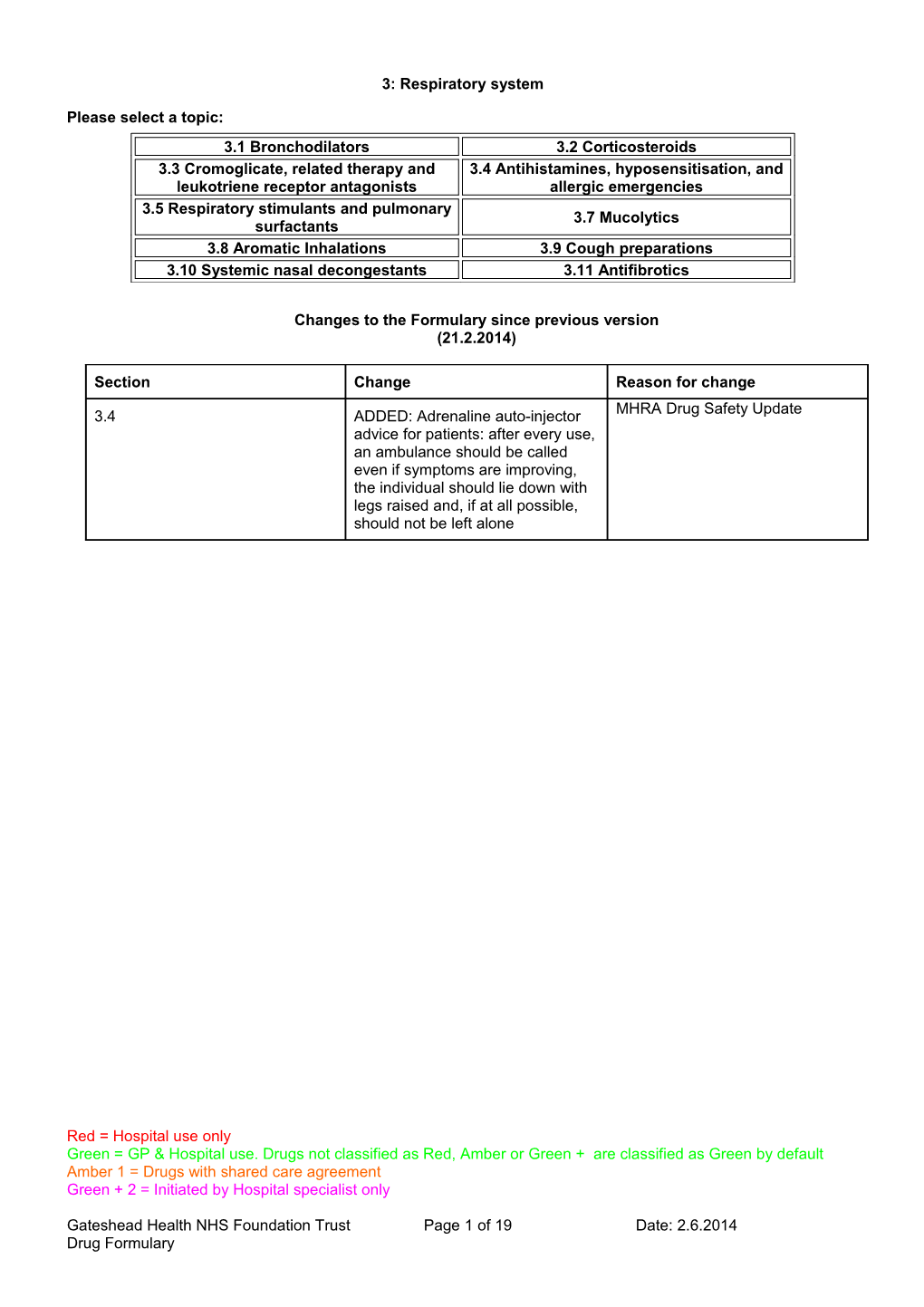
3: Respiratory system
Please select a topic: 3.1 Bronchodilators 3.2 Corticosteroids 3.3 Cromoglicate, related therapy and 3.4 Antihistamines, hyposensitisation, and leukotriene receptor antagonists allergic emergencies 3.5 Respiratory stimulants and pulmonary 3.7 Mucolytics surfactants 3.8 Aromatic Inhalations 3.9 Cough preparations 3.10 Systemic nasal decongestants 3.11 Antifibrotics
Changes to the Formulary since previous version (21.2.2014)
Section Change Reason for change
3.4 ADDED: Adrenaline auto-injector MHRA Drug Safety Update advice for patients: after every use, an ambulance should be called even if symptoms are improving, the individual should lie down with legs raised and, if at all possible, should not be left alone
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 1 of 19 Date: 2.6.2014 Drug Formulary General notes
Prescribers should refer to the 'British Guideline on the Management of Asthma' produced by the British Thoracic Society (BTS) and SIGN (see www.sign.ac.uk). For chronic obstructive pulmonary disease (COPD) refer to: BTS guidelines for COPD and NICE Clinical Guideline 12 See BNF section 3.1.1. and local GMMC Guidelines for COPD.
Chlorofluorocarbon (CFC) in metered dose inhalers (MDIs) are gradually being replaced by non-ozone-depleting propellants such as hydrofluorocarbons; doses are not always equivalent.
Qvar® beclometasone is not equipotent to the existing CFC-containing beclometasone pMDI. Therefore it is important that prescribers are aware of the key prescribing issues
Prescribing issues:
CFC-free beclometasone must be prescribed by brand name to avoid confusion with other beclometasone inhalers (MHRA guidance).
Patients should be made aware of the change in their prescription and the potential differences in treatment e.g. taste and feel of activation (less obvious than with CFC-containing pMDI).
Dissemination of these guidelines and implementation of changes will be conducted by the GP practice pharmacists in agreement with the GPs within each practice.
When transferring a well controlled patient onto Qvar® treatment, initially a 100mcg metered dose of Qvar® should be substituted for: . 200-250mcg of beclometasone dipropionate or budesonide . 100mcg of fluticasone
When transferring a poorly controlled patient onto Qvar® treatment, initially a 100mcg metered dose of Qvar® should be substituted for 100mcg beclometasone dipropionate, budesonide or fluticasone.
Patients admitted to secondary care should remain on their prescribed therapy unless a change is clinically appropriate.
Changing the type of inhaler device may affect the effectiveness of therapy and the incidence of adverse effects.
Generally, manually actuated pressurised metered dose inhalers (MDIs) are the cheapest devices available and should be first choice provided that the patient can use them efficiently. When use is inefficient, alternatives include large volume spacers, dry powder inhalers (DPIs) or breath-actuated MDIs (e.g. Autohaler, Easi-Breathe®). Choice of device should be considered on basis of cost, patient-acceptability and ability to use the inhaler. If a patient elects not to use a prescribed spacer, then an alternative device should be used. See table on the following page for devices available for medicines used for asthma and COPD.
Inhaler-induced cough by MDI may be an indicator for change of device.
It is essential to specify inhaler device, strength and dose.
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 2 of 19 Date: 2.6.2014 Drug Formulary Not all spacers are compatible with all inhalers; users should seek advice from their pharmacist or respiratory nurse specialist regarding the appropriate spacer to be used.
Patients with an acute severe asthma attack may benefit from the unlicensed use of intravenous or nebulised magnesium sulphate.
Older Patients - Inhaler devices
Older patients may have difficulty using any inhaler device due to reduced hand strength, poor inspiratory effort, or confusion. Individual assessment is required.
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 3 of 19 Date: 2.6.2014 Drug Formulary Inhaler devices available for drugs in the GMMC Formulary for asthma and COPD
Device Brand of Device Drug Aerosol inhaler MDI Beclomethasone CFC free (QVAR) Beclomethasone CF free (Clenil Modulite) Fluticasone Ipratropium Salbutamol Salmeterol Seretide (Fluticasone / salmeterol combined) Flutiform (Fluticasone / formoterol combined) Sodium cromoglicate Autohaler Salbutamol Beclomethasone (QVAR) Easibreathe Beclomethasone Salbutamol Dry powder inhaler Accuhaler Fluticasone Salbutamol Salmeterol Seretide (Fluticasone / salmeterol combined) Handihaler Tiotropium Respimat Tiotropium Turbohaler Budesonide Formoterol Symbicort (Budesonide / eformoterol combined) Terbutaline Nebuliser Budesonide Ipratropium Salbutamol Terbutaline
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 4 of 19 Date: 2.6.2014 Drug Formulary 3.1 Bronchodilators Adrenoceptor stimulants – short acting 1st Choice Salbutamol 2mg, 4mg tablets
Salbutamol 4mg, 8mg m/r/ capsules
Salbutamol 2mg/5ml syrup
Salbutamol 500mcg/ml injection
Salbutamol 5mg/5ml infusion solution
Salbutamol 100mcg/dose aerosol inhalation
Salbutamol 100mcg/dose AUTOHALER
Salbutamol 200mcg/dose Accuhaler
Salbutamol 2.5mg, 5mg nebules
2nd choice
Terbutaline 500mcg/dose turbohaler
Terbutaline 500mcg/ml injection
Dose
- Salbutamol aerosol inhalation or breath-actuated aerosol inhalation, 100micrograms/puff: 100- 200 micrograms; persistent symptoms up to 3-4 times daily; prophylaxis in exercise-induced bronchospasm, 200 micrograms. - Salbutamol DPI: Ventolin Accuhaler®, 200micrograms; persistent symptoms, up to 4 times daily; prophylaxis in exercise-induced bronchospasm, 200micrograms. Asmasal Clickhaler® 95micrograms/puff: acute bronchospasm, 1-2 puffs; persistent symptoms, 2 puffs 3-4 times daily; prophylaxis in exercise-induced bronchospasm, 2 puffs. - Salbutamol nebuliser solution, 2.5mg or 5mg in 2.5mL; respirator solution 5mg/mL (20mL): chronic bronchospasm unresponsive to conventional therapy and severe acute asthma, 2.5-5mg up to 4 times daily. - Salbutamol injection 50micrograms/mL, 100micrograms/mL, 500micrograms/mL, 1mg/mL: subcutaneous or intramuscular injection, 500micrograms, repeated every 4 hours if necessary. Slow intravenous injection, 250micrograms repeated if necessary. Intravenous infusion, initially 5micrograms/minute, adjusted according to response and heart rate usually in range 3-20 micrograms/minute, or more if necessary.. - Terbutaline DPI: Turbohaler®, 500 micrograms (1 inhalation); for persistent symptoms up to 4 times daily. - Terbutaline injection 500micrograms/mL: subcutaneous, intramuscular or intravenous injection, 250-500micrograms up to 4 times daily. Continuous intravenous infusion: as solution containing 3- 5micrograms/mL, 1.5-5micrograms/minute for 8-10 hours.
Prescribing notes
There is virtually no difference in efficacy between salbutamol and terbutaline; currently salbutamol is cheaper and available in a wider range of devices. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 5 of 19 Date: 2.6.2014 Drug Formulary Inhalation is preferred to oral administration because it provides more rapid relief and causes fewer side-effects.
Short-acting beta2-agonist bronchodilators should only be prescribed on a "when required" basis for rescue therapy.
Patients with asthma using a short-acting beta2-agonist bronchodilator once or more per day should have their asthma control re-assessed.
Adrenoceptor stimulants – long acting
Salmeterol 25mcg/dose aerosol inhalation
Salmeterol 50mcg/dose Accuhaler
Formoterol 6mcg/dose, 12mcg/dose turbohaler
Dose
- Salmeterol aerosol inhalation 25micrograms/puff; salmeterol DPI (Accuhaler® 50micrograms/blister): 50 micrograms twice daily; up to 100 micrograms twice daily in more severe airways obstruction. - Formoterol DPI: Oxis Turbohaler® 6 or 12 micrograms/inhalation, 6-12micrograms once or twice daily increased to 24micrograms twice daily in more severe airways obstruction. For short-term symptom relief (but not acute asthma), additional doses may be taken to a total max 72micrograms daily (max single dose 36 micrograms); reassess treatment if additional doses required on more than 2 days a week.
Prescribing notes
In patients with asthma, long-acting beta2-agonists should only be prescribed when they are already receiving inhaled corticosteroids.
There is a risk of inadvertent monotherapy with long-acting beta2-agonist bronchodilators in
patients with asthma. It is recommended that a combination (steroid and long-acting beta2- agonist) inhaler is considered in patients who may have poor compliance to treatment regimens.
Antimuscarinic bronchodilators Ipratropium bromide 20mcg/dose aerosol inhalation
Ipratropium bromide 250mcg, 500mcg nebules
Tiotropium 18 microgram handihaler
Tioptropium 2.5 microgram inhaler (Respimat®)
Dose - Ipratropium bromide aerosol inhalation 20micrograms/puff: 20-40 micrograms, in early treatment up to 80 micrograms at a time, 3-4 times daily. - Ipratropium bromide nebuliser solution 250 micrograms in 1mL, 500micrograms in 2mL: usually Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 6 of 19 Date: 2.6.2014 Drug Formulary 250-500 micrograms up to 4 times daily; dilution of solution is adjusted according to equipment and length of administration; due to risk of paradoxical bronchospasm, first dose should be inhaled under medical supervision. - Tiotropium capsule 18micrograms: by inhalation of powder using HandiHaler®, 18micrograms daily. - Tiotropium inhaler 2.5micrograms: by inhalation using Respimat®, 5micrograms daily.
Prescribing notes
The principal role of regular inhaled ipratropium is in the management of COPD. Tiotropium is only licensed for COPD.
For maximum benefit, ipratropium should be administered 4 times daily.
Tiotropium is not suitable for the relief of acute bronchospasm and must not be given in combination with ipratropium. Patients with very severe COPD who are receiving regular home nebulisers should not be prescribed tiotropium in addition. MHRA Drug Safety Update Tiotropium: safety studies of Spiriva (Respimat®)
Article date: November 2010 Summary Recent analyses found that Spiriva Respimat was associated with a non-significant increase in all-cause mortality compared with placebo. By contrast, Spiriva HandiHaler was associated with a decrease in all-cause mortality compared with placebo. The underlying reasons for the apparent difference are unclear, and may be a chance finding; further studies are ongoing. Spiriva Respimat should be used with caution in patients with known cardiac rhythm disorders.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON099869
MHRA Drug Safety Update
Long-acting β2-agonists: reminder for use in children and adults
Article date: September 2010 Summary
Following a previous review in 2007 of long-acting β2-agonists (LABA) in the treatment of adults, adolescents, and children with asthma, we have further reviewed the use of LABA, specifically in children younger than age 12 years. All available data on the use of LABA in the treatment of asthma in children were reviewed, and it was concluded that the benefits of these medicines used in conjunction with inhaled corticosteroids (ICS) in the control of asthma symptoms in children outweigh any apparent risks.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON093845
Theophylline Aminophylline 225mg, 350mg s/r tablets (Phyllocontin®)
Aminophylline 250mg/10ml injection
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 7 of 19 Date: 2.6.2014 Drug Formulary Theophylline 175mg & 250mg tablets (Nuelin® SA)
Theophylline 200mg, 300mg, 400mg m/r tablets (Uniphyllin®)
Theophylline 60mg, 125mg, 250mg s/r capsules (Slo-Phyllin®)
Dose
- Uniphyllin Continus® tablets m/r 200mg, 300mg, 400mg: 200mg every 12 hours increased after 1 week to 300mg every 12 hours; over 70kg, 200-300mg every 12 hours increased after 1 week to 400mg every 12 hours. May be appropriate to give larger evening or morning dose to achieve optimum therapeutic effect when symptoms most severe; in patients whose night- or daytime symptoms persist despite other therapy, who are not currently receiving theophylline, total daily requirement may be added as single evening or morning dose. - Aminophylline 25mg/mL injection: deteriorating acute severe asthma not previously treated with theophylline, by slow intravenous injection over at least 20 minutes, 250-500 mg (5mg/kg) then as for acute severe asthma. Acute severe asthma, by intravenous infusion 500micrograms/kg/hour, adjusted according to plasma-theophylline concentration. Note: patients taking oral theophylline or aminophylline should not normally receive a bolus or loading dose but could receive the infusion dose ideally guided by plasma levels.
Prescribing notes
Theophylline is a bronchodilator used for reversible airways obstruction, which may have an
additive effect when used with small doses of beta2-adrenoceptor stimulants; this combination may increase the risk of side-effects including hypokalaemia.
Theophylline has a narrow margin between therapeutic and toxic effects; therapy should be monitored.
Different brands of modified-release theophylline have different bioavailability; the brand to be dispensed must be specified. Uniphyllin Continus® has been selected on basis of uniformity of drug release and cost; patients maintained on other theophylline preparations need not be changed.
Intravenous aminophylline is not a recommended drug in primary care having been
superceded by nebulised beta2-agonists.
Theophylline and aminophylline interact with many drugs; see BNF for details.
Smoking cessation may increase theophylline levels, this is independent of any nicotine replacement therapies that may be prescribed.
Older Patients - Theophylline preparations
Theophylline preparations are best avoided due to increased potential for drug interactions and risk of arrhythmia.
3.1.5 Peak flow meters, inhaler devices and nebulisers Aerochamber Plus standard Volumatic Paediatric Volumatic Peak flow meter (Ferraris low range) Peak flow meter (mini-wright standard) Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 8 of 19 Date: 2.6.2014 Drug Formulary Haleraid
Prescribing notes Measurement of peak flow is helpful for patients who are unable to detect deterioration in their asthma, and for those with moderate or severe asthma. Mini-Wright® and Vitalograph® peak flow meters are the most commonly prescribed.
New peak flow meters (identified by EU or CE marks) give different readings compared to old meters. These readings need to be interpreted using new published predicted equations (see www.airwaysextra.com/AJJune2004-Miller-published.pdf).
Spacer devices may be useful for patients with poor inhalation technique, children, and for those prone to oral candidiasis with inhaled steroids. They should be prescribed for patients receiving high dose steroids (>800micrograms/day of beclometasone or budesonide).
Local advice is that patients should inhale from the spacer device using a single breath with 5-10second breath hold.
Spacers should be cleaned no more than monthly with water and washing-up liquid, and allowed to air dry. More frequent cleaning affects their performance due to build up of static.
Nebulisers are not currently prescribable in general practice; patients should be referred for respiratory assessment. A spacer should be tried before considering a nebuliser. All nebulisers should be serviced regularly. However, difficulties are often encountered in the servicing of privately owned nebulisers. Aerochamber Plus®, and Volumatic®, and should be replaced every 12 months following regular use.
Compatible spacers for different MDIs
Drug Brand of MDI Compatible spacer(s) Airomir® AeroChamber® Plus Salbutamol Salbulin® Volumatic® Ventolin® Volumatic® Salmeterol Serevent® Volumatic® Becloforte® Volumatic® Becotide® Volumatic® Beclometasone QVAR® Aerochamber® Plus Clenil Modulite® Voumatic® AeroChamber® Plus Beclometasone + formoterol Fostair®
Fluticasone Flixotide® Volumatic® Fluticasone + Seretide® Volumatic® Salmeterol AeroChamber® Plus Fluticasone + formoterol Flutiform®
Ipratropium Atrovent® AeroChamber® Plus
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 9 of 19 Date: 2.6.2014 Drug Formulary 3.2 Corticosteroids
Beclometasone 50mcg, 100mcg aerosol inhalation and Easi-breathe (QVAR®)
Beclometasone 50mcg, 100mcg, 200mcg aerosol inhalation (Clenil Modulite®)
Budesonide 100mcg, 200mcg, 400mcg/dose turbohaler
Budesonide 500mcg/2ml, 1mg/2ml respules
Fluticasone 50mcg, 125mcg, 250mcg/dose aerosol inhalation
Fluticasone 50mcg, 100mcg, 250mcg, 500mcg/dose Accuhaler
Seretide® (Fluticasone/Salmeterol) 250mcg, 500mcg/dose Accuhaler
Seretide® (Fluticasone/Salmeterol) 50mcg, 125mcg, 250mcg/dose Evohaler
Symbicort® (Budesonide/Formoterol) 100/6, 200/6, 400/12 dose Turbohaler
Flutiform® (Fluticasone/Formoterol) 50microgram/5microgram, 125microgram/5microgram, 250microgram/10microgram aerosol inhalation (FOR ASTHMA ONLY)
Dose - Beclometasone Qvar® aerosol inhalation 50micrograms/puff, 100micrograms/puff,; breath-actuated aerosol inhalation 50micrograms/puff, 100micrograms/puff: 200micrograms twice daily; in more severe cases 400micrograms twice daily. - Budesonide aerosol inhalation 50micrograms/puff, 200micrograms/ puff; Turbohaler® DPI 100micrograms, 200micrograms or 400micrograms per inhalation: 100- 800micrograms twice daily by aerosol or dry powder inhalation. - Budesonide nebuliser solution 500micrograms or 1mg in 2mL: 1-2mg twice daily (may be increased further in very severe asthma). - Fluticasone aerosol inhalation 25micrograms, 50micrograms, 125micrograms or 250micrograms per puff: 100-250 micrograms twice daily, increased according to severity of asthma to 1mg twice daily. - Fluticasone DPI (Accuhaler®) 50micrograms, 100micrograms, 250micrograms or 500micrograms per blister: 100-250 micrograms twice daily, increased according to severity of asthma to 1mg twice daily. - Flutiform® aerosol inhalation(containing fluticasone propionate 50micrograms, 125micrograms or 250micrograms with formoterol 5microgram or 10microgram/puff): asthma, by aerosol inhalation, 2 puffs twice daily. - Seretide Evohaler® (containing fluticasone propionate 50micrograms, 125micrograms or 250micrograms with salmeterol 25micrograms/puff): asthma, by aerosol inhalation, 2 puffs twice daily. - Seretide Accuhaler® (containing fluticasone propionate 100micrograms, 250micrograms or 500micrograms with salmeterol 50micrograms/blister): asthma, by inhalation of powder, 1 blister twice daily. COPD, by inhalation of powder, 1 blister of Seretide 500 Accuhaler® twice daily. - Symbicort Turbohaler® (Symbicort® 100/6 equivalent to budesonide 100micrograms with formoterol 6micrograms/puff; Symbicort® 200/6 equivalent to budesonide 200micrograms with formoterol 6micrograms/puff; Symbicort® 400/12 equivalent to budesonide 400micrograms with formoterol 12micrograms/puff): asthma, Symbicort® 100/6 and 200/6, by inhalation of powder, 1-2 puffs twice daily. May be reduced in well- controlled asthma to 1-2 puffs once daily. Symbicort® 400/12, by inhalation of powder, 1 puff twice daily, titrated to the lowest effective dose which may be given once daily. COPD, Symbicort® 200/6, 2 puffs twice daily. COPD, Symbicort® 400/12, 1 puff twice daily. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 10 of 19 Date: 2.6.2014 Drug Formulary Prescribing notes
When switching patients to CFC-free beclmetasone QVAR devices the dose may not be equipotent (see General Notes)
At doses greater than 800micrograms daily of beclometasone, a spacer device should also be used.
Patients receiving more than 1500micrograms daily of beclometasone or budesonide (or 750micrograms of fluticasone) may have some systemic effects and should be given a steroid card.
Patients on high doses of inhaled steroids (more than 1000micrograms/day of beclometasone dipropionate or equivalent) who receive more than three to four courses of oral steroids per year should be considered for bone protection.
Asthma guidelines suggest patients may do better with moderate doses of steroid (400-
800micrograms beclometasone dipropionate) plus a long-acting beta2-adrenoceptor stimulant rather than increasing the steroid dose.
When considering doses, beclometasone dipropionate (except when prescribed as Qvar®) and budesonide are equipotent and fluticasone is twice as potent (see BTS guidelines).
Inhaled corticosteroids for COPD should only be prescribed for patients with an FEV1 of 50% predicted or less, who have two or more exacerbations needing treatment with antibiotics or oral corticosteroids a year.
Ideally, in asthma, Seretide® (and Symbicort®) should be used when salmeterol (or formoterol) and inhaled steroids have been given separately before, and patients are stable on established doses. They can be a cost-effective alternative to the individual products and are more convenient to use.
Seretide Accuhaler® is designed to be administered as 1 blister per dose, in contrast to Evohaler® which should be administered as 2 puffs of the appropriate inhaler strength.
Problems with oral candidiasis may be reduced by advising patients to take the evening dose of inhaled steroid before their evening meal.
Clinicians should be aware that higher doses of inhaled steroids may be needed in patients who are smokers/ex-smokers.
Fostair®, licensed for use in asthma, is a combination inhaler (beclometasone dipropionate 100micrograms and formoterol fumarate 6micrograms). In this inhaler the beclometasone is an extrafine particle and therefore is more potent than Clenil Modulite®. Beclometasone dose 100micrograms in Fostair® is equivalent to 250micrograms in Clenil Modulite®. Fostair® cannot provide the high dose inhaled corticosteroid doses that are required for Step 4 (of the BTS guidelines) asthma management, therefore patients will require an alternative inhaler prescribed.
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 11 of 19 Date: 2.6.2014 Drug Formulary MHRA Drug Safety Update Inhaled and intranasal corticosteroids: risk of psychological and behavioural side effects
Article date: September 2010 Summary Psychological and behavioural side effects may occur in association with use of inhaled and intranasal formulations of corticosteroids.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON093853
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 12 of 19 Date: 2.6.2014 Drug Formulary 3.3 Cromoglicate, related therapy and leukotriene receptor antagonists
Montelukast 10mg tablets
Montelukast 4mg chewable tablets
Montelukast 5mg chewable tablets
Montelukast 4mg sachets
Dose
- Montelukast tablets 10mg: 10mg at bedtime.
Prescribing notes
Sodium cromoglicate has largely been superceded by inhaled corticosteroids but may have a role in some individuals as add-on therapy or with exercise-induced asthma.
Montelukast is indicated for add-on therapy in mild-moderate persistent asthma, and to prevent exercise-induced bronchospasm.
If montelukast is prescribed between steps 2 and 3 of the BTS guidelines (see BNF), symptoms and peak expiratory flow should be monitored and treatment stopped if there is no demonstrative benefit within 4 weeks.
Leukotriene receptor antagonists should not be used to relieve an attack of acute severe asthma.
Montelukast should be taken at bedtime; those patients that experience sleep disturbances will still get a clinical benefit by switching the dose to the morning.
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 13 of 19 Date: 2.6.2014 Drug Formulary 3.4 Antihistamines, hyposensitisation, and allergic emergencies Sedating antihistamines 1st Choice Chlorphenamine/Chlorpheniramine 4mg tablets
Chlorphenamine/Chorpheniramine 10mg/ml injection
Chlorphenamine/Chlorpheniramine 2mg/5ml syrup
Alternative
Alimemazine/Trimeprazine 7.5mg/5ml, 30mg/5ml syrup, 10mg tablets
Promethazine 50mg/2ml injection
Promethazine 10mg, 25mg tablets
Promethazine 5mg/5ml elixir
Hydroxyzine 10mg/5ml syrup
Hydroxyzine 10mg, 25mg tablets Non-sedating antihistamines Loratidine 5mg/5ml syrup
Loratidine 10mg tablets
Cetirizine 10mg tablets
Cetirizine 5mg/5ml solution
Fexofenadine 120mg, 180mg tablets
Dose - Cetirizine tablets 10mg; solution 5mg/5ml: 10mg daily or 5mg twice daily. - Chlorphenamine tablets 4mg; syrup 2mg/5mL; injection 10mg/mL: orally, 4mg every 4-6 hours, max 24mg daily. Subcutaneous or intramuscular injection: 10-20mg repeated if required, max 40mg in 24 hours. Slow intravenous injection: 10-20mg over 1 minute. - Loratadine tablets 10mg: 10mg daily. - Hydroxyzine tablets 10mg,25mg; syrup 10mg/5ml: 25mg at night, increased if necessary to 25mg 3-4 times daily. - Fexofenadine tablets 120mg, 180mg: 120-180mg once a day. Prescribing notes
Antihistamines may be of value in the treatment of nasal allergies, especially hay fever, and vasomotor rhinitis. They reduce rhinorrhoea and sneezing but are usually less effective for nasal congestion.
Oral antihistamines are of value in preventing urticaria and are used to treat urticarial rashes, pruritus, and insect bites and stings; they are also used in drug allergies.
Cetirizine and loratadine cause less sedation than chlorphenamine but are more expensive; they are available over-the-counter.
Loratadine may be a suitable alternative for patients who develop sedation with cetirizine.
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 14 of 19 Date: 2.6.2014 Drug Formulary First choice preparation for allergic rhinitis is beclometasone nasal spray.
Older Patients - Antihistamines
Chlorphenamine is more liable to cause drowsiness in older patients.
Allergic emergencies Adrenaline/Epinephrine 1 in 1000 injection
Adrenaline/Epinephrine 1 in 10,000 injection
Adrenaline/Epinephrine 300microgram/0.3ml autoinjector (Jext®)
Adrenaline/Epinephrine 150microgram/0/3ml autoinjector (Jext®)
Adrenaline/Epinehrine 1 in 100 000 (Unlicensed – A&E only)
Hydrocortisone sodium succinate 100mg injection (Solu-Cortef)
Dose
- Adrenaline 1 in 1000 (1mg/mL) injection: intramuscularly, 0.5mL repeated if necessary at 5- minute intervals according to blood pressure, pulse and respiratory function. - Adrenaline for self-administration: Jext® Auto-injector 0.3mg consists of a fully assembled syringe and needle delivering adrenaline 300micrograms by intramuscular injection; repeated after 15 minutes as necessary. - Chlorphenamine injection 10mg/mL: 10-20mg by slow intravenous injection over 1 minute. - Hydrocortisone sodium succinate injection 100mg: 100-300mg intravenously.
Prescribing notes
Adrenaline should be given immediately for an acute anaphylactic reaction (laryngeal oedema, bronchospasm and hypotension).
Chlorphenamine injection is a useful adjunctive treatment given after adrenaline injection and continued for 24-48 hours to prevent relapse.
Hydrocortisone injection is of secondary value in the initial management of anaphylactic shock because the onset of action is delayed for several hours, but should be given to prevent further deterioration in severely affected patients.
Atopic individuals are particularly at risk of anaphylactic reactions; patients with known severe allergy to insect stings, foods or peanuts should carry, and receive instruction for the use of, prefilled syringes (e.g. Jext®) for self-administration. Patients should usually be prescribed two.
Adrenaline for self-administration should be prescribed by brand name to ensure that the patient gets the device that they have been taught to use.
Jext® and Epipen® (the previous formulary choice) are very similar in device design and are administered in a similar way. If changing a patient from Epipen® to Jext® ensure that they patient is aware of how to use the new device.
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 15 of 19 Date: 2.6.2014 Drug Formulary MHRA Drug Safety Update Adrenaline auto-injector advice for patients: after every use, an ambulance should be called even if symptoms are improving, the individual should lie down with legs raised and, if at all possible, should not be left alone
Article date: May 2014 Summary People who have been prescribed an adrenaline auto-injector because of the risk of anaphylaxis should carry two with them at all times for emergency, on-the-spot use. After every use of an adrenaline auto-injector, an ambulance should be called (even if symptoms are improving), the individual should lie down with their legs raised and, if at all possible, should not be left alone..
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON418520
3.4.2 Allergen immunotherapy
Omalizumab 150mg and 300mg injection
Dose
- Omalizumab 150mg, 300mg injection: consult product literature.
MHRA Drug Safety Update Omalizumab: potential risk of arterial thrombotic events
Article date: February 2011 Summary Use of omalizumab may be associated with an increased risk of arterial thrombotic events. Prescribers should be vigilant for possible thrombotic adverse reactions, and should report these events to us promptly via the Yellow Card Scheme.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON108685
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 16 of 19 Date: 2.6.2014 Drug Formulary 3.5 Respiratory stimulants and pulmonary surfactants Respiratory stimulants Doxapram 100mg/5ml injection
Caffeine 5mg/ml injection Pulmonary surfactants Poractant alfa 80mg/ml injection(Curosurf)
MHRA Drug Safety Update Caffeine for apnoea of prematurity: all products to be named and prescribed as caffeine citrate
Article date: August 2013 Summary In order to minimise potential risk to premature newborns when prescribing or dispensing, the name of caffeine products supplied by Viridian Pharma Limited is being changed to caffeine citrate. This change brings the Viridian products in line with the naming of other products available on the UK market (ie, which are already named in the salt form as caffeine citrate). All product doses should be prescribed as caffeine citrate, taking into account the different strengths of the marketed products.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON300399
3.7 Mucolytics
Carbocisteine 375mg capsules
Carbocisteine 250mg/5ml oral liquid
Sodium chloride 7% nebuliser solution (Nebusal®)
Dose
- Carbocisteine capsules 375mg; oral liquid 250mg/5ml: initially 750mg three times daily, then 1.5g daily in divided doses as condition improves.
Prescribing notes
Carbocisteine should be prescribed in accordance with local GMMC COPD Treatment Guideline.
Nebulised sodium chloride may be used in hospital for bronchiectasis.
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 17 of 19 Date: 2.6.2014 Drug Formulary 3.8 Aromatic Inhalations
Benzoin compound tincture (Friars Balsam)
Prescribing notes
Inhalations are traditionally used and although the vapour may contain little of the additive it encourages inspiration of warm moist air which can be of help in bronchitis, acute rhinitis and sinusitis.
Boiling water should not be used owing to the risk of scalding.
3.9 Cough preparations Cough suppressants Pholcodine 5mg/5ml linctus (sugar free)
Codeine 15mg/5ml linctus Demulcent cough preparations
Simple linctus (sugar free)
Prescribing notes
There is little evidence to support the use of cough suppressants.
For persistent cough lasting 4-6 weeks, the underlying cause should be established.
MHRA Drug Safety Update Codeine-containing liquid over the counter medicines: should not be used for cough in under 18 years
Article date: October 2010 Summary The Commission on Human Medicines and its Paediatric Medicines Expert Advisory Group have advised that codeine-containing OTC liquid medicines should not be used for cough suppression in children and young people younger than age 18 years.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON096805
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 18 of 19 Date: 2.6.2014 Drug Formulary 3.10 Systemic nasal decongestants
Pseudoephedrine 60mg tablets
Pseudoephedrine 30mg/5ml elixer
Prescribing notes
Systemic decongestants should be used with caution in diabetes, hypertension, hyperthyroidism, raised intra-ocular pressure, prostate hypertrophy, hepatic impairment, renal impairment, ischaemic heart disease, and avoided in patients taking monoamine oxidase inhibitors.
MHRA Drug Safety Update Pseudoephedrine and ephedrine: update on managing risk of misuse
Article date: October 2012 Summary Implementation of measures to regulate sales, together with the additional voluntary actions overseen by the profession, has made an important contribution to managing the risk of misuse of pseudophedrine and ephedrine. The CHM recommended that existing levels of monitoring, education, and awareness measures by pharmacists should be maintained.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON199567
Drug Safety Update 3.10 Antifibrotics Pirfenidone
Prescribing notes
Pirfenidone approved in line with NICE TAG. Noted only available via clinics approved by NHS England Specialised Commissioning.
Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 19 of 19 Date: 2.6.2014 Drug Formulary