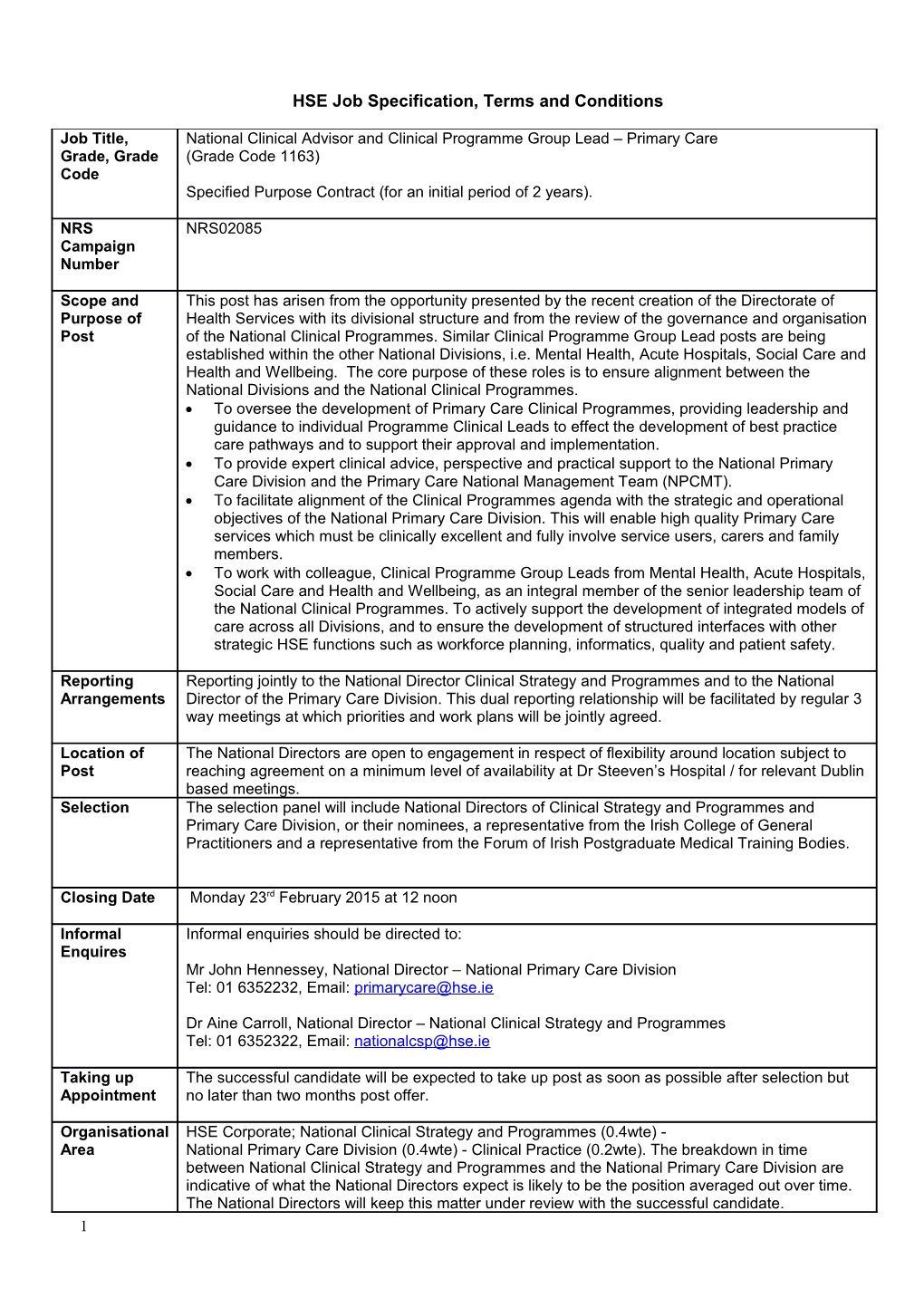
HSE Job Specification, Terms and Conditions
Job Title, National Clinical Advisor and Clinical Programme Group Lead – Primary Care Grade, Grade (Grade Code 1163) Code Specified Purpose Contract (for an initial period of 2 years).
NRS NRS02085 Campaign Number
Scope and This post has arisen from the opportunity presented by the recent creation of the Directorate of Purpose of Health Services with its divisional structure and from the review of the governance and organisation Post of the National Clinical Programmes. Similar Clinical Programme Group Lead posts are being established within the other National Divisions, i.e. Mental Health, Acute Hospitals, Social Care and Health and Wellbeing. The core purpose of these roles is to ensure alignment between the National Divisions and the National Clinical Programmes. To oversee the development of Primary Care Clinical Programmes, providing leadership and guidance to individual Programme Clinical Leads to effect the development of best practice care pathways and to support their approval and implementation. To provide expert clinical advice, perspective and practical support to the National Primary Care Division and the Primary Care National Management Team (NPCMT). To facilitate alignment of the Clinical Programmes agenda with the strategic and operational objectives of the National Primary Care Division. This will enable high quality Primary Care services which must be clinically excellent and fully involve service users, carers and family members. To work with colleague, Clinical Programme Group Leads from Mental Health, Acute Hospitals, Social Care and Health and Wellbeing, as an integral member of the senior leadership team of the National Clinical Programmes. To actively support the development of integrated models of care across all Divisions, and to ensure the development of structured interfaces with other strategic HSE functions such as workforce planning, informatics, quality and patient safety.
Reporting Reporting jointly to the National Director Clinical Strategy and Programmes and to the National Arrangements Director of the Primary Care Division. This dual reporting relationship will be facilitated by regular 3 way meetings at which priorities and work plans will be jointly agreed.
Location of The National Directors are open to engagement in respect of flexibility around location subject to Post reaching agreement on a minimum level of availability at Dr Steeven’s Hospital / for relevant Dublin based meetings. Selection The selection panel will include National Directors of Clinical Strategy and Programmes and Primary Care Division, or their nominees, a representative from the Irish College of General Practitioners and a representative from the Forum of Irish Postgraduate Medical Training Bodies.
Closing Date Monday 23rd February 2015 at 12 noon
Informal Informal enquiries should be directed to: Enquires Mr John Hennessey, National Director – National Primary Care Division Tel: 01 6352232, Email: [email protected]
Dr Aine Carroll, National Director – National Clinical Strategy and Programmes Tel: 01 6352322, Email: [email protected]
Taking up The successful candidate will be expected to take up post as soon as possible after selection but Appointment no later than two months post offer.
Organisational HSE Corporate; National Clinical Strategy and Programmes (0.4wte) - Area National Primary Care Division (0.4wte) - Clinical Practice (0.2wte). The breakdown in time between National Clinical Strategy and Programmes and the National Primary Care Division are indicative of what the National Directors expect is likely to be the position averaged out over time. The National Directors will keep this matter under review with the successful candidate. 1 Details of National Primary Care Division and National Clinical Strategy and Programmes Service The Government’s health reform programme; Future Health, aims to improve the population’s health, assist health services staff to improve services to the public, and demonstrate to taxpayers that value for money is being delivered.
The Primary Care Division will carry full operational accountability and responsibility for all Primary Care services in Ireland with the core objective of improving the Primary Care services available to the population. The Clinical Strategy and Programmes, established in 2010, aim to improve and standardise patient care. They are a key change vehicle for the National Primary Care Division and the clinical leadership of the Clinical Programmes is a critical success factor. The National Clinical Programmes are embarking on the next level of evolution in 2014, as the Director of Clinical Strategy and Programmes oversees the development of a suite of Integrated Care Pathways, which design models of best care across the continuum of health services from primary to secondary to tertiary and quaternary care. The Forum of Irish Postgraduate Medical Training Bodies has been engaged with the Clinical Programmes since their outset and functions to represent their commonality of interests and underpin leadership and integration. The development of a proactive sustainable relationship between the post holder and the ICGP in the development of the programmes will be key to their success.
With the establishment of the five new Divisions and, on reviewing the outcomes of the Clinical Programmes to date, it is timely to restructure the programmes to allow more alignment with the National Divisions and the operational side of the organisation.
This restructuring will allow for better alignment of the Clinical Programmes with the priorities of the ‘Future Health’ and will facilitate strategic development of priority programmes which take full account of available resources, current deficits, clinical evidence and emerging developments. These programmes will be monitored against an agreed benefits realisation plan.
The Primary Care Division is responsible for a budget of approximately €3bn and over 9,000 staff. Primary Care Services also includes the services of the Primary Care Reimbursement Service (PCRS) which provides a wide range of primary care services to the general public, through over 7,000 primary care contractors across 12 community health schemes.
The post holder will be a key member of the National Primary Care Management Team (NPCMT) which in summary is charged with:
• Managing primary care service delivery on a day to day basis • Driving continuous service improvement • Leading primary care services through the full implementation of the Healthcare reform programme.
The Primary Care Management Team will:
Be accountable for delivery of safe, cost effective and appropriate primary care services within the allocated budget. Achieve national performance targets as specified in the HSE’s Annual National Service Plan. Reform the primary care system in order to provide faster access for patients to high quality services and prepare for the introduction of a single tier system of health care supported by Universal Health Insurance. Create the conditions necessary to enable those working in primary care to fulfil their potential and take full ownership of their responsibilities to service users. Create the clinical and managerial capacity to deliver safe, high quality services which are cost effective and can transition safely to the commissioner/provider model i.e. within autonomous community healthcare organisations. Design and implement world class models of health promotion and models of recovery focused health care. Adopt a well-structured approach to designing, incentivising and measuring integration within primary care services and between primary care and other services (Health and Socialcare, and other public services). Develop and implement a performance management culture within our primary care services. Maximise the benefits to service users and their carers of the on-going government 2 investment in primary care. Cultivate sustainable positive relationships with key internal and external stakeholders. This includes service user and family / carer organisations, government departments, state agencies, NGO partners and funded organisations, public representatives, media, professional and training bodies, trade unions, HSE service divisions (Mental Health, Acute Hospitals, Social Care and Wellbeing) and HSE functions. Foster sustainable practical models for individual volunteerism and community involvement in promoting health and supporting service delivery. Build the capacity to demonstrate with evidence that they have delivered on the critical success factors above
Key Working The proper execution of duties will involve the development of appropriate communication Relationships arrangements with key stakeholders both internal and external, as mentioned above.
Principal These will include: Duties and To participate as a key member of the NPCMT in the collective decisions and actions Responsibiliti necessary to manage and improve the Primary Care services to the population. es To provide clinical expertise and leadership to the Primary Care clinical leads involved in the National Clinical Programmes / Integrated Care Pathways.
To involve, as appropriate, the service users, carers and family members and the general public in the design of National Clinical Programmes / Integrated Care Pathways.
To provide expert clinical advice, perspective and practical support to the Primary Care Service and its National Management Team.
To advise on the development of a clinical governance framework and clinical resources for Primary Care
To provide clinical advice to the NPCMT on the implementation of national quality and safety standards as they relate to primary care services.
To work collaboratively with other National Clinical Group Leads, to ensure there is coherent guidance across Divisions and National Clinical Programmes / Integrated Care Pathways and highlight Primary Care service / clinical priorities within that group.
To identify interdependencies between National Clinical Programmes / work streams / Integrated Care Pathways and facilitate agreement on how best these are managed.
To advise and support each member of the NPCMT in carrying out their duties with the benefit of expert, up to date and practical senior clinical input.
To oversee the development of Primary Care Clinical Programmes and support their approval and implementation by the NPCMT.
To oversee the development and implementation of a framework to allow all clinical disciplines within Primary Care to inform the clinical advice and input received by the NPCMT.
To assist with national input to operational issues.
To provide significant senior clinical input into the development and implementation of: o A clinical and management information system detailed specification which supports the delivery and improvement of Primary Care services. o Workforce planning and scope of practice developments o Continuing professional development o A strategic, service and operational planning framework o A performance management framework to facilitate controlling against the plans above incorporating relevant performance indicators. o A relative demand, resource and productivity analysis framework to inform resource allocation decisions. 3 Support the development of a network of clinical leaders and advisors nationally in Primary Care services including encouraging clinical audit, research and standard setting in conjunction with the National Clinical Effectiveness Committee.
To proactively foster sustainable working relationships with key clinical training and accreditation bodies.
To act as a spokesperson for the HSE (e.g. with the media, professional groups and other relevant fora) when appropriate.
To put in place systems and processes to ensure the NPCMT and staff in the Primary Care services are kept appropriately up to date with relevant international trends and best practice as it pertains to the post holders core remit.
To model a collaborative and influencing style of working, negotiating with others to achieve the best outcomes.
To provide clinical input into the development of quality standards and, through clinical leadership, influence the introduction and achievement of such standards.
To provide leadership and support to the staff working within each Integrated Care Pathway team by ensuring regular, productive and open communication with staff who they lead (e.g. Division and matrix teams).
To harness expertise and advocacy by engaging with a range of organisations; including, the voluntary sector, post graduate training bodies, specialist professional associations, patient groups, community health services and social care to develop a shared focus on improvement and alignment of purpose.
Take lead responsibility for cultivating effective relationships and advancing integration with colleagues in HSE and external stakeholders across the main competency areas above.
The above Job Description is not intended to be a comprehensive list of all duties involved and consequently, the post holder may be required to perform other duties as appropriate to the post which may be assigned to him/her from time to time and to contribute to the development of the post while in office.
Eligibility On the closing date of the campaign each applicant must: Criteria Be registered with the Irish Medical Council in the Specialist Division in the Specialty of Qualifications General Practice. and/ or Be currently practising as a General Practitioner. experience Significant experience in a leadership role in Primary Care Services. Experience in a change management role, for example as a professional representative or in a clinical programme management role or involvement in education programmes or quality improvement initiatives. Possess relevant recent clinical experience and up to date knowledge of current evidence based best practice and standards for Primary Care services including policy formulation and implementation, performance management, clinical audit and research.
Health A candidate for and any person holding the office must be fully competent and capable of undertaking the duties attached to the office and be in a state of health such as would indicate a reasonable prospect of ability to render regular and efficient service.
Character Each candidate for and any person holding the office must be of good character
Age Age restrictions shall only apply to a candidate where he/she is not classified as a new entrant
4 (within the meaning of the Public Service Superannuation Act, 2004). A candidate who is not classified as a new entrant must be under 65 years of age.
Skills, competencies Clinical/ Professional Knowledge and/or knowledge Candidates should demonstrate an understanding of Project Management technologies, Health Informatics and Standard setting.
Demonstrates: Credibility and ability to command respect as a recognised clinical leader within the clinical community with a good understanding of the reform programme and its requirements of clinical leaders. Experience of providing significant senior clinician input to operational decision making. A track record as an effective leader who has developed effective teams and driven and delivered sustainable change programmes to transform clinical services. A capacity to operate successfully and efficiently in a challenging environment. A commitment to and focus on quality, promotes high standards to improve patient outcomes, by consistently putting clinicians at the heart of decision making and involving patients and the public in their work. Excellent interpersonal and communications skills.
Results focused with critical analysis and decision making
Demonstrates: Strong personal emphasis on achieving high standards of excellence and willingness to take personal responsibility to initiate activities and drive objectives through to a conclusion. Ability to rapidly assimilate and analyse complex information, make timely decisions and take ownership of those decisions and their implications. Capacity to anticipate problems and to recognise when to involve other parties at the appropriate time and level. Uses evidence to make improvements and seeks out innovations.
Working with and through others
Demonstrates: An ability to influence and negotiate effectively in furthering the objectives of the role. An ability to build excellent collaborative networks and a track record of building and maintaining key internal and external relationships in furtherance of organisational goals. Highly developed communication skills which include an ability to convey clinical priorities and complex messages to colleagues, various stakeholders, media and interest groups.
Specific Short listing may be carried out on the basis of information supplied in your application. The criteria Selection for short listing are based on the requirements of the post as outlined in the eligibility criteria and Process skills, competencies and/or knowledge section of this job specification. Therefore it is very important that you think about your experience in light of those requirements. Failure to include information regarding these requirements may result in you not being called forward to the next stage of the selection process. Those successful at the shortlisting stage of this process (where applied) will be called forward to a meeting with the selection panel.
Other Access to own transport will be required as post will involve travel. requirements specific to the post Code of The Health Service Executive will run this campaign in compliance with the Code of Practice Practice prepared by the Commissioners for Public Service Appointments (CPSA). The Code of Practice sets out how the core principles of probity, merit, equity and fairness might be applied on a principle basis. The Code also specifies the responsibilities placed on candidates, feedback facilitates for applicants on matters relating to their application when requested, and outlines procedures in relation to requests for a review of the recruitment and selection process and review 5 in relation to allegations of a breach of the Code of Practice. Additional information on the HSE’s review process is available in the document posted with each vacancy entitled “Code of Practice, Information For Candidates”. Codes of practice are published by the CPSA and are available on www.careersinhealthcare.ie in the document posted with each vacancy entitled “Code of Practice, information for candidates or on www.cpsa-online.ie.
The reform programme outlined for the Health Services may impact on this role and as structures change the job description may be reviewed. This job specification is a guide to the general range of duties assigned to the post holder. It is intended to be neither definitive nor restrictive and is subject to periodic review with the employee concerned.
The reform programme outlined for the Health Services may impact on this role and as structures change the job description may be reviewed. This job description is a guide to the general range of duties assigned to the post holder. It is intended to be neither definitive nor restrictive and is subject to periodic review with the employee concerned.
6 Terms and Conditions of Employment National Clinical Advisor and Clinical Programme Lead – Primary Care
Tenure The appointment is specified purpose (for an initial period of 2 years). The appointment is whole-time and pensionable.
Appointment as an employee of the Health Service Executive is governed by the Health Act 2004 and the Public Service Management (Recruitment and Appointment) Act 2004.
Remuneration The annual salary will be €143,000.
Working Week The standard working week applying to the post is: 39 hours per week
Annual Leave The annual leave associated with the post is: 30 Working Days per annum and as determined by the Organisation of Working Time Act 1997.
Superannuation This is a pensionable position within the HSE. The successful candidate will upon appointment become a member of the appropriate pension scheme. Please be advised that pension scheme membership will be notified within the contract of employment. Members of pre-existing pension schemes who transferred to the HSE on 1st January 2005 pursuant to Section 60 of the Health Act 2004 are entitled to superannuation benefit terms under the HSE Scheme which are no less favourable to those to which they were entitled at 31st December 2004.
Probation Every appointment of a person who is not already a permanent officer of the Health Service Executive or of a Local Authority shall be subject to a probationary period of 12 months as stipulated in the Department of Health Circular No.10/71.
Special Conditions A leave of absence arrangement will be put in place to allow the appointee to undertake related to this post this role and maintain GMS contract(s). The capitation payment and all other financial elements of the GMS contract(s) will be paid to the assignee.
Protection of Persons As this post is one of those designated under the Protection of Persons Reporting Child Reporting Child Abuse Abuse Act 1998, appointment to this post appoints one as a designated officer in Act 1998 accordance with Section 2 of the Act. You will remain a designated officer for the duration of your appointment to your current post or for the duration of your appointment to such other post as is included in the categories specified in the Ministerial Direction. You will receive full information on your responsibilities under the Act on appointment.
Infection Control All HSE Employees must have a working knowledge of HIQA Standards as they apply to the role for example, Standards for Healthcare, National Standards for the Prevention and Control of Healthcare Associated Infections, Hygiene Standards etc.
Ethics in Public Office Positions remunerated at or above the minimum point of the Grade VIII salary scale (€ 1995 and 2001 64,812 as at 01.01.2010) are designated positions under Section 18 of the Ethics in Public Office Act 1995. Any person appointed to a designated position must comply with the requirements of the Ethics in Public Office Acts 1995 and 2001 as outlined below; Positions remunerated at or above the A) In accordance with Section 18 of the Ethics in Public Office Act 1995, a person minimum point of the holding such a post is required to prepare and furnish an annual statement of any Grade VIII salary scale interests which could materially influence the performance of the official functions of the (€ 64,812 as at 01.01.10) post. This annual statement of interest should be submitted to the Chief Executive Officer not later than 31st January in the following year.
B) In addition to the annual statement, a person holding such a post is required, whenever they are performing a function as an employee of the HSE and have actual knowledge, or a connected person, has a material interest in a matter to which the function relates, provide at the time a statement of the facts of that interest. A person 7 holding such a post should provide such statement to the Chief Executive Officer. The function in question cannot be performed unless there are compelling reasons to do so and, if this is the case, those compelling reasons must be stated in writing and must be provided to the Chief Executive Officer.
C) A person holding such a post is required under the Ethics in Public Office Acts 1995 and 2001 to act in accordance with any guidelines or advice published or given by the Standards in Public Office Commission. Guidelines for public servants on compliance with the provisions of the Ethics in Public Office Acts 1995 and 2001 are available on the Standards Commission’s website http://www.sipo.gov.ie/
8