.3-65 70-73 Only reported for Only Only et al. 2012 III) warfarin group: reported reported [51] prior for for stroke/TIA/syst warfarin warfarin embolism: 19.7- group: group: 54.6% ≤1: 0- 55-64 HF: 31.9-62.3% 34% Diabetes: 23.4- 39.5% 2: 13.1- Hypertension: 37%; 78.9-90.8% ≥3:30.2- 86.9% Segal et al. RCT 24-100 66-80 DM: 8%-32%, Not Not 2000 [56] CHF: 9%-71%, reported reported hypertension: 32%-58% Senoo et al. RCT 76.7-82.9 70-73 previous 2.0-3.27 60 2015 NOAC or stroke/TIA: 24.8- warfarin 63.8% Japanese Heart failure: 18- patients with 41.3% AF Follow Up >1 year Sharma et al. RCT (phase II 60.3-82.4 Only data Not reported 1.8-3.5 55-65 2015 [22] or III) for (Subgroup > AF and VTE patients 75 with AF) NOACs vs. >75 VKA included FU > 3 month Taylor et al. Non-rheumatic Combined use Not 64-80 Prior TIA/stroke: Not Not 2001 [60] AF of reported 5.5-50% reported reported Antiplatelet or anticoagulatio anticoagulation n/antiplatelet >1 year
RCT 35.5-64.3 70-73 Prior Not 55-65 Comparison to stroke/TIA/SE: reported a Vit. K 19.2-54.9% Testa et al. antagonist Previous MI: 2012 [32] FU >1year 14.5-16.9% Intention-to- Diabetes 23.1- treat analysis 40.4% Verdecchia et RCT (phase 60-65 70-73 Prior stroke/TIA: 2.1-3.5 55-65 al. 2015 [48] III) 20.0-54.8 NOACs vs. HF: 32.0-62.5 warfarin Diabetes: 23.3- Non-valvular 40.0 AF Hypertension: 78- Intention-to- 9-90.5% treat analysis FU >1 year
Note: AF=atrial fibrillation, ASA=aspirin, CAD=coronary artery disease, CHF=congestive heart failure, DM=diabetes mellitus, FU= Follow up, GFR= glomerular filtration rate, HF=heart failure, LVD=left ventricular diastolic, MGIB=major gastrointestinal bleeding, MI=myocardial infarction, NOAC=new oral anticoagulants, OAC=oral anticoagulation, RCT=randomised controlled trial, SE=systemic embolism, TIA= transient ischemic attack, VKA= vitamin K antagonists, VTE= venous thromboembolism