Hematology PPT Flashcards Unit 4
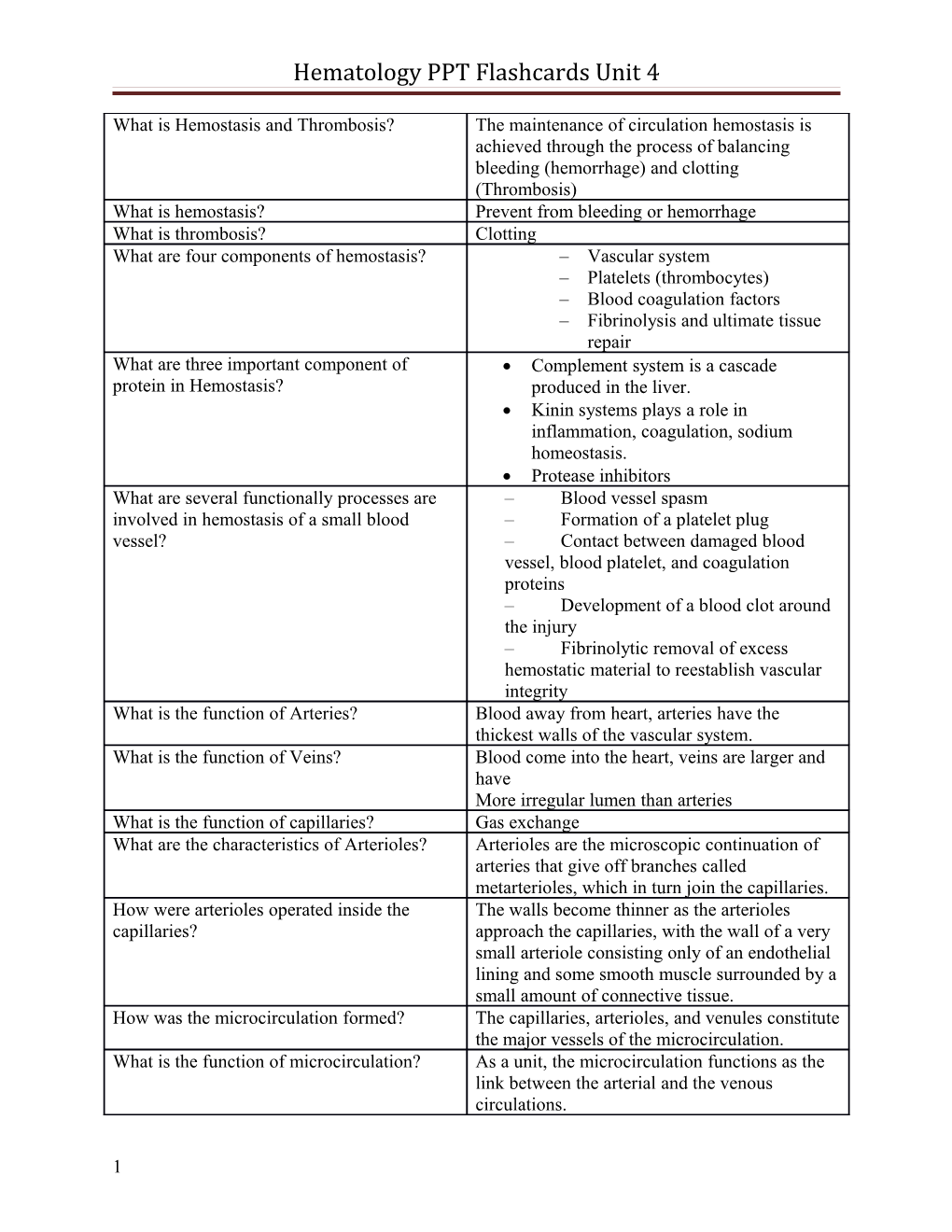
What is Hemostasis and Thrombosis? The maintenance of circulation hemostasis is achieved through the process of balancing bleeding (hemorrhage) and clotting (Thrombosis) What is hemostasis? Prevent from bleeding or hemorrhage What is thrombosis? Clotting What are four components of hemostasis? – Vascular system – Platelets (thrombocytes) – Blood coagulation factors – Fibrinolysis and ultimate tissue repair What are three important component of Complement system is a cascade protein in Hemostasis? produced in the liver. Kinin systems plays a role in inflammation, coagulation, sodium homeostasis. Protease inhibitors What are several functionally processes are – Blood vessel spasm involved in hemostasis of a small blood – Formation of a platelet plug vessel? – Contact between damaged blood vessel, blood platelet, and coagulation proteins – Development of a blood clot around the injury – Fibrinolytic removal of excess hemostatic material to reestablish vascular integrity What is the function of Arteries? Blood away from heart, arteries have the thickest walls of the vascular system. What is the function of Veins? Blood come into the heart, veins are larger and have More irregular lumen than arteries What is the function of capillaries? Gas exchange What are the characteristics of Arterioles? Arterioles are the microscopic continuation of arteries that give off branches called metarterioles, which in turn join the capillaries. How were arterioles operated inside the The walls become thinner as the arterioles capillaries? approach the capillaries, with the wall of a very small arteriole consisting only of an endothelial lining and some smooth muscle surrounded by a small amount of connective tissue. How was the microcirculation formed? The capillaries, arterioles, and venules constitute the major vessels of the microcirculation. What is the function of microcirculation? As a unit, the microcirculation functions as the link between the arterial and the venous circulations.
1 Hematology PPT Flashcards Unit 4
What is vasculature physiology role in • The role of vasoconstriction in hemostasis? hemostasis • The role of the endothelium • Maintenance of vascular integrity How does the vasoconstriction play a role in When a smaller vessel, such as an arteriole, hemostasis? venule, or capillary, is injured, contraction occurs to control bleeding. This contraction of the blood vessel wall is called vasoconstriction. What is the endothelium? The endothelium contains connective tissues such as collagen and elastin. How does endothelium play a role in The endothelium is highly active metabolically hemostasis? and is involved in the clotting process by producing or storing clotting components. What was endothelium role in lysis of fibrin It is also rich with plasminogen activator, clots hemostasis? which, if appropriately stimulated, is released and activates plasminogen, which ensures rapid lysis of fibrin clots. What is the prostacyclin role in hemostasis? Additionally, the endothelium elaborates prostacyclin, which is synthesized by the endothelium from prostaglandin precursors and strongly inhibits platelet aggregation and adhesion. How was the primary phase hemostasis Initially, rapid vasoconstriction for up to 30 activated after disruption of the endothelium? minutes reduces blood flow and promotes contact activation of platelets and coagulation factors How was the second phase hemostasis In the second phase, platelets adhere activated after disruption of the endothelium? immediately to the exposed subendothelial connective tissue, particularly collagen. The aggregated platelets enhance sustained vasoconstriction by releasing thromboxane A2 and vasoactive amines, including serotonin and epinephrine How was the third phase hemostasis activated In the third phase, coagulation is initiated after disruption of the endothelium? through both the intrinsic and extrinsic systems How was the final phase hemostasis activated Finally, fibrinolysis occurs following the after disruption of the endothelium? release of tissue plasminogen activators (t-PAs) from the vascular wall. Fibrinolytic removal of excess hemostatic material is necessary to reestablish vascular integrity How many factors are required to maintain of Vascular integrity or the resistance to vessel Vascular Integrity hemostasis? disruption requires three essential factors What are the essential factors of vascular Circulating functional platelets integrity in hemostasis? Adrenocorticosteroids
2 Hematology PPT Flashcards Unit 4
Ascorbic acid What will be happened if there is lack of A lack of these factors produces fragility of the essential factors in vascular integrity vessels, which makes them prone to disruption. hemostasis? What will be the initial series observation of General characteristics of megakaryocytic megakaryocytic cell? development What will be the second series observation of The developmental sequence of platelets megakaryocytic cell? What is the third series observation of Cellular ultrastructure of a mature platelet megakaryocytic cell? What will be the last series observation of Platelet kinetics, life span, and normal values megakaryocytic cell? How were the platelets (thrombocytes) role in Mature platelets (thrombocytes) hemostasis of megakaryocytic development? (metabolically active cell fragments) are the second critical component in the maintenance of hemostasis Where were the platelets (thrombocytes) These anuclear cells circulate in the peripheral found? blood after being produced from the cytoplasm of bone marrow megakaryocytes, the largest cells found in the bone marrow What are the stages of being formed platelets? 1) Megakaryoblast 2) Promegakaryocyte 3) Megakaryocyte a. Platelets Where were the bone marrow Bone marrow megakaryocytes are derived from megakaryocytes found? pluripotential stem cells How were the platelets formed inside the The sequence of development from cytoplasmic membrane? megakaryocytes to platelets is thought to progress from the proliferation of progenitors to polyploidization, that is, nuclear endoreduplication, and finally to cytoplasmic maturation and the formation of platelets Where was the initial process of Megakaryocytopoiesis proceeds initially megakaryocytopoiesis take place? through a phase characterized by mitotic division of a progenitor cell; Followed by a wave of nuclear endoreduplication. What is endoreduplication process of Endoreduplication is the process in which progenitors? chromosomal material (DNA) and the other events of mitosis occur without subsequent division of the cytoplasmic membrane into identical daughter cells What are two classes of progenitors that have 1) Burst-forming-unit megakaryocyte been identified in the early development of (BFU-M) platelets? 2) Colony-forming-unit megakaryocyte (CFU- M) What is the function of Burst-forming-unit The BFU-M is the most primitive progenitor
3 Hematology PPT Flashcards Unit 4 megakaryocyte (BFU-M)? cell committed to megakaryocyte lineage What is the second stage of megakaryocyte The next stage of megakaryocyte development development of platelets? is a small, mononuclear marrow cell that expresses platelet-specific phenotypic markers but is not morphologically identifiable as a megakaryocyte How well were the mononuclear marrow cells These transitional cells represent 5% of of platelets visible in cytoplasmic? marrow megakaryocyte elements. Have the transitional immature Some transitional immature megakaryocyte megakaryocyte cells been undergoing cells may be capable of cellular division, but endomitosis? most are nonproliferating while actively undergoing endomitosis. Described the final stage of megakaryocyte The final stage of megakaryocyte development development: is the morphologically identifiable megakaryocyte. These cells are readily recognizable in the marrow because of their large size and lobulated nuclei. These cells are polyploid. What is the size of a mature platelet? Platelets have an average diameter of 2 to 4 mm, with younger platelets being larger than older ones Does a platelet have a nucleus? In contrast to megakaryocytes, platelets have no nucleus. What is the characteristic of a platelet? The cytoplasm is light blue, with evenly dispersed, fine red-purple granules. What is the characteristic of an inactive An inactive or unstimulated platelet circulates as platelet? a thin, smooth-surfaced disc. What is platelet adhesion? When vascular injury exposes the endothelial surface, underlying collagen platelets adhere to the subendothelial collagen fibers, spread pseudopods along the surface, and clump together (aggregate). How quickly does platelet adhesion to 1-2 minutes after a break in the endothelium. subendothelial connective tissue, especially collagen happen? What’s the best test to use to determine Platelet aggregation. platelet function? What is a thrombus? When the bridges formed by fibrinogen in the presence of calcium produce a sticky surface on platelets, resulting in aggregation and then reinforced by fibrin is considered a thrombus. What substances can cause a blockage of a Prostaglandin E (PG E), adenosine, and pathway by an aggregation of platelets? nonsteroidal anti-inflammatory agents (e.g., aspirin).
How are permanently anchored platelet plugs With fibrinogen, under the influence of small
4 Hematology PPT Flashcards Unit 4 given additional consolidation and amounts of thrombin. This process involves the stabilization? precipitation of polymerized fibrin around each platelet resulting in a fibrin clot that produces an irreversible platelet plug. Why is a platelet count a fundamental Examination of the peripheral blood smear for component in the evaluation of a patient? platelet number and morphology is critical because many clinical clues may be obtained from an evaluation of platelet quantity and morphology. What are other fundamental evaluations of Platelet aggregation, platelet adhesion, and platelets? antiplatelet antibody assays. Blood coagulation factors are one of the most important of the assays. What are blood coagulation factors? Basic concepts of blood coagulation, common characteristics of coagulation factors, characteristics of individual factors, the mechanism of coagulation, fibrin formation, laboratory assessment of blood coagulation factors, and assays for fibrin formation. What is blood coagulation a sequential Chemical reactions, involving plasma proteins, process of? phospholipids, and calcium ions. What are circulating factors that participate in Roman numerals. the coagulation process designated by? How are the roman numerals effected if the It’s a roman numeral followed by the suffix –a enzymatic factor is activated? and the inactive enzymatic factor, zymogens are the roman numeral alone. What are 3 assays that are conducted by 1) One-stage quantitative assay for factors II, V, specialized coagulation laboratories? VII, and X. 2) One-stage quantitative assay for factors VIII, IX, XI, and XII. 3) Factor VIII antibodies in hemophiliacs. What specimen is used for the One-stage Aged serum and absorbed plasma in the PT. quantitative assay for factors II, V, VII, and X? What factors does age serum contain? Factors VII, IX, X, IX, and XII. What factors does absorbed plasma contain? Factors V, VIII, XI, and XIII Who is the PT for One-stage quantitative Using specific factor-deficient plasma with assay for factors II, V, VII, and X conducted? specific dilutions of patient plasma.
Why is the percentage of factor activity To construct an activity curve. plotted? For One-stage quantitative assay for factors The APTT assay. VIII, IX, XI, and XII, what procedure is it And it is based on the results of patient plasma based on? to correct specific factor-deficient plasma. Who are the results expressed in One-stage In percent activity on an activity curve.
5 Hematology PPT Flashcards Unit 4 quantitative assay for factors VIII, IX, XI, and XII? What is the factor VIII antibodies in An ELISA technique that uses the binding of hemophiliacs assay? antibodies in the plasma to solid phase antigen, which is subsequently detected by a human polyclonal IgG labeled with the alkaline phosphatase-p-nitrophenyl phosphate substrate system. What is Warfarin? The traditional oral anticoagulant (Coumadin). Warfarin drugs are vitamin K antagonists that interfere with the normal synthesis of factors II, VII, IX, and X as well as proteins C and S. Why do Warfarin drugs cause incomplete Because they lack calcium-binding sites and coagulation? cannot form enzyme substrate complexes. Thus, these factors are unable to function as procoagulants or anticoagulants. Biological activity is significantly1)______Decreased (decreased or increased) as revealed by the PT. The onset of action of most warfarin 8 and 12 hours derivatives is between how many hours? The maximum affect occurs in approximately 36 hours how many hours? What is the duration of action of Warfain? Approximately 72 hours. What is the mainstay of immediate therapy Heparin anticoagulation for acute PE. How does Heparin acts as an anticoagulant? Heparin has no anticoagulant activity of its own but acts as an anticoagulant by accelerating the binding of antithrombin to target enzymes (e.g., thrombin and factor Xa). Why is Heparin termed an antithrombin? Because it helps prevent new thrombus formation and buys time for endogenous fibrinolytic mechanisms to lyse the clot. What can Heparin cause? Bleeding, thrombocytopenia, and osteopenia. Before initiating heparin, what should Clinical evidence of active bleeding patients be screened for? What should the baseline laboratory CBC, platelets, PTT, PT, stool analysis for evaluation include? occult blood, and urine dipstick for hematuria. When is Heparin anticoagulation used? During percutaneous transluminal coronary angioplasty (PTCA) and cardiopulmonary bypass (CPB) to prevent clot formation. What are 2 other Antithrombin-Dependent 1) Danaparoid (Orgaran) inhibiters? – 2) Fondaparinux (Arixtra) What 2 new types of drugs are direct 1) Hirudin, lepirudin (Refludan) thrombin inhibitors? 2) Argatroban
6 Hematology PPT Flashcards Unit 4
What are the new types of thromboplastins Mixtures of phospholipids and recombinantly for measuring the PT? derived human tissue factor. What are Fibrinogen assays useful for? Detecting deficiencies of fibrinogen and alterations in the conversion of fibrinogen to fibrin. The normal value of 200 to 400 mg/dL may Liver disease or the consumption of fibrinogen be decreased in? owing to accelerated intravascular clotting What is the normal titer of fibrinogen? 1:128 to 1:256. What does the thrombin time test determines? The rate of thrombin-induced cleavage of fibrinogen to fibrin monomers and the subsequent polymerization of hydrogen-bonded fibrin polymers to form an insoluble fibrin clot. What is the normal value of thrombin? The normal value is less than 20 seconds. What is the Reptilase time assay similar to? The thrombin time assay. What is the D-Dimer? Is a specific fragment generated from two cross- linked fibrin molecules after a clot has formed. What are the 3 major hemostatic stages that 1) Coagulation to form the clot must be functioning in order for D-dimers to 2) Covalent cross-linking of fibrin by activated form? factor XIII 3) Fibrinolysis to dissolve the fibrin clot into smaller fragment All 3 of these stages require adequate Thrombin formation of? What are 4 normal protective mechanisms 1) Normal blood flow against Thrombosis? 2) Removal of activated clotting factors and particulate material 3) The natural anticoagulant systems 4) Cellular regulators In the blood circulation, the predisposition to The balance between procoagulant and thrombosis depends on? anticoagulant factors. Several important biological activities -The normal flow of blood normally protect the body against thrombosis. -The removal of activated clotting factors and What are these activities? particulate material -Natural anticoagulant systems known to be operative in vivo: * Antithrombin III (AT-III) * Heparin cofactor II (HC-II) * Protein C and its cofactor, protein S -Cellular regulators
What does the normal flow of blood prevent? The accumulation of procoagulant material. This mechanism reduces the chance of? Local fibrin formation. What is another normal mechanism against The removal of activated clotting factors by inappropriate thrombosis? hepatocytes from the blood.
7 Hematology PPT Flashcards Unit 4
What does this process, along with the Limits intravascular clotting and fibrinolysis by naturally occurring inhibitors do? inactivation of such factors as XIa, IXa, Xa, and IIa. Why is the removal of particulate material by It prevents the initiation of coagulation. the cells of the mononuclear phagocytic system also important? Why is the in vivo existence of natural To prevent thrombosis. anticoagulant systems essential? What are the natural anticoagulant systems? Antithrombin III, heparin cofactor II, and protein C and its cofactor, protein S What are AT-III and HC-II? Serine-protease inhibitors. When activated, protein C is capable of V (Va) and VIII (VIIIa) in the presence of the degrading which activated factors? cofactor protein S. What is considered the major inhibitor of Antithrombin III (AT-III) coagulation? What are the serpin superfamily of serine III (AT-III), alpha-1 antitrypsin, C1 inhibitor, proteinase inhibitors? alpha-2 antiplasmin, heparin cofactor II, and plasminogen activator inhibitor. Heparin is produced endogenously by? Mass cells. Heparin-like molecules are found in the? Endothelium. What are the two heparin-dependent thrombin AT-III heparin cofactor and heparin cofactor II, inhibitors present in human plasma? previously referred to as heparin cofactor A. The inhibitory activity of heparin cofactor II Heparin. is accelerated by? What does the inhibition of thrombin by The activity of thrombin or fibrinogen; also heparin cofactor II not limited to? inhibited are thrombin-induced platelet aggregation and release. In addition to thrombin, heparin cofactor II Chymotrypsin also inhibits? Heparin cofactor II does not significantly Blood coagulation factors IXa, Xa, and XIa or inhibit? plasmin. What 2 proteins are involved in one of the Protein C and S major natural anticoagulation systems in the body? Deficiency and/or alteration in either protein Predisposition to thrombosis. (C and/or S) have been clearly associated with? What does Protein C (A vitamin K–dependent A natural anticoagulant formed in response to plasma protein synthesized in the liver) thrombin generation. represents What is APC resistance (A hypercoagulable A point mutation in the factor V gene [factor V condition discovered in 1993) is associated (Leiden)]. with What does the mutation results in? The replacement of Arg506 with Gln(Q) in the factor V protein.
8 Hematology PPT Flashcards Unit 4
This mutation slows the inactivation of what Factor Va by APC factor causing a hypercoagulable state? What is the most common cause of The Inherited thrombophilia. presence of factor V (Leiden)? It accounts for ____? % to _____? % of the 20% to 50% cases. Protein S is another vitamin K–dependent APC to express an anticoagulant effect. plasma protein that is an essential cofactor for? Protein S does not require 1) ____? 1) Proteolytic modification to function, but it can be 2) proteolysis. regulated by 2) ____? What is becoming recognized as essential to Cellular activities related to thrombosis the maintenance of hemostasis and thrombosis? What are 2 powerful mechanisms to limit the Plasma possesses, and plasmin formation or spread of clotting and the reliquefication of clots? What have been demonstrated to be the major Tissue factor and factor VIIa in the extrinsic pathway for activation of coagulation? pathway What has also been discovered about That it has a far more important role as an thrombi? activator and an inhibitor. What is the key enzyme in the conversion of Thrombin soluble fibrinogen into fibrin What is required for the activation of the Thrombin protein C system, which downregulates hemostasis? What is required for the activation of Thrombin thrombin-activatable fibrinolysis inhibitor (TAFI), which is involved in the downregulation of the fibrinolytic process? What has led to the development of The cumulative result of new discoveries in alternative schematic representations of the coagulation has led. pathways that better represent the normal in vivo process of coagulation? What may cause abnormal bleeding? Disorders of the microcirculation, platelets, or plasma proteins. What is purpura? Abnormal bleeding involving the loss of red blood cells from the microcirculation. Purpura is characterized by? Hemorrhages into the skin, mucous membranes, and internal organs. Purpura may be produced by a variety of 1) Purpura associated with direct endothelial vascular abnormalities such as? cell damage. Endothelial damage may result from physical or chemical injury to the tissue caused by microbial agents such as in rickettsial disease or immunological antibody-mediated injury. Bacterial toxins produce deendothelialization induced by an endotoxin. Antibody vascular injury, vasculitis, may be
9 Hematology PPT Flashcards Unit 4
induced by drug reactions, insect bites, or the activation of complement. 2) Purpura associated with an inherited disease of the connective tissue. Alterations of the vascular supportive framework can occur in disorders such as diabetes. 3) Purpura associated with decreased mechanical strength of the microcirculation. Decreased strength can be seen in conditions such as scurvy and amyloidosis. 4) Purpura associated with mechanical disruption of small venules. The principal cause of this type of purpura is increased intraluminal pressure. This condition can be observed around the ankles with prolonged standing and may be caused by the presence of abnormal proteins in macroglobulinemias or hyperviscosity disorders. 5) Purpura associated with microthrombi (small clots). This type of disorder is associated with abnormal intravascular coagulation conditions. 6) Purpura associated with vascular malignancy. Purpura of this origin is observed in Kaposi sarcoma and vascular tumors. What are the disorders of platelet size? 1) Wiskott-Aldrich syndrome 2) May-Hegglin anomaly 3) Alport syndrome 4) Bernard-Soulier syndrome What is Wiskott-Aldrich syndrome? Is the smallest platelets seen.
What is May-Hegglin anomaly? It is characterized by the presence of large platelets and the presence of Döhle-like bodies in the granulocytic leukocytes. What is Alport syndrome? Exhibits giant platelets and thrombocytopenia
What is Bernard-Soulier syndrome? Is the largest platelets seen and is also referred to as giant platelet syndrome. What is the normal range of circulating 150 x 109/L to 450 x 109/L platelets? When the quantity of platelets decreases to Thrombocytopenia levels below 150 x 109/L to 450 x 109/L a condition known as _____? exists. Is the quantity of platelets increases then what Thrombocytosis is the result? Disorders of platelets can be classified as? Quantitative (thrombocytopenia or thrombocytosis) or qualitative (thrombocytopathy). If platelets are absent or severely decreased The presence of petechiae or purpura. below 100 x 109/L, what clinical symptoms are usually seen? What is Petechiae? Small purplish hemorrhagic spots on the skin or
10 Hematology PPT Flashcards Unit 4
mucous membranes. What is Purpura? It is characterized by extensive areas of red or dark-purple discoloration. Most thrombocytopenic conditions can be 1) Disorders of production of platelets may be classified into major categories such as? caused by hypoproliferation of the megakaryocytic cell line or ineffective thrombopoiesis caused by acquired conditions or hereditary factors. 2) Disorders of destruction, including decreased megakaryocytopoiesis and ineffective platelet production, and disorders of utilization. It may result from a number of mechanisms—drugs, bacterial sepsis, etc. 3) Disorders of platelet distribution and dilution What is the most drug-induced Heparin-Induced Thrombocytopenia (HIT) thrombocytopenia? What are the predominant clinical symptoms Thrombocytopenia and thrombosis of HI? What are the two types of HIT that exist? 1) Nonimmune HIT: Type I 2) Immune HIT: Type II What replace the term idiopathic New standard nomenclature, immune thrombocytopenic purpura? thrombocytopenia (ITP) What is immune thrombocytopenia (ITP)? ITP is an acquired immune-mediated disorder characterized by isolated thrombocytopenia (platelet count <100 x 109/L) and the absence of any obvious initiating and/or underlying cause of the thrombocytopenia. What can contribute to the increased Intravascular coagulation, vascular injury or utilization of platelets? occlusion, and tissue injury. What rapidly consumes platelets? DIC (disseminated intravascular coagulation) What are some examples of disorders that can Trauma, obstetrical complications, and trigger the accelerated consumption of microbial sepsis. platelets? What can contribute to the In the case of bacterial sepsis, thrombin-induced thrombocytopenia? platelet aggregation in vivo contributes to thrombocytopenia. Why do vascular injuries (vasculitis) causes a Because of the direct consumption of platelets at decrease in platelets? the sites of endothelial loss without appreciable depletion of clotting factors such as fibrinogen. What is thrombotic thrombocytopenic Is a clinical syndrome with a high mortality rate purpura (TTP)? that is characterized by formation of microthrombi in the microvasculature. What are the diagnostic of the diseases TTP? The hematological findings of thrombocytopenia and red blood cell schistocytes. In TTP, coagulation testing will demonstrate 1) Normal
11 Hematology PPT Flashcards Unit 4
1) ____ prothrombin and 2) _____ partial 2) Activated thromboplastin time but 3) ______D-dimer 3) Elevated and fibrinogen levels. TTP is in contrast to DIC, which 1) Abnormal demonstrates 1) _____ prothrombin time and 2) Activated 2) _____ partial thromboplastin time. What 3 types of TTP have been identified? 1) Idiopathic 2) Secondary 3) Inherited (Upshaw-Shculman) A platelet distribution disorder can result A pooling of platelets in the spleen, which is from? frequent if splenomegaly is present. This type of thrombocytopenia develops More than a double or triple increase in platelet when? production is required to maintain the normal quantity of circulating platelets. Disorders that may produce splenomegaly Alcoholic or posthepatic cirrhosis with portal with resultant splenic pooling or delayed hypertension, lymphomas, and leukemias and intrasplenic transit include? lipid disorders, for example, Gaucher disease.
Generally defined as a substantial increase in 1) Hereditary or familial thrombocytosis circulating platelets over the normal upper associated with germline mutations of the limit of 450 x109/L. Thrombocytosis can be thrombopoietin (THPO) gene in the classified into three major categories which thrombopoietin receptor (MPL) gene are? 2) Thrombocytosis associated with myeloproliferative neoplasms and/or myelodysplastic disorders (clonal thrombocytosis associated with somatic mutations of JAK2 [V617F], MPL, and additional currently unknown genes) 3) Reactive (secondary thrombocytosis)
If platelets are normal in number but fail to A platelet dysfunction exists. perform effectively then….? In addition to both individual and family Determining a platelet dysfunctional diagnosis. medical histories, laboratory tests are critical for? What do Laboratory tests of platelet function bleeding time, clot retraction, platelet include? aggregation, platelet adhesiveness, and antiplatelet antibody assay. Three separate categories of platelet dysfunction can be identified based on? Etiology- the more common acquired causes and the less frequent hereditary causes. Hyperactive platelets associated with Abnormal platelet function. hypercoagulability and thrombosis make up
12 Hematology PPT Flashcards Unit 4 an additional category of what? Examples of inherited disorders include? Bernard-Soulier syndrome and Glanzmann thrombasthenia. What is responsible for the initial phases of Vascular response and platelet plug formation. hemostasis. Subsequent to these activities what is initiated The clotting factors to form the fibrin clot? Fibrin formation can occur if ? The activity of various factors is at least 30% to 40% of normal. Bleeding and defective fibrin clot formation A coagulation factor are frequently related to what? Disorders of the blood coagulation factors can 1) Defective production may be related to a be grouped into three categories, which are? deficiency of vitamin K. Classic hemophilia (hemophilia A) and von Willebrand disease are examples of hereditary disorders that represent functionally inactive factor VIII. 2) Excessive destruction 3) Pathological inhibition What is hemophilia ? When a clotting factor is either missing or is not working to its full ability causing for a greater chance of prolonged bleeding as well as the blood taking longer to clot Is there a cure for hemophilia No cure is a life long disease but can be treated and managed What causes hemophilia ? It is an X-linked autosomal recessive disease this means that the women are the carries and the men are affected What is hemophilia A? Clotting factor 8 is either deficient or not present What is hemophilia B? Clotting factor 9 is deficient or not present What is Von willebrand Disease ? This is when vonon willebrand clotting factor is not present this can affect both men and women
What is mild severity of hemophilia? 6%-50% of the clotting factor is active What are manifestation of hemophilia ? Hemarthrosis- bledding in the joint Hematuria- blood in the urine Ecchymosis-bruising What types of tests are done to diagnose Partial thromboplastin time (ptt) hemophilia? Typically prolonged Prothrombin time (pt) Bleeding time Fibrinogen level Platelet count Factor 8,9 and van willebrand assay Genetic testing True or false ? von willebrand disease may be True
13 Hematology PPT Flashcards Unit 4 an acquired or inherited disorder ? What distinguish von willebrand disease from A deficiency of factor V111 procoagulant classic factor V111: C ? activity Von wildebrand’s disease occurs in ____of 1-2% population ______is a major relatory mechanism of Protein C (PC) hemostasis Pts who have herediatary protein Cor S Skin necrosis deficiency have of what if take Coumadin? Is homozygous antithrombin deficiency No compatible with life? What is DIC ? DIC is a complication or intermediary phase of many diseases and does not constitute a disorder in itself
What include triggering events that may Alterations in the endothelium direct activation predispose patients to DIC ? of fibrinogen release of thromboplastin-like substances and erythrocyte or platelet destruction What are some examples of clinical situations Extravascular trauma abruption placentae in which tissue thromboplastin can activate advanced malignancy leukemia and retained coagulation ? fetal synf=rome Through what 4 ways does the body stop the TFPI clotting process ? antithrombin III Protein C / Protein S / Thrombomodulin Plasminogen How does Heparin help inhibit the clotting catalyzes antithrombin III's inactivation of IX, process ? X, XI, and thrombin How does TFPI (Tissue Factor Pathway complexes with factors VIIa, TF, and Xa, and Inhibitor) work ? inactivates Xa How does fibrinolysis happen ? TPA (Tissue Plasminogen Activator), which is on the surface of endothelial cells, converts plasminogen--> plasmin. Plasmin is a general protease that loves blasting proteins w/lysine residues. Fibrin has a lot of lysine residues, so it looks particularly sexy to plasmin (high affinity). It turns what was once a cold-hearted insoluble clot all soluble and easygoing, and D- dimers float around. What is disseminated intravascular A life-threatening uncontrolled activation of the coagulation coagulation system What are some characteristics of DIC 1. Widespread small vessel thrombosis 2. Consumption of platelets and factors 3. Uncontrolled bleeding due to depletion of platelets and coagulation factors
14 Hematology PPT Flashcards Unit 4
4. organ failure What is DIC caused by? Various clinical conditions that activate clotting mechanisms:InfectionsHemorrhageShockSeptic shock Is DIC a primary or secondary? DIC is never a primary condition. It is always secondary to another problem (ex: a person in septic shock would have DIC as a consequence Describe the onset and end result of DIC Stimulation of clottiing --> Thrombosis emboli formation --> Vascular occlusion --> Organ/tissue ischemia --> Infarction --> Necrosis Why is DIC considered a consumptive Because there's a primary stimulus that colaguopathy ? stimulates the body to think that it has a major issue where it needs to form clots (may be true in some cases for a trauma patient that is actively bleeding)As the small clots consume coagulation proteins and platelets, normal coagulation is disrupted and abnormal bleeding occurs from the skin What does consumption of coagulation Bleeding factors and platelets result in? Why does hemorrhage occur? Because platelets and coagulation factors are no longer present What occurs in all preestablished clots? Clot is programmed to break down and Fibrinolysis starts How type of cycle is DIC? Vicious cycle of clotting and bleeding
What are two abnormal coagulation Thrombocytopenia (decrease in platelets)and profiles that decrease? Decreased clotting factors (any Roman numeral, fibrinogen, or thrombin)
What are two abnormal coagulation Increased clotting measurements/ amount of profiles that increase? time (Prothrombin time, Partial prothrombin time, bleeding times)andIncreased Fibrin Degradation Products (FDPs) or Fibrin Split Products (FSPs)-->D-Dimer is specifically measurable with FDP to indicate Fibrinolysis How should DIC be evaluated? Monitor CBC for evolving and worsening anemia*The anemia will normally be Normocyctic normochromic from acute hemorrhage situation What are some treatments for DIC? What are some treatments for DIC?
15 Hematology PPT Flashcards Unit 4
Remove percipitating primary) problem (because DIC is secondary consequenceRestore balance between coagulation and fibrinolysis Maintain organ viability Administer anti- coagulants (heparin) What is responsibility of hematology Gross physical examination, total cell count, technicians and technologists? microscopic examination, and other special tests
Where are chemical analyses and Examinations are generally performed in the microbial and cytological examinations? chemistry, microbiology, and cytology departments, respectively
Where sterile body fluid can be found? It found in various body cavities under normal conditions. In diverse disorders and disease processes, the quantity of these fluids can increase significantly. Fluid specimens aspirated from different anatomical sites and examined for the total number of cells, differentiation of cell types, chemical composition, and microbial contents.
How all body fluids are should be Standard precautions must be practiced. handled with caution?
What are the type of examination the body fluid depends on the source of the performed on the body fluid depends specimen. However, a portion of the on? examination of cerebrospinal fluid (CSF); serous fluids from the pleural, pericardial, and peritoneal cavities; synovial fluid; and seminal fluid is frequently performed in the hematology laboratory.
What the most is commonly analyzed body Cerebrospinal Fluid fluid?
How cerebrospinal fluids (CSF) are acts? CSF acts as a shock absorber for the brain and spinal cord, circulates nutrients, lubricates the central nervous system (CNS), and may also contribute to the nourishment of brain tissue.
16 Hematology PPT Flashcards Unit 4
Where cerebrospinal fluids (CSF) are The CSF circulates through the ventricles and circulates through? subarachnoid space that surrounds both the brain and the spinal cord. The ventricles consist of four hollow, fluid-filled spaces inside the brain. A lateral ventricle lies inside each hemisphere of the cerebrum What CSF is production? Primarily a function of the choroid plexus, with a smaller proportion being derived from the ependymal lining and perivascular spaces What the plexus is composed of two layers? The ependyma (the lining epithelium of the ventricle) and the pia mater. The plexuses in the lateral ventricles are the largest and produce most of the CSF. What make constitute the anatomical The choroid plexus epithelium and the structure of the blood-brain barrier? endothelium of capillaries in contact with CSF. Where CSF is found? Inside all the ventricles, in the central canal of the spinal cord, and in the subarachnoid space around both the brain and the spinal cord. How many the total maximum volume of About 150 mL. The maximum volume in CSF in adults is? neonates is approximately 60 mL. How to measure CSF? Introducing a needle into the subarachnoid space makes it possible to measure CSF pressure and to obtain fluid for analysis. How a specimen of CSF is examined? A specimen of CSF is examined visually and microscopically. The total number of cells can be enumerated, and the types of cells can be morphologically distinguished. .Gross physical examination • Turbidity • Color • Viscosity • Microscopic examination: cellular enumeration
What normal CSF is contains? A few mononuclear cells (lymphocytes and monocytes) and rare ependymal cells. Very few leukocytes should be seen in normal CSF. The generally accepted total number of WBCs in the CSF ranges from 0 to 5 cells/mL or 0 to 5 × 106/L. A value of up to 20 x106/L can be considered within the range of normal for
17 Hematology PPT Flashcards Unit 4
children and adults. Neonates have a higher normal range, 0 to 30 cells × 106/L. How many WBC count are low or high? Occasionally, the WBC count may be very low (0 to 20 × 106/L), but the CSF is turbid because of a high concentration of bacteria. In acute, untreated bacterial meningitis, the CSF leukocyte count usually ranges from 100 to 10,000 cells × 106/L. Very high WBC counts (greater than 50,000 × 106/L) are unusual and suggest intraventricular rupture of a brain abscess. Cells Unique to the Cerebrospinal Fluid • Ependymal cells Choroidal cells Body fluids that are analyzed in the Pleural, Peritoneal, and Pericardial hematology laboratory. Fluids What is an effusion? An effusion is an abnormal accumulation of fluid in a particular space of the body. Effusions in the pleural, pericardial, and peritoneal cavities are divided into transudates and exudates. What transudates generally? Fluid has accumulated because of the presence of a systemic disease. What exudates are? Associated with disorders such as inflammation, infection, and malignant conditions involving the cells that line the surfaces of organs (e.g., lung or abdominal organs). What is pleural fluid? normally produced by the parietal pleura and absorbed by the visceral pleura as a continuous process. Although healthy individuals form 600 to 800 mL of fluid daily, the normal volume of fluid in each pleural space is estimated at less than 10 mL. Aspiration of pleural fluid is referred to as thoracentesis. How difference color between transudates Transudates are usually clear, are pale yellow, and exudates? and do not clot. In comparison, exudates can display a range of colors depending on the associated disorder. Erythrocyte and leukocyte counts They are of limited value in the differential diagnosis of pleural effusions. A massively bloody (hemorrhagic) effusion in the absence of trauma almost always suggests malignancy, or occasionally pulmonary infarct. How WBC count are effect transudates and Extremely elevated total leukocyte (WBC) exudates counts of 50.0 × 109/L or higher are consistent
18 Hematology PPT Flashcards Unit 4
with a diagnosis of empyema. In general, WBC counts less than 1.0 × 109/L are associated with transudates, and WBC counts greater than 1,000 × 109/L are associated with exudates. Cell types that can be encountered in the Neutrophils (PMNs) examination of a Wright-Giemsa–stained Eosinophils specimen include the following: Basophils Lymphocytes Plasma cells Mononuclear phagocytes (monocytes, histiocytes, and macrophages) Mesothelial cells (normal, reactive, atypical, and malignant) Metastatic tumor (malignant) cells What is peritoneal Fluid? A body fluid that is analyzed in the hematology laboratory. How about an abnormal amount of fluid (an It can accumulate in the peritoneal cavity if the effusion)? balance between fluid formation and reabsorption is altered by a disease process. What are result of the collection of fluid in Results from increased hydrostatic pressure in the peritoneal cavity, ascites? the systemic circulation, increased peritoneal capillary permeability, decreased plasma oncotic pressure, or decreased fluid reabsorption by the lymphatic system. What are causes of Peritoneal Effusions? The causes of peritoneal effusions range from disorders and diseases that directly represent involvement of the peritoneum, such as bacterial peritonitis, to abdominal conditions that do not directly involve the peritoneum, such as hepatic cirrhosis, cirrhosis, congestive heart failure, Budd-Chiari syndrome, hypoalbuminemia (caused by nephrotic syndrome or protein-losing enteropathy malnutrition), and miscellaneous disorders such as myxedema, ovarian diseases, pancreatic disease, and chylous ascites. How can effusions that may conform with the Can be associated with congestive heart failure, definition of transudates? hepatic cirrhosis, and hypoproteinemia. What the laboratory are criteria for less clearly defined for peritoneal (ascitic) fluid distinguishing transudates from exudates? than for pleural fluid. How difference baboratory Analysis of Transudates are usually clear and pale yellow. transudates and exudates? Exudates are cloudy or turbid because of an increased concentration of leukocytes, elevated protein levels, and occasionally microorganisms. Exudates may be seen in peritonitis, cases of perforated or infarcted
19 Hematology PPT Flashcards Unit 4
intestine, and pancreatitis. What includes of an evaluation of ascitic fluid gross inspection, total cell count, microscopic in? examination of sediment for cell differentiation, cytological studies, chemical analysis for constituents such as total protein and lactic dehydrogenase, and microbial culture. What is total WBC count higher than 0.3 × Total WBC counts are of limited value in 109/L? differential diagnosis, but a total WBC count higher than 0.3 × 109/L is considered to be abnormal. What is A wide variation in the peritoneal It seen in patients with chronic liver disease WBC count? because of extracellular shifts in fluid associated with ascites formation or resolution. An abnormal accumulation of fluid in the pericardial effusion cavity, a ?, is most frequently caused by damage to the lining of the cavity and increased capillary permeability. In addition, in acute pericarditis, interference pericardial with ? venous and lymphatic drainage predisposes the patient to effusion development. A wide variety of diseases and disorders can pericardial produce ? effusion. Normal fluid is 1 and 2. Hemorrhagic 1. Transparent (bloody) effusions may result from a variety 2. pale yellow of abnormal conditions or from aspiration of intracardiac blood into the specimen. On visible examination, a hemorrhagic pseudochylous effusion should not form clots in a plain (nonanticoagulant) tube, but aspirated blood usually exhibits clotting. A milky-appearing effusion may be a true or ? fluid. Erythrocyte and leukocyte cell counts are of pericardial effusion limited value in the differential diagnosis of a ?. A ? is a body fluid that is analyzed in the Seminal fluid hematology laboratory. Seminal fluid (semen) is examined 1 and 2. 1. macroscopically 2. microscopically Semen analysis is the primary test for the subfertile, of indeterminate fertility, or fertile. evaluation of male infertility. Sperm concentration, motility, and morphology can be used to classify men as what other 3 categories ? also can be analyzed for a variety of Semen
20 Hematology PPT Flashcards Unit 4 reasons, including artificial insemination protocols, postvasectomy assessment, and evaluation of probable sexual assault. A fresh specimen is needed. It is mandatory 37°C that the specimen be kept at ?°C and examined within 1 hour of collection. After 60 minutes of storage in a plastic container, sperm motility is significantly reduced. Is the following macroscopic or microscopic? Macroscopic A fresh specimen should be examined for coagulum formation, color, pH, volume, and viscosity. Is the following macroscopic or microscopic? microscopic Enumeration of the number of sperms and examination of the morphological characteristics of the cells are routinely performed procedures. Other microscopic procedures include motility, viability, and agglutination studies. What type fluid is a transparent, viscous fluid Synovial (joint) secreted by the synovial membrane. This fluid is found in joint cavities, bursae, and tendon sheaths Arthrocentesis constitutes a liquid biopsy joint of the ?.
Disorders such as gout, calcium systemic lupus erythematosus (SLE). pyrophosphate dihydrate (CPPD) deposition disease, and septic arthritis can be diagnosed definitively by synovial fluid analysis and may allow for consideration or exclusion of rheumatoid arthritis and ? Synovial fluid is readily obtained by ? from aspiration most joints. Frequent sites of ? include the knee, shoulder, elbow, wrist, interphalangeal joints, hip, and ankle. Routine analysis of synovial fluid should microbiological include microscopic examination of a wet preparation, crystals, Gram stain, and ? culture. If the fluid is very turbid, or if septic arthritis 1. Gram stain is considered for other reasons, the specimen 2. culture should be sent for 1. And 2.? True or False? A Gram stain is needed if a – True high likelihood of infection exists. Other observations or procedures can include – Gross
21 Hematology PPT Flashcards Unit 4 volume and appearance, viscosity, mucin test, chemical analysis for protein, and glucose. This is what type of examination? Normal, noninflammed joints have small – appearance quantities of clear or transparent fluid. This fluid is viscous and slightly alkaline and, if normal, does not clot. This describes what? The best use of the ? test is to distinguish the – mucin clot anatomical origin of bloody or other fluids. The presence of a mucin clot implies that it is synovial fluid. A differential cell count on a body fluid – hemocytometer should be performed on stained smears prepared from a concentrated preparation— not in a ?. Some of the techniques of sediment preparation and staining are different for body fluids than for blood. Morphological descriptions of cells 1. Wright encountered in body fluids reflect their 2. Wright-Giemsa stain. microscopic appearance with 1. or 2? The coloration of cells with Papanicolaou • Cytological stain is somewhat different. Papanicolaou stain is a commonly used what type of stain? The following describe what type of CLSI Pricedural Format format? • Procedure title and specific method • Test principle including type of reaction and the clinical reasons for the test • Specimen collection and preparation • Reagents, supplies, and equipment • Calibration of a standard curve • Quality control • Procedure • Calculations • Reporting results (normal values) • Procedure notes including sources of error, clinical applications, and limitations of the procedure • References
T or F? All specimens should be treated True with caution. All blood, tissues, and blood derivatives should be considered potentially infectious. A stained smear is examined to determine morphology
22 Hematology PPT Flashcards Unit 4
the percentage of each type of leukocyte present and assess the erythrocyte and platelet ?. Increases in any of the normal leukocyte leukemia. types and the presence of immature leukocytes or erythrocytes in peripheral blood are important diagnostically in a wide variety of inflammatory disorders and ? Erythrocyte abnormalities are clinically anemias. important in various ?. Platelet size irregularities are suggestive thrombocyte of particular what type of disorders? Disorders associated with increases or Increase decrease in normal leukocyte types? • • Neutrophils Bacterial infections, inflammation, stress, and chronic leukemia • Lymphocytes Viral infections, whooping cough, and chronic leukemia • Monocytes Tuberculosis, rheumatoid arthritis, and fever of unknown origin • Eosinophils Active allergies and invasive parasites • Basophils Ulcerative colitis and hyperlipidemia
The packed cell volume (PCV) is a capillary or venous blood measurement of the ratio of the volume occupied by the RBCs to the volume of whole blood in a sample of ?. Following centrifugation, this ? is measured ratio and expressed as a percentage or decimal fraction. The ? is used to calculate the mean PCV corpuscular volume (MCV) and the mean corpuscular hemoglobin concentration (MCHC).
23 Hematology PPT Flashcards Unit 4
True or False? The PCV is used to detect True anemia, polycythemia, hemodilution, or hemoconcentration.
Name the 11 elements that the CLSI • Procedure title and specific method Procedural Format must have. • Test principle • Specimen collection and preparation • Reagents, supplies, and equipment • Calibration of a standard curve • Quality control • Procedure • Calculations • Reporting results (normal values) • Procedure notes • References What must be included in Test Principle? • Type of reaction and Clinical reasons for the test What must be included in the Procedure • Sources of error, clinical applications, Notes? and limitations of the procedure. How must all specimens be treated? • With Caution
What specimens should be considered • All blood, tissues, and blood derivatives. potentially infectious? What are the 5 basic procedures in • Leukocyte differential count Hematology? • Packed cell volume of whole blood • Red blood cell indices • Reticulocyte count • Sedimentation rate of erythrocytes What is the principle of Leukocyte To determine the percentage of each type of Differential Count? leukocyte present and assess the erythrocyte and platelet morphology Increases in any of the normal leukocyte A wide variety of inflammatory disorders and types and the presence of immature leukemia. leukocytes or erythrocytes in peripheral blood are important diagnostically in what? What are erythrocyte abnormalities are Various anemias clinically important in? Platelet size irregularities are suggestive of Thrombocyte disorders what? Disorders associated with Neutrophils are? Bacterial infections, inflammation, stress, and chronic leukemia Disorders associated with Lymphocytes are? Viral infections, whooping cough, and chronic leukemia Disorders associated with Monocytes are? Tuberculosis, rheumatoid arthritis, and fever of unknown origin Disorders associated with Eosinophils are? Active allergies and invasive parasites
24 Hematology PPT Flashcards Unit 4
Disorders associated with Basophils are? Ulcerative colitis and hyperlipidemia How to you read a slide when doing a Up, Across, Down, Across differential count? What is packed cell volume (PCV)? A measurement of the ratio of the volume occupied by the RBCs to the volume of whole blood in a sample of capillary or venous blood How is the ratio is measured and expressed? As a percentage or decimal fraction. What does the PCV calculate? The mean corpuscular volume (MCV) and the mean corpuscular hemoglobin concentration (MCHC). What are the PCV Reference values? Males, 0.47 L/L ± 0.07 Females, 0.42 L/L ± 0.05 What is the PCV is used to detect? Anemia, polycythemia, hemodilution, or hemoconcentration What are the 3 calculations of RBC Indices? Mean corpuscular volume Mean corpuscular hemoglobin Mean corpuscular hemoglobin concentration What does Mean Corpuscular Volume It expresses the average volume (size) of an (MCV) do? erythrocyte What is the MCV Reference value? 80 to 96 fL What does Mean Corpuscular Hemoglobin It expresses the average weight (content) of (MCH) do? hemoglobin in an average erythrocyte. What is MCH directly proportional to? The amount of hemoglobin and the size of the erythrocyte. What is the MCH Reference value? 27 to 32 pg
What does Mean Corpuscular Hemoglobin It expresses the average concentration of Concentration (MCHC) do? hemoglobin per unit volume of erythrocytes. What does the MCHC defined as the ratio of? The weight of hemoglobin to the volume of erythrocytes. What is the MCHC Reference value? 32% to 36% How do you calculate MCHC? Hemoglobin (g / dL) MCHC= = g / dL PCV or hematocrit (L / L) What is a reticulocyte? An erythrocyte still possessing RNA What is Renumeration of reticulocytes Assessing the status of erythrocyte production important in? in the bone marrow (erythropoiesis). What type of stain is new methylene blue N? Supravital stains What does new methylene blue N cause? Ribosomal and residual RNA to co-precipitate with the few remaining mitochondria and ferritin masses in living young erythrocytes to form microscopically visible dark-blue clusters and filaments. What is Reticulum? Clusters and filaments. What is the Reference value of Reticulocytes 0.5% to 1.5%; neonates, 2.5% to 6.5% in methyl blue?
25 Hematology PPT Flashcards Unit 4
Name 2 disorders associated with abnormal Decreased reticulocytes - Aplastic anemia reticulocyte results. Increased reticulocytes - Acute blood loss What does Sedimentation rate measures? The rate of settling of erythrocytes in diluted human plasma What does Sedimentation rate depend on? An interrelationship of variables, such as the plasma protein composition, the concentration of erythrocytes, and the shape of the erythrocytes. What is the clinical value of this procedure? It is in the diagnosis and monitoring of inflammatory or infectious states. What are 2 other names for Sedimentation ESR and Sedrate Rate of Erythrocytes? What is ESR directly proportional to? The weight of the cell aggregate and inversely proportional to the surface area. Which sediments more slowly, microctytes or Microcytes macrocytes? Name 3 factors that contribute to decrease in The removal of fibrinogen by ESR. defibrination Erythrocytes with abnormalities o Erythrocytes with irregular shapes Name 3 irregular erythrocyte shapes. Sickle cells Spherocytes Hinder rouleaux When is an increased ESR value seen various abnormal blood conditions: rouleaux, increased fibrinogen levels, a relative increase of plasma globulins caused by the loss of plasma albumin, and an absolute increase of plasma globulins. What are some clinical conditions associated a) Anemia, infections, inflammation, tissue with increased ESR values? necrosis, pregnancy, and some types of hemolytic anemia Give an example of tissue necrosis. b) Myocardial infarction. Name 10 Specialized hematology procedures. • Acidified serum lysis test • Bone marrow examination • Donath-Landsteiner screening test • Glucose-6-phosphate dehydrogenase activity in erythrocytes • Hemoglobin electrophoresis • Hemoglobin S screening test • Malarial smears • Monospot test • Osmotic fragility of erythrocytes • Sucrose hemolysis test What test is Acid serum lysis called? HAM test How do you test for hemolysis? Erythrocytes are incubated with fresh and heated
26 Hematology PPT Flashcards Unit 4
serum Weak acid is used in specific serum cell Hemolytic activity. mixtures to maximize what? The presence of hemolysis may be observed Antibody-sensitized coated erythrocytes, in cases such as? spherocytes, or paroxysmal nocturnal hemoglobinuria (PNH). How is a marrow examined histologically? By using a hematoxylin-eosin (H&E) stain. Who preforms a bone marrow aspiration? A physician What does the physician examine in the bone Cellular activities of the marrow marrow? What Stain(s) is used on bone marrow Wright-Giemsa stain examinations? Prussian blue and cytochemical stains What is bone marrow examination? Is valuable in the diagnosis of disorders and in the study of leukemia’s and some types of anemia specifically involving the marrow Give an example of a bone marrow Multiple myeloma. examination. What's the normal distribution of bone Rubricytes, neutrophils, lymphocytes, marrow cells in an adult? monocytes, megakaryocytes, reticulum cells, plasma cells, myeloid, erythroid What is the myeloid:erythroid ratio? M/E ratio 2.5:1 The Donath-Landsteiner screening antibody Cold incubation to exhibit hemolysis in the test requires? patient's serum. A positive result shows? Paroxysmal cold hemoglobinuria(PCH), the rarest form of autoimmune hemolytic anemia True or False: The observed rate of TRUE appearance of bright fluorescence is proportional to the blood G6PD activity. What is one of the most prevalent hereditary Glucose-6-Phosphate Dehydrogenase (G6PD) erythrocyte enzyme deficiencies? deficiency A deficiency of G6PD can produce? Drug or stress induced hemolytic anemia The movement of charged particles on Electrophoresis various media under the influence of an electric current is called? True or False: Particles move at the same FALSE speeds because of their weight and electric charge. How is hemoglobin electrophoresis useful? To identify and quantify hemoglobin variants and abnormal quantities of hemoglobin fractions A hemolysate prepared from intact Cellulose acetate erythrocytes is placed on which medium? What describes a biphasic system with an Hemoglobin S Screening Test upper organic phase of toulene and a lower aqueous phase of phosphate buffer, saponin, and reducing agents? How are erythrocytes lysed? By toluene and saponin
27 Hematology PPT Flashcards Unit 4
The released hemoglobin is reduced by? Sodium hydrosulfite The resulting colors of the aqueous phase and AA, AS, and SS the interface phase allow for the differentiation of which hemoglobin types? True or False: Detection of the abnormal Hb TRUE S is diagnostic of sickle cell disease. The detection of this heterozygous state is Long distance runners, test pilots important to which individuals? Thick and thin blood smears are prepared, Plasmodium malariae, P. vivax, P. falciparum, stained and examined microscopically for P. ovale which malaria types? What is the diagnosis of malaria based on? The demonstration of the Plasmodium species in the blood. What is based on agglutination of horse Monospot Test erythrocytes by heterophile antibody in infectious mononucleosis? How is the specific heterophile antibody By differential absorption of the patient's serum distinguished from the Forssman type? Serum or plasma is absorbed with? Both guinea pig kidney and beef erythrocyte stroma What does Guinea pig kidney absorb? Only heterophile antibodies of the Forssman type What does beef erythrocytes absorb? Only the heterophile antibody of infectious mononucleosis A positive reaction for heterophile antibody Agglutination of horse RBCs by the absorbed occurs when? patient specimen happens Agglutination of horse RBCS by the absorbed A positive reaction patient specimen indicates____ for heterophile antibody Guinea pig kidney contains only the ___ and Forssman antigen, antigen associated with beef erythrocytes contain only the __ infectious mononucleosis Whole blood is added to varying Osmotic fragility test concentrations of sodium chloride solution and allowed to incubate at room temperature in the ____ test? How is the amount of hemolysis determined? By examining the supernatant fluid either visually or with a spectrophotometer The main factor in this procedure is? The shape of the erythrocyte The shape of the erythrocyte depends on? The volume, surface area, functional state of the erythrocytic membrane True or False: The fragility of erythrocytes is TRUE increased when the rate of hemolysis is increased True or False: If the rate of hemolysis is FALSE increased, the erythrocytic fragility is
28 Hematology PPT Flashcards Unit 4 decreased Which test demonstrates the sensitivity of Sucrose Hemolysis Test erythrocytes to the protein complement? When do erythrocytes in PNH lyse? When exposed to serum solutions of low ionic strength containing complement Which cells are tartrate resistant? Hairy cell leukemia, Sezary syndrome, some T- cell acute lymphoblastic leukemias Most of the acid phosphatase isoenzyme is L-tartaric acid inhibited by? Where are peripheral blood or bone marrow In a solution of naphthol As-BI phosphoric acid smears fixed and incubated? and fast garnet GBC salt True or False: Lymphocytes display more FALSE activity than other leukocytes. Leukocyte alkaline phosphatase(LAP) Leukemoid reactions and chronic granulocytic activity is often used to distinguish? (myelogenous) leukemia In a variety of conditions LAP activity can be Increased, normal, or decreased ___? What is the leukocyte alkaline phosphatase Leukemoid reactions and chronic granulocytic (LAP) procedure often used to distinguish? (myelogenous) leukemia Which best describes esterases? Ubiquitous in nature and encompass a variety of different enzymes acting on selective substrates This method distinguishes what? Cells of the granulocytic series from cells of the monocytic series, useful in differentiation of leukemias How are positive reacting cells differentiated Sodium fluoride is incorporated with the from monocytes? incubation system. In the alpha- naphthyl acetate esterase Blood or bone marrow smears procedure, which is incubated with naphthol AS-D chloroacetate? Naphthol compounds are coupled with what? Diazonium salt, forming highly colored deposits at the sites of enzyme activity Which represent unstable types of Heinz bodies hemoglobin, denatured by dyes and appear as intraerythrocytic stained bodies? How are Heinz bodies formed? When the glycolytic enzymes in the erythrocytes are unable to prevent the oxidation of hemoglobin What is the significance of increased numbers Unstable forms of hemoglobin in hemolytic of Heinz bodies? disorders such as G6PD. What happens shortly after birth to the It decreases to low levels amount of fetal hemoglobin (Hb F)? Increased amounts of Hb F are found in Sickle cell anemia, thalassemias, and hereditary which conditions? persistence of fetal hemoglobin What happens when leukocytes are treated When treated with periodic acid, glycols are with Periodic Acid–Schiff (PAS)? oxidized to aldehydes. After reaction with Schiff’s reagent (a mixture of pararosaniline and
29 Hematology PPT Flashcards Unit 4
sodium metabisulfite) a pararosaniline adduct is released that stains the glyco-containing cellular elements. Clinically, the PAS stain is helpful in recognizing some cases of erythroleukemia and acute lymphoblastic leukemia. How is Myeloperoxidase (MP) detected? Myeloperoxidase (MP) is detected by means of the enzyme’s interaction with diaminobenzidine (DAB), a benzidine substitute. The brown reaction product is first intensified with copper salts followed by Gill’s modified Papanicolaou stain, which results in intense gray-black granules at sites of neutrophil and monocyte myeloperoxidase activity. This procedure differentiates cells of lymphoid origin from granulocytes and their precursors and monocytes. What is the Prussian blue reaction? The Prussian blue reaction precipitates free iron into small blue or blue-green granules in erythrocytes. Free iron is not identifiable on Wright-stained or Wright-Giemsa–stained blood smears. What is a sideroblast ? A sideroblast or siderocyte is an immature or mature erythrocyte containing free iron. Increased numbers of siderocytes are seen in disorders such as thalassemia major or in patients after a splenectomy. When does a ring sideroblast occurs? If the iron granules encircle the nucleus of the erythrocyte, it is referred to as a ring sideroblast. Although alcoholism is the most common cause of ring sideroblasts, they may also be seen in cases of lead poisoning or anemia. When is a Sudan Black B Stain performed? Following fixation, blood or bone marrow films are immersed in a buffered Sudan black B solution. After rinsing, slides are counterstained with Mayer hematoxylin. Cells are examined microscopically for the presence of blue-black discrete granulation. Cells committed to the lymphoid pathway display negative staining reactions, whereas myeloid and monocytoid forms display characteristic positive reactions. The Sudan black B staining pattern usually parallels the myeloperoxidase stain and is useful in the identification of myelogenous and myelomonocytic leukemias. What is a Terminal Deoxynucleotidyl Terminal deoxynucleotidyl transferase (TdT) is
30 Hematology PPT Flashcards Unit 4
Transferase Test and where is it found? a non–template-directed DNA polymerase that catalyzes the irreversible addition of deoxynucleotides to the 3-hydroxy groups on the end of DNA. The primary methods of detection are immunofluorescence and immunoperoxidase using a monoclonal antibody. TdT is a cell marker found on immature and neoplastic cells frequently seen in leukemic states. What is a Specimen quality procedure? All coagulation testing critically depends on the quality of the specimen. Minimum tissue trauma and the avoidance of hemolysis are essential. Proper phlebotomy techniques must be strictly followed. What is a Special collection techniques? To reduce the possibility of introducing tissue thromboplastin into a whole blood sample and the subsequent utilization of certain factors with clot formation, certain techniques should be followed. What are some general sources of error? All procedural directions must be strictly followed because variations in pH, reagent concentration, and temperature are major sources of error. How is quality control maintained? Water baths and heat blocks must be monitored continually for accurate temperatures. Refrigerators and freezers should also be monitored to ensure the stability of specimens and test reagents. Reagents must not be beyond their stated expiration date. Procedural technique must be consistent and appropriate. List some of the Coagulation Procedures Activated partial thromboplastin time, Antithrombin III, Bleeding time, Circulating anticoagulants, D-dimer assay, Euglobulin lysis time, Substitution studies and factor assays,Fibrin split products, Fibrinogen assay Describe the principle of the Activated Partial The aPTT procedure measures the time required Thromboplastin Time procedure to generate thrombin and fibrin polymers via the intrinsic pathway. Although a partial thromboplastin time test can be performed, contact factors can be activated more thoroughly by the addition of substances such as kaolin in the activated form of this assay. In the aPTT, calcium ions and phospholipids that substitute for platelet phospholipids are
31 Hematology PPT Flashcards Unit 4
added to blood plasma. The generation of fibrin is the end point. How is the aPTT used? –Clinically, the aPTT is used to identify and quantitate deficiencies in the intrinsic clotting system and to control anticoagulant therapy.
How are the aPTT results reported? Reference values are dependent on the activator and phospholipid reagents used; however, 20 to 35 seconds is typically normal. In some laboratories, ranges may be from 28 to 42 seconds, with 42 to 46 seconds being marginal. What are the Clinical applications of the The aPTT is widely advocated as the test of aPTT? choice for the control of heparin therapy. It is also important in the screening profile of prekallikrein; high-molecular-weight kininogen; factors XII, XI, IX, VIII, X, V, II, and I; and inhibitors against these factors. Describe the principle of the Antithrombin In the presence of heparin, thrombin is (AT III) neutralized at a rate that is proportional to the antithrombin (AT III) concentration. Following defibrination, plasma is assayed in a two-stage procedure that utilizes standardized amounts of heparin, fibrinogen, and thrombin. The resulting clotting time is interpreted using a calibration curve. Clinically, the AT III assay is useful prior to and subsequent to treatment with heparin in cases of disseminated intravascular coagulation (DIC). What is the advantage of the Bleeding Time The bleeding time test is an in vivo test? measurement of platelet adhesion and aggregation on locally injured vascular subendothelium. This test provides an estimate of the integrity of the platelet plug and thereby measures the interaction between the capillaries and the platelets. Clinically, the bleeding time is prolonged in thrombocytopenia, qualitative platelet disorders such as von Willebrand disease, aspirin ingestion, or the presence of vascular problems What is a circulating anticoagulant? When coagulation deficiencies are caused by inhibitors to specific factors rather than the lack of a factor, these inhibitors are sometimes referred to as circulating anticoagulants . How can a circulating anticoagulant be To detect a circulating anticoagulant, the aPTT detected? and the PT that were originally abnormal are repeated using various dilutions of patient
32 Hematology PPT Flashcards Unit 4
plasma and normal plasma. The detection of an inhibitor may show up immediately or may require incubation of the normal plasma in the presence of the inhibitor. Differentiation between a coagulation factor deficiency and a circulating anticoagulant is important. How can a circulating anticoagulant be If the abnormality is that of a deficiency, a reported? normal plasma sample will correct the assay results to a reference value. If the abnormality is caused by a circulating anticoagulant (inhibitor), a greater correction is demonstrated as the ratio of normal plasma increases in the mixture. What are some of the anticoagulants that may Various types of anticoagulants may interfere interfere with coagulation? with coagulation at different stages, especially factor VIII, heparin-like activity, and antithromboplastins. Most acquired anticoagulants are autoantibodies (usually IgG, sometimes IgM) directed against specific coagulation factors. What is principle of the D-dimer assay? The fundamental principle of the D-dimer assay has remained largely unchanged: recognition of the unique neoepitope in D-dimer by specific antisera. D-dimer contains a neoepitope that is formed following the cross-linking of adjacent D domains by factor XIIIa. It is this epitope that is recognized by specific antisera used in clinical assays. Explain the principle of the Euglobulin Lysis The euglobulin fraction of plasma contains Time plasminogen, fibrinogen, and activators with the potential for transforming plasminogen to plasmin. This fraction is precipitated with 1% acetic acid and resuspended in a borate solution. The euglobulins are then clotted by the addition of thrombin. The clot is incubated and the time of lysis is reported. Clinically, the euglobulin lysis test is a screening procedure for fibrinolytic activity. Describe Substitution studies Assay and how Substitution studies and factor assays can be they can be performed used to identify specific coagulation factor deficiencies. Substitution studies may be performed using adsorbed plasma and aged serum with the aPTT to identify deficiencies of blood coagulation. Substitution studies may also be performed
33 Hematology PPT Flashcards Unit 4
using adsorbed plasma with the PT to identify a factor VII deficiency. What is the principle of Specific factor Factor assays are based on the ability of the assays? plasma in question to correct a factor-deficient substrate, such as factor VIII. The actual assay is the same as the aPTT with the exception of the factor-deficient substrate. Identification of specific factor deficiencies is valuable in both the diagnosis and the treatment of patients. When conducting a Fibrin Split Products Thrombin is added to ensure complete clotting (FSP) test, what is the purpose of adding of the sample, and the soy bean enzyme thrombin as well as soy bean enzyme inhibitors are added to prevent any breakdown inhibitors to the whole blood sample? of fibrin. What is demonstrated from FSP elevated Elevated results demonstrate that the activation results? of plasmin has occurred or is occurring, such as in primary fibrinolysis and DIC with secondary fibrinolysis. What is the principle behind a fibrinogen When plasma is diluted and clotted with assay? excess thrombin, the fibrinogen concentration is inversely proportional to the clotting time Fibrinogen assays are useful in detecting deficiencies of fibrinogen and in detecting an alteration in the conversion of fibrinogen to fibrin. What is the use of the simple protein, – Protamine is used to neutralize the protamine? effects of heparin. What is the indication of a positive result – Inappropriate presence of intravascular from a Protamine Sulfate Assay? fibrin monomers What is being measured when conducting a – Length of time required to form a fibrin prothrombin time? clot (measured in seconds) What are some situations in which to monitor oral anticoagulant therapy prothrombin time test is used? as a screening test in the diagnosis of coagulation deficiencies – as a component of a liver profile assessment What is indicated from prolonged results in a Deficiency of one or more factors in the prothrombin time? extrinsic pathway: factors VII, X, and V and factor II or I. The presence of an inhibitor will also produce prolonged values. – What is determined from a thrombin time Determines the rate of thrombin-induced test? cleavage of fibrinogen to fibrin monomers and the subsequent polymerization of hydrogen- bonded fibrin polymers
34 Hematology PPT Flashcards Unit 4
What might cause the abnormal result of a Extremely low fibrinogen levels thrombin time test? Abnormal fibrinogen thrombin inhibitors High concentrations of immunoglobulin (e.g., myeloma proteins) Presence of heparin High concentrations of fibrin-fibrinogen degradation products How is cell size and quantity determined Cell counting and sizing are based on the based on the use of an electrical impedance detection and measurement of changes in procedure? electrical impedance (resistance) produced by a particle as it passes through a small aperture. Which method of cell counting uses a laser Optical Detection method light? How does the diluted blood specimen interact A diluted blood specimen passes in a steady with the laser light during optical detection? stream through which a beam of laser light is focused. As each cell passes through the sensing zone of the flow cell, it scatters the focused light. Scattered light is detected by a photodetector and converted to an electrical pulse. What is represented by the number of The number of pulses generated is directly electrical pulses detected in an optical proportional to the number of cells passing detection method? through the sensing zone in a specific period. What are the three operational processes of Diffraction and the bending of light light amplification generated by emission of around corners with the use of small radiation? angles Refraction and the bending of light because of a change in speed with the use of intermediate angles Reflection and light rays turned back by the surface or an obstruction with the use of large angles How is Radio Frequency (RF) used to detect – High-voltage electromagnetic current is cell size? used to detect cell size, based on the cellular density. Why is laser light the most common light – Because of the properties of intensity, source used in flow cytometers? stability, and monochromatism. What is flow cytometry? – The simultaneous measurement of multiple physical characteristics of a single cell, as the cell flows in suspension through a measuring device. How can flow cytometry rapidly classify – Flow cytometry combines the groups of cells? technologies of fluid dynamics, optics, lasers, computers, and fluorochrome- conjugated monoclonal antibodies that rapidly classify groups of cells with
35 Hematology PPT Flashcards Unit 4
heterogeneous mixtures. In flow cytometry, what intrinsic properties of – Forward- and right-angle light scatter, a cell are detected? which correlate with size and granularity of a cell, respectively. Regarding scattered light, what is a forward – Light scattered along the axis of the laser scatter? beam Regarding scattered light, what is a side/ – Light scattered perpendicular to the axis orthogonal scatter? Forward scatter is proportional to? – Cell size Side scatter is proportional to? – Cytoplasmic granularity Define parameter: – Statistical term that refers to any numerical value that describes an entire population. Major types of automation are representations Representative of the ways that blood cells can of what? be counted, leukocytes differentiated, and other components (e.g., MCH and MCHC) calculated How does hemoglobin being measured? Measured by the traditional cyanmethemoglobin flow-cell method at 525 and 546 nm, depending on the instrument manufacturer What are histograms? Histograms are graphic representations of cell frequencies versus sizes. In a homogeneous cell population, the curve A symmetrical bell-shaped or gaussian assumes what shape or distribution? distribution. In a histogram, a wide or more flattened curve A wide or more flattened curve is seen when the is seen in what? standard deviation from the mean is increased. True or false. True Histograms not only provide information about erythrocyte, leukocyte, and platelet frequency and their distribution about the mean but also depict the presence of subpopulations. True or False True Histograms provide a means of comparing the sizes of a patient’s cells with normal populations. True or False. True In a histogram, shifts in one direction or the other can be of diagnostic importance. Tue or False False (x-axis represents the size) In the Coulter system, the size (volume in femtoliters) is represented on the y-axis. In analysis of instrumental data output The erythrocyte histogram includes what? Quantitative descriptors of erythrocytes The leukocyte histograms Platelet histograms Derived platelet parameters
36 Hematology PPT Flashcards Unit 4
What does an erythrocyte histogram reflects? The erythrocyte histogram reflects the native size of erythrocytes or any other particles in the erythrocyte size range. The erythrocyte histogram in the Coulter 1) 24 fL system displays cells as small as __(1)___fL., 2) 36 fL but only those greater than ___(2)___fL are counted as erythrocytes. In a erythrocyte histogram, what is the It allows for the detection of erythrocyte advantage of the extension of the lower end fragments, leukocyte fragments, and large of the scale from 36 to 24 fL? platelets An expression of erythrocyte size is the RDW ______in the Coulter series. This term refers to variation in erythrocyte size. Correlations between the ______and the RDW and the MCV ______exist for various types of anemia. What does size-referenced leukocyte The classification of leukocytes according to histograms displays? size following lysis. It does not display the native cell size What does a platelet histogram reflects? Platelet counting and sizing in both the electrical impedance and the optical systems reflect the native cell size. What is the measure of the average volume of MPV platelets in a sample? True or False True The MPV is analogous to the erythrocytic MCV. True or False True Mean platelet volume calculation is derived from the same data as the platelet count. True or False True In healthy patients, there is an inverse relationship between platelet count and size. What are the three steps in a laser Cytochemical reactions prepare the blood cells technology? for analysis. A cytometer measures specific cell properties. Algorithms convert these measurements into familiar results for cell classification, cell count, cell size, and hemoglobinization. RBC/platelet channel uses a laser-based The basophil/lobularity channel. optical assembly that is shared with what channel? Where is the platelet histogram derived? The platelet histogram is derived from measurements made with the high-angle detector. What is the mode of the measured platelet MPV volumes?
37 Hematology PPT Flashcards Unit 4
Most flow-cell instruments can at the rate of 5,000 to 10,000 cells/sec. simultaneously analyze multiple parameters at what rate? In flow cytometry, the cellular analysis yields The cellular analysis yields quantitative data what properties of individual cells? about the chemical and physical properties of individual cells. Major advances in this technology are owing The ability to produce monoclonal to several factors, what are these factors? antibodies resulted in the subsequent development of specific surface markers for various subpopulations of cells. The development of new fluorescent probes for DNA, RNA, and other cellular components increased the variety of possible applications at the molecular and cellular levels. The expansion of computer applications has improved the instrumentation technology, making it easier to operate and more practical for use in clinical as well as research laboratories. In hematology, automated differentials can be – Determination of cell volume by based on a variety of principles which electrical impedance or forward light includes what? scatter, cytochemistry or peroxidase staining, and VCS technology. Because single-cell suspensions of peripheral – hematology and immunology blood and bone marrow are easy to obtain, most clinical applications of flow cytometry are in the specialties of ______and ______. Reticulocytes Enumeration by flow cytometry – accurate, precise, and cost-effective. is more ______. Platelet counts can provide an estimate of – with an RNA dye. young, reticulated platelets by counting platelets that stain with what kind of dye? What kind of typing identified by a cluster – Immunophenotyping monoclonal designation (CD), are used in most flow antibodies cytometry immunophenotyping. A cellular application that has become an – Flow Cytometry important tool in the diagnosis and classification of hematologic neoplasia by immunophenotyping. This techniques with bone marrow cells are applicable to DNA cell cycle analysis.What is this technique? What kind of new technology that referred to – Digital Technology as automated digital cell morphology, provides an unprecedented level of efficiency
38 Hematology PPT Flashcards Unit 4 and consistency. In its simplest form, automated digital cell morphology is a process where blood cells are automatically located and preclassified into categories of blood cell? This is the earliest instruments to detect blood – Electromechanical methods clotting. This uses a methodology to measure the conduction or impedance of an electrical current by the formation of fibrin. What kind of instrumental methodology is this? This principle/methodology measures is the – Photo-optical Method change in light transmission as optical density (absorbance) versus time can be used to quantitatively determine the activity of various coagulation stages or factors. ______is defined as the resistance that a – Viscosity material has to a change in its form. This principle usesthe natural thickening – Viscosity-Based Detection System (viscosity) and monitored by the motion (VDS) (amplitude of an oscillating steel ball in a specially designed cuvette), as a change in form takes place. What type of platelet agglutination method – ristocetin cofactor assay measures the ability of a patient’s plasma to agglutinate formalin-fixed platelets in the presence of ristocetin? The principle of the test is that platelet-rich – Platelet Aggregation plasma is treated with a known aggregating agent. What is this test? A new type of automated system that – Siemens PFA-100 incorporates a high shear flow system to simulate the in vivo hemodynamic conditions of platelet adhesion and aggregation as encountered at a vascular lesion.
39