Autonomic Hyperreflexia After Spinal Cord Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Treatment of Autonomic Dysreflexia for Adults & Adolescents with Spinal
Treatment of Autonomic Dysreflexia for Adults & Adolescents with Spinal Cord Injuries Authors: Dr James Middleton, Director, State Spinal Cord Injury Service, NSW Agency for Clinical Innovation. Dr Kumaran Ramakrishnan, Honorary Fellow, Rehabilitation Studies Unit, Sydney Medical School Northern, The University of Sydney, and Consultant Rehabilitation Physician & Senior Lecturer, Department of Rehabilitation Medicine, University Malaya. Dr Ian Cameron, Head of the Rehabilitation Studies Unit, Sydney Medical School Northern, The University of Sydney. Reviewed and updated in 2013 by the authors. AGENCY FOR CLINICAL INNOVATION Level 4, Sage Building 67 Albert Avenue Chatswood NSW 2067 PO Box 699 Chatswood NSW 2057 T +61 2 9464 4666 | F +61 2 9464 4728 E [email protected] | www.aci.health.nsw.gov.au Produced by the NSW State Spinal Cord Injury Service. SHPN: (ACI) 140038 ISBN: 978-1-74187-972-8 Further copies of this publication can be obtained from the Agency for Clinical Innovation website at: www.aci.health.nsw.gov.au Disclaimer: Content within this publication was accurate at the time of publication. This work is copyright. It may be reproduced in whole or part for study or training purposes subject to the inclusion of an acknowledgment of the source. It may not be reproduced for commercial usage or sale. Reproduction for purposes other than those indicated above, requires written permission from the Agency for Clinical Innovation. © Agency for Clinical Innovation 2014 Published: February 2014 HS13-136 ACKNOWLEDGEMENTS This document was originally published as a fact sheet for the Rural Spinal Cord Injury Project (RSCIP), a pilot healthcare program for people with a spinal cord injury (SCI) conducted within New South Wales involving the collaboration of Prince Henry & Prince of Wales Hospitals, Royal North Shore Hospital, Royal Rehabilitation Centre Sydney, Spinal Cord Injuries Australia and the Paraplegic & Quadriplegic Association of NSW. -

Scienti®C Review Spastic Movement Disorder
Spinal Cord (2000) 38, 389 ± 393 ã 2000 International Medical Society of Paraplegia All rights reserved 1362 ± 4393/00 $15.00 www.nature.com/sc Scienti®c Review Spastic movement disorder V Dietz*,1 1Paracare, Paraplegic Centre of the University Hospital Balgrist, ZuÈrich, Switzerland This review deals with the neuronal mechanisms underlying spastic movement disorder, assessed by electrophysiological means with the aim of ®rst, a better understanding of the underlying pathophysiology and second, the selection of an adequate treatment. For the patient usually one of the ®rst symptoms of a lesion within the central motor system represents the movement disorder, which is most characteristic during locomotion in patients with spasticity. The clinical examination reveals exaggerated tendon tap re¯exes and increased muscle tone typical of the spastic movement disorder. However, today we know that there exists only a weak relationship between the physical signs obtained during the clinical examination in a passive motor condition and the impaired neuronal mechanisms being in operation during an active movement. By the recording and analysis of electrophysiological and biomechanical parameters during a functional movement such as locomotion, the signi®cance of, for example, impaired re¯ex behaviour or pathophysiology of muscle tone and its contribution to the movement disorder can reliably be assessed. Consequently, an adequate treatment should not be restricted to the cosmetic therapy and correction of an isolated clinical parameter but should be based on the pathophysiology and signi®cance of the mechanisms underlying the disorder of functional movement which impairs the patient. Spinal Cord (2000) 38, 389 ± 393 Keywords: spinal cord injury; spasticity; electrophysiological recordings; treatment Introduction Movement disorders are prominent features of impaired strength of electromyographic (EMG) activation of function of the motor systems and are frequently best antagonistic leg muscles as well as intrinsic and passive re¯ected during gait. -

Neuromuscular Disorders Neurology in Practice: Series Editors: Robert A
Neuromuscular Disorders neurology in practice: series editors: robert a. gross, department of neurology, university of rochester medical center, rochester, ny, usa jonathan w. mink, department of neurology, university of rochester medical center,rochester, ny, usa Neuromuscular Disorders edited by Rabi N. Tawil, MD Professor of Neurology University of Rochester Medical Center Rochester, NY, USA Shannon Venance, MD, PhD, FRCPCP Associate Professor of Neurology The University of Western Ontario London, Ontario, Canada A John Wiley & Sons, Ltd., Publication This edition fi rst published 2011, ® 2011 by Blackwell Publishing Ltd Blackwell Publishing was acquired by John Wiley & Sons in February 2007. Blackwell’s publishing program has been merged with Wiley’s global Scientifi c, Technical and Medical business to form Wiley-Blackwell. Registered offi ce: John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK Editorial offi ces: 9600 Garsington Road, Oxford, OX4 2DQ, UK The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK 111 River Street, Hoboken, NJ 07030-5774, USA For details of our global editorial offi ces, for customer services and for information about how to apply for permission to reuse the copyright material in this book please see our website at www.wiley.com/wiley-blackwell The right of the author to be identifi ed as the author of this work has been asserted in accordance with the UK Copyright, Designs and Patents Act 1988. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher. -

Non-Progressive Congenital Ataxia with Cerebellar Hypoplasia in Three Families
248 Non-progressive congenital ataxia with cerebellar hypoplasia in three families . No 1.6 Z. YAPICI & M. ERAKSOY . .. I.Y.. \ .~ ---················ No of Neurology, of Child Neuro/ogy, Facu/ty of Turkey Abstract Non-progressive with cerebellar hypoplasia are a rarely seen heterogeneous group ofhereditary cerebellar ataxias. Three sib pairs from three different families with this entity have been reviewed, and differential diagnosis has been di sc ussed. in two of the families, the parents were consanguineous. Walking was delayed in ali the children. Truncal and extremiry were then noticed. Ataxia was severe in one child, moderate in two children, and mild in the remaining revealed horizontal, horizonto-rotatory and/or vertical variable degrees ofmental and pvramidal signs besides truncal and extremity ataxia. In ali the cases, cerebellar hemisphere and vermis were in MRI . During the follow-up period, a gradual clinical improvement was achieved in ali the Condusion: he cu nsidered as recessive in some of the non-progressive ataxic syndromes. are being due to the rarity oflarge pedigrees for genetic studies. Iffurther on and clini cal progression of childhood associated with cerebellar hypoplasia is be a cu mbined of metabolic screening, long-term follow-up and radiological analyses is essential. Key Words: Cerebella r hy poplasia, ataxic syndromes are common during Patients 1 and 2 (first family) childhood. Friedreich 's ataxia and ataxia-telangiectasia Two brothers aged 5 and 7 of unrelated parents arc two best-known examples of such rare syn- presented with a history of slurred speech and diffi- dromes characterized both by their progressive nature culty of gait. -

Autonomic Hyperreflexia Associated with Recurrent Cardiac Arrest
Spinal Cord (1997) 35, 256 ± 257 1997 International Medical Society of Paraplegia All rights reserved 1362 ± 4393/97 $12.00 Autonomic hyperre¯exia associated with recurrent cardiac arrest: Case Report SC Colachis, III1 and DM Clinchot2 1Associate Professor and 2Assistant Professor, Department of Physical Medicine and Rehabilitation1, Director, SCI Rehabilitation, The Ohio State University, College of Medicine, Columbus, Ohio, USA Autonomic hyperre¯exia is a condition which may occur in individuals with spinal cord injuries above the splanchnic sympathetic out¯ow. Noxious stimuli can produce profound alterations in sympathetic pilomotor, sudomotor, and vasomotor activity, as well as disturbances in cardiac rhythm. A case of autonomic hyperre¯exia in a patient with C6 tetraplegia with recurrent ventricular ®brillation and cardiac arrest illustrates the profound eects of massive paroxysmal sympathetic activity associated with this condition. Keywords: autonomic hyperre¯exia; spinal cord injury; ventricular ®brillation Introduction Autonomic hyperre¯exia is a condition of paroxysmal by excessive sweating and ¯ushing. Past episodes of re¯ex sympathetic activity which occurs in response to autonomic hyperre¯exia were generally attributed to noxious stimuli in patients with spinal cord injuries re¯ex voiding, position changes and the presence of above the major splanchnic sympathetic out¯ow.1±3 pressure sores. The heightened sympathetic activity during an episode The attendant had completed the patient's morning of autonomic hyperre¯exia accounts for several of the bowel program, hygiene and dressing activities, and clinical features commonly observed including sudo- started to exit the apartment when he heard gasping. motor and pilomotor phenomenon,1,4 ± 6 vasomotor He returned to ®nd him pulseless, apneic, and sequelae,1 ± 4,7 and alterations in cardiac inotropic and cyanotic. -

Late-Onset Oro-Facial Dyskinesia in Spinocerebellar Ataxia Type 2: a Case Report Floriana Giardina1†, Giuseppe Lanza2,3*† , Francesco Calì3 and Raffaele Ferri3
Giardina et al. BMC Neurology (2020) 20:156 https://doi.org/10.1186/s12883-020-01739-8 CASE REPORT Open Access Late-onset oro-facial dyskinesia in Spinocerebellar Ataxia type 2: a case report Floriana Giardina1†, Giuseppe Lanza2,3*† , Francesco Calì3 and Raffaele Ferri3 Abstract Background: Genetic familiar causes of oro-facial dyskinesia are usually restricted to Huntington’s disease, whereas other causes are often missed or underestimated. Here, we report the case of late-onset oro-facial dyskinesia in an elderly patient with a genetic diagnosis of Spinocerebellar Ataxia type 2 (SCA2). Case presentation: A 75-year-old man complained of progressive balance difficulty since the age of 60 years, associated with involuntary movements of the mouth and tongue over the last 3 months. No exposure to anti- dopaminergic agents, other neuroleptics, antidepressants, or other drugs was reported. Family history was positive for SCA2 (brother and the son of the brother). At rest, involuntary movements of the mouth and tongue were noted; they appeared partially suppressible and became more evident during stress and voluntary movements. Cognitive examination revealed frontal-executive dysfunction, memory impairment, and attention deficit. Brain magnetic resonance imaging (MRI) disclosed signs of posterior periventricular chronic cerebrovascular disease and a marked ponto-cerebellar atrophy, as confirmed by volumetric MRI analysis. A dopamine transporter imaging scan demonstrated a bilaterally reduced putamen and caudate nucleus uptake. Ataxin-2 (ATXN2) gene analysis revealed a 36 cytosine-adenine-guanine (CAG) repeat expansion, confirming the diagnosis of SCA2. Conclusions: SCA2 should be considered among the possible causes of adult-onset oro-facial dyskinesia, especially when the family history suggests an inherited cerebellar disorder. -

History-Of-Movement-Disorders.Pdf
Comp. by: NJayamalathiProof0000876237 Date:20/11/08 Time:10:08:14 Stage:First Proof File Path://spiina1001z/Womat/Production/PRODENV/0000000001/0000011393/0000000016/ 0000876237.3D Proof by: QC by: ProjectAcronym:BS:FINGER Volume:02133 Handbook of Clinical Neurology, Vol. 95 (3rd series) History of Neurology S. Finger, F. Boller, K.L. Tyler, Editors # 2009 Elsevier B.V. All rights reserved Chapter 33 The history of movement disorders DOUGLAS J. LANSKA* Veterans Affairs Medical Center, Tomah, WI, USA, and University of Wisconsin School of Medicine and Public Health, Madison, WI, USA THE BASAL GANGLIA AND DISORDERS Eduard Hitzig (1838–1907) on the cerebral cortex of dogs OF MOVEMENT (Fritsch and Hitzig, 1870/1960), British physiologist Distinction between cortex, white matter, David Ferrier’s (1843–1928) stimulation and ablation and subcortical nuclei experiments on rabbits, cats, dogs and primates begun in 1873 (Ferrier, 1876), and Jackson’s careful clinical The distinction between cortex, white matter, and sub- and clinical-pathologic studies in people (late 1860s cortical nuclei was appreciated by Andreas Vesalius and early 1870s) that the role of the motor cortex was (1514–1564) and Francisco Piccolomini (1520–1604) in appreciated, so that by 1876 Jackson could consider the the 16th century (Vesalius, 1542; Piccolomini, 1630; “motor centers in Hitzig and Ferrier’s region ...higher Goetz et al., 2001a), and a century later British physician in degree of evolution that the corpus striatum” Thomas Willis (1621–1675) implicated the corpus -
Tremor, Abnormal Movement and Imbalance Differential
Types of involuntary movements Tremor Dystonia Chorea Myoclonus Tics Tremor Rhythmic shaking of muscles that produces an oscillating movement Parkinsonian tremor Rest tremor > posture > kinetic Re-emergent tremor with posture Usually asymmetric Pronation-supination tremor Distal joints involved primarily Often posturing of the limb Parkinsonian tremor Other parkinsonian features Bradykinesia Rigidity Postural instability Many, many other motor and non- motor features Bradykinesia Rigidity Essential tremor Kinetic > postural > rest Rest in 20%, late feature, only in arms Intentional 50% Bringing spoon to mouth is challenging!! Mildly asymmetric Gait ataxia – typically mild Starts in the arms but can progress to neck, voice and jaw over time Jaw tremor occurs with action, not rest Neck tremor should resolve when patient is lying flat Essential tremor Many other tremor types Physiologic tremor Like ET but faster rate and lower amplitude Drug-induced tremor – Lithium, depakote, stimulants, prednisone, beta agonists, amiodarone Anti-emetics (phenergan, prochlorperazine), anti-psychotics (except clozapine and Nuplazid) Many other tremor types Primary writing tremor only occurs with writing Orthostatic tremor leg tremor with standing, improves with walking and sitting, causes imbalance Many other tremor types Cerebellar tremor slowed action/intention tremor Holmes tremor mid-brain lesion, unilateral Dystonia Dystonia Muscle contractions that cause sustained or intermittent torsion of a body part in a repetitive -

Hemiballismus: /Etiology and Surgical Treatment by Russell Meyers, Donald B
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.13.2.115 on 1 May 1950. Downloaded from J. Neurol. Neurosurg. Psychiat., 1950, 13, 115. HEMIBALLISMUS: /ETIOLOGY AND SURGICAL TREATMENT BY RUSSELL MEYERS, DONALD B. SWEENEY, and JESS T. SCHWIDDE From the Division of Neurosurgery, State University of Iowa, College ofMedicine, Iowa City, Iowa Hemiballismus is a relatively uncommon hyper- 1949; Whittier). A few instances are on record in kinesia characterized by vigorous, extensive, and which the disorder has run an extended chronic rapidly executed, non-patterned, seemingly pur- course (Touche, 1901 ; Marcus and Sjogren, 1938), poseless movements involving one side of the body. while in one case reported by Lea-Plaza and Uiberall The movements are almost unceasing during the (1945) the abnormal movements are said to have waking state and, as with other hyperkinesias con- ceased spontaneously after seven weeks. Hemi- sidered to be of extrapyramidal origin, they cease ballismus has also been known to cease following during sleep. the supervention of a haemorrhagic ictus. Clinical Aspects Terminology.-There appears to be among writers on this subject no agreement regarding the precise Cases are on record (Whittier, 1947) in which the Protected by copyright. abnormal movements have been confined to a single features of the clinical phenomena to which the limb (" monoballismus ") or to both limbs of both term hemiballismus may properly be applied. sides (" biballismus ") (Martin and Alcock, 1934; Various authors have credited Kussmaul and Fischer von Santha, 1932). In a majority of recorded (1911) with introducing the term hemiballismus to instances, however, the face, neck, and trunk as well signify the flinging or flipping character of the limb as the limbs appear to have been involved. -

PREVENTING SECONDARY MEDICAL COMPLICATIONS: a Guide for Personal Assistants to People with Spinal Cord Injury
PREVENTING SECONDARY MEDICAL COMPLICATIONS: A Guide for Personal Assistants to People with Spinal Cord Injury Medical Rehabilitation Research and Training Center in Secondary Complications in Spinal Cord Injury SPAIN REHABILITATION CENTER University of Alabama at Birmingham Preventing Secondary Medical Complications: A Guide For Personal Assistants to People With Spinal Cord Injury Developed by: Medical Rehabilitation Research and Training Center in Secondary Complications in Spinal Cord Injury Training Office Department of Physical Medicine and Rehabilitation Spain Rehabilitation Center University of Alabama at Birmingham Acknowledgment Our thanks to the following individuals who helped us in the development of this booklet: Lorraine Arrington Judy Matthews Brenda Bass Margaret A. Nosek, PhD Betty Bass Scott and Donna Sartain Cathy Crawford, RD Drenda Scroggin Charles Cowan Anna Smith Allan Drake Brenda Smith David Felton Susan Smith, RN,BSN Peg Hale, RN,BSN Nita Straiton Bobbie Kent Donna Thornton Phillip Klebine Frank Wilkinson C.J. and Cindy Luster Larrie Waters c 1992, Revised 1996, The Board of Trustees of the University of Alabama This publication is supported in part by a grant (#H133B30025) from the National Institute on Disability and Rehabilitation Research, Department of Education, Washington, D.C. 20202. Opinions expressed in this document are not necessarily those of the granting agency. The University of Alabama at Birmingham administers its educational programs and activities, including admissions, without regard to race, color, religion, sex, national origin, handicap or Vietnam era or disabled veteran status. (Title IX of the Education Amendments of 1972 specifically prohibits discrimination on the basis of sex.) Direct inquires to Academic Affirmative Action Officer, The University of Alabama at Birmingham, UAB Station, Birmingham, Alabama, 35294. -

Recognition and Management of Intraoperative Autonomic Dysreflexia Thomas Lyford1, Katherine Borowczyk1, Simon Danieletto1 and Ruan Vlok1,2*
Editorial iMedPub Journals Journal of Surgery and Emergency Medicine 2016 http://www.imedpub.com/ Vol.1 No. 1:1000e102 Recognition and Management of Intraoperative Autonomic Dysreflexia Thomas Lyford1, Katherine Borowczyk1, Simon Danieletto1 and Ruan Vlok1,2* 1School of Medicine Sydney, University of Notre Dame Australia, Australia 2Wagga Wagga Rural Referral Hospital, Australia *Corresponding author: Vlok R, School of Medicine Sydney, University of Notre Dame Australia, Australia, Tel: 411388932; E-mail: [email protected] Received date: November 15, 2016; Accepted date: November 16, 2016; Published date: November 18, 2016 Copyright: © 2016 Vlok R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Citation: Lyford T, Borowczyk K, Danieletto S, Vlok R (2016) Recognition and Management of Intraoperative Autonomic Dysreflexia. J Surgery Emerg Med 1: e102. leading to sympathetic over-activity in the presence of noxious stimuli [9]. The release of sympathetic mediators such as Abstract noradrenaline results in significant vasoconstriction, leading to skin pallor below the level of the SCI and significant As the life expectancy of patients with spinal cord injuries hypertension [9]. This hypertension is sensed in baroreceptors continues to rise, consideration needs to be given to the in the aortic arch and carotid bodies, leading to reflex implications of this condition in the surgical setting. bradycardia, flushing and sweating above the level of the SCI Autonomic Dysreflexia is a medical emergency and has [9]. This flushing is likely to be the mechanism for the profound been described as the most common complication in headaches experienced in AD [9]. -
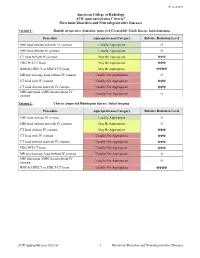
Movement Disorders and Neurodegenerative Diseases
Revised 2019 American College of Radiology ACR Appropriateness Criteria® Movement Disorders and Neurodegenerative Diseases Variant 1: Rapidly progressive dementia; suspected Creutzfeldt-Jakob disease. Initial imaging. Procedure Appropriateness Category Relative Radiation Level MRI head without and with IV contrast Usually Appropriate O MRI head without IV contrast Usually Appropriate O CT head without IV contrast May Be Appropriate ☢☢☢ FDG-PET/CT brain May Be Appropriate ☢☢☢ HMPAO SPECT or SPECT/CT brain May Be Appropriate ☢☢☢☢ MR spectroscopy head without IV contrast Usually Not Appropriate O CT head with IV contrast Usually Not Appropriate ☢☢☢ CT head without and with IV contrast Usually Not Appropriate ☢☢☢ MRI functional (fMRI) head without IV Usually Not Appropriate O contrast Variant 2: Chorea; suspected Huntington disease. Initial imaging. Procedure Appropriateness Category Relative Radiation Level MRI head without IV contrast Usually Appropriate O MRI head without and with IV contrast May Be Appropriate O CT head without IV contrast May Be Appropriate ☢☢☢ CT head with IV contrast Usually Not Appropriate ☢☢☢ CT head without and with IV contrast Usually Not Appropriate ☢☢☢ FDG-PET/CT brain Usually Not Appropriate ☢☢☢ MR spectroscopy head without IV contrast Usually Not Appropriate O MRI functional (fMRI) head without IV Usually Not Appropriate O contrast HMPAO SPECT or SPECT/CT brain Usually Not Appropriate ☢☢☢☢ ACR Appropriateness Criteria® 1 Movement Disorders and Neurodegenerative Diseases Variant 3: Parkinsonian syndromes. Initial