“There's Somebody Like Me:” Perspectives of a Peer-To-Peer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 Superior Court of California County of Alameda Before the Hono
1 SUPERIOR COURT OF CALIFORNIA 2 COUNTY OF ALAMEDA 3 BEFORE THE HONORABLE WINIFRED Y. SMITH, JUDGE PRESIDING 4 DEPARTMENT NUMBER 21 5 -- oOo--- 6 COORDINATION PROCEEDING ) SPECIAL TITLE (RULE 3.550) ) 7 ) ROUNDUP PRODUCTS CASE ) JCCP No. 4953 8 ) _______________________________ ) 9 ) THIS TRANSCRIPT RELATES TO: ) 10 ) Pilliod, et al. ) Case No. RG17862702 11 v s . ) Monsanto Company, et al. ) Pages 1533 - 1833 12 ________________________________ ) Volume 12 13 14 15 Reporter's Transcript of Proceedings 16 Tuesday, April 2, 2019 17 18 Reported by: Kelly L. Shainline, CSR No. 13476, RPR, CRR 19 Lori Stokes, CSR No. 12732, RPR Court Reporters 20 21 22 23 BAY AREA REPORTING 24 SOLUTIONS 25 888.526.8243 v.ww B.iyAro^ReporlingSolulions coin 1533 1 APPEARANCES OF COUNSEL: 2 3 For Plaintiffs: 4 THE MILLER FIRM, LLC 108 Railroad Avenue 5 Orange, Virgina 22960 (540)672-4224 6 BY: MICHAEL J. MILLER, ATTORNEY AT LAW [email protected] 7 8 BAUM HEDLUND ARISTEI & GOLDMAN PC 10940 Wilshire Boulevard, 17th Floor 9 Los Angeles, California 90024 (310) 207-3233 10 BY: R. BRENT WISNER, ATTORNEY AT LAW [email protected] 11 PEDRAM E S FANDIARY, ATTORNEY AT LAW [email protected] 12 13 AUDET Sc PARTNERS, LLP 221 Main Street, Suite 1460 14 San Francisco, California 94105 (415)568-2555 15 BY: MARK BURTON, ATTORNEY AT LAW [email protected] 16 17 18 (APPEARANCES CONTINUED ON FOLLOWING PAGE) 19 20 21 22 23 24 25 1534 1 APPEARANCES : (CONTINUED) 2 For Defendants: 3 EVANS FEARS & SCHUTTERT LLP 2300 W. Sahara Ave, Suite 950 4 Las Vegas, Nevada 89102 (702) 805-0290 5 BY: KELLY A. -

“The Stories Behind the Songs”
“The Stories Behind The Songs” John Henderson The Stories Behind The Songs A compilation of “inside stories” behind classic country hits and the artists associated with them John Debbie & John By John Henderson (Arrangement by Debbie Henderson) A fascinating and entertaining look at the life and recording efforts of some of country music’s most talented singers and songwriters 1 Author’s Note My background in country music started before I even reached grade school. I was four years old when my uncle, Jack Henderson, the program director of 50,000 watt KCUL-AM in Fort Worth/Dallas, came to visit my family in 1959. He brought me around one hundred and fifty 45 RPM records from his station (duplicate copies that they no longer needed) and a small record player that played only 45s (not albums). I played those records day and night, completely wore them out. From that point, I wanted to be a disc jockey. But instead of going for the usual “comedic” approach most DJs took, I tried to be more informative by dropping in tidbits of a song’s background, something that always fascinated me. Originally with my “Classic Country Music Stories” site on Facebook (which is still going strong), and now with this book, I can tell the whole story, something that time restraints on radio wouldn’t allow. I began deejaying as a career at the age of sixteen in 1971, most notably at Nashville’s WENO-AM and WKDA- AM, Lakeland, Florida’s WPCV-FM (past winner of the “Radio Station of the Year” award from the Country Music Association), and Springfield, Missouri’s KTTS AM & FM and KWTO-AM, but with syndication and automation which overwhelmed radio some twenty-five years ago, my final DJ position ended in 1992. -

Artwork / Streetlives, Street-Involved Youth in Thunder Bay: a Community-Based, Arts-Informed Inquiry
ARTWORK / STREETLIVES, STREET-INVOLVED YOUTH IN THUNDER BAY: A COMMUNITY-BASED, ARTS-INFORMED INQUIRY by Amy Campbell McGee A thesis submitted in conformity with the requirements for the degree of Doctor of Philosophy Graduate Department of Adult Education and Counselling Psychology Ontario Institute for Studies in Education University of Toronto © Copyright by Amy Campbell McGee (2010) ARTWORK / STREETLIVES, STREET-INVOLVED YOUTH IN THUNDER BAY: A COMMUNITY-BASED, ARTS-INFORMED INQUIRY Doctor of Philosophy, 2010 Amy Campbell McGee Graduate Department of Adult Education and Counselling Psychology University of Toronto Abstract Artwork / Streetlives is a community-based, arts-informed, research project which addresses harm reduction amongst street youth in Thunder Bay, Ontario. Nine street-involved participant researchers (supported by a team of researchers and community organizations) used art making and storytelling as ways of understanding the risks specific to street-involved youth in Thunder Bay. Due to the heterogeneous nature of the participant researcher group and a majority of Aboriginal research participants, a novel approach was used to create principles of research collaboration, in pursuit of the principles of ownership, control, access and possession for ethical research with Aboriginal peoples. The participant researchers found that their most common experience was their vulnerability to governmental social services and law enforcement personnel and policies. They further agreed that the risk of losing their children to child protection services is a source of increased vulnerability and a barrier to accessing treatment. They all agreed that the process of art making was fruitful and were surprised by the clarity and evocative nature of their artwork, finding that meeting weekly to do art is gratifying and therapeutic. -
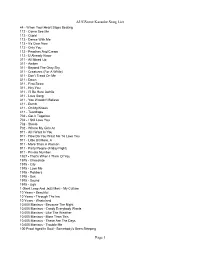
Augsome Karaoke Song List Page 1
AUGSome Karaoke Song List 44 - When Your Heart Stops Beating 112 - Come See Me 112 - Cupid 112 - Dance With Me 112 - It's Over Now 112 - Only You 112 - Peaches And Cream 112 - U Already Know 311 - All Mixed Up 311 - Amber 311 - Beyond The Gray Sky 311 - Creatures (For A While) 311 - Don't Tread On Me 311 - Down 311 - First Straw 311 - Hey You 311 - I'll Be Here Awhile 311 - Love Song 311 - You Wouldn't Believe 411 - Dumb 411 - On My Knees 411 - Teardrops 702 - Get It Together 702 - I Still Love You 702 - Steelo 702 - Where My Girls At 911 - All I Want Is You 911 - How Do You Want Me To Love You 911 - Little Bit More, A 911 - More Than A Woman 911 - Party People (Friday Night) 911 - Private Number 1927 - That's When I Think Of You 1975 - Chocolate 1975 - City 1975 - Love Me 1975 - Robbers 1975 - Sex 1975 - Sound 1975 - Ugh 1 Giant Leap And Jazz Maxi - My Culture 10 Years - Beautiful 10 Years - Through The Iris 10 Years - Wasteland 10,000 Maniacs - Because The Night 10,000 Maniacs - Candy Everybody Wants 10,000 Maniacs - Like The Weather 10,000 Maniacs - More Than This 10,000 Maniacs - These Are The Days 10,000 Maniacs - Trouble Me 100 Proof Aged In Soul - Somebody's Been Sleeping Page 1 AUGSome Karaoke Song List 101 Dalmations - Cruella de Vil 10Cc - Donna 10Cc - Dreadlock Holiday 10Cc - I'm Mandy 10Cc - I'm Not In Love 10Cc - Rubber Bullets 10Cc - Things We Do For Love, The 10Cc - Wall Street Shuffle 112 And Ludacris - Hot And Wet 12 Gauge - Dunkie Butt 12 Stones - Crash 12 Stones - We Are One 1910 Fruitgum Co. -

07 EP+45.Pdf
7" records - US releases, 4 tracks/45 rpm, if not noted otherwise 5820* Hank Locklin Encores Parlophone gep 8875\UK Zz * = picture cover MINIMUM = € 3.00 / US$ 3.50 = MINIMUM 5821* Die Maui-Hawaiians Aloha-Oe | Song of Haiti | Hula Girl +1 CBS ep 0045\D Zz EP's 5822* George Morgan Please Don’t Let Me Love You | Almost +2 Col b 2832 Zg 5823* Pantja Warna Krontjong Orkest olv Ming Luhulima CiD 75.860\NL Zz 5824 Phipps Family Glad Reunio n Day | Soul Winner for Jesus +4 (6tr) Faith 976 Z 5825* Elvis Presley in Kid Galahad - Four Great Songs RCA epa 9068\D Zz 5826* Malcolm Price Trio Pickin’ on the Country Strings (signed) Oak rgj 106\UK Gg 5827 Wayne Raney & Family I’ll Be Listening +5 (6tr) Starday sep 126 Z 5828* Jim Reeves Adios Amigo | I Love You Because | Marie +1 RCA epa 9124\D Zz 5829* ~ Welcome to My World | Rose Are Red | A Fool to Care +1 RCA rcx 7119\UK Gz 5830* ~ Die Ou Kalahari | Tahiti | Ek Verlang na Jou +1 RCA epa 9107\D Zz 5831* ~ Hillbilly VI: Tall Tales & Short Tempers RCA epa 9026\D Zz 5801* A G & Kate That Christmasy Feeling (signed) (6tr) SCR 1001\NL Zg 5832* Rivendel Country Young Faces Kamela 01\UK Zz 5802* Roy Acuff Sweeter Than the Flowers | Tennessee Waltz +2 Col b 2825 Zz 5833* Rockabilly’s Vol 1: Cliff Blakley, Joe Clay, George Hamilton, Narvel Felts, 5803* Eddy Arnold Kentucky Waltz | There’s Been a Change in Me RCA epa 5087 Zz Buddy Holly, Art Adams, Jim McDonald (8tr) Gypsy trg 101\EU Zz 5804* Fred Artmeier & zijn Hawaiian Band Groeten uit Hawaii Fono-Disc 1133\NL Zz 5834 Carl Smith Night Train to Memphis -

RCA Victor 12 Inch Popular Series LPM/LSP 3700-3999
RCA Discography Part 12 - By David Edwards, Mike Callahan, and Patrice Eyries. © 2018 by Mike Callahan RCA Victor 12 Inch Popular Series LPM/LSP 3700-3999 LPM/LSP 3700 – Norma Jean Sings Porter Wagoner – Norma Jean [1967] Dooley/Eat, Drink And Be Merry/Country Music Has Gone To Town/Misery Loves Company/Company's Comin'/I've Enjoyed As Much Of This As I Can Stand/Howdy Neighbor, Howdy/I Just Came To Smell The Flowers/A Satisfied Mind/If Jesus Came To Your House/Your Old Love Letters/I Thought I Heard You Calling My Name LPM/LSP 3701 – It Ain’t necessarily Square – Homer and Jethro [1967] Call Me/Lil' Darlin'/Broadway/More/Cute/Liza/The Shadow Of Your Smile/The Sweetest Sounds/Shiny Stockings/Satin Doll/Take The "A" Train LPM/LSP 3702 – Spinout (Soundtrack) – Elvis Presley [1966] Stop, Look And Listen/Adam And Evil/All That I Am/Never Say Yes/Am I Ready/Beach Shack/Spinout/Smorgasbord/I'll Be Back/Tomorrow Is A Long Time/Down In The Alley/I'll Remember You LPM/LSP 3703 – In Gospel Country – Statesmen Quartet [1967] Brighten The Corner Where You Are/Give Me Light/When You've Really Met The Lord/Just Over In The Glory-Land/Grace For Every Need/That Silver-Haired Daddy Of Mine/Where The Milk And Honey Flow/In Jesus' Name, I Will/Watching You/No More/Heaven Is Where You Belong/I Told My Lord LPM/LSP 3704 – Woman, Let Me Sing You a Song – Vernon Oxford [1967] Watermelon Time In Georgia/Woman, Let Me Sing You A Song/Field Of Flowers/Stone By Stone/Let's Take A Cold Shower/Hide/Baby Sister/Goin' Home/Behind Every Good Man There's A Woman/Roll -

Songs by Artist
Songs by Artist Karaoke Collection Title Title Title +44 18 Visions 3 Dog Night When Your Heart Stops Beating Victim 1 1 Block Radius 1910 Fruitgum Co An Old Fashioned Love Song You Got Me Simon Says Black & White 1 Fine Day 1927 Celebrate For The 1st Time Compulsory Hero Easy To Be Hard 1 Flew South If I Could Elis Comin My Kind Of Beautiful Thats When I Think Of You Joy To The World 1 Night Only 1st Class Liar Just For Tonight Beach Baby Mama Told Me Not To Come 1 Republic 2 Evisa Never Been To Spain Mercy Oh La La La Old Fashioned Love Song Say (All I Need) 2 Live Crew Out In The Country Stop & Stare Do Wah Diddy Diddy Pieces Of April 1 True Voice 2 Pac Shambala After Your Gone California Love Sure As Im Sitting Here Sacred Trust Changes The Family Of Man 1 Way Dear Mama The Show Must Go On Cutie Pie How Do You Want It 3 Doors Down 1 Way Ride So Many Tears Away From The Sun Painted Perfect Thugz Mansion Be Like That 10 000 Maniacs Until The End Of Time Behind Those Eyes Because The Night 2 Pac Ft Eminem Citizen Soldier Candy Everybody Wants 1 Day At A Time Duck & Run Like The Weather 2 Pac Ft Eric Will Here By Me More Than This Do For Love Here Without You These Are Days 2 Pac Ft Notorious Big Its Not My Time Trouble Me Runnin Kryptonite 10 Cc 2 Pistols Ft Ray J Let Me Be Myself Donna You Know Me Let Me Go Dreadlock Holiday 2 Pistols Ft T Pain & Tay Dizm Live For Today Good Morning Judge She Got It Loser Im Mandy 2 Play Ft Thomes Jules & Jucxi So I Need You Im Not In Love Careless Whisper The Better Life Rubber Bullets 2 Tons O Fun -

Eddy Arnold Somebody Like Me Mp3, Flac, Wma
Eddy Arnold Somebody Like Me mp3, flac, wma DOWNLOAD LINKS (Clickable) Genre: Folk, World, & Country Album: Somebody Like Me Country: US Released: 1966 Style: Country MP3 version RAR size: 1306 mb FLAC version RAR size: 1175 mb WMA version RAR size: 1164 mb Rating: 4.6 Votes: 438 Other Formats: MIDI WAV DMF APE DXD MP4 MMF Tracklist A1 Somebody Like Me 2:25 A2 Lay Some Happiness On Me 2:18 A3 There's Always Me 2:14 A4 Come By Me Nice And Slow 2:36 A5 You Made Up For Everything 2:06 A6 At Sunset 2:13 B1 The Tip Of My Fingers 2:55 B2 Love On My Mind 2:20 B3 I Love You Drops 2:04 B4 Don't Laugh At My Love 2:31 B5 Ev'ry Step Of the Way 2:09 B6 It's Only Love 2:20 Other versions Category Artist Title (Format) Label Category Country Year Somebody Like Me (LP, LSP-3715 Eddy Arnold RCA Victor LSP-3715 US 1966 Album) Somebody Like Me (LP, LSP 3715 Eddy Arnold RCA Victor LSP 3715 Germany 1966 Album) Somebody Like Me (LP, LSP 3715 Eddy Arnold RCA Victor LSP 3715 US 1966 Album) Somebody Like Me (LP, LPM-3715 Eddy Arnold RCA Victor LPM-3715 Canada Unknown Album, Mono) Somebody Like Me (LP, LPM-3715 Eddy Arnold RCA Victor LPM-3715 Canada Unknown Album, Mono) Related Music albums to Somebody Like Me by Eddy Arnold Eddy Arnold - Christmas With Eddy Arnold Eddy Arnold - Lonely People Eddy Arnold - Eddy Eddy Arnold - Moonlight And Roses (Bring Mem'ries Of You) Eddy Arnold - Our Man Down South Eddy Arnold - Just Out Of Reach Eddy Arnold And His Tennessee Plowboys - I Couldn't Believe It Was True / It's A Sin Eddy Arnold - Turn The World Around Eddy Arnold - Wanderin' With Eddy Arnold Eddy Arnold, The Tennessee Plowboy And His Guitar - Eddy Arnold Sings. -
Songs by Artist
Songs by Artist Title DiscID Title DiscID 10 Years 2 Pac & Eric Will Wasteland SC8966-13 Do For Love MM6299-09 10,000 Maniacs 2 Pac & Notorious Big Because The Night SC8113-05 Runnin' SC8858-11 Candy Everybody Wants DK082-04 2 Unlimited Like The Weather MM6066-07 No Limits SF006-05 More Than This SC8390-06 20 Fingers These Are The Days SC8466-14 Short Dick Man SC8746-14 Trouble Me SC8439-03 3 am 100 Proof Aged In Soul Busted MRH10-07 Somebody's Been Sleeping SC8333-09 3 Colours Red 10Cc Beautiful Day SF130-13 Donna SF090-15 3 Days Grace Dreadlock Holiday SF023-12 Home SIN0001-04 I'm Mandy SF079-03 Just Like You SIN0012-08 I'm Not In Love SC8417-13 3 Doors Down Rubber Bullets SF071-01 Away From The Sun SC8865-07 Things We Do For Love SFMW832-11 Be Like That MM6345-09 Wall Street Shuffle SFMW814-01 Behind Those Eyes SC8924-02 We Do For Love SC8456-15 Citizen Soldier CB30069-14 112 Duck & Run SC3244-03 Come See Me SC8357-10 Here By Me SD4510-02 Cupid SC3015-05 Here Without You SC8905-09 Dance With Me SC8726-09 It's Not My Time (I Won't Go) CB30070-01 It's Over Now SC8672-15 Kryptonite SC8765-03 Only You SC8295-04 Landing In London CB30056-13 Peaches & Cream SC3258-02 Let Me Be Myself CB30083-01 Right Here For You PHU0403-04 Let Me Go SC2496-04 U Already Know PHM0505U-07 Live For Today SC3450-06 112 & Ludacris Loser SC8622-03 Hot & Wet PHU0401-02 Road I'm On SC8817-10 12 Gauge Train CB30075-01 Dunkie Butt SC8892-04 When I'm Gone SC8852-11 12 Stones 3 Doors Down & Bob Seger Crash TU200-04 Landing In London CB30056-13 Far Away THR0411-16 3 Of A Kind We Are One PHMP1008-08 Baby Cakes EZH038-01 1910 Fruitgum Co. -

Songs by Artist
Songs by Artist Title Versions Title Versions Title Versions 10 Years 3 Doors Down 50 Cent Through The Iris TH Kryptonite 9 Just A Lil Bit SF PH TH Wasteland PH Sc TH Let Me Go 4 PIMP SC PH 10,000 Maniacs Live For Today SC PH TH PIMP (Remix) TH Because The Night SC MM Loser 6 Straight To The Bank PH Candy Everybody Wants DK Road I'm On, The 5 Wanksta SC Like The Weather MM Rt Train CB What Up Gangsta PH More Than This SC MM PH When I'm Gone 8 Window Shopper PH TH These Are The Days SC PI 3 Doors Down & Bob Seger 50 Cent & Eminem Trouble Me SC Rt Landing In London CB PH TH Patiently Waiting SC 100 Proof Aged In Soul 3 Of Hearts 50 Cent & Justin Timberlake Somebody's Been Sleeping SC Arizona Rain 4 Ayo Technology PH 10cc Christmas Shoes TU 50 Cent & Mobb Deep Donna SF Love Is Enough 4 Outta Control PH TH Dreadlock Holiday SF 30 Seconds To Mars Outta Control (Remix Version) SC I'm Mandy SF Kill, The SC TH 50 Cent & Nate Dogg I'm Not In Love 5 311 21 Questions 4 Rubber Bullets SF ZM All Mixed Up SC PH RS 50 Cent & Olivia Things We Do For Love, The SC SF ZM Amber PH TH Best Friend PH TH Wall Street Shuffle SF Beyond The Gray Sky PH TH 5th Dimension, The 112 Creatures (For A While) PH TH Aquarius (Let The Sun Shine In) 6 Come See Me SC Don't Tread On Me SC PH Last Night I Didn't Get To Sleep At All SC DG Cupid SC Down SC One Less Bell To Answer SC MM Dance With Me SC CB TH First Straw PH Stoned Soul Picnic 5 It's Over Now SC I'll Be Here Awhile TH Up, Up & Away DK SF Cb Only You SC Love Song SC PH TH Wedding Bell Blues SC DK Cb Peaches & Cream -

Songs by Artist
Songs by Artist Title Title Title +44 112 2 Pac When Your Heart Stops Beating Cupid Dear Mama When Your Heart Stops Beating Dance With Me How Do You Want It 1 Block Radius Its Over Now So Many Tears You Got Me Peaches & Cream Thugz Mansion 1 Fine Day Right Here For You Until The End Of Time For The 1st Time U Already Know 2 Pac Ft Eminem 1 Flew South 112 Ft Ludacris 1 Day At A Time My Kind Of Beautiful Hot & Wet 2 Pac Ft Eric Will 1 Night Only 112 Ft Super Cat Do For Love Just For Tonight Na Na Na 2 Pac Ft Notorious Big 1 Republic 12 Gauge Runnin Mercy Dunkie Butt 2 Pistols Ft Ray J Say (All I Need) 12 Stones You Know Me Stop & Stare Crash 2 Pistols Ft T Pain & Tay Dizm 1 True Voice We Are One She Got It After Your Gone 18 Visions 2 Play Ft Thomes Jules & Jucxi Sacred Trust Victim Careless Whi 1 Way 1910 Fruitgum Co 2 Tons O Fun Cutie Pie Simon Says Its Raining Men 1 Way Ride 1927 2 Unlimited Painted Perfect Compulsory Hero No Limit 10 000 Maniacs If I Could 20 Fingers Because The Night Thats When I Think Of You Short Dick Man Candy Everybody Wants 1975 21 Demands Like The Weather Chocol - Give Me A Minute More Than This Chocolate 21 Savage & Offset & Metro Boomin & Travis Scott (Duet) These Are Days City Ghostface Killers Trouble Me Love Me 21 St Century Girls 10 Cc Sound 21 St Century Girls Donna The Sound 2AM Club Dreadlock Holiday UGH Not Your Boyfriend Good Morning Judge 1st Class 2Pac & Eric Williams Im Mandy Beach Baby Do For Love Im Not In Love 2 Chainz 3 6 Mafia Rubber Bullets I'm Different (Clean) Poppin My Collar The Things We Do For Love 2 Chainz & Pharrell Stay Fly Feds Watching (Expli Wall Street Shuffle 3 6 Mafia Ft Young Buck 10 Years 2 Chainz And Drake Stay Fly No Lie (Clean) Beautiful 3 Colors Red Through The Iris 2 Chainz Feat. -

Elite Karaoke Draft by Artist 2 Pistols Feat
Elite Karaoke Draft by Artist 2 Pistols Feat. Ray J You Know Me (Hed) Planet Earth 2 Pistols Feat. T-Pain & Tay Bartender Dizm Blackout She Got It Other Side 2 Play Feat. Thomas Jules & Renegade Jucxi D 10 Years Careless Whisper Actions & Motives 2 Unlimited Beautiful No Limit Drug Of Choice Twilight Zone Fix Me 20 Fingers Fix Me (Acoustic) Short Dick Man Shoot It Out 21 Demands Through The Iris Give Me A Minute Wasteland 21 Savage Feat. Offset, Metro 10,000 Maniacs Boomin & Travis Scott Because The Night Ghostface Killers Candy Everybody Wants 2Pac Like The Weather Changes More Than This Dear Mama These Are The Days How Do You Want It Trouble Me I Get Around 100 Proof (Aged In Soul) So Many Tears Somebody's Been Sleeping Until The End Of Time 101 Dalmations 2Pac Feat. Dr. Dre Cruella De Vil California Love 10cc 2Pac Feat. Elton John Dreadlock Holiday Ghetto Gospel Good Morning Judge 2Pac Feat. Eminem I'm Not In Love One Day At A Time The Things We Do For Love 2Pac Feat. Eric Williams Things We Do For Love Do For Love 112 2Pac Feat. Notorious B.I.G. Dance With Me Runnin' Peaches & Cream 3 Doors Down Right Here For You Away From The Sun U Already Know Be Like That 112 Feat. Ludacris Behind Those Eyes Hot & Wet Citizen Soldier 112 Feat. Super Cat Dangerous Game Na Na Na Duck & Run 12 Gauge Every Time You Go Dunkie Butt Going Down In Flames 12 Stones Here By Me Arms Of A Stranger Here Without You Far Away It's Not My Time (I Won't Go) Shadows Kryptonite We Are One Landing In London 1910 Fruitgum Co.