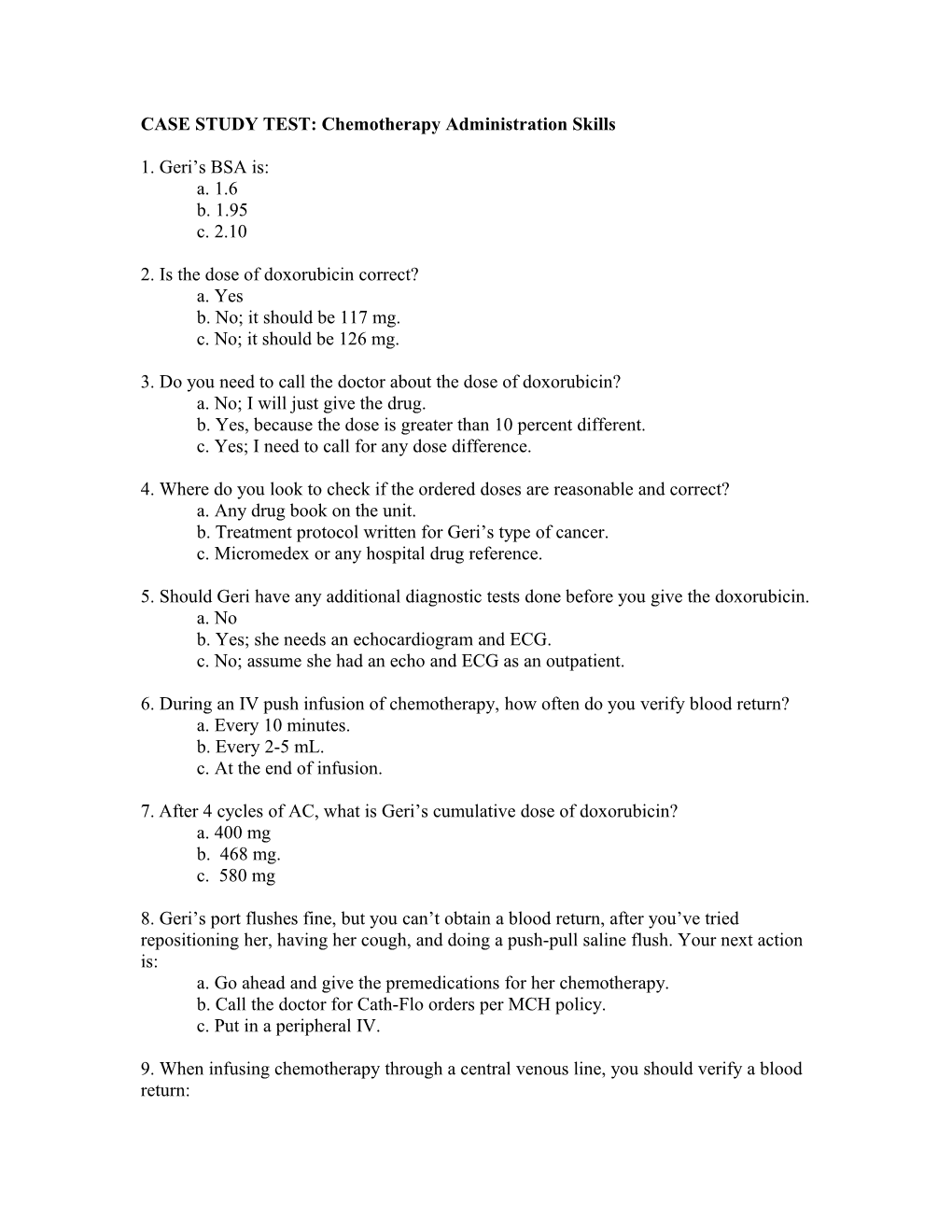
CASE STUDY TEST: Chemotherapy Administration Skills
1. Geri’s BSA is: a. 1.6 b. 1.95 c. 2.10
2. Is the dose of doxorubicin correct? a. Yes b. No; it should be 117 mg. c. No; it should be 126 mg.
3. Do you need to call the doctor about the dose of doxorubicin? a. No; I will just give the drug. b. Yes, because the dose is greater than 10 percent different. c. Yes; I need to call for any dose difference.
4. Where do you look to check if the ordered doses are reasonable and correct? a. Any drug book on the unit. b. Treatment protocol written for Geri’s type of cancer. c. Micromedex or any hospital drug reference.
5. Should Geri have any additional diagnostic tests done before you give the doxorubicin. a. No b. Yes; she needs an echocardiogram and ECG. c. No; assume she had an echo and ECG as an outpatient.
6. During an IV push infusion of chemotherapy, how often do you verify blood return? a. Every 10 minutes. b. Every 2-5 mL. c. At the end of infusion.
7. After 4 cycles of AC, what is Geri’s cumulative dose of doxorubicin? a. 400 mg b. 468 mg. c. 580 mg
8. Geri’s port flushes fine, but you can’t obtain a blood return, after you’ve tried repositioning her, having her cough, and doing a push-pull saline flush. Your next action is: a. Go ahead and give the premedications for her chemotherapy. b. Call the doctor for Cath-Flo orders per MCH policy. c. Put in a peripheral IV.
9. When infusing chemotherapy through a central venous line, you should verify a blood return: a. Before the infusion. b. Before, during (at least once per shift), and after the infusion. c. At completion of infusion.
10. You have started Geri’s paclitaxel treatment. What do you do next? a. Wish Geri well and go out to the desk to finish your charting. b. Stay with Geri for at least the first 15 minutes of treatment to watch for a hypersensitivity reaction. c. Go out to give the next nurse report; it’s time to leave!
11. What are signs of a hypersensitivity reaction? a. Redness along infusion site. b. Itching, hives, wheezing, chest pain, dyspnea, hypotension, angioedema, or tachycardia. c. Hypotension.
12. What is the appropriate apparel to be worn when giving chemotherapy or when you may be exposed to body fluids of a patient who has received chemotherapy: a. Nonpermeable, disposable gown and gloves. b. Nonpermeable, disposable gown, two pairs of gloves, and face shield. c. No special apparel required.
13. Geri was incontinent of about 50 mL of urine on her way to the bathroom. Is this treated as a hazardous drug spill? a. Yes. b. No; wear PPE and use chemo precautions guidelines to clean the urine. c. No, ask a team assistant to clean it up.
14. Chemotherapy precautions for body fluids are maintained for a. 48 hours after starting chemotherapy b. 48 hours after the last dose of chemotherapy c. For remainder of patient’s stay
15. The tubing has disconnected from the IV site, and you notice a puddle on the floor of approximately 50 mL. Your next action is to: a. Mop it up with towels. b. Don your PPE, get hazardous spill kit and place sign to warn others of a spill, call Facilities to notify them of a spill, and start laying down absorbent pads from spill kit. c. Go home, this has been a really hard day.