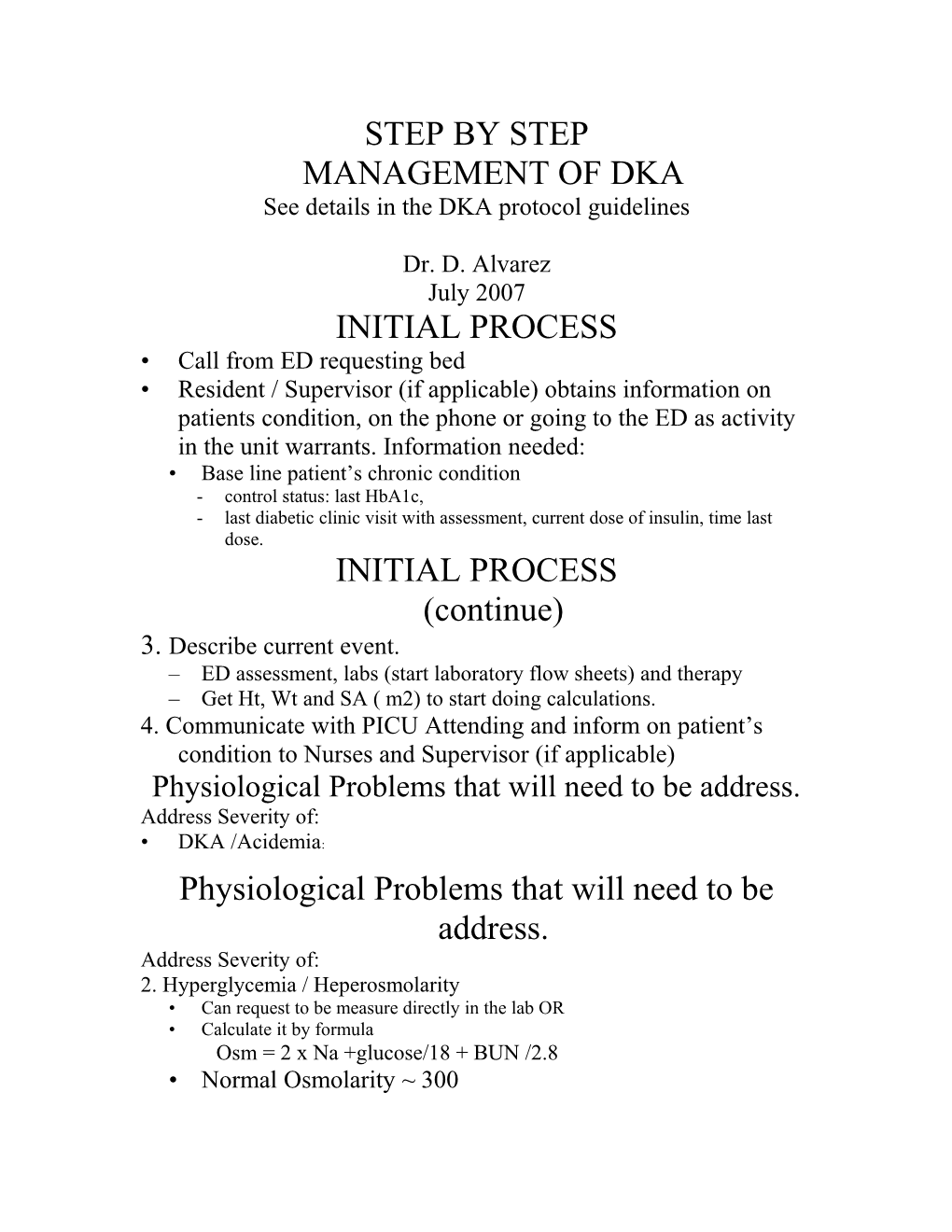
STEP BY STEP MANAGEMENT OF DKA See details in the DKA protocol guidelines
Dr. D. Alvarez July 2007 INITIAL PROCESS • Call from ED requesting bed • Resident / Supervisor (if applicable) obtains information on patients condition, on the phone or going to the ED as activity in the unit warrants. Information needed: • Base line patient’s chronic condition - control status: last HbA1c, - last diabetic clinic visit with assessment, current dose of insulin, time last dose. INITIAL PROCESS (continue) 3. Describe current event. – ED assessment, labs (start laboratory flow sheets) and therapy – Get Ht, Wt and SA ( m2) to start doing calculations. 4. Communicate with PICU Attending and inform on patient’s condition to Nurses and Supervisor (if applicable) Physiological Problems that will need to be address. Address Severity of: • DKA /Acidemia: Physiological Problems that will need to be address. Address Severity of: 2. Hyperglycemia / Heperosmolarity • Can request to be measure directly in the lab OR • Calculate it by formula Osm = 2 x Na +glucose/18 + BUN /2.8 • Normal Osmolarity ~ 300 Address Severity of: 3. Dehydration:
Address Severity of: 4. Electrolyte Imbalance: – Na: correct serum sodium level as per formula • Add 1.6 for each 100 mg/dl of glucose over 100 • Example: if Na 130 and BS of 800 – Corrected Na will be 1.6 x 700 = 11.2 – 130 + 11.2 =141 (this is the true Na, still the total body sodium is low) – K: even though the serum K may be initially high, the total body sodium is always low. – Ph and Calcium abnormalities as well MANAGEMENT Fluid Replacement Calculations • Check how much and what kind of fluids patient received in ED. (usually patient should had received NS, 20 to 40 cc/kg boluses) • Check if patient passed urine and how much and calculated Fluid Balance • Example: if patient received 1 Liter of NS and passed 1 liter of urine because hyperosmolarity; the balance is ZERO. Fluid Replacement Calculations (CONTINUES) 3. Calculate patient’s maintenance fluids (requirements); Wt. base OR per SA(m2) • Wt base: 100 ml/kg for the first 10 kg 50 ml/kg for the next 10 kg 20 ml/kg for the rest…. kg. • Per SA (m2) 1500 mL/M2 4. Calculate deficit for ideal (pre-illness) wt. Example: Pt. is 22.2 kg. Maintenance is 1540 mL Fluid Replacement Calculations (CONTINUES) 4. Calculate deficit per ideal (pre-illness wt) Example: • Pt. current (dehydrated) wt is 20 kg • Pt. is assess to be 10% dehydrated. • Ideal wt is: 22.2 kg (20 kg is 90% >>> 100 % =100 x 20 / 90) • Deficit will be 22.2 – 20 = 2.2 Liters
Fluid Replacement Calculations (CONTINUES) 4. To calculate IV rate: ml/hr – Add Maintenance + ½ of deficit (*) – 1540 + 1.1= 2640 mL in 24 hrs - IV rate of 2640/24 hr = 110 cc/hr. (*) correction should be given in 48 hrs. 5. IV solution selection: use standard solution pre-mixed by pharmacy: • There are 3 standard solutions. To select them go to> IV solution (16) > then select “IV solution (peds)” (7) >> from Solution for DKA - 0.45 NS with 20 mEq KCl and 15 mM of KPh / Liter - D5% 0.45 NS with 20 mEq KCl and 15 mM of KPh / Liter - D 10% 0.45 NS with 20 mEq KCl and 15 mM of KPh / Liter Insulin drip • Dose: 0.05 to 0.1 Units /kg/hr. Choice will depend on: • the severity of the acidosis. If severe, start with 0.1 U/kg/hr • The patient’s sensitivity to Insulin, according to age and individual response. • Solution Concentration: select standard solutions as per “Insulin drip guideline”. • Rate: select rate from pre-calculated rate charts. • RUN IT IN A SEPARATE IV LINE. FOLLOW - UP • Cardio-respiratory monitoring and Neuro checks • Neuro checks: observe for changes of metal status as signs of dehydration and or complications of DKA: Cerebral edema, strokes • Respiratory: Observe for changes/ type of respiration as sign of acidosis (Kussmaul respirations) and /or respiratory depression 2nd to CNS depression as an imminent CNS complication. • CV: Observe for signs of dehydration and / or electrolyte abnormalities, I.e. Hyper /hypokalemia. FOLLOW - UP 2. Fluid Balance • The goals of fluid therapy are: • Initial fluid resuscitation is aim to replenish intravascular volume to reverse lactic acidosis. • Slow rehydration (48 hr) and slow decrease in osmolarity to prevent risk of cerebral edema. • Divide the 24 Fluid deficit by 3 to anticipate /estimated the positive 8 hour balance to achieve. • Daily Wt will be the best objective way to assess rehydration FOLLOW - UP 3. Acid-Base-Balance – VVG and electrolytes including Ca and Ph every 2-3 hours until a steady improving trend, then it can be done Q 4hours till all normal. 4. FS Q1H as long patient is on insulin drip - Aim to have a slow decrease of BS /Osmolarity, may need to add glucose containing solution and /or use NS for a longer period of time at the beginning of rehydration. - Keep BS between 150 – 250 before changing IV solutions - At the beginning and until the acidosis is corrected, control BS with IV solutions with or without Dext. using the “2 bag system” “2 bag solutions” • Acidosis improving – No changes in Insulin drip, except for temporarily hold if low FS until corrected with Glucose solutions. – Adjust IV solution rates to keep FS Between ~150 (increase Dextrose Sol if < 100 or decrease if close to 200) • Acidosis Resolved – Patient is ready to have the insulin drip switch to SC (dose to be given by Endocrinologist) and start Diabetic Diet. – If FS is low can decrease Insulin drip instead of increase Glucose in the IV solution. – After the first dose of SC given and Pt. Ate. D/c insulin drip after 1 hr. Switching Insulin from drip to SC • Get SC dose of insulin from Endocrinologist • Order Diet as per Endo recommendations, usually: – If < 5 yo is 3 meals and 3 snack – If > 5 yo 3 meals and 2 snacks • Order initial dose as instructed, – NPH dose is usually started in AM before breakfast. – Lantus is given PM • D/C insulin drip 1 hours after SC dose given • D/C glucose in IV fluids after tolerating breakfast and BS is within normal level. • Decrease IV fluid rate to replacement rate only. • Change schedule of FS to 7 times /day as per diabetic protocol. (see guideline orders) Dextrostics (FS) monitoring when pt. in on SC insulin. 7 (times per day) • Order entry … “dextrosticks “ (Fingersticks Glucose by Nursing) • Expand… • Choose # 7 ( _ X per day) • Write 7 (times per day) • In instructions field please Write : As per diabetic protocol, using Glucometer Guidelines for ordering sliding scale Humalog insulin coverage. • Order entry • Write “Humalog” • 1) ____SC ___ Now • Expand • Route (5) • Choose #73 (subcutaneous) • 3) When • Change…. to PRN (# 34) • Write your sliding scale as per endocrinology consult • NOTE! Type your sliding scale without “ Comma” but leave space in between. • Example: Glucose 15 minutes before breast fast if glucose less 50 mg/dl 0U 51-100 5U 101-150 8U 151-200 10U 201-300 12U 301-400 14U >400 16U
Ordering insulin in relation to Carbohydrate caloric count
Example: Write 2 separate orders • 15 minutes before meal and snack administer (1) U of Humalog for each (15) gr of carbohydrate. • (1) U for each (50) mg/dl glucose level above the patient target (X) mg/dl