Chapter 21 - Assessment of Respiratory Assessment
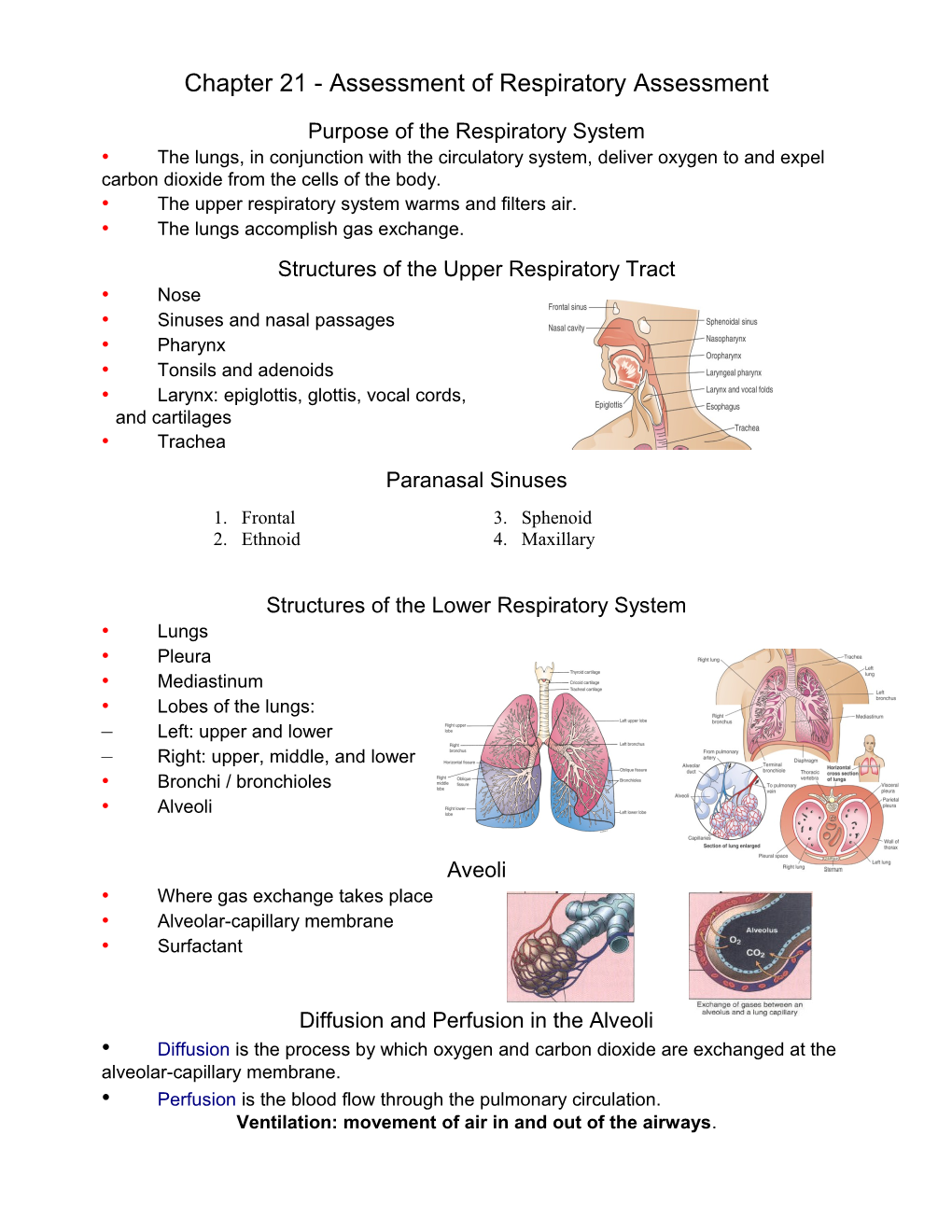
Purpose of the Respiratory System • The lungs, in conjunction with the circulatory system, deliver oxygen to and expel carbon dioxide from the cells of the body. • The upper respiratory system warms and filters air. • The lungs accomplish gas exchange. Structures of the Upper Respiratory Tract • Nose • Sinuses and nasal passages • Pharynx • Tonsils and adenoids • Larynx: epiglottis, glottis, vocal cords, and cartilages • Trachea Paranasal Sinuses 1. Frontal 3. Sphenoid 2. Ethnoid 4. Maxillary
Structures of the Lower Respiratory System • Lungs • Pleura • Mediastinum • Lobes of the lungs: – Left: upper and lower – Right: upper, middle, and lower • Bronchi / bronchioles • Alveoli
Aveoli • Where gas exchange takes place • Alveolar-capillary membrane • Surfactant
Diffusion and Perfusion in the Alveoli • Diffusion is the process by which oxygen and carbon dioxide are exchanged at the alveolar-capillary membrane. • Perfusion is the blood flow through the pulmonary circulation. Ventilation: movement of air in and out of the airways. • The thoracic cavity is an airtight chamber. • The floor of this chamber consists of the diaphragm. • Upon Inspiration: the diaphragm contracts (moves this chamber floor downward) and contraction of the external intercostal muscles increases the space in this chamber. • The expansion of space lowers the intrathoracic pressure (negative pressure) causing air to enter through the airways and inflate the lungs.
Ventilation: movement of air in and out of the airways • Expiration: diaphragm relaxes, the diaphragm moves up and intrathoracic pressure increases. • This increased pressure pushes air out of the lungs. • Expiration requires the elastic recoil of the lungs. • Inspiration normally is 1/3 of the respiratory cycle and expiration is 2/3.
Respiration • The process of gas exchange between atmospheric air and the blood at the alveoli, and between the blood cells and the cells of the body. • Exchange of gases occurs because of differences in partial pressures. • Oxygen diffuses from the air into the blood at the alveoli to be transported to the cells of the body. • Carbon dioxide diffuses from the blood into the air at the alveoli to be removed from the body.
Gas Exchange and Respiratory Function Ventilation/Perfusion (V/Q Ratio) • Ventilation is the movement of air in and out of the lungs. • Air must reach the alveoli to be available for gas exchange. • Perfusion is the filling of the pulmonary capillaries with blood. • Adequate gas exchange depends upon an adequate V/Q ratio, a match of ventilation and perfusion. • Shunting occurs when there is an imbalance of ventilation and perfusion. This results in hypoxia. What affects the Ventilation-Perfusion Ratios?
A- Normal Ratio B- Shunts C- Dead Space D- Silent Unit
Assessment of Breath Sounds • Normal breath sounds: (Table 21-5, p 575) • Vesicular – soft, relatively low sounds, sounds are longer during inspiration Heard over entire lung field except over the upper sternum & between scapulae • Bronchovesicular – intermediate sound, inspiration & expiration are equal Often heard in the anterior 1st & 2nd intercostals spaces and between the Scapulae (over the main bronchus) • Bronchial - loud and relatively high sounds, expiration sounds last longer than inspiration. Heard over the manubrium, if heard at all. - Tracheal sounds – heard over the trachea in the neck area. They are very loud, & relatively high. Inspiration & expiration are equal
Breathing Patterns p 572
During inspiration, the thoracic cavity must have a lower pressure than the atmosphere. Eupnea – normal respiration Bradypnea – slow breathing rate, < 10 breaths/min. normal depths and regular rhythm Tachypnea – rapid, shallow breathing, > 24 breaths/min. Hypoventilation – shallow, irregular breathing Hyperventilation – increase breathing rate & depth of breathing Called Kussmaul’s respiration when caused by a metabolic disorder (diabetic ketoacidosis) Apnea – periods of breathing cessation, time duration varies: dependent upon disorder that is causing it: (sleep apnea). Life threatening conditions if breathing is sustained Cheyne-Stokes – regular cycles of alternating rapid breathing with periods of apnea (20 sec). Biot’s respiration – periods of normal breathing (2-4 breaths) followed by varying periods of apnea lasting 10-60 seconds. Seen in patients with increase CP Breath Sounds • Abnormal (adventious) breath sounds: (Table 21-5, p 575) • Crackles (formerly called rales) • Wheezes (includes rhonchi) • Friction rubs (a form of crackles) _ Bronchopony, Egophony and Whipered pectoriloquy REVIEW
Function of Respiratory System - Oxygen transport Supplies oxygen to and CO2 is removed from cells via the blood Occurs by diffusion - Respiration Breathing is regulated by the medulla oblongata in the brain After diffusion takes place, blood returns through the veins to the pulmonary system At the alveoli, the CO2 moves out of the blood. Oxygen moves from the alveoli into the blood. This is called respiration - Pulmonary system is considered a low pressure system (systolic 20-30, diastolic 5-15) - Pulmonary artery pressure, gravity, alveolar pressure determine the patterns of perfusuion. Gas Exchange CO2 and O2 are exchanged at the alveoli Oxygen diffuses across the alveolar memebrane to dissolve in blood until the oc pressure is the same in the blood as it is in the alveoli CO2 is in venous blood is at a higher concentration than the alveolar gasses, so in the lung, CO2 diffuses from the venous blood into the alveolar gases until the pressure is the same. O2 is carried in the blood by plasma and hemoglobin o The amt. Of O2 dissovled in the plasma varies with partial pressure of O2 in the arterires (PaO2). Norma PaO2 = 80-100 Lung Volumes & Capacities: (p.558) Lung function reflects mechanic of ventilation in view of the lung volumes & capacities. Lung Volume • Tidal volume (TV): air volume of each full breath • Inspiratory reserve volume (IRV): maximum volume of air that can be inhaled after a normal inhalation • Expiratory reserve volume (ERV): maximum volume of air exhaled after a normal exhalation. • Residual volume – is the vol. Of air remaining in the lungs after a maximum exhalation Lung Capacity • Vital capacity (VC): the max. vol. of air exhaled from a maximal inspiration, VC = TV + IRV + ERV • Inspiratory capacity – max. vol. of air inhaled after normal expiration • Functional residual capacity (FRC) – vol. of air remaining in the lungs after normal Expiration. FRV = ERV + RV • Total lung capacity (TLC) - vol. of air in lungs after mx. Inspiration Forced expiratory volume (FEV): volume exhaled forcefully over time in seconds. Time is indicated as a subscript, usually 1 second.
Measurement of Volume and Inspiratory Force • A spirometer measures volumes of air exhaled and is used to assess lung capacities. • Measure several breaths when assessing total volume. TV varies from breath to breath. • Pulmonary function tests assess respiratory function and determine the extent of dysfunction. • Peak flow rate reflects maximal expiratory flow and is frequently done by patients using a home spirometer. Inspiratory Force • Evaluates the effort of the patient in making an inspiration. • A manometer that measures inspiratory effort can be attached to a mask or endotracheal tube to occlude the airway and measure pressure. • Normal inspiratory pressure is approximately 100 cm H2O. • Force of less than 25 cm usually requires mechanical ventilation. Arterial Blood Gases • Measurement of arterial oxygenation and carbon dioxide levels. • Used to assess the adequacy of alveolar ventilation and the ability of the lungs to provide oxygen and remove carbon dioxide. • Also assesses acid-base balance Symbols for pressure gasses on p. 560-561 S/B book.
Pulse Oximetry • A noninvasive method of measuring the oxygen saturation of the hemoglobin. • Does not replace ABGs • Normal level is 95-100%. If <85% the tissue is not receiving adequate O2 • May be unreliable some situations Diagnostic Tests • Pulmonary function tests • Arterial blood gases • Sputum culture tests – collected to determine if pathogens or malignant cells are present.. Expectoration is theusual method of collecting sputum. Imaging studies: • Chest x-ray • Computed tomography (CT) • Magnetic resonance imaging (MRI) • Fluoroscopic studies and angiography • Radioisotope procedures (lung scans) Diagnostic Tests • Bronchoscopy – endoscopic procedure for direct visualization and inspection of the larynx, trachea, bronchi, done through a scope. • Used to examine tissue, obtain biopsy, excise lesions, determine if surgery is possible, and remove foreign objects. • Sedation is given; consent form required Fiberoptic Bronchoscopy • NPO after procedure until gag reflex returns
• Thoracoscopy – examination of the pleural cavity through endoscopy. Used for evaluation of pleural effusion, staging of tumors. (similar to laproscopic procudure) Rigid Bronchoscopy
• Biopsies – excision of a small amt. of tissue for examination • Pleural biopsy – biopsy of the pleural done by a needle • Lung biopsy – done by bronchoscopy or needle biopsy • Lymph node biopsy = scalene lump nodes are in the neck and drain the lungs and mediastinum Changes indicate thoracic diseases: Hodgkin’s, TB, CA, fungal disease Position of a Patient for Thoracentesis Endoscopic Thoracoscopy
RESPIRATORY ASSESSMENT Assessment LOC – be alert for LOC level of concsciousness: alert, confused, unresponsive. Look for changes: lethargy, agitation, inc.anxiety, somnolence, confusion, irritability Health history focused on physical and functional problems o Usually seeking health care for dyspnea, pain, accumulation of mucus, wheezing, hemoptysis, edema of the feet, fatigue, weakness Look for Signs & Symptoms of dyspnea, orthopnea, cough o Major s/sx – dyspnea, sputum production, chest pain, wheezing, clubbing of fingers, hemoptysis, cyanosis Clubbing of nails, sign of lung disease found in pts. with chronic hypoxic conditions Sputum and hemoptysis – expectoration of blood from the respiratory tract and is a symptom of both resp. and cardiac disorders. Most common causes are: o Pulmonary infections, lung CA, heart or blood vessel abnormalities, pulmonary artery or vein abnormalities, pulmonary emboli or infart. Assessment Patient’s position – are they trying to compensate LOC – be alert for LOC level of consciousness: alert, confused, unresponsive. Look for changes: lethargy, agitation, inc. anxiety, somnolence, confusion, irritability Skin – inspect under natural light. Beware! Fluorescent light – doesn’t show true skin color Cyanosis – a bluish coloring of the skin; it’s a very late indicator of hypoxia Presence or absence is determined by amt. of deoxygenated hemoglobin in the blood Cyanosis appears when there is 5g/dL of unoxygenated hemoglobin A person with a hemoglobin of 15g/dL will not show cyanosis until 5g/dL of that becomes unoxygenated Anemic pts. rarely show cyanosis. Pts with Polycythemia may show cyanosis even if adequately oxygenated. They have a concentrated number of RBCs than the normal levels so when 5g/dL show cyanosis, they may still have enough RBCs carrying adequate (O2) oxygenation Cyanosis is not a reliable sign of hypoxia Assessment of cyanosis may be affected by room lighting, skin color, temperature of environment Central cyanosis (as in pulmonary conditions) is assessed by looking at the color of the tongue and lips. This indicates a decrease of oxygen tension of the blood. Peripheral cyanosis results from decreased blood flow to a certain area of the body, as in vasoconstriction of the nailbeds or earlobes from exposure to cold. Assessment Face – ck for signs of respiratory distress: nasal flaring - does he have O2, endotracheal tube, ck redness or exoriation neck – tracheal tube? How is the skin (infection?), Palpate for crepitus – air leaking into the subcutaneous tissue. Observe/palpate trachea for midline position – trachea deviation may indicate tension pneumothorax. Palpate for swelling, masses that might obstruct breathing. Assessment: Chest Configuration There are 4 main deformities of the chest associated with respiratory disease 1. barrel chest – occurs as a result of over inflation of the lungs. There is an increase in the anterior-posterior diameter of the thorax. In a pt with emphysema, the rigs are widely spaced at the intercostals spaces. Intercostal spaces tend to bulge on expiration. The appearance is quite characteristic of pts with advanced emphysema. 2. Funnel chest – occurs when there is depression of the lower portion of the sternum. This may compress the heart and great vessels, resulting in murmurs. Funnel chest may occur with rickets or Marfan’s syndrome. 3. Pegeon chest – displacement of the sternum. There is an increase in the anterior-posterior diameter. May occur with rickets, Marfan’s syndrome or severe kyphoscoliosis. 4. Kyphoscoliosis – Abnormal curvature of the spine characterized by an elevation of the scapula and a corresponding S-shaped spine. o Limits lung expansion within the thorax o May occur with osteoporosis, or other skeletal disorders Assessment Chest movement, are they using accessory mucles to breath? • Is there retraction of intercostals space during inspiration? A sudden violent retraction indicates airway obstruction or tension pneumothorax. • In COPD – muscles may retract during expiration as the pt forces air from the alveoli • Intercostal bulging may be seen with cardiac enlargement & aneurys, fx ribs and flail chest • Note expansion of chest – unequal thoracic expansion may indicate pleural effusion, atelectasis, pulmonary embolus, fx rib or sternum, or an endotracheal tube has been inserted too far & entered the Right mainstem broncus. Listen to Breath Sounds • Abnormal (adventious) breath sounds: (Table 21-5, p 575) • Crackles (formerly called rales) • Wheezes (includes rhonchi) • Friction rubs (a form of crackles) • Voice Sounds – vocal resonance heard through the stethoscope as pt speaks. (99 or ee) • Bronchopony – intense & clear vocal resonance than normal • Egophony – distorted voice sounds produced by consolidation (pneumonia) • Whipered pectoriloquy – a subltle sound heard only in dense consolidation p.576 Look at Breathing Patterns p 572 Eupnea – normal respiration Bradypnea – slow breathing rate, < 10 breaths/min. normal depths and regular rhythm Tachypnea – rapid, shallow breathing, > 24 breaths/min. Hypoventilation – shallow, irregular breathing Hyperventilation – increase breathing rate & depth of breathing Called Kussmaul’s respiration when caused by a metabolic disorder (diabetic ketoacidosis) Apnea – periods of breathing cessation, time duration varies: dependent upon disorder that is causing it: (sleep apnea). Life threatening conditions if breathing is sustained Cheyne-Stokes – regular cycles of alternating rapid breathing with periods of apnea (20 sec). Biot’s respiration – periods of normal breathing (2-4 breaths) followed by varying periods of apnea lasting 10-60 seconds. Seen in patients with increase CP Sputum Sputum indicates the reaction of the lung to any constant recurring irritant or to nasal discharge. Thick, viscous, frothy, mucoid, watery, or mucopurulent • Bacterial infection - indicated by a thick, yellow green, or rust colored sputum • Viral bronchitis - thin, mucoid sputum • Lung tumor - pink-tinged sputum • Pulmonary edema – profuse, frothy material often welling up in the throat • Lung abcess, Bronchiectasis – foul, smelling sputum and bad breath Bronchiectasis – chronic, irreversible dilation of the bronchi and bronchioles Sputum: Relief Measures • Decrease viscosity by increasing hydration (drink water) • Inhalation of awrosolized solutions • Stop smoking – it interferes with ciliary action, increases bronchila secrestions, causes inflammation, reduces surfactant. • Nutrition may be compromised due to smell or taste of sputum - Citrus juice before meals cleanses the palate and may make food more palatable Cough Timing; frequency- does it get worse, Chronic, Acute, Paroxysmal Productive – nonproductive; Dry - moist Barking, Hoarseness, Hacking Hemoptysis Blood tinged sputum • Review chest x-ray, chest angiography, bronchospcopy, medical history, physical. • Determine source of blood (gums, throat lungs, stomach) – From lungs – bright red, frothy – From nose or throat – usually preceded by sniffling, with blood possibly visible in the nose – From stomach – is it from vomiting or from coughing; dark “coffee grounds” color Clubbing • Sign of lung disease found in pts. with chronic hypoxic conditions, chronic lung infections, & malignancies. • Sponginess of nail beds with loss of nail-bed angle Chest Pain • Pain Associated with pulmonary or cardiac disease • May occur with pneumonia, P. emboli, lung infarction, pleurisy, cancer * Relief measures: analgesic, regional anesthetics, nonsteriodal anti- inflammatory drugs (NSAIDs) • Wheezing – airway narrowing heard mainly on expiration, but may be heard on both inspirations and expiration’ * Relief measures: oral or inhaled bronchodilators • Clubbing – sign of lung disease found in pts. c chronic hypoxic conditions, chronic lung infections, malignancies. - Sponginess of the nail beds with loss of nail-bed angle Thoracic Auscultation
• Adventitious sounds (additional) - produced by abnormal conditions that affect the bronchial tree and alveoli. – The duration of the sound is important in identifying the sound as non-continuous or continuous sounds • Divided into 2 types: – Discrete: non-continuous sounds (like crackles) – result from delayed re-opening of deflated airways – pleural friction rub is an example of crackles, usually heard on inspiration and expiration – Crackles used to be called rales – May or may not clear with coughing – May hear in pneumonia, bronchitis, heart failure, bronchiectasis, pulmonary fibrosis – Continuous, musical sounds (wheezes): associated with bronchial wall oscillations (vibrations) and changes in the diameter of the airways. (include rhonchi sounds) - usually heard in asthma, chronic bronchitis Assessing light to dark skin
Description Light skin Dark skin Cyanosis - bluish Bluish tinge Ashen gray
Pallor - paleness Loss of rosy glow Ashen gray (drk skin) Yellowish brown (brown skin)
Erythema - redness Visible redness Diffused; rely on palpation of warmth or edema
Petechiae – small size Purplish pinpoints Usually invisible; check oral Description Light skin Dark skin pinpoint ecchymosis mucosa, conjunctiva, eyelids, Jaundice - yellow Yellow sclera, skin, Reliableconjunctiva on sclera,covering hard eyeballs. palate, fingernails, soles, palms and soles. palms, oral mucosa
Ecchymosis – large Purplish to yellow- Difficult to see, check mouth diffused bluish black green or conjunctiva Brown-Tan – cortisol Bronze; Easily masked. deficiency, increased Tan to light melanin production brown Nursing 125 Pediatric Respiratory Problems Infants under 3 months have fewer respiratory infections probably because of protective maternal antibodies. The infection rate increases from 3 to 6 months. S/S Of Respiratory Infections In Infants & Small Children • Fever – may be absent in newborn; Greatest ages 6months-3yrs even /w mild infections. • Anorexia is common & often early sign; Vomiting may precede other signs by several hrs • Diarrhea usually mild 7 often accompanies viral respiratory infection • Abdominal pain is common complaint – Similar to appendicitis – Mesenteric lymphadenitis may be cause • Nasal blockage – interferes with breathing & feeding and can contribute to otitis media. • Nasal discharge, Cough, Sore throat Nursing Actions to Ease Respiratory Efforts • Ease respiratory effort, Rest, Comfort, Reduce fever • Prevent spread of infection, Promote hydration and Provide nutrition • Family support, teaching and home care. Acute Streptococcal Pharyngitis • Group a B-hemolytic (GABHS) strep throat – Not a serious infection itself but – Can lead to acute rheumatic fever or acute glomerulonephritis Assessment: • Brief illness, c/o headache, fever; Sudden onset. • Abdominal pain in small children.. Severity varies from subclinical to severe toxicity. • Inflamed tonsils and pharynx covered with exudate in 50 – 80% of cases. • Cervical lymphadenopathy. • Course of illness runs in 3 to 5 days. • Complications: Acute nephritis may occur in 10 days; and Rheumatic fever in 18 days. Acute Streptococcal Pharyngitis- Diagnostics • 80 –90% of sore throats are viral. • Throat culture should be done to rule out strep throat. • Some children harbor streptococci in their throats so a positive culture does not always mean that the infection is strep. Acute Streptococcal Pharyngitis – Treatment • Penicillin for 10 days • Cefdinir for 5 days combination of penicillin and rifampin • Obtain throat swab. • Teach parents of importance of having child take antibiotics as instructed. • Encourage bedrest; Warm or cold compressed to the neck. Acute Streptococcal Pharyngitis – Nursing Care • Warm saline gargles; Cool liquids or ice chips. • Child becomes noncontagious 24 hours after being on antibiotics. • Child should discard toothbrush after being on antibiotics for 24 hours to prevent reinfection. Croup Syndromes • Croup – broad classification of upper airway illnesses that result from swelling of the epiglottis and larynx.. The swelling usually extends to the trachea and bronchi. • It is characterized by hoarseness; barking, brassy or croupy cough and Inspiratory stridor • Infants and small children have a much smaller diameter of airway and infection here results in significantly narrowed airway. • More common in boys; in children 6 months to 3 years of age, especially 2 years of age • Occurs late autumn to early winter • Hospitalization needed for 1 to 15% of children Described according to the primary anatomic area affected 1. Epiglotitis 2. Laryngitis 3. Laryngotracheobronchitis (LTB) 4. Tracheitis
Croup Syndromes: Epiglottitis • Inflammation of the epiglottis. • Edema in this area can rapidly (within minutes or hours) obstruct the airway by occluding the trachea. • Is considered potentially life threatening • Difficulty in swallowing; drooling • As larynx becomes obstructed, stridor develops. Croup Syndromes : Acute Epiglottitis • Sits up and leans forward with jaws thrust forward in “sniffing” or “tripod posture”. • A previously healthy child suddenly becomes very ill with: – High fever >102.2 f.; Sore throat. • Dysphonia (muffled, hoarse or absent voice sounds). • The 4 classic signs of epiglotitis, in order of appearance are: Dysphonia, Dysphagia. Drooling. Distressed respiratory effort. Croup Syndromes : Epiglottitis • Often caused by bacterial infection. – Haemophilus influenzae type B (Hib); Streptococcus.; Staphylococcus. • Use of Hib vaccine has decreased number of cases of epiglottitis. • DX based on lateral neck x-ray – reveals enlarged, rounded epiglottis, seen as mass at base of tongue. • Laryngospasm can occur as result of irritation of airway muscles. For this reason visual inspection of the mouth & throat are contraindicated. • Obstruction is almost certain is physical manipulation - further irritates the tissue. • A physician can perform immediate intubation if needed • Immediate treatment consists of: – Maintaining the airway, usually via endotracheal tube (24-36 hrs) with cool mist and supplemental oxygen. – Antibiotics and Antipyretic for fever and sore throat pain. – Hydration; Emotional support.
Acute Laryngotracheobronchitis (LTB) • LTB is the most common type of croup. • Usual cause is viral. Infection affects the larynx, trachea, & bronchi. • Most common in children under 5 years. • Usually preceded by URI which descends. • Gradual onset of fever; with Swelling of the airway occurs ASSESSMENT • History of being ill for several days with upper respiratory symptoms which progress to a cough and hoarseness. • Fever may or may not be present, Copious, tenacious secretions are produced. • Tachypnea; Inspiratory stridor; Seal-like barking cough. • Forced air passing through the obstruction increases negative pressure in the thoracic cavity. This causes pulmonary vascular fluid to leak into interstitial spaces. • Can progress to respiratory failure. THERAPEUTIC MANAGMENT – Maintain airway; Children with no stridor are managed at home. – Parents must be taught to recognize signs of respiratory distress. – Cool mist – constricts edematous blood vessels; Oxygen Hoods for infants; Mist tents for toddlers. – Maintain fluid intake. – Nebulized epinephrine is used to TX severe cases of croup (stridor at rest, retraction). – Corticosteroids – anti-inflammatory effect reduces subglottic edema. – Nursing care involves continuous observation & assessment of respiratory system. – Intubation equipment should be sent with child during transport to areas such as x-ray. Acute Spasmodic Laryngitis • Also called midnight croup. Usually ocurs among ages 1 – 3 yrs. • Paroxysmal attacks for laryngeal obstruction that chiefly occurs at night, • Signs of inflammation are absent or mild; Suspected cause is viral, allergy or emotional; usually no fevers; Child goes to bed apparently well or with mild respiratory symptoms. • Awakens suddenly with barking, metallic cough, hoarseness, noisy inspiration and restlessness. Attack subsides in few hours. • Interventions: Managed at home; Cool mist; Racemic epinephrine
Bacterial Tracheitis • Infection of the mucosa of the upper trachea • Occurs mostly among children ages 1 month to 6 years; Often a complication of LTB • Interventions: Humidified oxygen, Suctioning; Antipyretics; Antibiotics; Many children require endotracheal intubation
Respiratory Syncytial Virus (RSV) • Bronchiolitis – acute viral infection of the bronchiolar level. Occurs primarily in winter and spring. • Rare in children over 2 years of age. Caused by RSV 80% of time. • RSV causes fusion of infected cell membrane with those of adjacent epithelial cells forming a giant cell with multiple nuclei. • Bronchiole mucosa swell; Filled with mucus and exudate. Air trapping.occurs • Transmitted through direct contact with respiratory secretions. • RSV can survive for hours on counter tops, gloves, & paper. • Assessment: 2 – 5 mo. is peak age for infection • Can be reinfected. 5 – 8 day incubation • Rhinorrhea, Low grade fever • Otitis media and conjunctivitis may be present • Cough, Wheezing, Retractions, Crackles, Dyspnea, Tachypnea, Diminished breath sounds DIAGNOSIS • Use nasal or nasopharyngeal secretions for rapid immunofluorescent antibody (IFA) or • Enzyme-linked immunosorbent assay (ELISA) • High humidity, Increase fluid intake, Rest, IV fluids, O2 sats, Oxygen by hood or tent • More seriously ill child treated in hospital setting • Ribavirin, (antiviral agent ). Give aerosolized 12 – 20 hrs/day for 1 - 7 days – Controversy over use – Shut aerosol generator off a few minutes before opening tent – Pregnant health care worker should not care for a child receiving ribavirin.
Respiratory Syncytial Virus (RSV) • Respiratory syncytial virus immune globulin (RSV-IGIV or RespiGam) have been used prophylactically to prevent infection in high risk infants. • Private room or grouped with other RSV children • Hand washing; Do not touch nasal mucosa or conjunctiva; Minimal hospital personal and visitors • Nurses caring for infants with RSV should not care for other infants. List at Least 5 Complications of Otitis Media. • 1. Tympanic membrane rupture • 2. Tympanosclerosis • 3. Meningitis • 4. Labyrinthitis • 5. Chronic suppurative otitis media • 6. Mastoiditis Foreign Body Aspiration • Common in children ages 1 - 3 yrs. • Severity is determined by location, type of object aspirated, and extent of obstruction. • Dry vegetable matter such as seed, nut or piece of carrot or popcorn that do not dissolve, may swell when wet and cause major problem. • Fatty foods like potato chips pose problem of lipoid pneumonia. • Offending food in order of frequency : Hot dogs, Round candy, Peanut or other nut, Grape , Cookie or biscuit, Meat, Carrot, Apple, Peanut butter. Asessment: • Choking, gagging or coughing., Symptoms depend on the site. • Cyanosis asymmetrical breath sounds; Wheezing; Dyspnea. • May asphyxiation and die or may show few symptoms for hours, days or weeks. • X-rays reveal opaque objects; Bronchoscopy is required for definitive diagnosis of objects in trachea and larynx. Therapeutic management: • Abdominal thrust for children over 1 yr.; Back blows and chest thrust or infants less than 1 yr. • Can be removed by bronchscopy. • High humidity environment. • Appropriate antibiotics for resulting infections. Cystic Fibrosis Cystic Fibrosis • Characterized by exocrine or mucus-producing gland dysfunction - producing multisystem involvement. • Most common lethal genetic illness among white children, adolescents and young adults. • 3.3 % of white persons in U.S. are symptom free carriers. Clinical manifestations: • Primary symptom is production of thick, sticky mucus. Chronic moist, productive cough • Early signs in newborn is meconium ileus, a small bowel obstruction that occurs the first few days of life. • In infants & toddlers: fecal impaction & intussusception may be first signs. • Steatorrhea (fatty stool). • Rectal prolapse from large, bulky, difficult-to-pass stools. Clinical manifestations: • Frequent respiratory infections, Poor weight gain, Delayed bone age, Short stature; Delayed onset of puberty, Clubbing of fingers. Cystic Fibrosis: Etiology • Gene on chromosome 7 causes defective chloride-ion transport across epithelial cells. • Leads to viscous secretions. • All body organs with mucous ducts become obstructed and damaged. GI Symptoms: • Pancreatic ducts are blocked & result in pancreatic damage. • Enzymes needed to digest fats and proteins are not secreted and essential nutrients are excreted in the stool.
• Cough occurs because lungs are filled with mucus that the cilia cannot clear. • Air becomes trapped in small airways leading to atelectasis. Reproductive system: • Nearly all males /w CF are sterile because the vas deferens is blocked or absent. • Females have difficulty conceiving because of increased mucus in reproductive system interfering with passage of sperm. Metabolic function • Altered due to excessive electrolyte loss thru perspiration, saliva, & mucus secretions. Skin has salty taste. Cystic Fibrosis: Dignostic tests • Newborn –meconium ileus, malabsorbtion or failure to thrive or chronic respiratory infections. • Absence of pancreatic enzymes • Definitive test is a positive sweat test (increase in electrolytes) • Positive family history and Chronic pulmonary involvement Cystic Fibrosis: Medical management Maintain respiratory function, Manage infection; Promote optimal nutrition & exercise Prevent GI blockage; The disease is terminal but many survive to adulthood. Aerosol bronchodilators.; Aerosol Dormase alfa – liquefies secretions. Anti-inflammatory agents: steroids, high dose ibuprofen. Chest physiotherapy for all lung segments; and Infection management. Nutritional needs. • Pancreatic enzyme supplement (Cotazym-S, Pancrease, Viokase) taken with meals 7 snacks. • Well balanced diet with 120-150% of RDA calories and 200% of RDA protein, moderate fat, nutritional counseling needed. • Multivitamin, vit. E in water soluble form, vit. A,D, & K when deficient, iron supplement. • Oxygen Administered via Plastic Hood; Tent for Oxygen Administration • Percussion with Hand or Device • Silastic Pediatric Tracheostomy Tube and Obturator: Temporary vs. long term • Routine care and Trach care, Trach suctioning • Emergency care: occlusion, accidental decannulation