Carcroft Doctors Group Quality Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sustainability Appraisal Addendum
DMBC30 Doncaster Metropolitan Borough Council Doncaster Local Plan Addendum to the Publication Plan Sustainability Report (August 2019) and the Addendum to the Publication Plan Sustainability Report (March 2020) - Appraisal of Proposed Main Modifications (2021) Wood Group UK Limited – February 2021 2 © Wood Group UK Limited Report For Copyright and Non-Disclosure Notice Jonathan Clarke The contents and layout of this report are subject to copyright Principal Local Plan Delivery Officer owned by Wood (© Wood Group UK Limited 2021) save to the Doncaster Council extent that copyright has been legally assigned by us to another Civic Office party or is used by Wood under licence. To the extent that we Waterdale own the copyright in this report, it may not be copied or used Doncaster without our prior written agreement for any purpose other than DN1 3BU the purpose indicated in this report. The methodology (if any) contained in this report is provided to you in confidence and must not be disclosed or copied to third parties without the prior written agreement of Wood. Disclosure of that information Main Contributors may constitute an actionable breach of confidence or may Ryan Llewellyn otherwise prejudice our commercial interests. Any third party Robert Deanwood who obtains access to this report by any means will, in any event, Pete Davis be subject to the Third Party Disclaimer set out below. Issued By Third Party Disclaimer Any disclosure of this report to a third party is subject to this disclaimer. The report was prepared by Wood at the instruction ................................................................................. of, and for use by, our client named on the front of the report. -

Doncaster Historic Designed Landscapes Project Campsmount Park
YORKSHIRE GARDENS TRUST Doncaster Historic Designed Landscapes Project Campsmount Park Report by Mary Ratcliffe [April 2019] 1. CORE DATA 1.1 Name of site: Campsmount Park 1.2 Grid reference: SE 538 140 1.3 Administrative area: Norton Civil Parish, South Yorkshire County (modern), West Riding of Yorkshire County (historic) 1.4 Current site designation: Not on Historic England’s Register of Historic Parks and Gardens of Special Historic Interest 2. SUMMARY OF HISTORIC INTEREST The landscape of Campsmount Park reflects the continued ownership by the Yarborough family from the 17th century to the 1930s. Thomas Yarborough (1687-1772) masterminded the development of Campsmount Park. With a strong interest in contemporary landscape design, in the early-to-mid 1700s Thomas Yarborough commissioned woodland walks, tree planting, a summer house and a walled garden on the slopes to the north of his existing house, Brayton Hall. In the 1750s he completed his revised estate with the construction of his new house, Campsmount, designed by Robert Carr, and Campsmount (Home) Farm, designed by his son, John Carr. Brayton Hall was demolished. George Cooke-Yarborough, a successor in the early 19th century, made some changes to Campsmount and commissioned a new landscape plan from John Webb of Staffordshire. However, little of the plan was effected apart from the enlargement of five existing fish ponds to form one much larger fish pond. Although minor amendments were made to the walled garden and pleasure grounds in the late 19th century, the landscape design remained mostly unaltered until the mid-20th century. Campsmount, the summer house and contents of the walled garden were demolished in the 1950s. -
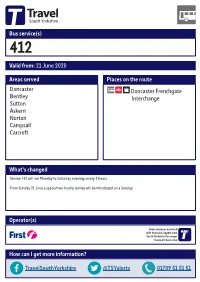
Valid From: 21 June 2020 Bus Service(S) What's Changed Areas
Bus service(s) 412 Valid from: 21 June 2020 Areas served Places on the route Doncaster Doncaster Frenchgate Bentley Interchange Sutton Askern Norton Campsall Carcroft What’s changed Service 412 will run Monday to Saturday evenings every 2 hours. From Sunday 21 June a special two hourly service will be introduced on a Sunday. Operator(s) Some journeys operated with financial support from South Yorkshire Passenger Transport Executive How can I get more information? TravelSouthYorkshire @TSYalerts 01709 51 51 51 Bus route map for service 412 19/07/2016# Norton, West End Rd/Broc-O-Bank Fenwick Ñ Norton Kirk Smeaton 412 Campsall, High St/ Campsall, Old Bells/High St Church View Moss Barnsdale Bar Campsall 412 Ñ Askern, Selby Rd/ Ð Campsall Rd Askern, Norbreck Rd/Plantation Cl Ô Askern Askern, Station Rd/High St Ò Sutton Sutton, Sutton Rd/Manor Farm Cl Burghwallis Braithwaite Owston Skellow Toll Bar, Doncaster Rd/Askern Rd Carcroft Barnby Dun Hampole Carcroft, High St/Park Av 412 Carcroft, High St/Queens Rd Toll Bar Adwick Le Street Toll Bar, Doncaster Rd/Bentley Moor Ln Woodlands Kirk Sandall Arksey Pickburn Highfields Scawthorpe Bentley Bentley, High St/Central Av Marr Scawsby database right 2016 and Wheatley yright Cusworth p o c own r C Intake data © y e v Sur e Sprotbrough c Doncaster, Frenchgate Interchange 412 dnan r O High Melton ontains Belle Vue C 6 = Terminus point = Public transport = Shopping area = Bus route & stops = Rail line & station = Tram route & stop Stopping points for service 412 Doncaster, Frenchgate Interchange North -

South Yorkshire
INDUSTRIAL HISTORY of SOUTH RKSHI E Association for Industrial Archaeology CONTENTS 1 INTRODUCTION 6 STEEL 26 10 TEXTILE 2 FARMING, FOOD AND The cementation process 26 Wool 53 DRINK, WOODLANDS Crucible steel 27 Cotton 54 Land drainage 4 Wire 29 Linen weaving 54 Farm Engine houses 4 The 19thC steel revolution 31 Artificial fibres 55 Corn milling 5 Alloy steels 32 Clothing 55 Water Corn Mills 5 Forging and rolling 33 11 OTHER MANUFACTUR- Windmills 6 Magnets 34 ING INDUSTRIES Steam corn mills 6 Don Valley & Sheffield maps 35 Chemicals 56 Other foods 6 South Yorkshire map 36-7 Upholstery 57 Maltings 7 7 ENGINEERING AND Tanning 57 Breweries 7 VEHICLES 38 Paper 57 Snuff 8 Engineering 38 Printing 58 Woodlands and timber 8 Ships and boats 40 12 GAS, ELECTRICITY, 3 COAL 9 Railway vehicles 40 SEWERAGE Coal settlements 14 Road vehicles 41 Gas 59 4 OTHER MINERALS AND 8 CUTLERY AND Electricity 59 MINERAL PRODUCTS 15 SILVERWARE 42 Water 60 Lime 15 Cutlery 42 Sewerage 61 Ruddle 16 Hand forges 42 13 TRANSPORT Bricks 16 Water power 43 Roads 62 Fireclay 16 Workshops 44 Canals 64 Pottery 17 Silverware 45 Tramroads 65 Glass 17 Other products 48 Railways 66 5 IRON 19 Handles and scales 48 Town Trams 68 Iron mining 19 9 EDGE TOOLS Other road transport 68 Foundries 22 Agricultural tools 49 14 MUSEUMS 69 Wrought iron and water power 23 Other Edge Tools and Files 50 Index 70 Further reading 71 USING THIS BOOK South Yorkshire has a long history of industry including water power, iron, steel, engineering, coal, textiles, and glass. -

Investing in South Yorkshire Introducing Northern Powergrid
INVESTING IN SOUTH YORKSHIRE INTRODUCING NORTHERN POWERGRID Here at Northern Powergrid we work behind the scenes to deliver electricity to 3.9 million businesses and homes in the North East, Yorkshire and northern Lincolnshire. Our network consists of more than 61,000 substations and around 93,000 kilometres Operating in South Yorkshire of overhead lines and underground cables. This booklet provides you with a handy We have more than 2,200 employees who personalised directory of our services work to keep the lights on for our in South Yorkshire. 8 million customers. We have included information about our Our operating zones are coordinated so we investment schemes across the region and can tailor our services and our response to the full range of other services we provide. the needs of you and your local community. Our services complement much of the We moved from five larger zones to nine work that local authorities and Local zones defined by their industrial, urban or Enterprise Partnerships have responsibility rural landscape. This operating model for and we want to work as closely as demonstrates our commitment to improving possible with other local partners to help service and providing locally based managers achieve these objectives. These range from who are able to keep in touch with the local taking care of our vulnerable customers, community to understand the best way we promoting skilled careers to school and can meet your needs. college students, supporting economic growth, reducing crime and minimising our environmental impact. As one of our urban operating zones, South Yorkshire covers the main cities and towns of Sheffield, Rotherham, Doncaster and Barnsley. -

Registered Pharmacies 2019-07-12
The list of pharmacies registered to sell PPCs on our behalf is sorted alphabetically in postcode order. 0 NAME PREMISES ADDRESS 1 PREMISES ADDRESS 2 PREMISES ADDRESS 3 PREMISES ADDRESS 4 POSTCODE LLOYDS PHARMACY SAINSBURYS, EVERARD CLOSE ST ALBANS HERTFORDSHIRE AL1 2QU BOOTS UK LIMITED 9 ST PETERS STREET ST.ALBANS HERTFORDSHIRE AL1 3DH FREEMAN GRIEVES LTD 111-113 ST PETERS STREET ST.ALBANS HERTFORDSHIRE AL1 3ET LLOYDS PHARMACY PARKBURY HOUSE ST PETER ST ALBANS HERTFORDSHIRE AL1 3HD IMED PHARMACY 67 HATFIELD ROAD ST ALBANS HERTFORDSHIRE AL1 4JE ST ALBANS PHARMACY 197 CELL BARNES LANE ST ALBANS HERTFORDSHIRE AL1 5PX LLOYDS PHARMACY SAINSBURYS, BARNET ROAD LONDON COLNEY ST ALBANS HERTFORDSHIRE AL2 1AB LLOYDS PHARMACY 17 RUSSELL AVENUE ST ALBANS HERTFORDSHIRE AL3 5ES NORMANDY PHARMACY 52 WAVERLEY ROAD ST ALBANS HERTFORDSHIRE AL3 5PE CROWN PHAMRACY 65 HIGH STREET REDBOURN ST ALBANS HERTFORDSHIRE AL3 7LW MANOR PHARMACY (WHEATHAMPSTEAD) LTD 2 HIGH STREET WHEATHAMPSTEAD HERTFORDSHIRE AL4 8AA BOOTS UK LIMITED 23-25 HIGH STREET HARPENDEN HERTFORDSHIRE AL5 2RU LLOYDS PHARMACY 40 HIGH STREET WELWYN GARDEN CITY HERTFORDSHIRE AL6 9EQ LLOYDS PHARMACY 84 HALDENS WELWYN GARDEN CITY HERTFORDSHIRE AL7 1DD BOOTS UK LIMITED 65 MOORS WALK WELWYN GARDEN CITY HERTFORDSHIRE AL7 2BQ BOOTS UK LIMITED 31 COLE GREEN LANE WELWYN GARDEN CITY HERTFORDSHIRE AL7 3PP PEARTREE PHARMACY 110 PEARTREE LANE WELWYN GARDEN CITY HERTFORDSHIRE AL7 3UJ BOOTS UK LIMITED 126 PEARTREE LANE WELWYN GARDEN CITY HERTFORDSHIRE AL7 3XY BOOTS UK LIMITED 31 THE HOWARD CENTRE WELWYN GARDEN -

Uk Regional Development Programme 1986-90
EUROPEAN REGIONAL DEVELOPMENT FUND UK REGIONAL DEVELOPMENT PROGRAMME 1986-90 Section 7E: England — South Yorkshire Section 7F: England — Workington Section 7G: England — Greater Manchester Section 7H: England — Greater Merseyside lUlaUmiãl· I U If ΦΟ DOCUMENT DOCUMENTI CUMENT DOCUMENTO DOK1 ¡NT ΕΓΓΡΑΦΟ DOCUMENT DI JMENTO DOCUMENT UUCUM TU ηυκυΜΕΝΤΕΓΓΡΑΦΟηΐ (MENT DOCUMENTO OUCUMI MHB ΡΑΦΟΟΟΟΟΜΕΜ I tvivl COMMISSION POOGIIIÌEN^DOG OF THE EUROPEAN COMMUNITIES ΝΤΕΓΓΡΑΦ( uranFrinii nni-iiupuiiiAnAni This document has been prepared for use within the Commission. It does not necessarily represent the Commission's official position. Cataloguing data can be found at the end of this publication Luxembourg: Office for Official Publications of the European Communities, 1987 Vol.3 : ISBN 92-825-7194-7 Vol. 1-7: ISBN 92-825-7199-8 Catalogue number: CB-98-87-00J-EN-C © ECSC-EEC-EAEC, Brussels · Luxembourg, 1987 Reproduction is authorized, except for commercial purposes, provided the source is acknowledged. Printed in Belgium Commission of the European Communities European Regional Development Fund UK RE6I0NAL DEVELOPMENT PROGRAMME 1986-90 Section 7E: EngLand - South Yorkshire Section 7F: EngLand - Workington Section 7G: EngLand - Greater Manchester Section 7H: EngLand - Greater Merseyside Document This document has been prepared for use within the Commission. It does not necessarily represent the Commission's official position. Copyright ECSC-EEC-EAEC, Brussels - Luxembourg, 1987 Reproduction is authorized, except for commercial purposes, provided the source is acknowledged. / L European Regional Development Fund UK REGIONAL DEVELOPMENT PROGRAMME 1986-90 Section 7E: England - South Yorkshire d UCJ [ \j \ 1' UK REGIONAL DEVELOPMENT PROGRAMME 1986-90 CONTENTS The Programme consists of detailed information on regional or sub-regional areas (Sections 7 to 10) preceded by general information on the United Kingdom (Sections 1 to 6). -

Otc Medicines Independent Report Prepared by Standout Media Limited for South Yorkshire and Bassetlaw Ics
OTC MEDICINES INDEPENDENT REPORT PREPARED BY STANDOUT MEDIA LIMITED FOR SOUTH YORKSHIRE AND BASSETLAW ICS DECEMBER 2018 2 OTC MEDICINES INDEPENDENT REPORT Contents Introduction and purpose 3 About the South Yorkshire and Bassetlaw area and its population 4 Who was involved? 5 About the insight and engagement campaign 6 Who were our target audiences? 7 Methodology 7 Toolkits 9 About the people who engaged with us 11 Patient and public survey 14 What did the patients and public tell us? 16 Staff engagement 19 Community engagement 21 Social media 22 Website statistics 24 How our insight campaign compares 26 What we propose – next steps 27 Awards 29 Appendices Appendix 1 – SYB ICS partner organisations 30 Appendix 2 – Rotherham CCG Start Well, Choose Well, Stay Well campaign assets 32 Appendix 3 – SYB ICS Citizens’ Panel 33 Appendix 4 – Patient and public survey results in graphs 34 Appendix 5 – Prescriber survey results in graphs 41 Appendix 6 – Doncaster prescriber survey results 45 Appendix 7 – Barnsley consultation report 67 Appendix 8 – GP practices by CCG area 89 Appendix 9 – Community pharmacies by CCG area 95 Appendix 10 – Parish councils by CCG area 105 Appendix 11 – Libraries by CCG area 107 Appendix 12 – Community centres by CCG area 109 Appendix 13 – ONS data by CCG area 112 Appendix 14 – MPs by CCG area 117 Appendix 15 – Comms toolkit 118 3 OTC MEDICINES INDEPENDENT REPORT Introduction and purpose In early 2018 NHS England carried out a public consultation on reducing prescribing of over the counter (OTC) medicines for minor, short-term health concerns which could save the NHS high costs and encourage more people to self-care. -

Doncaster Cycling Map
6 A 6 N V T O 4 W 3 E B Bentley Moor E A R N H 2 E 8 L O Wood N R M E 2 C TH OA R D A OR D M N L IN W E I D E V S A N P L I V E BO E L EADO F T N IV O A M W IE S U R R N F H E E D T E H F V E L U R BE T E AR I Dunscroft M A R S L O UM EN O LO M L W V N O W C PA A NT A UTTERW R E RK G O L E N Y ORT T R W E Barnby Dun O R AV H UT U S Adwick D U D O A T EN L B Y R B U R AD A E M E WIC S IV A E K LA Common V T E C T NE E F N T A 9 H E U H V C PO 1 E S E A H N E C E R A AVE D I GTON I K T ENNIN R YN IN O K C L N U GSLE A I Y V Adwick Pk E T R E E B V L O N N D A A A A U LA Jun Sch A W D O C E K E L R K Barnby Dun Frickley OOD N E A R U V B E L W A A R T A E N E E S R E V T N A S N N A Common H V E R E C E H A Park Hill N U T A N F T A B D Playing Fields O SB U IN W D U E Almholme Hooton R Y SW Outwood IC A Grange AVENUE ADWICK K R 49 50 51 52 53 W54 55 56 57 Shaftholme 58 59 60 61 62 63 64 L M Town and country maps with hundreds of miles of routes E A A N Academy S N E T E N Grumble Hurst H Pagnell R H LA O I A O G N L R B LE STREET L M R G I OO P L S O T V O North Ridge L O E S O L R L E CLAYT U LAN V N A NE AN L ON L ALK H LA E E A ANE N GE B Community E R TPT SHAFT ME G PO ID E N HOL H C N R D R C D N O Q C E A E L E E A E Lound Hill L L X R S U E N A School T O S U K R RT E N 'S O D N L O T N M D G E A N O E A A S E B N ECT R V R Plantation R E O O N V S L V R ND U O O U L O R O A R A I I Toll Bar R E T A N L A V R O D ENT N M L R T A ESC D Almholme Field I E I G E A V R E D A EW E E O E C N V V T D IV E D I V I T G N S E E R R Prim Sch -

Corporate Performance Report 2020-21
SOUTH YORKSHIRE FIRE & RESCUE AUTHORITY Meeting PERFORMANCE AND SCRUTINY BOARD Meeting Date 10 SEPTEMBER 2020 CHIEF FIRE OFFICER & CHIEF EXECUTIVE / CLERK TO THE FIRE Report of AND RESCUE AUTHORITY DEPUTY CHIEF FIRE OFFICER / CHIEF OPERATING OFFICER & Report Sponsor(s) DIRECTOR OF SERVICE DEVELOPMENT CORPORATE PERFORMANCE REPORT - QUARTER ONE - 2020/21 & Subject FORWARD LOOK TO HALLOWEEN AND BONFIRE NIGHT PERIOD – 2020 EXECUTIVE SUMMARY This report provides members with information on how South Yorkshire Fire and Rescue (SYFR) has performed against our Local Performance Indicators (LPIs) during quarter one of 2020/21. It also provides a forward look at the planned initiatives and prevention work that will take place during the Halloween and Bonfire Night period, 2020. It enables Members to comment upon the performance and explore in more detail the work behind the statistics. The dashboards in the report offer a view of our performance against each of our LPIs. These measures, approved by members, help us to gauge how we are doing against our priorities. Nine LPIs are monitored using ‘tolerance levels’, which provide a range of acceptable performance levels. Areas where we have performed well in quarter one include: Fires in non-domestic premises were particularly low in quarter one, with 43 incidents. In quarter one of 2019/20 there were 84. The low number of these fires could be attributable to the Covid-19 lockdown, however they were at a similar level during quarter one in 2014/15. The number of accidental dwelling fires was the second lowest out of the previous 12 years. Only quarter one of 2018/19 had a lower number at 131. -

412 Bus Time Schedule & Line Route
412 bus time schedule & line map 412 Campsall <-> Doncaster Town Centre View In Website Mode The 412 bus line (Campsall <-> Doncaster Town Centre) has 4 routes. For regular weekdays, their operation hours are: (1) Campsall <-> Doncaster Town Centre: 5:30 AM (2) Carcroft <-> Doncaster Town Centre: 7:00 PM - 9:15 PM (3) Doncaster Town Centre <-> Campsall: 6:15 AM (4) Doncaster Town Centre <-> Carcroft: 8:15 PM - 10:15 PM Use the Moovit App to ƒnd the closest 412 bus station near you and ƒnd out when is the next 412 bus arriving. Direction: Campsall <-> Doncaster Town Centre 412 bus Time Schedule 51 stops Campsall <-> Doncaster Town Centre Route VIEW LINE SCHEDULE Timetable: Sunday Not Operational High Street/Church View, Campsall Monday Not Operational The Avenue/Byron Avenue, Campsall Tuesday 5:30 AM Byron Avenue, Norton Civil Parish Wednesday 5:30 AM Ryecroft Road/The Avenue, Campsall Thursday 5:30 AM Ryecroft Road/Windmill Lane, Campsall Friday 5:30 AM West End Road/Broc-O-Bank, Norton Saturday 5:30 AM West End Road/Fir Tree Drive, Norton High Street/Arundel Road, Norton 412 bus Info Station Road/Ashburnham Close, Norton Direction: Campsall <-> Doncaster Town Centre Stops: 51 Station Road/Cridling Gardens, Norton Trip Duration: 41 min Line Summary: High Street/Church View, Campsall, Hawke Close, Norton Civil Parish The Avenue/Byron Avenue, Campsall, Ryecroft Norton Common Road/Selby Road, Norton Road/The Avenue, Campsall, Ryecroft Road/Windmill Lane, Campsall, West End Road/Broc-O-Bank, Norton, West End Road/Fir Tree Selby Road/Station -
Carcroft Health Centre QA Visit
Screening Quality Assurance visit report NHS Cervical Screening Programme Carcroft Health Centre 21 July 2017 Public Health England leads the NHS Screening Programmes Screening Quality Assurance visit report: NHS Cervical Screening Programme About Public Health England Public Health England exists to protect and improve the nation’s health and wellbeing, and reduce health inequalities. We do this through world-leading science, knowledge and intelligence, advocacy, partnerships and the delivery of specialist public health services. We are an executive agency of the Department of Health and Social Care, and a distinct delivery organisation with operational autonomy to advise and support government, local authorities and the NHS in a professionally independent manner. Public Health England, Wellington House, 133-155 Waterloo Road, London SE1 8UG Tel: 020 7654 8000 www.gov.uk/phe Twitter: @PHE_uk Facebook: www.facebook.com/PublicHealthEngland About PHE Screening Screening identifies apparently healthy people who may be at increased risk of a disease or condition, enabling earlier treatment or better informed decisions. National population screening programmes are implemented in the NHS on the advice of the UK National Screening Committee (UK NSC), which makes independent, evidence-based recommendations to ministers in the 4 UK countries. The Screening Quality Assurance Service ensures programmes are safe and effective by checking that national standards are met. PHE leads the NHS Screening Programmes and hosts the UK NSC secretariat. www.gov.uk/phe/screening Twitter: @PHE_Screening Blog: phescreening.blog.gov.uk Prepared by: Screening QA Service (North). For queries relating to this document, please contact: [email protected] © Crown copyright 2018 You may re-use this information (excluding logos) free of charge in any format or medium, under the terms of the Open Government Licence v3.0.