Shock and Circulatory Support
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Differentiating Between Anxiety, Syncope & Anaphylaxis
Differentiating between anxiety, syncope & anaphylaxis Dr. Réka Gustafson Medical Health Officer Vancouver Coastal Health Introduction Anaphylaxis is a rare but much feared side-effect of vaccination. Most vaccine providers will never see a case of true anaphylaxis due to vaccination, but need to be prepared to diagnose and respond to this medical emergency. Since anaphylaxis is so rare, most of us rely on guidelines to assist us in assessment and response. Due to the highly variable presentation, and absence of clinical trials, guidelines are by necessity often vague and very conservative. Guidelines are no substitute for good clinical judgment. Anaphylaxis Guidelines • “Anaphylaxis is a potentially life-threatening IgE mediated allergic reaction” – How many people die or have died from anaphylaxis after immunization? Can we predict who is likely to die from anaphylaxis? • “Anaphylaxis is one of the rarer events reported in the post-marketing surveillance” – How rare? Will I or my colleagues ever see a case? • “Changes develop over several minutes” – What is “several”? 1, 2, 10, 20 minutes? • “Even when there are mild symptoms initially, there is a potential for progression to a severe and even irreversible outcome” – Do I park my clinical judgment at the door? What do I look for in my clinical assessment? • “Fatalities during anaphylaxis usually result from delayed administration of epinephrine and from severe cardiac and respiratory complications. “ – What is delayed? How much time do I have? What is anaphylaxis? •an acute, potentially -

CIRCULATORY COLLAPSE - EMERGENCY (ISS MED/3A - ALL/FIN) Page 1 of 2 Pages
SHOCK - CIRCULATORY COLLAPSE - EMERGENCY (ISS MED/3A - ALL/FIN) Page 1 of 2 pages NOTE The most critical step is identifying and treating the underlying cause. Basic causes of shock are: Anaphylaxis - severe allergic reaction Heart attack Loss of circulating blood volume (bleeding, burns, dehydration) Decompression sickness Venous dilation (allergy, pain, drugs, heat stroke, infection) High or low body temperature SIGNS Pulse - rapid, weak, thready Respiration - shallow, irregular, labored Blood Pressure - low, falling Mental State - confused, sluggish, anxious Eyes - pupils may be dilated Skin - cold, clammy, sweating If no pulse or respiration, perform {CARDIOPULMONARY RESUSCITATION: CPR - EMERGENCY} (SODF: ISS MED: EMERGENCY). 1. Evaluate vital signs and record every 5 minutes every 5 minutes. Time (minutes) 0 5 10 15 20 25 30 ALSP Blood Presssure (ALSP-4) Pulse Respiratory Rate ALSP Temperature (Assessment-4) ALSP Pulse Oximeter (Assessment-3) 2. Unstow and don Non-Sterile Gloves (ALSP Airway-4,5,6). If bleeding, control by applying direct pressure using Gauze Pads (Airway-11). 3. Prevent loss of body heat with clothing, sleeping bag, warm environment. 24 AUG 00 4044.shock.circ.collapse.em.doc SHOCK - CIRCULATORY COLLAPSE - EMERGENCY (ISS MED/3A - ALL/FIN) Page 2 of 2 pages 4. Attach ECG leads. Refer to {CARDIOPULMONARY RESUSCITATION: CPR - ECG DATA STORAGE - EMERGENCY} (SODF: ISS MED: EMERGENCY). 5. Contact Surgeon. 6. If no immediate ground communication available, start IV with 1L bag Normal Saline. Fully open roller clamp assembly to allow maximum flow. Refer to {INJECTIONS - NONPOWERED INTRAVENOUS FLUID INFUSION} (SODF: ISS MED: INJECTIONS/IV). 24 AUG 00 4044.shock.circ.collapse.em.doc. -

59 Arterial Catheter Insertion (Assist), Care, and Removal 509
PROCEDURE Arterial Catheter Insertion 59 (Assist), Care, and Removal Hillary Crumlett and Alex Johnson PURPOSE: Arterial catheters are used for continuous monitoring of blood pressure, assessment of cardiovascular effects of vasoactive drugs, and frequent arterial blood gas and laboratory sampling. In addition, arterial catheters provide access to blood samples that support the diagnostics related to oxygen, carbon dioxide, and bicarbonate levels (oxygenation, ventilation, and acid-base status). PREREQUISITE NURSING aortic valve closes, marking the end of ventricular systole. KNOWLEDGE The closure of the aortic valve produces a small rebound wave that creates a notch known as the dicrotic notch. The • Knowledge of the anatomy and physiology of the vascu- descending limb of the curve (diastolic downslope) repre- lature and adjacent structures is needed. sents diastole and is characterized by a long declining • Knowledge of the principles of hemodynamic monitoring pressure wave, during which the aortic wall recoils and is necessary. propels blood into the arterial network. The diastolic pres- • Understanding of the principles of aseptic technique is sure is measured as the lowest point of the diastolic needed. downslope, which should be less than 80 mm Hg in • Conditions that warrant the use of arterial pressure moni- adults. 21 toring include patients with the following: • The difference between the systolic and diastolic pres- ❖ Frequent blood sampling: sures is the pulse pressure, with a normal value of about Respiratory conditions requiring arterial blood gas 40 mm Hg. monitoring (oxygenation, ventilation, acid-base • Arterial pressure is determined by the relationship between status) blood fl ow through the vessels (cardiac output) and the Bleeding, actual or potential resistance of the vessel walls (systemic vascular resis- Electrolyte or glycemic abnormalities, actual or tance). -
Reducing Arterial Catheters
Reducing the Risk of Catheter-Related Bloodstream Infections: Peripheral Arterial Catheters Amy Bardin Spencer, EdD(c), MS, RRT, VA-BC™ Manager, Clinical Marketing – Strategic Programs – Teleflex Russ Olmsted, MPH, CIC Director, Infection Prevention & Control, Trinity Health Paid consultant, Ethicon, BIOPATCH products Disclosure • This presentation reflects the technique, approaches and opinions of the individual presenters. This Ethicon sponsored presentation is not intended to be used as a training guide. The steps demonstrated may not be the complete steps of the procedure. Before using any medical device, review all relevant package inserts with particular attention to the indications, contraindications, warnings and precautions, and steps for use of the device(s). • Amy Bardin Spencer and Russ Olmsted are compensated by and presenting on behalf of Ethicon and must present information in accordance with applicable regulatory requirements. 0.8% of arterial lines become infected Maki DG et al., Mayo Clinic Proc 2006;81:1159-1171. Are You Placing Arterial Catheters? 16,438 per day 6,000,000 arterial catheters 680 every hour Maki DG et al., Mayo Clinic Proc 2006;81:1159-1171. 131 per day 48,000 arterial catheter-related bloodstream infections 5 patients every hour Maki DG et al., Mayo Clinic Proc 2006;81:1159-1171. Risk Factors • Lack of insertion compliance • No surveillance procedure • No bundle specific to arterial device insertion or maintenance • Multiple inserters with variations in skill set Maki DG et al., Mayo Clinic Proc 2006;81:1159-1171. -

Arterial Line
Arterial Line An arterial line is a thin catheter inserted into an artery. Arterial line placement is a common procedure in various critical care settings. It is most commonly used in intensive care medicine and anesthesia to monitor blood pressure directly and in real time (rather than by intermittent and indirect measurement, like a blood pressure cuff) and to obtain samples for arterial blood gas analysis. There are specific insertion sites, trained personnel and procedures for arterial lines. There are also specific techniques for drawing a blood sample from an A-Line or arterial line. An arterial line is usually inserted into the radial artery in the wrist, but can also be inserted into the brachial artery at the elbow, into the femoral artery in the groin, into the dorsalis pedis artery in the foot, or into the ulnar artery in the wrist. In both adults and children, the most common site of cannulation is the radial artery, primarily because of the superficial nature of the vessel and the ease with which the site can be maintained. Additional advantages of radial artery cannulation include the consistency of the anatomy and the low rate of complications. After the radial artery, the femoral artery is the second most common site for arterial cannulation. One advantage of femoral artery cannulation is that the vessel is larger than the radial artery and has stronger pulsation. Additional advantages include decreased risk of thrombosis and of accidental catheter removal, though the overall complication rate remains comparable. There has been considerable debate over whether radial or femoral arterial line placement more accurately measures blood pressure and mean arterial pressure, however, both approaches seem to perform well for this function. -
Circulatory Collapse During Wound Closure In
Zhang et al. BMC Anesthesiology (2021) 21:4 https://doi.org/10.1186/s12871-020-01220-6 CASE REPORT Open Access Circulatory collapse during wound closure in spine surgery with an unknown cause: a possible adverse effect of topical application of vancomycin? Xiaoqing Zhang, Wenwen Zhai, Min Li and Xiangyang Guo* Abstract Background: Vancomycin (VCM) is effective in fighting Gram-positive bacteria related severe infections, and topical application of VCM powder is widely used in orthopedic surgery to prevent wound infection. However, VCM could lead to infusion rate-dependent antibody-and complement-independent anaphylaxis reaction by inducing direct release of histamine. Case presentation: We retrospectively analyzed seven cases of severe hypotension and shock during wound closure or immediately after orthopedic surgery with unidentifiable reasons. We found that these cases were all associated with local application of VCM powder during wound closure process. Two patients experienced sudden cardiac arrest. Most of the cases (6/7) with circulatory collapse were discharged without severe sequelae. While one case with application of 3 g VCM developed cardiac arrest and remained in a coma due to hypoxic-hypoxic encephalopathy. The clinical presentations and the time of the shock onset were considered to be related with a VCM induced anaphylaxis reaction. However, as this was a retrospective study, and there was no laboratory examination performed, the conclusion was made upon differential diagnosis based on clinical manifestations and the timing of the shock. Conclusions: Local application of VCM may not be as safe as was once believed and may lead to a related anaphylaxis. As VCM induced infusion-rate dependent, non-IgE mediated anaphylaxisischaracterizedbydelayed occurrence, severe hypotension and even circulatory collapse, surgeons and anesthesiologists should be extra vigilant during and after VCM application. -

Development of a Large Animal Model of Lethal Polytrauma and Intra
Open access Original research Trauma Surg Acute Care Open: first published as 10.1136/tsaco-2020-000636 on 1 February 2021. Downloaded from Development of a large animal model of lethal polytrauma and intra- abdominal sepsis with bacteremia Rachel L O’Connell, Glenn K Wakam , Ali Siddiqui, Aaron M Williams, Nathan Graham, Michael T Kemp, Kiril Chtraklin, Umar F Bhatti, Alizeh Shamshad, Yongqing Li, Hasan B Alam, Ben E Biesterveld ► Additional material is ABSTRACT abdomen and pelvic contents. The same review published online only. To view, Background Trauma and sepsis are individually two of showed that of patients with whole body injuries, please visit the journal online 1 (http:// dx. doi. org/ 10. 1136/ the leading causes of death worldwide. When combined, 37.9% had penetrating injuries. The abdomen is tsaco- 2020- 000636). the mortality is greater than 50%. Thus, it is imperative one area of the body which is particularly suscep- to have a reproducible and reliable animal model to tible to penetrating injuries.2 In a review of patients Surgery, Michigan Medicine, study the effects of polytrauma and sepsis and test novel in Afghanistan with penetrating abdominal wounds, University of Michigan, Ann treatment options. Porcine models are more translatable the majority of injuries were to the gastrointes- Arbor, Michigan, USA to humans than rodent models due to the similarities tinal tract with the most common injury being to 3 Correspondence to in anatomy and physiological response. We embarked the small bowel. While this severe constellation Dr Glenn K Wakam; gw akam@ on a study to develop a reproducible model of lethal of injuries is uncommon in the civilian setting, med. -

Hemodynamic Profiles Related to Circulatory Shock in Cardiac Care Units
REVIEW ARTICLE Hemodynamic profiles related to circulatory shock in cardiac care units Perfiles hemodinámicos relacionados con el choque circulatorio en unidades de cuidados cardiacos Jesus A. Gonzalez-Hermosillo1, Ricardo Palma-Carbajal1*, Gustavo Rojas-Velasco2, Ricardo Cabrera-Jardines3, Luis M. Gonzalez-Galvan4, Daniel Manzur-Sandoval2, Gian M. Jiménez-Rodriguez5, and Willian A. Ortiz-Solis1 1Department of Cardiology; 2Intensive Cardiovascular Care Unit, Instituto Nacional de Cardiología Ignacio Chávez; 3Inernal Medicine, Hospital Ángeles del Pedregal; 4Posgraduate School of Naval Healthcare, Universidad Naval; 5Interventional Cardiology, Instituto Nacional de Cardiología Ignacio Chávez. Mexico City, Mexico Abstract One-third of the population in intensive care units is in a state of circulatory shock, whose rapid recognition and mechanism differentiation are of great importance. The clinical context and physical examination are of great value, but in complex situa- tions as in cardiac care units, it is mandatory the use of advanced hemodynamic monitorization devices, both to determine the main mechanism of shock, as to decide management and guide response to treatment, these devices include pulmonary flotation catheter as the gold standard, as well as more recent techniques including echocardiography and pulmonary ultra- sound, among others. This article emphasizes the different shock mechanisms observed in the cardiac care units, with a proposal for approach and treatment. Key words: Circulatory shock. Hemodynamic monitorization. -

Impact of Intra-Aortic Balloon Support on Endothelial Function and Tissue Perfusion Markers in Severe Heart Failure
Central Journal of Cardiology & Clinical Research Bringing Excellence in Open Access Research Article *Corresponding author Silvia Gelás Lage, Instituto do Coração, Hospital das Clinicas HCFMUSP, Faculdade de Medicina, Impact of Intra-Aortic Balloon Universidade de Sao Paulo, Sao Paulo, SP, Brazil, Av. Dr. Enéas de Carvalho Aguiar, 44, 05403-000 - São Support on Endothelial Paulo, SP, Brazil, Tel: (55-11) 26615302; Email: Submitted: 12 September 2018 Accepted: 03 October 2018 Function and Tissue Perfusion Published: 05 October 2018 Copyright Markers in Severe Heart © 2018 Lage et al. OPEN ACCESS Failure Keywords • Intra-aortic balloon pump; Severe heart failure; Antônio A. P. Fagundes Júnior, Liliane Kopel, Claudia Bernoche, Endothelial function; Central venous oxygen saturation; Arteriovenous carbon dioxide gradient; Milena F. Macatrão-Costa, Leonardo N. Lopes, Antonio P. B-type natriuretic peptide Mansur, and Silvia Gelás Lage* Heart Institute, Hospital das Clinicas HCFMUSP, Brazil Abstract Background: The intra-aortic balloon pump (IABP) is a common therapy available for ventricular support in critical cardiac patients. The aim of this study was to characterize the effect of IABP on endothelial function, on serum B-type natriuretic peptide (BNP) levels and on central venous oxygen saturation (ScVO2) and arteriovenous carbon dioxide gradient (∆PCO2) as perfusion tissue markers. Methods and results: Twenty-three patients with severe heart failure, mean age 50±13 years, left ventricular ejection fraction of 22±8% were included. All were on IABP support and the protocol considered 3 conditions: 1) IABP ratio 1:1, 2) IABP ratio 1:3 and 3) IAPB ratio 1:1. The period of time between conditions was 20 minutes. -

Placement of an Arterial Line
T h e ne w engl a nd jour na l o f medicine videos in clinical medicine Placement of an Arterial Line Ken Tegtmeyer, M.D., Glenn Brady, M.D., Susanna Lai, M.P.H., Richard Hodo, and Dana Braner, M.D. Indications Radial arterial lines are important tools in the treatment of critically ill patients. From the Departments of Medical Infor- Continuous monitoring of blood pressure is indicated for patients with hemody- matics and Clinical Epidemiology and Pediatrics, Oregon Health and Sciences namic instability that requires inotropic or vasopressor medication. An arterial line University, Portland, Oreg. Address re- allows for consistent and continuous monitoring of blood pressure to facilitate the print requests to Dr. Braner at 3181 S.W. reliable titration of supportive medications. In addition, arterial lines allow for reli- Sam Jackson Park Rd., Portland, OR 97239-3098, or at [email protected]. able access to the arterial circulation for the measurement of arterial oxygenation and for frequent blood sampling. The placement of arterial lines is an important N Engl J Med 2006;354:e13. skill for physicians to master as they treat critically ill patients. Copyright © 2006 Massachusetts Medical Society. An arterial line is also indicated for patients with significant ventilatory deficits. Measurement of the partial pressures of arterial oxygen and arterial carbon dioxide provides more information about the status of gas exchange than does arterial oxygen saturation. Contraindications The contraindications to the placement of an arterial line are few but specific. Placement of an arterial line should not compromise the circulation distal to the placement site, which means that sites with known deficiencies in collateral circu- lation — such as those involved in Raynaud’s phenomenon and thromboangiitis obliterans or end arteries such as the brachial artery — should be avoided. -
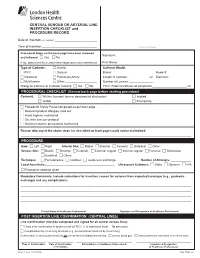
CENTRAL VENOUS OR ARTERIAL LINE INSERTION CHECKLIST and PROCEDURE RECORD
CENTRAL VENOUS OR ARTERIAL LINE INSERTION CHECKLIST and PROCEDURE RECORD Date of Insertion (YYYY/MM/DD): _________________________________ Time of Insertion:___________________________________________ ADDRESSOGRAPH Procedural Steps on the back page have been reviewed Signature:____________________________________________________________ and followed: c Yes c No If no, document the reason why steps were not maintained. Print Name: __________________________________________________________ Type of Catheter: c Arterial Catheter Model: c PICC c Dialysis Brand: ________________________________ Model #: __________________ c Introducer c Pulmonary Artery Length of catheter: ________________ cm Diameter: _________________ c Multi-lumen c Other:_________________________ Number of Lumens:___________________ Allergy to Catheter or Catheter Coating c Yes c No PICC: External catheter at completion___________________________ cm PROCEDURAL CHECKLIST (Review back page before starting procedure) Consent: c Written (consent form or documented discussion) c Implied c Verbal c Emergency c Procedural Safety Pause completed as per back page c Relevant product allergies ruled out c Hand hygiene maintained c Site/skin care per protocol c Maximum barrier precautions maintained Reason why any of the above steps (as described on back page) could not be maintained: ___________________________________ ______________________________________________________________________________________________________________________________________ PROCEDURE Side: c Left c Right -

Critical Review Form Therapy Early Goal Directed Therapy in Severe Sepsis and Septic Shock, NEJM 2001; 345: 1368-1377
Critical Review Form Therapy Early Goal Directed Therapy in Severe Sepsis and Septic Shock, NEJM 2001; 345: 1368-1377 Objective: To examine “whether early goal-directed therapy before admission to the ICU effectively reduces the incidence of multi-organ dysfunction, mortality, and the use of health care resources among patients with severe sepsis or septic shock.” (p. 1369) Methods: Open, randomized, partially blinded trial” (p. 1376). See CONSORT diagram (Figure 1, p. 1369) for an overview of patient enrollment and hemodynamic support. Eligible if > 18 years old presenting between March 1997 and March 2000 to Henry Ford Hospital (Detroit, MI) without bleeding risk, complicated sepsis (such as concurrent acute coronary syndrome or cardiogenic shock), atypical immune system (HIV or cancer), or contra-indications to invasive procedures. Eligible subjects also had to possess a systolic blood pressure < 90 mm Hg (after a 20-30 cc/kg bolus over 30-minutes) OR lactate > 4mmol/L AND two out of five of the following: 36°C > T > 38°C, heart rate > 90, respiratory rate > 20, partial pressure of carbon dioxide < 32 mm Hg, 4 > WBC > 12 OR >10% Bands. “The study was conducted during the routine treatment of other patients in the ED” (p. 1370) in a setting nearly identical to TCC at BJH. Patients were followed up to 60-days or death. Primary outcome was in-hospital mortality. Secondary outcomes included resuscitation endpoints, organ dysfunction, severity scores (APACHE II, SAPS II, MODS – see the original article for references if you are not familiar with these scoring systems), coagulation related variables, administered treatments, and the consumption of healthcare resources.